Back to Journals » Patient Related Outcome Measures » Volume 10
Optimistic bias: the more you do, the better you think it goes. Survey analysis of reverse shoulder arthroplasty
Authors Torrens C , Miquel J, Santana F
Received 7 June 2019
Accepted for publication 14 August 2019
Published 27 August 2019 Volume 2019:10 Pages 277—282
DOI https://doi.org/10.2147/PROM.S218710
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Carlos Torrens,1 Joan Miquel,2 Fernando Santana1
1Department of Orthopedic Surgery, Hospital del Mar, Barcelona, Spain; 2Department of Orthopedic Surgery, Consorci Hospitalari Igualada, Igualada, Spain
Correspondence: Carlos Torrens
Department of Orthopedic Surgery, Hospital del Mar, Barcelona, Spain
Tel +34 9 360 975 3620
Fax +34 93 248 3196
Email [email protected]
Objective: Even though heuristics are very helpful, several biases have been described related to their use. The aim of this study is to analyze the influence of surgery volume on the surgeon’s perception of pain improvement in patients after having received a reverse total shoulder arthroplasty.
Design: Successive independent samples study.
Setting: Shoulder surgeons attending four shoulder meetings.
Participants: 149 Shoulder surgeons were included.
Intervention: Physicians were asked to postulate the preoperative and postoperative pain of patients receiving a reverse shoulder arthroplasty and respond by putting a mark on two visual pain scales.
Main outcome measures: Pain improvement, years of shoulder practice, number of shoulder studies read over 6 months and the number of reverse shoulder arthroplasties performed per year. To compare the answers of the survey-study, a cohort of 95 patients who had undergone reverse shoulder Arthroplasty because of a rotator cuff arthropathy were prospectively followed.
Results: Regarding the pain score before and after surgery, the patient cohort showed a mean improvement of 6.84 points. In terms of the doctors, the more years of surgical practice, led them to have a greater expectation of improvement (p=0.004). Moreover, the greater the number of prostheses they implanted, the greater the expectation of improvement (p=0.0005). It was the same in terms of the number of studies read by them (p=0.001).
Conclusions: Years of practice, hospital position and the number of shoulder arthroplasties done per year all favor the surgeon’s perception that their patients obtain a greater pain relief after receiving a shoulder arthroplasty than the real improvement in pain relief the patients experience.
Keywords: pain measurement, heuristics, outcome assessment, shoulder, arthroplasty
Plain language summary
The author’s wanted to test the assumption that surgeons doing a lot of surgeries tend to believe that their patients do better than they really do. For that purpose, a survey-study was carried out in which shoulder surgeons attending meetings were asked to rate the pain their patients had before and after surgery to evaluate the pain relief they thought their patients obtained. Surgeons were categorized by surgery volume, hospital position and years of surgical practice. The data obtained from the surgeons was compared with the real improvement that the patients perceived after receiving surgery. The results of the study show that the chiefs were the more pessimistic ones in thinking that the patients had more pain than they really had before surgery. Moreover, surgeons doing a lot of surgeries think that their patients improve significantly more than they really do. This fact may potentially create unrealistic patient expectations and predispose patients to acquiescing to surgery.
Introduction
The psychology of decision-making is becoming a more and more useful tool to analyze medical decisions.1–8 When doctors are confronted with probabilistic data, they quite often use heuristics to come up with a diagnosis or a treatment strategy. Heuristics can be defined as simple decision-making strategies that make for arriving at a decision without the need to analyze all the available information on the issue at hand. Even though heuristics are very helpful in saving time and mainly lead doctors to making good decisions, several biases have been described related to their use. They include, among others, the anchoring bias, availability bias, status quo bias and optimist bias or optimistic overconfidence.9–11
Diagnostic errors and overtreatment present a threat of harming patients as well as the possibility of resource wastage. Diagnostic error prevalence can be as high as 10–15%. Although the causes seem to be multifactorial, cognitive biases are also involved.12–16 In a recent study, the physicians admitted that the 20.6% of overall medical care was unnecessary. That percentage includes prescriptions for medications, tests and procedures.17
Shoulder arthroplasty procedures have increased exponentially from 14.000 in 2000 to nearly 47.000 in 2008.18 However, the distribution of shoulder replacement procedures among surgeons and hospitals remains unequal and very different when compared to hip and knee, with only a few high-volume surgeons (3%) doing most of the shoulder replacements (more than 10 per year). Then again, most shoulder surgeons do very few cases per year.19–21 The reasons for this unequal distribution are multifactorial but cognitive bias might also influence it to some extent.
The aim of this study is to analyze the influence of surgery volume on the surgeon’s perception of improvement in terms of pain in patients after having received a reverse total shoulder arthroplasty.
Methods
A successive independent samples study was performed during four shoulder meetings that were held from March 2017 to November 2017. All the doctors attending the meetings were asked to participate in a survey during the meeting. There were 2 shoulder meetings at the national level and 2 at the international level with surgeons from several different countries. The surgeons attending the meetings were advised not to fill out the survey if they had done it in a previous meeting. The survey included epidemiological data such as the surgeon’s age, years of shoulder practice, the number of shoulder studies published in indexed journals and those read over the last 6 months, number of reverse shoulder arthroplasties performed per year and the position of the medical doctor in the Hospital. After that, the physicians were asked to answer the following two questions by putting a mark on a 15cm visual pain scale:
- Point out (where A is the absence of pain and B the maximum pain imaginable) what level of pain the patients who are candidates to receive a reverse prosthesis for cuff arthropathy have.
- Point out (where A is the absence of pain and B the maximum pain imaginable) what level of pain the patients have after receiving a reverse prosthesis due to cuff arthropathy.
The visual scale was designed to be 15cm in length to resemble the pain scale recorded in the Constant Score, in which the maximum pain is 0 and minimum pain is 15 points.22
To compare the answers of the survey-study, a cohort of 95 patients who had undergone reverse shoulder arthroplasty because of rotator cuff arthropathy were prospectively followed for a minimum of 2 years. Preoperative pain and postoperative pain at a minimum of two years follow-up was recorded for this selected cohort of patients with the aid of the Constant Score.
The Comité Ético de Investigación Clínica–Parc de Salut Mar approved this study (number 2018/8379/I). In addition, the patient cohort provided written informed consent.
Statistical analysis
Preoperative and postoperative pain assessment by the staff group was checked with the one-way ANOVA test. Moreover, The Student’s t-test was applied to check differences in accordance with the number of reverse shoulder arthroplasties performed per year. Comparing the survey sample with respect to the cohort of reference, differences in pain with respect to the mean cohort reference were also checked with the Student’s t-test. Differences in pain improvement were checked by means of the same analysis (the one-way ANOVA and Student’s t-test). STATA version 15.1 (StataCorp, College Station, TX, USA) was used for statistical analysis. When the p-values <0.05, they were considered statistically significant.
The sample size was expressly calculated to power the analysis comparing surgeons doing less than 15 prostheses per year with surgeons implanting 15 or more prostheses per year. Accepting an alpha risk of 0.05 and a beta risk of 0.2 in a two-sided test, 30 subjects are necessary in the first group and 90 in the second to recognize a difference greater than or equal to 1.5 units as statistically significant. The common standard deviation was assumed to be 2.5.
Results
Various shoulder surgeons who attended 1 of the 4 meetings in either March, April, September or November of 2017 were included in the study. There were 152 surgeons included that filled out the questionnaire. Three of them were subsequently excluded from the study for not correctly filling out the questionnaire. Thus, the study included 149 surgeons/questionnaires, 108 males and 41 females. Of the surgeons finally included, there were 23 residents, 101 staff members devoted to the shoulder and 25 chiefs of shoulder units. The mean time in shoulder practice was of 15.3 years (SD 10.3). The mean number of shoulder replacements per year was of 11.4 (SD 27.3). The mean number of studies read per 6-month period was of 21.9 (SD 35.1).
The cohort of 95 patients that underwent a reverse shoulder arthroplasty because of rotator cuff arthropathy included 80 females and 15 males with a mean age of 75.2 years (63–87).
The mean preoperative pain determined by the shoulder surgeons was of 4.41. No significant differences (p=0.11) were noted among the medical practitioners. The residents pain perception score was 4.57, the staff members 4.48 and it was 4.0 for the chiefs. No significant differences were noted in preoperative pain perception in terms of years of practice (p=0.38), the number of prostheses implanted (p=0.905) or the number of studies read (p=0.38). The mean preoperative pain score in the patient cohort was of 5.18. The surgeons’ perception of mean preoperative pain was significantly higher than the mean pain referred to by the patients themselves before surgery (p<0.000), being the chiefs the more pessimistic in thinking that the patients had more pain than they really had before surgery.
The mean postoperative pain determined by the shoulder surgeons was 11.86. Significant differences were noted between residents, staff members and chiefs (p=0.02), being the chiefs those who recorded greater improvement. Significant differences were noted in postoperative pain perception according to years of practice (p=0.003), the number of prostheses implanted (p=0.000) and the number of studies read (p=0.001). The mean postoperative pain score in the patient cohort was 12.02. No significant differences were noted between shoulder surgeons’ mean perception of pain after surgery and the pain referred to by the patients after surgery (p=0.29). (Table 1)
 |
Table 1 Preoperative and postoperative pain assessment of surgeons and patients cohort |
Regarding the pain score before and after surgery, the cohort of patients included referred to a mean improvement of 6.84 points. Residents and staff members considered a slightly superior improvement in pain compared to the cohort population (6.90 and 7.35, respectively) while the unit chiefs described greater improvement (8.28). These differences were significant (p=0.03). The determination was that the more years of practice, the greater improvement expected (p=0.004), the higher the number of prostheses implanted, the greater the improvement expected (p=0.0005). It was the same in terms of the number of studies read (p=0.001). Stratifying the number of shoulder arthroplasties performed per year between less than 15 shoulder replacements and more than 15 replacements, these differences were maintained (7.15 and 8.29 respectively) (p=0.003). (Table 2)
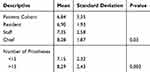 |
Table 2 Difference in pain improvement assessment (postop minus preop) between surgeons and patients cohort |
Discussion
The more surgeries the surgeons do, the better they think it goes. Surgeons with more years of practice and who perform a greater number of procedures involving prosthesis per year think that their patients have greater pain relief than might be the case. There is the potential for this bias to lead to overtreatment.
When doctors confront large amounts of information and complex probabilistic scenarios in the decision-making process, heuristics can be helpful in simplifying the task.3,23 However, the use of heuristic strategies may lead to several systematic errors including, but not limited to, the anchoring bias, availability bias, status quo bias and optimist bias or optimistic overconfidence.9–11 Overconfidence has been related to diagnostic error in medicine.10 Diagnostic error in medicine can be as high as the 10–15% of all diagnosis,10–14 and seem to be more related to systematic bias rather than to knowledge deficits.12 Senior residents seem to do better than more experienced residents when managing heuristic scenarios on trauma teams in providing initial care to a severely injured patient. The reason for that might be that more experienced residents are more reliant on heuristic approaches.15
In the present study, doctors having more years of experience perceive that the improvement in pain of their patients undergoing shoulder replacement is greater than the improvement in pain perceived by the doctors with less experience. The higher a doctor’s position in the hierarchy of the hospital also significantly correlates with greater pain improvement perception, with Chiefs’ giving higher improvement values than staff members or residents. Moreover, years of experience and hospital position lead to estimating that patients have greater pain improvement than that observed in a real cohort of patients.
Overtreatment has been considered a source of preventable harm in health care. In a recent study, physicians reported that a median of 20.6% of medical actions were unnecessary. That figure includes 22.0% of medication prescriptions, 24.9% of diagnostic tests and 11.1% of procedures. The reasons for overtreatment are multifactorial. They include fear of malpractice (84.7%) and patient pressure/requests (59.0%).17 The results of this study show that there is a positive correlation between the number of the shoulder replacements prescribed and the doctor’s perception of pain improvement. The greater the number of shoulder replacements, the more the surgeon thinks that pain references improve. There is the potential for this to have an influence on shoulder replacement overtreatment. High-volume surgeons think that the results are better than they are and this can potentially influence the patient’s decision-making relative to the shoulder arthroplasty indication.
The distribution of shoulder replacements among surgeons and hospitals is different than that of hip and knee replacement as is the distribution of high-volume shoulder arthroplasty surgeons in the United States.18–21 Few surgeons do a high number of shoulder replacements. In fact, many surgeons only do a very limited number. In Catalonia, the hospitals in the public health system, the Catsalut hospitals, produce about 0.009 shoulder procedures per 1,000 insured persons each year in their healthcare region. Among the different hospitals there is a variability of 117 surgeries performed among the 5th and 95th percentiles, which means that the hospital that falls in the 95th percentile does 117 times more procedures than the hospital that is in the 5th percentile.24 The reason for this extreme difference is multifactorial but the results of the present study support the tendency for higher-volume surgeons to keep on doing more surgeries and for low-volume surgeons to keep on doing few procedures. The high-volume shoulder surgeons believe that their patients obtain greater pain relief than may be the case and are potentially more prone to see indications for shoulder replacement. Low-volume shoulder surgeons are more modest in their thoughts related to pain improvement and might be less prone to see indications for shoulder replacement.
It is still not clear whether high-volume hospitals and surgeons are more desirable rather than low-volume hospitals and surgeons. First, no volume standard exists and almost all studies arbitrarily chose thresholds.25 Secondly, while it has been reported that mortality rates for patients are higher if shoulder arthroplasty is performed by surgeons doing fewer than two procedures a year or between two and four procedures (0.36% and 0.32%, respectively) when compared with mortality rates of surgeons doing four or more procedures a year (0.20%), a recent systematic review concludes that there is insufficient evidence to support the concept that only the number of shoulder arthroplasties performed (either per hospital or per surgeon) results in better patient reported outcomes as well as functional outcomes.25
Among the limits of the present study are the fact that the reasons for doing more or fewer shoulder arthroplasty surgeries are multifactorial. Furthermore, the authors only analyze one of them and the conclusions are only applicable to reverse shoulder arthroplasty. Among the strengths are the number of participants and the small number of incomplete surveys.
Conclusion
In conclusion, the hospital position in terms of hierarchy influences the perception of pain before surgery, being the chiefs the more pessimistic. The years of surgical practice, the position in the hospital hierarchy and the number of shoulder arthroplasties done per year all favor the surgeon’s perception that their patients obtain a greater pain relief after receiving a shoulder arthroplasty than the real improvement in terms of pain that the patients experience. The difference of 1.45 points of improvement might not be very relevant for patients, but what the authors wanted to analyze in the present study was whether surgeons doing more surgeries thought that their patients improved more than they really did. That they thought so has been shown to be true (1.45 more) and to a significant degree (p<0.000) in this study. Therefore, the surgeon’s perception potentially has an effect on the patient-decision making process.
Ethics approval and informed consent
The Comité Ético de Investigación Clínica–Parc de Salut Mar approved this study (number 2018/8379/I).
Acknowledgment
The authors thank Xavier Duran Jordà, MStat, PhD (AMIB [Assessoria metodològica i Bioestadística], IMIM [Institut Hospital del Mar d’Investigacions Mèdiques]) for his work on data analysis. The authors also wish to thank Xavier Garcia, MSc., Àrea d’Avaluació | Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS), Departament de Salut | Generalitat de Catalunya for his help gathering the data of Catalonian Shoulder Arthroplasty. The authors have not received any financial support for the preparation of this paper.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wegwarth O, Gaissmaier W, Gigerenzer G. Smart strategies for doctors and doctors-in-training: heuristics in medicine. Med Educ. 2009;43:721–728. doi:10.1111/j.1365-2923.2009.03359.x
2. Croskerry P. From mindless to mindful practice. Cognitive bias and clinical decision making. N Engl J Med. 2013;368:2445–2448. doi:10.1056/NEJMp1303712
3. Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185:1124–1131. doi:10.1126/science.185.4157.1124
4. Kahneman D, Tversky A. Choices, values, and frames. Am Psychologist. 1984;39(4):341–350. doi:10.1037/0003-066X.39.4.341
5. Kahneman D, Klein G. Conditions for intuitive expertise. Am Psychologist. 2009;64(6):515–526. doi:10.1037/a0016755
6. Dawson NV, Arkes HR. Systematic errors in medical decision making: judgment limitations. J Gen Intern Med. 1987;2:183–187. doi:10.1007/bf02596149
7. Elstein AS. Heuristics and biases: selected errors in clinical reasoning. Acad Med. 1999;74(2):791–794. doi:10.1097/00001888-199907000-00012
8. Marewski JN, Gigerenzer G. Heuristic decision making in medicine. Dialogues Clin Neurosci. 2012;14:77–89.
9. Blumenthal-Barby JS, Krieger H. Cognitive biases and heuristics in medical decision making: a critical review using a systematic search strategy. Med Decis Making. 2015;35:539–557. doi:10.1177/0272989X1457740
10. Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121:S2–S23. doi:10.1016/j.amjmed.2008.01.001
11. Croskerry P, Norman G. Overconfidence in clinical decision making. Am J Med. 2008;121:524–529. doi:10.1016/j.amed.2008.02.001
12. Norman GR, Eva KW. Diagnostic error and clinical reasoning. Med Educ. 2010;44:94–100. doi:10.1111/j.1365-2923.2009.03507.x
13. Christakis NA, Lamoni EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320:469–472. doi:10.1136/bmj.320.7233.469
14. Graber ML. The incidence of diagnostic error in medicine. BMJ Qual Saf. 2013;22:ii21–ii27. doi:10.1136/bmjqs-2012-001615
15. Murray DJ, Freeman BD, Boulet JR, Woodhouse J, Fehr JJ, Klingensmith ME. Decision making in trauma settings. Simul Healthc. 2015;10:139–145. doi:10.1097/SIH.0000000000000073
16. Wolfson AM, Doctor JN, Burns SP. Clinician judgments of functional outcomes: how bias and perceived accuracy affect rating. Arch Phys Med Rehabil. 2000;81:1567–1574. doi:10.1053/apmr.2000.16345
17. Lyu H, Xu T, Brotman D, et al. Overtreatment in the United States. PLoS One. 2017;12(9):e0181970. doi:10.1371/journal.pone.0181970
18. Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015;24:91–97. doi:10.1016/j.jse.2014.08.026
19. Hasan SS, Leith JM, Smith KL, Matsen III FA. The distribution of shoulder replacement among surgeons and hospitals is significantly different than that of hip or knee replacement. J Shoulder Elbow Surg. 2003;12:164–169. doi:10.1067/mse.2003.23
20. Jain N, Pietrobon R, Hocker S, Guller U, Shjankar A, Higgins LD. The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg. 2004;86-A:496–505. doi:10.2106/00004623-200403000-00006
21. Somerson JS, Stein BA, Wirth MA. Distribution of high-volume shoulder arthroplasty surgeons in the United States. J Bone Joint Surg. 2016;98(1–8):e77. doi:10.2106/JBJS.15.00776
22. Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164.
23. Dawson NV. Physician judgment in clinical settings: methodological influences and cognitive performance. Clin Chem. 1993;39:1468–1480.
24. Divisió d’Anàlisi de la Demanda i l’Activitat. Gerència de Serveis Assistencials. Àrea d’Atenció Sanitària. Servei Català de la Salut. Registre del conjunt mínim bàsic d’hospitalització d’aguts 2012-2017 (CMBD-HA), Sistema integrat d’informació de Salut [base de dades]. 2018. Available from: https://portalsiis.catsalut.cat. Accessed 24 January, 2019.
25. Kooistra BW, Flipsen M, van de Bekerom MPJ, van Raay JJAM, Gosens T, van Deurzen DFP. Shoulder arthroplasty volumen standarts: the more the better? Arch Orthop Trauma Surg. 2018;1:15–23. doi:10.2106/JBJS.15.00776
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
