Back to Journals » Cancer Management and Research » Volume 12
Optimal Laparoscopic Management and Oncological Outcomes of Gastrointestinal Stromal Tumors in Duodenum: Pancreaticoduodenectomy or Pancreas-Sparing Duodenectomy?
Authors Lu C, Jin W, Mou Y, Shao H, Wu X, Li S, Xu B, Wang Y , Zhu Q, Xia T, Zhou Y
Received 27 March 2020
Accepted for publication 29 May 2020
Published 19 June 2020 Volume 2020:12 Pages 4725—4734
DOI https://doi.org/10.2147/CMAR.S254972
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eileen O'Reilly
Chao Lu,1– 3 Weiwei Jin,1,2 Yiping Mou,1,2 Hongliang Shao,4 Xiaosan Wu,4 Shaodong Li,5 Biwu Xu,4 Yuanyu Wang,1,2 Qicong Zhu,1,2 Tao Xia,1,2 Yucheng Zhou1– 3
1Department of Gastrointestinal and Pancreatic Surgery, Zhejiang Provincial People’s Hospital, Hangzhou, Zhejiang Province, People’s Republic of China; 2Key Laboratory of Gastroenterology of Zhejiang Province, Hangzhou, Zhejiang Province, People’s Republic of China; 3School of Medicine, Soochow University, Suzhou, Jiangsu Province, People’s Republic of China; 4School of Medicine, Bengbu Medical College, Bengbu, Anhui Province, People’s Republic of China; 5School of Medicine, Zhejiang Chinese Medical University, Hangzhou, Zhejiang Province, People’s Republic of China
Correspondence: Yucheng Zhou; Yiping Mou
Department of Gastrointestinal and Pancreatic Surgery, Zhejiang Provincial People’s Hospital, Hangzhou, Zhejiang Province, People’s Republic of China
Email [email protected]; [email protected]
Background: Gastrointestinal stromal tumors (GIST) of the duodenum are rarely reported and optimal minimally invasive management has not been well proposed. Pancreaticoduodenectomy and different types of pancreas-sparing duodenectomy can be chosen; however, which to choose and its corresponding clinical outcomes and oncological concerns remain controversial.
Patients and Methods: Patients diagnosed with GIST of duodenum underwent laparoscopic pancreaticoduodenectomy (L-PD) or pancreas-sparing duodenectomy (L-PSD) in Zhejiang Provincial People’s Hospital were enrolled. All prospectively maintained data were analyzed retrospectively. Patients were grouped into the L-PD group or the L-PSD group, and the clinical outcomes and oncological outcomes were analyzed.
Results: Between June 2013 and March 2019, a total of 22 patients (11 males/11 females) underwent surgical management, including 13 L-PDs and 9 L-PSDs. The average age was 58.2± 9.5 year-old (median 60.5 year-old). The most common presentations were GI bleeding (54.5%) and abdominal discomfort (27.2%), and the dominant lesion located in the second portion of duodenum (59.1%). Compared with L-PD group, L-PSD group showed much shorter operation time (364.2± 58.7min vs. 230.0± 12.3min, P< 0.001), less blood loss (176.9± 85.7mL vs. 61.1± 18.2min, P< 0.001), faster recovery to off-bed (2.6± 1.3d vs. 1.1± 0.3d, P=0.003), anus flatus (4.5± 1.0d vs. 2.4± 0.5d, P< 0.001) and liquid intake (4.9± 1.3d vs. 2.3± 0.5d, P< 0.001). Lymph node retrieval was much less in L-PSD, but no lymph node metastasis was observed in any patients. L-PSD had much Lower morbidity of both minor (Grade I/II) and major (III/IV/V) complications than that of L-PD (11.1% vs. 61.6%, P=0.02), resulting in shorter hospital stays (10.9± 3.8d vs. 20.6± 11.1d, P=0.021) and less total cost (76,972.4± 11,614.8yuan vs 125,628.7± 46,356.8yuan, P=0.006). The median follow-up was 42 months (range from 12 to 82months) without loss. Only 1 L-PD patient suffered hepatic metastasis 36months after surgery, and given sunitinib to stabilize the disease, none of the rest observed recurrence or metastasis.
Conclusion: For GIST located opposite the major papilla, L-PSD showed comparable safety and oncological benefits when compared to L-PD, with shorter operation time, less blood loss and much faster recovery time, resulting in much less total cost. L-PSD should be applied in selected patients with experienced hands.
Keywords: GIST, duodenum, pancreaticoduodenectomy, pancreas-sparing duodenectomy
Introduction
Gastrointestinal stromal tumors (GISTs) were reported to be the most common mesenchymal tumors in gastrointestinal tract derived from the Cajal cells.1 GISTs can occur throughout the entire digestive tract; however, the prevailing locations are in the stomach (50–60%) and small intestine (30–35%), duodenal GISTs account for only 3–5%.2 Rare as duodenal GISTs are, the optimal surgical treatment and prognosis remain controversial.
For duodenal GISTs, complete surgical resection with negative margins is the criteria for curative management. Pancreaticoduodenectomy (PD) is commonly performed in terms of the potential of uncertain malignancy and proximity to adjacent pancreatico-biliary organs. However, in most cases PD was considered too aggressive even for oncological reasons with “innocent” resection of pancreas and bile duct,3 moreover, the reconstructions on un-dilated ducts were technically demanding and exerted great risks on postoperative complications.2–5 Pancreas-sparing duodenectomy (PSD) with a negative margin was reported to be technically feasible and presumed to have more functional preservation,3–6 while providing comparable recurrent rate,5,6 and even better long-term prognosis.2 Recently, more and more attempts were stressed on the indication and various surgical procedures,2,5,7 however, no routine methods were established because of the limited cases.
Minimal invasive surgery was recommended for gastric GISTs in various guidelines.8 However, for duodenal GISTs, the optimal minimally invasive surgical (MIS) management has not been proposed or described well. Proper indications and MIS method for different types of pancreas-sparing duodenectomy remained undefined. Moreover, its safety and oncological outcomes were controversial due to few published reports.3,9-11 In this study, we retrospectively concluded and analyzed the clinical outcomes of duodenal GIST that underwent different MIS treatments, including morbidity, economic cost and long-term survival data, then recommend the optimal MIS choice for duodenal GIST.
Patients and Methods
Patients and Methods
Patients who had been diagnosed with duodenal GIST and underwent minimally invasive procedures between June 2013 and March 2019 in Zhejiang Provincial People’s Hospital were enrolled. All lesions were evaluated by CT scan and diagnostic endoscopy, intended for excluding the possibilities of endoscopic resections and confirming the location of the tumor and Vater’s papilla as well. Surgical managements included minimally invasive procedures, and varied from pancreaticoduodenectomy to different types of pancreas-sparing duodenectomy based on tumor size and location. This study was approved by the Institutional Review Board and Ethics Committees of Zhejiang Provincial People’s Hospital. All patients were informed with the written consents in accordance with the Declaration of Helsinki.
All the clinical data were retrospectively reviewed based on prospectively maintained database, including perioperative data, pathological parameters, adjuvant therapy, morbidity, mortality and long-term oncological outcomes. Pathological diagnosis was confirmed by 2 specialized pathologist and risk stratifications were classified based on NIH consensus.12 Pancreatic fistula and postoperative hemorrhage were defined and classified according to the International Study Group of Pancreatic Fistula (ISGPF) criteria.13,14 Furthermore, complications were all classified using the Clavien-Dindo classification.15 All the clinical outcomes of duodenal GIST that underwent PD and PSD were compared, including morbidity, economic cost and long-term survival.
Indication and Surgical Techniques
All patients underwent minimally invasive procedure with the intent to completely remove tumors without rupture. The extent of procedure and various types of operation were determined based on the tumor size and proximity to the Vater’s papilla (Figure 1). For duodenal GISTs with diameter greater than 5cm or lesions located on the same side of the major duodenal papilla, laparoscopic pancreaticoduodenectomy (L-PD) was indicated and performed. However, for supra-ampulla and infra ampulla duodenal GISTs that were less than 5cm, and the lesions that were located opposite to the major papilla, laparoscopic pancreas-sparing duodenectomy (L-PSD) was suggested and performed.
 |
Figure 1 Flow diagram and indication for laparoscopic pancreaticoduodenectomy (L-PD) or laparoscopic pancreas-sparing duodenectomy (L-PSD) for duodenal GISTs. |
Laparoscopic Pancreaticoduodenectomy (L-PD)
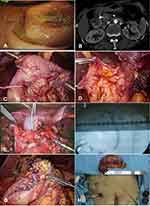
The L-PD procedure has been described in a previously published study.15 All L-PDs were performed as standard PD without pylorus preservation. We routinely used the modified approach based on the “Five Trocars” method to perform L-PD (Figure 2). Make sure to dissect the specimen gently and never grab the tumor directly to prevent tumor rupturing and spreading. After the specimens were removed from the enlarged umbilical port, a frozen section was sent to confirm the duodenal GISTs and negative margins. Because of the un-dilated pancreatic and bile ducts, the reconstruction was performed with duct-to-mucosa pancreatojejunostomy and interrupted sutures hepaticojejunostomy.16
Laparoscopic Pancreas-Sparing Duodenectomy (L-PSD)
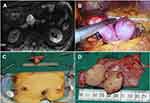
For small duodenal lesions located opposite the major papilla, different types of L-PSD were performed based on the relative location of the Vater’s papilla (Figures 3 and 4). These patients underwent preoperative endoscopy (Figure 3A), intended to evaluate and locate the proximal/distal margins of tumors and the Vater’s papilla. Dye or clips were also used (Figure 3B).
For supra-ampulla lesions (Figure 3), the gastro-colic ligament was divided first and then the Kocher maneuver was made to have better exposure of the pancreatic head and the duodenal. After the right gastro-epipoloic vessels were dissected, we used ultrasonic shears to gradually separate the duodenum from the pancreatic head, all the vessels that supply to the targeted duodenum rather than pancreas were carefully dissected and coagulated from cephalad to caudad (Figure 3C). Then the dissection plane was extended stepwise to the pre-set margin marked by dye or clips. After mobilization, the proximal margin was transected by linear stapler. However, when dissecting the distal margin one should not use a stapler to keep the ampulla intact. Usually, we incised directly along the preset margin (Figure 3D) and perform Intraoperative cholangiogram (IOC) to locate the ampulla with definite preservation. We keep the catheter along the common bile duct all the way to the outlet of ampulla (Figure 3E and F), and with the guidance of catheter the opening was closed by hand-sewn suture without injuring the ampulla (Figure 3G). At last, an ante-colic loop gastrojejunostomy was completed approximately 20cm from the Treiz ligament.
As for infra-ampulla lesions (Figure 4), the duodenum was also exposed by dividing the gastro-colic ligament and Kocherization. Moreover, complete separation from retro-peritoneum and mesocolon was completed to detach the descending and horizontal parts of the duodenum. Next, proximal jejunum for distal margin was mobilized from the Treitz ligament and transected with a linear stapler, then placed it to the right of the SMA through the retro-mesenteric root. Similarly, all the responsible vessels along the inferior border of the uncinate process were carefully dissected and coagulated from left to right till the preset proximal margin around ampulla. After clamping the preset margin, routine IOC was performed to make sure the ampulla was intact as described previously. After that, the proximal margin was transected by linear stapler (Figure 4B), and a side-to-side duodenojejunostomy was done in a retro-colic manner.
Preserving the function of the major duodenal papilla is critical and is the ultimate goal for both supra- and infra-ampulla L-PSD. So cholecystectomy is needed for all L-PSD to perform IOC, and ensure the preservation of the papilla.
Adjuvant Imatinib and Follow-Up
For patients classified as moderate-risk and high-risk grade according to NIH criteria, adjuvant Imatinib with 400mg per day was indicated and recommended for 3 year and 5 years, respectively. Regular follow-up for every 3 months was obtained by medical records and telephone. Computed tomography and endoscopy were carried out every 6 months and 12 months, respectively. Recurrence was evaluated by multi-disciplinary team (MDT) discussion.
Statistical Analysis
Continuous data were expressed as means ± standard deviations, and the categorized data were summarized as frequencies and percentages. The student t-test and Fisher exact χ2 test were used to compare the differences between the PD group and the PSD group. PFS and OS curves were determined using the Kaplan-Meier method and survival differences were compared by the Log rank test. P value<0.05 was considered statistically significant. All of the data were analyzed by R 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Demographic and Clinico-Pathological Characteristics
Twenty-two patients diagnosed with duodenal GIST underwent laparoscopic surgery and were enrolled, including 13 L-PDs and 9 L-PSDs. All patients’ demographic characteristics are listed in Table 1.
 |
Table 1 Demographic and Clinico-Pathological Characteristics for 22 Duodenal GISTs |
The average age was 58.2±9.5 year-old (Median 60.5 year-old). The most common presentations were GI bleeding (54.5%) and abdominal discomfort (27.2%), and the dominant lesion was located in the second portion of duodenum (59.1%). Most of the tumors (72.7%) were smaller than 5cm. According to the grading system by NIH, pathology confirmed 4(18.2%) as very low risk, 10 (45.5%) as low risk, 0(0%) as moderate risk and 8(36.3%) as high risk, respectively. As to the mitotic count, <5/50HPF accounts for 91%. No lymph nodes metastasis was observed. 7(31.8%) of patients were classified as high-grade risk and received adjuvant Imatinib.
Operative Outcomes and Complications
Based on tumor size and proximity to the Vater’s papilla, L-PD (Table 2) and different types of L-PSD were performed (Table 3). Thirteen duodenal GISTs underwent LPDs. And L-PSD were all performed with duodenal GISTs located opposite the major papilla, including 4 supra-ampulla L-PSDs and 5 infra-ampulla L-PSDs (Tables 1 and 3).
 |
Table 2 Clinico-Pathological Detail and Follow-Up of All L-PDs |
 |
Table 3 Clinico-Pathological Detail and Follow-Up of All L-PSDs |
Compared with the L-PD group, the L-PSD group showed much shorter operation times (364.2±58.7min vs. 230.0±12.3min, P<0.001), less blood loss (176.9±85.7mL vs. 61.1±18.2min, P<0.001), faster recovery to off-bed (2.6±1.3d vs. 1.1±0.3d, P=0.003), anus flatus (4.5±1.0d vs. 2.4±0.5d, P<0.001) and liquid intake (4.9±1.3d vs. 2.3±0.5d, P<0.001). Lymph node retrieval was much less in L-PSD, but no lymph node metastasis was observed in any patients. Moreover, according to the Clavien-Dindo classification, L-PSD had a much lower morbidity of both minor (Grade I/II) and major (III/IV/V) complications than that of L-PD (11.1% vs. 61.6%, P=0.02), resulting in shorter length of hospital stay (10.9±3.8d vs. 20.6±11.1d, P=0.021) and less total cost (76,972.4±11,614.8yuan vs 125,628.7±46,356.8yuan, P=0.006). However, reoperation rate and mortality failed to reach significant difference. Of note, all the 3 reoperations occurred in L-PD group, 2 of which complicated with pancreaticojejunostomy leakage presented as bleeding in postoperative day (POD) 7 and abdominal infection in POD5, respectively, and underwent reoperation with external drainage of the end loop together with main pancreatic duct; moreover, nutritional jejunostomy was suggested in the efferent loop. Finally, these 2 patients discharged in POD20 and POD23 without other morbidity. However, the rest one suffered bleeding due to pancreatic leakage in POD6 with reoperation; however, multi-organ dysfunction developed and resulted in death in POD15. Regarding late complication, L-PD had one stricture of hepaticojejunostomy 6 months after surgery (Table 4).
 |
Table 4 Peri-Operative Outcomes and Postoperative Complications |
Follow-Up and Oncological Outcomes
Regular follow-up was carried out and the median follow-up was 42 months (Ranging from 12 to 82months) without loss. Except for the perioperative mortality, the rest 7 patients with high-grade risk stratification, adjuvant Imatinib was recommended that lasted 60 months. During the follow-up, only 1 L-PD patient suffered hepatic metastasis 36 months after surgery, and sunitinib was given to maintain stabilize the disease, none of the rest observed recurrence or metastasis. No significant differences of overall survival (OS) and disease-free survival (DFS) were observed between the L-PD and the L-PSD group (Figure 5). Except for one mortality because of a major complication, the other 21 patients survived.
 |
Figure 5 Overall survival (A) and disease-free survival (B) of patients underwent L-PD and L-PSD. |
Discussion
Since duodenal GISTs are rare, the optimal surgical managements and oncological outcomes remain unclear. Generally, pancreaticoduodenectomy (PD) is indicated for duodenal GISTs for its uncertain malignancy and proximity to bilio-pancreatic ampulla. Moreover, it is technically difficult in a duodenectomy to dissect the duodenum from the pancreatic head because of their intimate relation both in anatomy and function. However, as the surgical skills and energy equipment developed, difficulties turned to feasibility3,9,11 and the higher complication rate after PD outweighs its benefits.2 Studies seldom compared the postoperative complications of PSD with PD directly or oncological outcomes for duodenal GISTs, especially for minimal invasive management.
In this study, duodenal GISTs that underwent L-PD suffered alarming morbidity and mortality, 61.6% of patients had postoperative complications and half of them (30.8%) experienced major complications (Clavien-Dindo Grade III–V), much higher than that of routine L-PDs. Only 32.2% of patients in our previously 320 consecutive L-PDs developed morbidity with 10.9% developing major complications.16 To compare from national and international perspectives, Wang et al reported L-PD with 49.66% morbidity out of 1029 multi-center patients in China and 21.2% major complications,17 Adam from the US concluded that the complication rate was 47% out of 865 minimally invasive PD patients.18 Unlike with other periampullary lesions, duodenal GISTs seldom obstruct the bile ducts and pancreatic ducts, the un-dilated ducts and soft texture of pancreas exert great difficulty for reconstruction and resulted in an alarmingly higher morbidity than that of routine L-PDs, in this study 46% of patients ended up with POPF, including 23.1% Grade C POPF needing reoperation. It was also true with bile leakage at 15.4%, much higher than that of our previous study with 17.5% POPF and 3.8% bile leakage.16 Stricken by this, L-PSD was explored in selected patients when technically possible, avoiding troublesome biliary-enteric and pancreatic-enteric anastomoses.
Varied nomination of different types of duodenectomy were adopted and reported based on tumor location and vicinity to the ampulla, including limited or wedge resection,2,4-7,10,20 segmental duodenectomy,9,10 partial sleeve duodenectomy3,9 and pancreas-sparing duodenectomy.11,19 As all the procedures above aim to resect the duodenal lesions while preserving the pancreas and ampulla, pancreas-sparing duodenectomy (PSD) was believed to be more generalized and PSD was adopted. L-PSD was only indicated for supra-ampulla and infra ampulla duodenal GISTs < 5cm, and lesions located opposite the major papilla. For both supra and infra L-PSD, guaranteed negative margin without rupture from the Vater’s papilla is determinant to resectability. So, it is of great importance to locate the papilla and keep it intact. We adopted preoperatively endoscopic marking and intraoperative cannulation of the catheter along the common bile duct with cholangiogram to ensure the ampulla. The catheter was placed to penetrate through the papilla and removed after the duodenojejunostomy. However, questions about PSD in curative surgery still exist. Lee et al reported that 84% PSD group reached R0 resection and the remaining 16% required conversion to PD.21 While in this study, all the 9 patients intended to perform L-PSD were all succeeded without conversion to L-PD, and no ampulla injuries occurred. Only one patient complicated delayed gastric emptying (DGE), no stricture or fistula was observed. Similarly, Stauffer performed 10 PSDs and only experienced complication with 1 DGE because of pancreatic fistula,3 Chung reported 21 cases with only 2 pancreatic fistula and 1 wound infection.7 These show the technical feasibility and safety of L-PSD in selected hands.
L-PSD seemed to provide more attractive alternatives over L-PD for duodenal GISTs. However, to date, most studies focused on the feasibility while specific data on comparison between L-PSD and L-PD are still limited. Data on this issue are lacking, especially when taken laparoscopic management into consideration. Shen et al conducted a systematic review and concluded open PD group had significantly higher morbidities than that of the PSD group (40.8% vs. 19.2%, OR 2.90).2 Lee et al also indicated that the PD group had significantly greater intraoperative blood loss, longer operative time, longer hospital stay, and higher 90-day morbidity and readmission rates than that of the PSD group. This is also true in the set of laparoscopic surgery. In our study, the L-PSD group also confirmed much shorter operation time, less blood loss, faster recovery to off-bed, anus flatus and liquid intake. Moreover, L-PSD had much lower morbidity of both minor and major complications than that of L-PD, resulting in shorter length of hospital stay and less total cost. Obviating biliary-enteric and pancreatic-enteric anastomoses also free the L-PSD group out of long-term complications such as hepaticojejunostomy stricture and recurrent refluxing cholangitis, which affects the quality of life greatly. However, L-PD is irreplaceable for GISTs adjacent to the ampulla or large lesions that have a higher risk of rupture. Besides, L-PSD showed more acceptable clinical outcomes than L-PD for selected patients.
Another concerned question is whether L-PSD is an oncological adequate alternative to L-PD. Studies have shown that PD treatment was associated with worse long-term prognoses than PSD (HR = 1.93, 95% CI, 1.39–2.69; P < 0.001).2 Moreover, Lee et al indicated that patients with descending GISTs who underwent PD had poorer DFS than PSD patients. However, in multivariate analysis, the PD group was revealed to have larger tumor sizes and the surgical procedure was proven to be irrelevant to the prognosis.21 Similarly, our study showed that long-term DFS and OS had no significant difference between L-PSD and L-PD group, but this study failed to perform subgroup analysis for the limited sample size. Moreover, no lymph node metastasis was observed, and extra lymphadenectomy seemed unnecessary. L-PSD with negative margin had equivalent oncological outcomes when compared with L-PD.
However, the present study has several limitations. Firstly, the retrospective nature and small sample size may influence the validity of the analysis, but the incidence of duodenal GISTs is far low and the cases in a single center are limited. A multicenter study with prospective protocol is awaited to conclude more convincing results. Learning curve exists in both L-PD and L-PSD, and this may influence the outcomes. Moreover, the indication of adjuvant Imatinib and optimal duration has not been established, as Imatinib is very effective in most GISTs, it is difficult to evaluate the efficacy of the procedure without bias. Further analysis of prognostic factors including molecular characteristics is also important, which requires large-scale data.
Conclusion
L-PSD showed comparable safety and oncological benefits as L-PD, while having a much shorter operation time, less blood loss and much faster recovery. These resulted in much less total cost. For GIST located opposite to the major papilla, L-PSD should be applied in selected patients with experienced hands.
Acknowledgments
This study was supported by the Zhejiang Provincial Key Project of Research Foundations (Grant No.2015C03049) and the Natural Science Foundation of Zhejiang Province (Grant No. LGF20H1600011).
Disclosure
The authors have no conflicts of interest or financial ties to disclose.
References
1. Corless CL, Barnett CM, Heinrich MC. Gastrointestinal stromal tumours: origin and molecular oncology. Nat Rev Cancer. 2011;11:71. doi:10.1038/nrc3143
2. Shen Z, Chen P, Du N, et al. Pancreaticoduodenectomy versus limited resection for duodenal gastrointestinal stromal tumors: a systematic review and meta-analysis. BMC Surg. 2019;19(1):121. doi:10.1186/s12893-019-0587-4
3. Stauffer JA, Raimondo M, Woodward TA, et al. Laparoscopic Partial Sleeve Duodenectomy (PSD) for nonampullary duodenal neoplasms avoiding a whipple by separating the duodenum from the pancreatic head. Pancreas. 2013;42(3):461–466. doi:10.1097/MPA.0b013e3182649956
4. Hoeppner J, Kulemann B, Marjanovic G, et al. Limited resection for duodenal gastrointestinal stromal tumors: surgical management and clinical outcome. World J Gastrointest Surg. 2013;5:16–21. doi:10.4240/wjgs.v5.i2.16
5. Lee SJ, Song KB, Lee YJ, et al. Clinicopathologic characteristics and optimal surgical treatment of duodenal gastrointestinal stromal tumor. J Gastrointest Surg. 2019;23:270–279. doi:10.1007/s11605-018-3928-1
6. Goh BK, Chow PK, Kesavan S, et al. Outcome after surgical treatment of suspected gastrointestinal stromal tumors involving the duodenum: is limited resection appropriate? J Surg Oncol. 2008;97:388–391. doi:10.1002/jso.20954
7. Chung JC, Kim HC, Hur SM. Limited resections for duodenal gastrointestinal stromal tumors and their oncologic outcomes. Surg Today. 2016;46:110–116. doi:10.1007/s00595-015-1163-x
8. Liao GQ, Chen T, Qi XL, et al. Laparoscopic management of gastric gastrointestinal stromal tumors: a retrospective 10-year single-center experience. World J Gastroenterol. 2017;23:3522–3529. doi:10.3748/wjg.v23.i19.3522
9. Choi SH, Park J, Kang CM, et al. Laparoscopic partial sleeve duodenectomy for the infra-ampullary gastrointestinal stromal tumors of the duodenum. World J Surg. 2018;42(12):4005–4013. doi:10.1007/s00268-018-4707-6
10. Chung JC, Chu CW, Cho GS, et al. Management and outcome of gastrointestinal stromal tumors of the duodenum. J Gastrointest Surg. 2010;14:880–883. doi:10.1007/s11605-010-1170-6
11. Corcione F, Pirozzi F, Sciuto A, et al. Laparoscopic pancreas-preserving subtotal duodenectomy for gastrointestinal stromal tumor. Minim Invasive Ther Allied Technol. 2013;22:187–190. doi:10.3109/13645706.2012.698988
12. Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008;39:1411–1419. doi:10.1016/j.humpath.2008.06.025
13. Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161:584–591. doi:10.1016/j.surg.2016.11.014
14. Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. doi:10.1016/j.surg.2005.05.001
15. Clavien PA, Barkun J, de Oliveira ML, et al. The clavien-dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. doi:10.1097/SLA.0b013e3181b13ca2
16. Lu C, Jin WW, Mou YP, et al. Experience on postoperative complications of laparoscopic pancreaticoduodenectomy. Zhonghua Wai Ke Za Zhi. 2018;56(11):822.
17. Wang M, Peng B, Liu JH, et al. Practice patterns and perioperative outcomes of laparoscopic pancreaticoduodenectomy in China: a retrospective multicenter analysis of 1029 patients. Ann Surg. 2019;undefined:undefined.
18. Adam MA, Thomas S, Youngwirth L, et al. Defining a hospital volume threshold for minimally invasive pancreaticoduodenectomy in the United States. JAMA Surg. 2017;152:336–342. doi:10.1001/jamasurg.2016.4753
19. Maher MM, Yeo CJ, Lillemoe KD, et al. Pancreas-sparing duodenectomy for infra-ampullary duodenal pathology. Am J Surg. 1996;171(1):62–67. doi:10.1016/S0002-9610(99)80075-0
20. Liu Z, Zheng G, Liu J, et al. Clinicopathological features, surgical strategy and prognosis of duodenal gastrointestinal stromal tumors: a series of 300 patients. BMC Cancer. 2018;18(1):563. doi:10.1186/s12885-018-4485-4
21. Lee SY, Goh BK, Sadot E, et al. Surgical strategy and outcomes in duodenal gastrointestinal stromal tumor. Ann Surg Oncol. 2017;24:202–210. doi:10.1245/s10434-016-5565-9
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.