Back to Journals » Advances in Medical Education and Practice » Volume 14
Opportunities and Challenges for Implementation of Harmonized Competence-Based Curricula in Medicine and Nursing Programmes in Tanzania: Experiences of Biomedical Sciences’ Stakeholders
Authors Sirili N , Mloka D , Mselle L, Kisenge R, Mbugi E , Russa D , Nyongole O, Mshana SE , Laisser R, Mteta K, Msuya L, Lyamuya E , Martin-Holland J, Kwesigabo G, Kaaya E
Received 6 August 2022
Accepted for publication 20 April 2023
Published 22 May 2023 Volume 2023:14 Pages 487—498
DOI https://doi.org/10.2147/AMEP.S381242
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Md Anwarul Azim Majumder
Nathanael Sirili,1 Doreen Mloka,2 Lilian Mselle,3 Rodrick Kisenge,4 Erasto Mbugi,5 Dennis Russa,6 Obadia Nyongole,7 Stephen E Mshana,8 Rose Laisser,9 Kien Mteta,10 Levina Msuya,11 Eligius Lyamuya,12 Judith Martin-Holland,13 Gideon Kwesigabo,14 Ephata Kaaya15
1Department of Development Studies, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 2Department of Pharmaceutical Microbiology, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 3Department of Clinical Nursing, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 4Department of Pediatrics, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 5Department of Biochemistry, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 6Department of Anatomy, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 7Department of Surgery, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 8Department of Microbiology and Immunology, Catholic University of Health and Allied Sciences, Mwanza, Tanzania; 9Archbishop Anthony Mayalla School of Nursing, Catholic University of Health and Allied Sciences, Mwanza, Tanzania; 10Department of Surgery, Kilimanjaro Christian Medical University College, Moshi, Tanzania; 11Department of Paediatrics and Child Health, Kilimanjaro Christian Medical University College, Moshi, Tanzania; 12Department of Microbiology, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania; 13Department of Physiological Nursing, University of San Francisco California, San Francisco, CA, USA; 14Department of Epidemiology and Biostatistics, Muhimbili University of Health and Allied Sciences, Dar Es Salaam, Tanzania; 15Department of Pathology, Kilimanjaro Christian Medical University College, Moshi, Tanzania
Correspondence: Nathanael Sirili, Email [email protected]
Background: In 2012, the Muhimbili University of Health and Allied Sciences (MUHAS) embarked on structured competency-based curricula (CBC) for its programmes. Other health profession training institutions continued with their traditional way of teaching and thus causing variability in the competencies of the graduates. We aimed to analyze the experiences of different stakeholders on the implementation of CBC specifically on biomedical sciences by MUHAS to inform the development of harmonized competency-based curricula in three health professional training institutions in Tanzania.
Methods: We adopted an exploratory case study to analyse the implementation of CBC in programmes of Medicine and Nursing involving MUHAS graduates, immediate supervisors at the employment sites, faculty, and continuing students at MUHAS. Kiswahili guides were used to conduct the in-depth interviews (IDIs) and focus group discussions (FGDs). Qualitative content analysis was adopted for analysis.
Results: From the 38 IDIs and 15 FGDs, four categories of human resources teaching and learning environment; curriculum content; and support systems emerged. Human resources were attributed to the shortage of an adequate number of faculty and teaching skills variation. The curriculum content category was linked to the redundancy of courses or topics, poor sequencing of some topics or courses, and limited time for teaching some essential courses or topics. Training and practice area mismatch, accommodation to students, teaching space, and library were the sub-categories linked to teaching and learning environment. Lastly, support systems related to teaching methods and opportunities for improving teaching and learning were revealed.
Conclusion: The findings of this study highlight the challenges and opportunities for the implementation of CBC. The solutions to the revealed challenges are beyond the training institutions’ capacity. The latter call for multi-stakeholder engagement including those from the public and private sectors in health, higher education and finance for common and sustainable solutions.
Keywords: competency-based curricula, biomedical sciences, teaching pedagogy, health training institutions, harmonized training, Tanzania
Plain Language Summary
Changes in technology and diseases profile necessitate changes in how health workers are trained. Medical doctors and nurses are among the key people in the frontline health workforce teams who must at all times be vested with the necessary competencies and skills. Tanzania for many years had only one medical school that produced most of the little available health workforce in the country, the Muhimbili University of Health and Allied Sciences (MUHAS). Although pivotal to training, the curricula lacked a structured set of minimum competencies. Worse enough, when other training institutions emerged, each one used its own curriculum to train respective cadres. About ten years ago, MUHAS embarked on developing the minimum set of structured competencies to its curricula. However, about ten years later other institutions have continued to move with less structured curricula. This paper focused on learning from the MUHAS on implementing structured competencies to develop harmonized curricula for medicine and nursing programmes in Tanzania.
We interviewed trainers, trainees and employers to get their insights on the graduates from MUHAS. We found opportunities and challenges linked to human resources, curriculum content, teaching and learning environment, and support systems influenced the implementation of the CBC at MUHAS.
Introduction
Health professions training operates in a dynamic environment that reflects the policy changes at the country, regional and global levels. The changes in health policies often are driven by changes in; the labor market, burden, pattern and impact of diseases, political and economic orientation, community needs, and technological advances.1–4 Altogether, these changes compel the health training institutions to regularly review their curricula to produce graduates who can cope with these dynamics.5–8 Policy and decision-makers view universities not only as sources of human capital production but also as sources of evidence to inform innovation for sustainable development and competitiveness in a globalizing world.9–11 Therefore, graduates from higher learning institutions must be prepared to have competencies to fulfil these expectations.7 Although Competence-Based Education (CBE) dates back to 19th century, the concept has gained popularity in the 20th century as a tool to provide the aforementioned competencies.12 Often lack of teaching and learning materials, laboratory equipment and chemical reagents challenges the implementation of CBE.13 For the health Professions (i) Lack of structural models for CBME that accommodate individual, flexible learning plans (ii) Increased administrative requirements for CBME programmes and need for increased faculty development and (iii) Inconsistencies in how competencies are defined, developed, implemented and assessed are highlighted to challenge implementation of CBE.14
The training of health professions is organized into two main facets; the Basic sciences (popularly the Biomedical sciences) and clinical training. The Biomedical Sciences equip the students with the science behind health, ill-health and its management. The Clinical training prepares the graduates with the hands-on skills to mill health. However, in Tanzania, similar to many other places, the training for health professions although competency-based was not systematically structured to align learning outcomes, instructional methods and assessment methods. Employers and other consumers of these products have often complained that they have limited hands-on skills and soft skills such as communication skills and professionalism.15,16 This implies that all training curricula need to be designed so that students master a specific list of clearly defined competencies at graduation to be competitive in local and international labour markets. This requirement has resulted in an educational paradigm shift requiring curricula to impart lifelong learning skills and develop transferable competencies that can be traded as a commodity. Lack of inter-professionalism, teamwork, and smooth communication among health cadres has been blamed for hitching the delivery of healthcare services, and in some places, open rivalry exists.17,18
To address the competency gap raised by its graduates’ consumers, the Muhimbili University of Health and Allied Sciences (MUHAS) conducted a university-wide tracer study in 2009. From the tracer study, MUHAS realised that the deficiencies in competencies of its graduates were grounded in the training curricula, in the sense that they were not systematically designed to address competencies, and the implementation was not monitored and evaluated efficiently. Therefore, from the latter, MUHAS embarked on developing and implementing structured competency-based curricula (CBC) in all its academic study programmes in 2012.15,16,19 CBC emphasizes the outcomes of the learning process in ensuring that students acquire both specific professional competencies and general competencies that are key in mastering the operational environment.
Implementation of CBC requires the transformation of trainers, learners, and the learning environment to accommodate the otherwise new training and learning approaches.12,20,21 The main characteristics of the competency-based approach have been identified and include, among others, efficient use of skills that allows productive performance in the professional activity.22,23 The MUHAS CBC were geared to encourage multidisciplinary teaching to promote inter-professionalism in healthcare. Inter-professional teaching and learning optimize physical and human resource utilization through pooling and central administration.24
Close to a decade later, after MUHAS had started implementing the competency-based curricula, some challenges remain. Although not explicitly linked to CBC implementation, the quality of graduates from MUHAS and the university ranking both locally and internationally has placed MUHAS above all higher learning training institutions in Tanzania as of 2022.25,26 The latter hints that the CBC has produced better results compared to the originally less structured curricula. Furthermore, while it is prudent to continue improving the quality of training at MUHAS, the increase in the number of health training institutions with each one using its own curricula pose another major threat to the health training in Tanzania. Moreover, the latter makes it difficult for students’ mobility and resource sharing across the training institutions amidst the critical shortage of faculty.27 In view of the latter, three local health training institutions, Catholic University of Health and Allied Sciences (CUHAS), Kilimanjaro Christian Medical University College (KCMUCo) and MUHAS in collaboration with two universities from the United States of America (Duke and University of California San-Francisco) established a consortium (The Transforming Health Professions Education in Tanzania, THET consortium) in efforts to address these challenges. To inform the process of addressing the challenges, the THET consortium embarked to conduct tracer study following the implementation of the CBC by MUHAS. One of the major aims of the THET consortium was to develop a harmonized CBC for the programmes of Bachelor of Science in Nursing (BScN) and Doctor of Medicine degree (MD).
We aimed to analyze the experiences of different stakeholders on the implementation of CBC specifically on biomedical sciences by MUHAS and thus inform the development of harmonized competency-based curricula in three local THET institutions in Tanzania. We focused our analysis in this paper to Biomedical Sciences owing its role in understanding the scientific basis of health and its implication in clinical practices.
Materials and Methods
Study Design
We adopted an exploratory case study to analyse the implementation of CBC. According to Robert Yin,28 a case study is appropriate when studying a complex phenomenon that involves social processes. CBC implementation is a complex phenomenon, and it involves multiple players from both the supply and demand sides in which their interactions are not linear. Our case study involved MUHAS graduates from two programmes of Medicine and Nursing, as the only health training university that implemented the structured CBC in that period, employers of the MUHAS graduates both in the private and public sector, immediate supervisors of MUHAS graduates at employment sites, registrars of the Medical and Nursing councils, faculty at MUHAS and continuing students at MUHAS.
Study Context
Training in Medicine and Nursing at the degree level in Tanzania is under the Ministry of Education, Science, and Technology (MoEST). The Tanzania Commission for Universities (TCU) regulates training in all higher learning institutions, including Medicine and Nursing programs. Professional councils in Tanzania vet and approve the programmes training curricula before being accredited by the TCU. From the latter curriculum for training of Medicine degree receive vetting and approval from the Medical Council of Tanganyika while that of nursing receive vetting and approval from the Tanzania Nursing and Midwifery Council. Both programmes start with the training in biomedical sciences before clinical training. By 2016 there were over 10 health training institutions that had produced at least one batch of graduates either in medicine or nursing. This study was conducted to assess the implementation of CBC at MUHAS owing to its palpable experience and noted successes of CBC implementation. The latter aimed at informing development of a harmonized training curricula in medicine and nursing to start with in the three THET consortium institutions. MUHAS is located in Dar es Salaam, Tanzania, which is the country’s main economic hub, and a cosmopolitan metropolis. The university offers undergraduate programmes, postgraduate programmes, and continuing professional development in the form of short courses.29 MUHAS programmes are accessible to local and international applicants. The graduates from MUHAS therefore are expected to work across the country and abroad.
Training of Medicine at MUHAS dates back to 1968, and that of nursing in 1989.30 However, it was not until 2012 that MUHAS embarked on structured competency-based curricula for all its training programmes. The transformation followed a tracer study that was carried out in 2009. The graduates from these programmes are employed in public and private sectors in training, research, and health care delivery. This study was conducted in five regions of Tanzania mainland, namely: Kigoma, Dodoma, Kilimanjaro, Mwanza, and Dar es Salaam. These regions were purposefully selected to include five out of the seven geopolitical zones in Tanzania mainland. The zones were first stratified into three groups based on the density of health workers.31 The first group included zones with a high density of health workers. These included the Eastern zone, Southern Highland, and Northern zone. From this group, Dar es Salaam and Kilimanjaro were included. The second group had the Central, Lake, and Southern Highland zones. This group also included Dodoma and Mwanza. The last group was the west zone, where Kigoma was included.
Data Collection
From the selected regions, we purposefully selected informants for the in-depth interviews and focus group discussion based on their roles or interaction with MUHAS graduates or interaction with the MUHAS training curricula. We conducted In-Depth Interviews (IDIs) with employers (at district, regional, and institution level) and immediate supervisors (at clinical settings), and MUHAS recent past graduates. The IDIs were conducted with rich-information cases who were either directly supervising the MUHAS graduates or who were in frequent contact with the graduates on their day-to-day activities. Furthermore, in places where there were few graduates as they are not evenly distributed in the country, IDI was also used instead of FGD. We also conducted Focused Group Discussions (FGDs) with MUHAS faculty, continuing students, and MUHAS graduates across disciplines who completed their training between 2017 and 2018. We conducted with 38 IDIs and 15 FGDs with 113 participants. Each FGD contained between 6 and 9 participants (Table 1).
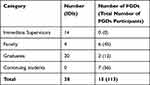 |
Table 1 Study Participants |
We developed three semi-structured interview guides and three semi-structured focused group discussion guides for the different groups of study participants based on the competency domains stipulated in the training curricula. We enriched the guides through a consultative workshop that included faculty, students, and invited faculty and supervisors of MUHAS graduates from three selected hospitals and two health training institutions offering the two programmes involved in this study. We first developed the guides in the English language, and after agreeing on the final version, we translated them into the Kiswahili language, which is the most widely spoken language for most of the targeted study participants.
We used the Kiswahili guides to conduct the IDIs and FGDs across the selected categories of participants. Although the guides had some slight variations on the questions, they all gave the opportunity for probing after the primary response from the participants. The IDI and FGD guides were structured to tap participants’ opinions on strengths, weaknesses, opportunities, and challenges facing the implementation of the competency-based curricula. The team of data collectors were comprised of a mix of medical doctors, nurses, pharmacists, dentistry, public health practitioners and social scientists who have varying experience in conducting qualitative research and have been involved at different times in training of doctor of medicine and nursing programmes. The team were further comprised of senior, mid-level and junior faculty to minimize social desirability during the interviewing. All the data collectors were faculty from the three THET consortium institutions and were fluent in both Kiswahili and English. Before commencing data collection, a two-day workshop was held to get a clear and common understanding of the tools and objectives of the study.
Data Analysis
The qualitative content analysis following Granheim and Lundman32 guided the analysis of data. Audio-recorded interviews were first transcribed verbatim. All authors first read the Kiswahili full transcripts and field notes to become familiar with the data and context. The data was then reduced to condensed meaning units related to the implementation of CBC in the two programmes under study. To enhance intercoder reliability, the first two transcripts were coded independently by three pairs of researchers and then discussed to agree on codes to use. Coding from the three pairs was almost similar, and thus each pair continued to code independent transcripts. All authors then discussed the initial list of codes, and the agreement on the final list of codes was reached. Similar codes were grouped and abstracted into sub-categories through comparison. Through checking on the similarities and differences of sub-categories and reflection on the interpretations of the participants` experience descriptions, the authors discussed and agreed on the categories to reflect the manifest content. With the support of succinct quotes, the results were presented in categories and sub-categories. Although the process is described linearly, the whole analysis exercise was iterative. After agreeing to all categories, sub-categories, and quotes in pairs, we translated them from Kiswahili to English.
Ethical Issues
This study was part of the capacity-building project (Health Education Partnership Initiative- To Reach People: Transforming Health Professions Education in Tanzania, HEPI-THET) that had three aims of; (i) Create and adopt common training curricula for medicine and nursing education in Tanzania to ensure that the graduates from these programs from the different institutions have good quality and have common competencies (ii) Enhance the academic environment to attract and retain the best early-career faculty by mentoring them to use innovative competency-based skills development and collaborate to build their research portfolios and (iii) Improve communication to reach out main stakeholders including tracking of graduates and thus establish and sustain a robust database for the graduates in health sector in Tanzania.
The whole project was waived by the Muhimbili University of Health and Allied Sciences Institutional Review Board which was the prime institution in this project (Ref. No. DA/282/298/01.C/). In the data collection process permissions were obtained from all relevant institutions to include Ministry of Health, President’s Office Regional Administration Authorities and data collection sites. All participants provided written informed consent before commencement of interview or discussion. The informed consent included consenting for publication, confidentiality, rights to participate, rights to withdraw, procedures for participating and anonymity.
Results
From the KIIs, IDIs, and FGDs, four categories emerged. These are, human resources teaching and learning environment, curriculum content and support systems (Figure 1).
 |
Figure 1 Summary of findings. |
Human Resources
In this category, both absolute and relative shortage were stated. Absolute shortage was described as a faculty shortage, while relative shortage was explained as variation in teaching skills among faculty.
Shortage of Faculty
Most of the faculty interviewed in this study informed that while there is an upsurge in the number of students admitted annually and thus increasing the workload, the number of faculty has remained relatively small. They expressed that in the biomedical sciences courses, most of the departments had less than five faculty while they were responsible for teaching big classes of sometimes more than six hundred students in a single sitting.
…We have a critical shortage of faculty…we rescue the situation by using our postgraduate students to train the undergraduate students…In my department, for instance, we are only three faculty.… (Faculty -IDI-1-MD)
Some participants added that most faculty members were trained as health personnel and did not receive teaching pedagogy when employed as faculty. They struggled to learn by looking at what their seniors or role models did.
…Most trainers have undergone only two training; their first degree and postgraduate degree. This makes most of us be devoid of the teaching and assessment skills and use experiences from how we were trained during our time… (Immediate supervisor-IDI- 2-MD)
Variation of Teaching Skills Among Faculty
The majority of the graduates and ongoing students said there was a wide variation in delivering content among faculty. They stated that some faculty entered into a session with too much content to be delivered within a short time and thus ended up with a long non-interactive lecture. On the other hand, some faculty were reported to be very good at delivering complex matters in a simple form that made the students understand the issues easily. Furthermore, students and interns complained about the impact of the variation in teaching skills. They stated that the impacts were much felt during the assessments. While some faculty were considered fair assessors, some were judged rude.
…You are in an oral exam, the examiner starts wondering, you can’t even answer this simple question, what do you know then? No, no you have failed…s/he talk to the panellist…this will be a dangerous Doctor if we let him/her go….so you fail in that way… (Graduate-FGD member no. 6 -MD)
Curriculum Content
Curriculum content was attributed to redundancy of courses or topics, poor sequencing of some topics or courses, and limited time for teaching some essential courses or topics.
Redundancy and Poor Sequencing of Some Topics or Courses
Graduates and continuing students from both medicine and nursing schools expressed their concerns about the redundancy of topics and some courses in their programmes. Both groups mentioned that some courses had been given much time compared to other courses they considered core. They also stated that some topics were repeated in similar ways and without alteration. They cited a good example of leadership topics taught three times in the same way and content. They further added that, while little to no value was gained from the extended time and repetition, it reduced time for covering other topics or courses.
…For instance, a subject like Information Technology is covered in three semesters while key subjects like Pharmacology are covered in one semester…I think the time used for the IT was too much, and I feel that some of this time would have been added to courses like pharmacology which is key in nursing practice… (Graduate-FGD member no.8-BScN)
Regarding the topics’ sequencing, some participants pointed out poor sequencing of some topics and modules, thus making the learning difficulties due to a disorganised flow of information. Giving an example of the nursing program, some graduates pointed out that leadership and management were placed far close to the end of the program while its application starts immediately when the students go for clinical rotations.
Sequencing of the courses in the nursing programme in many training institutions in the first and second year covers biomedical sciences training, and in the third year is focused more on clinical courses. In the last year, they have received training in management and leadership…. I think this sequence makes them exit as managers of the organization rather than a clinician and thus pose a major challenge to their nursing practice. (Immediate Supervisor-IDI 5 - BScN)
Limited Teaching for Some Essential Courses
As stated by some participants, limited teaching of some essential courses manifested as the absence of some courses to little emphasis on some other courses. For instance, participants complained of limited training on basic issues such as key diagnostic procedures (eg, X-rays and ultrasound) for the doctor of medicine program. They further stated that their training was devoid of the basics of oral health, and thus they were facing challenges to manage simple oral conditions.
…As a medical doctor, I have to take care of the whole patient…sadly, our training did not cover oral health…what I remember is that from the first to fifth year, I did not cover even the tooth anatomy…I think this is a weakness…. (Graduate-FGD member no.5 -MD)
In Nursing programmes, for instance, the majority of the participants stated that some key areas were not taught, thus limiting graduates from acquiring such skills. They gave examples of the lack of teaching on mental health issues in the BSc Midwifery program while stating the known chances of puerperal psychosis.
…for us midwives, we did not cover psychiatry during our training, but now I am an intern here, and I am required to rotate in the psychiatry department…I know nothing, thus, I am starting from scratch…I think this was a serious omission in our training and should be included in the revision of the curriculum…. (Graduate-FGD member no.10-BScN and Midwifery)
Teaching and Learning Environment
This study’s teaching and learning environment was revealed by four sub-categories related to training and practice area mismatch, accommodation to students, teaching space, and library.
Training and Practice Mismatch
Participants complained that some facilitators used experiences from high-tech facilities in teaching biomedical sciences. They said that the latter affected the graduates once posted to their areas of practice where the facilities did not match the level of technology they were trained on. They further added that the graduates should know the basic procedures before moving to complex procedures. Thus, adequate exposure to the relevant basics of diagnostics to inform the clinical practice environment at the district level is important.
”… we are being taught by some facilitators who think that in every facility we will find a CT SCAN or MRI…again here at Muhimbili, only major surgeries are performed. The latter does not help us when we go to practice at the district level as the exposure to district rotation during the training is very short….it would be ideal if the clinical rotation at the district hospitals is given adequate time so that we learn adequately the basic surgical procedures like herniorrhaphy, Hydrocelectomy, Caesarean section etc… (Graduate-FGD member no.3-MD)
Limited Teaching Space
Graduates, faculty, and ongoing students said there was a crisis of teaching space at MUHAS. They stated that teaching space manifested as a shortage of space for seminar rooms, lecture halls, and laboratories for practical skills. They further added that the crisis of space was also experienced as the relative size of the lecture halls, seminar halls, or laboratories in relation to the number of students.
The latter was explained to affect students’ learning as sometimes the lectures are delivered in an overcrowded class and limit interactions with the facilitator.
…This hospital is fit for the purpose; however, it is overwhelmed, and thus equipment, supplies, and space are inadequate…the space includes the wards, seminar rooms, and side rooms in the wards…. for instance, in my department, we have small rooms, is like this room is divided into six or seven and sometimes you have sixty people in that room, it is not conducive at all… (Faculty -FGD member no.7-MD)
Underequipped Library
Graduates and ongoing students mentioned the library as underequipped. They stated that the library missed updated textbooks used for teaching and had a small computer library that could accommodate only a few students. The shortage of books manifested as a lack of hardcovers and e-books. They added that the lack of updated textbooks caused learning difficulties.
Participants further added that, even when they opted to use their computers, they faced another challenge of internet connectivity. In explaining this, participants stated that MUHAS, for an extended period, was experiencing intermittent internet connectivity.
…Even if you opt to use your computer to access electronic books, the connectivity at MUHAS is unreliable as there are few WiFi access points in the open spaces… even if you visit the computer lab, there is fluctuation of internet connectivity…We thank telecommunication companies for bringing internet packages special for university students which are affordable…. (Continuing student-FGD member 9-BScN)
Support Systems
Graduates, faculty, and ongoing students expressed their hope for improving teaching and learning. These were stated to use multiple teaching methods and foreseen opportunities for enhancing teaching and learning.
Use of Multiple Methods for Teaching
Participants stated the existence of various methods used for teaching at MUHAS. They mentioned some methods, such as lectures, seminars, presentations, group discussions, role-plays, case studies, and practical labs. For them, these multiple teaching methods enhanced their acquisition of knowledge and skills.
…group discussions, presentations in class, peer-to-peer presentations, seminars, practical, assignments, and lectures helped us acquire the knowledge we have…I think this modality of using multiple methods, although it is of high cost, is important in learning. (Graduate IDI-16-BScN)
Foreseen Opportunities for Enhancing Teaching and Learning
This study revealed possible opportunities for improving teaching and learning in our medical and nursing schools. The use of Moodle was mentioned as one of the opportunities that can be used to overcome the challenge of big classes. Participants also mentioned the use of simulation labs and skills labs to enhance practical skills and make grasping clinical skills easier.
…the growing use of Moodle, simulation labs, zooms, and other technologies are a good avenue for strengthening teaching and learning nowadays…during our time, these things were not there, it is had to cope with them, but we have to learn… (Faculty -IDI-3-BScN)
Discussion
We aimed to analyze the experiences of different stakeholders on the implementation of CBC specifically on biomedical sciences by MUHAS to inform the development of harmonized competency-based curricula in three health professional training institutions which were part of the THET consortium in Tanzania. The analysis has revealed varying experiences that reflect challenges and opportunities for implementing the CBC for Biomedical Sciences training. The challenges were highlighted as inadequate human resource, limited capacity for priority setting of the curriculum content, and a non-conducive teaching and learning environment. The existence of possibilities for improving teaching and learning was a significant opportunity revealed by this study. The challenges revealed by our study corroborate findings from other studies conducted in other settings.13,33,34
Adequate human resource, both in number and skills, is the input and also an output of CBC.4 The shortage in the number of faculty and support staff in health training institutions in Tanzania is not a new phenomenon but rather a chronic problem that got its roots from the structural adjustments programme and the employment suspension of the 1990s.35 Impact of the retrenchment policy left universities as for other institutions with shortage of faculty without a succession plan. Even after uplifting the retrenchment in early 2000s, absence of dedicated training institutions for biomedical sciences amidst the increased number of health training institutions has made the shortage to persist. From the mid to late 1990s, universities (other than the University of Dar es Salaam) for the training of health professionals emerged and contributed to an increase in Human Resources for Health (HRH) output. Although the increasing number of health professions training institutions resulted to increase in number of graduates in the country, their employment in public and private sectors has remained low and thus persistence of the HRH shortage.31,36,37 In the study mentioned above, lack of interest in joining postgraduate training in biomedical sciences was cited as one of the factors contributing to a shortage of faculty in the biomedical sciences disciplines. Given the importance of proper and effective implementation of CBC, it is felt that it is high time to prioritize faculty development and employment for biomedical sciences in the training institutions. Furthermore, we feel that devising appropriate incentives for biomedical sciences faculty is necessary for attracting faculty for biomedical sciences.
Human resources sufficiency also involves the adequacy of skills for implementing the CBC. As revealed by this study, variation of teaching skills among faculty poses another challenge to the efficient and effective implementation of CBC. Although not documented in the available literature, the faculty in health sciences universities in Tanzania receive no structured formal training in teaching pedagogy. As a result, most faculty use their own experience based on their undergraduate and postgraduate training exposure. This is similar to what was documented in another study where tutors of mid-level cadres echoed the same challenge.38 CBC implementation requires adequate preparation of both trainers and trainees. In a country where there is no established training institution for the preparation of faculty for teaching, higher learning institutions will continue to suffer from the disparity in faculty teaching competence which poses a threat to the quality of graduates produced.39,40 In many other places, proper pedagogical preparation of university faculty is limited.41,42 To address this challenge in Tanzania, it is prudent to establish a mandatory formal teaching pedagogy for university faculty before one is allowed to engage in teaching students. To formalize this recommendation requires a broad stakeholders’ engagement and inclusiveness of all key partners in health and higher education.
Unfavourable teaching and learning environment has been reported from several other places to challenge the implementation of CBC.13,33,43 While CBC implementation requires using new technologies to enhance learning access, our study has revealed that the library is underequipped. Also, the internet connectivity, which is crucial for accessing learning materials, has intermittent connectivity. Intermittent connectivity challenges delivery of online lectures, tutorials and even access to virtual classes to learners and facilitators. In the era of increased enrolment and limited growth of training infrastructure, a stable internet connection is a necessary precursor for effective CBC implementation as it requires the use of new learning and teaching technologies. While the training has transformed into CBC, the work environment has not changed significantly to reflect the requirements for its implementation. Most of the challenges experienced before the implementation of CBC have persisted.15,19 Authors feel that it is prudent to align the training of CBC to the requirements of its implementation. This requires that the CBC design considers the development of an implementation strategy that defines the necessities of its implementation.
Limited capacity for curricula content priority setting was reflected by redundancies in some courses and limited time for others. This suggests that during the curriculum development, some issues, such as competing interests among partners, may have been overlooked may be due to lack of priority setting skills.43 Therefore, in this article, we advocate for capacity building on priority setting for curriculum development among faculty.44 Implementation of harmonized training should go in hand with capacity building on curricula development and implementation of CBC. The curricula focal persons in the health training institutions can be empowered to act as a pool of trainers for curricula development to faculty.
The existence of opportunities for improving teaching and learning as reflected through innovative multiple teaching approaches amidst increased enrolment of students is a vital ingredient in implementing CBC.6,45 The use of various methods in learning and teaching as an innovative strategy in addressing the growing number of students is a positive sign that faculty are ready to adapt to new realities and complexities. The faculty readiness can and should be used as an essential starting point in capacity building for staff in implementing CBC. Furthermore, strengthening policies on innovative teaching approaches to include the use of e-technology cannot be understated.
Methodological Consideration
This analysis is limited to the qualitative aspect of the tracer study and thus does not provide the magnitude of the opportunities and challenges unveiled. Furthermore, the study findings are interpreted in the context of Biomedical Sciences. They, therefore, do not give the overall picture of the whole CBC implementation covering the entire length of the training programme. However, the triangulation of study participants, settings, researchers with different professions, and experiences give this study a strength to reflect CBC implementation for the biomedical sciences. This provides a comprehensive view of multiple stakeholders rather than covering the entire program superfluously.
Furthermore, the fact that the study was conducted by faculty who are involved in training the medical doctors and nursing programmes pose a potential of social desirability. However, the mix of the team of data collectors across the discipline and seniority offset the effect. Additionally, having data collectors from the two other institutions whose graduates were not part of the study minimized the potential bias of the MUHAS faculty to their graduates and programmes.
We assessed the trustworthiness32 of our study findings using the four Guba’s criteria: credibility, dependability, transferability, and confirmability.46 To enhance the credibility of the findings of this study, we triangulated the study participants, researchers, data collection methods, and study settings. For dependability, on top of the triangulation stated for credibility, we collected data at the natural settings of the study participants. We enhanced confirmability through the inductive generation of the categories of this study to reflect the perspectives of the study participants rather than the researchers’ interpretation. The categories were presented with the support of codes and succinct quotes. A detailed methodological description, including the study setting, context, data collection process, and analysis, were used to enhance the transferability of the study findings.
Conclusions and Recommendations
The findings of this study underscore the challenges and opportunities for the implementation of CBC in biomedical sciences. The challenges raised suggest the need of multi-stakeholder engagement in addressing them. The challenges raised require concerted efforts and resources to strengthen the implementation of CBC for Biomedical Sciences. The government should explore teaching alternatives that can make arrangements in health training institutions to use hospital staff to train clinical sessions and the universities put more efforts on biomedical sciences. The latter requires multi-stakeholders’ engagement and dialogue on university staff qualifications.
Furthermore, a large-scale study is needed to establish the health training institutions readiness to implement harmonized competency-based curricula. The assessment should include the readiness of faculty to use e-technology as often there is resistance to change among faculty especially older generation in using technology.
Acknowledgment
The authors wish to acknowledge the following THET consortium members for their immense contribution in making this manuscript better. Their inputs during presentation of the draft manuscript during the manuscripts writing workshop has helped in making this manuscript better as it is to this stage. Edith Tarimo, Jane Rogath, Blandina Mmbaga, Haruna Dika, Orgenes Mbwambo and Irene Kida.
Funding
This work was supported through the Transforming Health Professions Education in Tanzania (THET) consortium, under the Health Education Partnership Initiative (HEPI) Project, funded by the NIH through the Fogarty International Centre, Grant No. IR25TWO11227-01.
Disclosure
The authors declare that they have no competing interests.
References
1. Shroff ZC, Javadi D, Gilson L, Kang R, Ghaffar A. Institutional capacity to generate and use evidence in LMICs: current state and opportunities for HPSR. Health Res Policy Systems. 2017;15(1):1. doi:10.1186/s12961-017-0261-1
2. Scheffler RM, Mahoney CB, Fulton BD, Dal Poz MR, Preker AS. Estimates of Health Care Professional Shortages In Sub-Saharan Africa By 2015: critical shortages of health workers are projected in 2015 throughout sub-Saharan Africa, and the projected cost to eliminate them approaches $20 billion. Health Aff. 2009;28(Suppl1):w849–62. doi:10.1377/hlthaff.28.5.w849
3. Sripathy A, Marti J, Patel H, Sheikh JI, Darzi AW. Health professional education and universal health coverage: a summary of challenges and selected case studies. Health Aff. 2017;36(11):1928–1936. doi:10.1377/hlthaff.2017.0517
4. Gruppen LD, Mangrulkar RS, Kolars JC. The promise of competency-based education in the health professions for improving global health. Hum Resour Health. 2012;10(1):1–7. doi:10.1186/1478-4491-10-43
5. Malone K, Supri S. A critical time for medical education: the perils of competence-based reform of the curriculum. Adv Health Sci Educ. 2012;17(2):241–246. doi:10.1007/s10459-010-9247-2
6. Taber S, Frank JR, Harris KA, Glasgow NJ, Iobst W, Talbot M; International CBME Collaborators. Identifying the policy implications of competency-based education. Med Teach. 2010;32(8):687–691. doi:10.3109/0142159X.2010.500706
7. Soare E. Perspectives on designing the competence-based curriculum. Procedia Soc Behav Sci. 2015;May(180):972–977. doi:10.1016/j.sbspro.2015.02.259
8. Lucey CR, Thibault GE, Ten Cate O. Competency-based, time-variable education in the health professions: crossroads. Acad Med. 2018;93(3S):S1–5. doi:10.1097/ACM.0000000000002080
9. Smith HL. Universities, innovation, and territorial development: a review of the evidence. Environ Plann C Gov Policy. 2007;25(1):98–114. doi:10.1068/c0561
10. Carree M, Malva AD, Santarelli E. The contribution of universities to growth: empirical evidence for Italy. J Technol Transf. 2014;39(3):393–414. doi:10.1007/s10961-012-9282-7
11. Valero A, Van Reenen J. The economic impact of universities: evidence from across the globe. Econ Educ Rev. 2019;1(68):53–67.
12. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–645. doi:10.3109/0142159X.2010.501190
13. Nsengimana V. Implementation of competence-based curriculum in Rwanda: opportunities and challenges. Rwandan J Educ. 2020;5(1):36.
14. Hawkins RE, Welcher CM, Holmboe ES, et al. Implementation of competency‐based medical education: are we addressing the concerns and challenges? Med Edu. 2015;49(11):1086–1102. doi:10.1111/medu.12831
15. Mwakigonja AR. The Doctor of Medicine curriculum review at the School of Medicine, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania: a tracer study report from 2009. BMC Med Educ. 2016;16(1):1–5. doi:10.1186/s12909-016-0745-7
16. Loomer PM, Masalu JR, Mumghamba E, Perry DA. New curriculum in dentistry for Tanzania: competency-based education for patient and population health (2008–2011). J Public Health Policy. 2012;33(1):S92–109. doi:10.1057/jphp.2012.39
17. Hine D. Principles and Paradoxes in Modern Healthcare: A Challenge to Professionalism: Queen Elizabeth the Queen Mother Fellowship Lecture 2007. Nuffield Trust; 2007.
18. McNeil KA, Mitchell RJ, Parker V. Interprofessional practice and professional identity threat. Health Soc Rev. 2013;22(3):291–307. doi:10.5172/hesr.2013.22.3.291
19. Ngassapa OD, Kaaya EE, Fyfe MV, et al. Curricular transformation of health professions education in Tanzania: the process at Muhimbili University of Health and Allied Sciences (2008–2011). J Public Health Policy. 2012;33(1):S64–91. doi:10.1057/jphp.2012.43
20. Alade IA. Trends and issues on curriculum review in Nigeria and the need for paradigm shift in educational practice. J Em Trends Educ Res Policy Studies. 2011;2(5):325–333.
21. Touchie C, ten Cate O. The promise, perils, problems and progress of competency‐based medical education. Med Edu. 2016;50(1):93–100. doi:10.1111/medu.12839
22. National Academies of Sciences, Engineering, and Medicine. Future Financial Economics of Health Professional Education: Proceedings of a Workshop; 2017.
23. Lawless WF. Towards an epistemology of interdependence among the orthogonal roles in human–machine teams. Found Sci. 2021;26(1):129–142. doi:10.1007/s10699-019-09632-5
24. Hood K, Cant R, Baulch J, et al. Prior experience of interprofessional learning enhances undergraduate nursing and healthcare students’ professional identity and attitudes to teamwork. Nurse Educ Pract. 2014;14(2):117–122. doi:10.1016/j.nepr.2013.07.013
25. Mgonzo WJ, Yonah ZO. A Review of open access publication in Tanzania. Int J Eng Computer Sci. 2014;3(9):8159–8165.
26. THE World University Rankings. The Muhimbili University of Health and Allied Sciences with the highest ranking among universities in Tanzania ranked #401. Universities in Tanzania-Rankings & Reviews. Available from: https://www.universityguru.com/universities--Tanzania.
27. Sirili N, Angwara K, Simba D. Challenges towards realization of health care sector goals of Tanzania development vision 2025, training and deployment of graduate Human resource for health. East Afr J Public Health. 2013;9(2):476–486.
28. Yin RK. Case Study Research: Design and Methods. sage; 2009.
29. Balandya E, Hyuha G, Mtaya M, et al. Advances in training of the specialized human resources for health in Tanzania: the case of Muhimbili University of Health and Allied Sciences. BMC Med Educ. 2022;22(1):1. doi:10.1186/s12909-022-03102-6
30. MUHAS. Annual Report 2010-2011. Directorate of Planning and Development. Dar es Salaam: Muhimbili University of Health and Allied Sciences; 2011.
31. Sirili N, Kiwara A, Gasto F, Goicolea I, Hurtig AK. Training and deployment of medical doctors in Tanzania post-1990s health sector reforms: assessing the achievements. Hum Resour Health. 2017;15(1):1–2. doi:10.1186/s12960-017-0202-7
32. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. doi:10.1016/j.nedt.2003.10.001
33. Muraraneza C, Mtshali NG, Mukamana D. Issues and challenges of curriculum reform to competency‐based curricula in Africa: a meta‐synthesis. Nurs Health Sci. 2017;19(1):5–12. doi:10.1111/nhs.12316
34. Gruppen LD, Burkhardt JC, Fitzgerald JT, et al. Competency‐based education: programme design and challenges to implementation. Med Edu. 2016;50(5):532–539. doi:10.1111/medu.12977
35. SPHSS-MUHAS. Analysis of the Constraints in Human Resource Availability (Training, Recruitment, Deployment and Retention) Especially in Hard to Reach Areas. Dar Es Salaam: School of Public Health and Social Sciences-Muhimbili University of Health and Allied Sciences. 2009:1–83
36. Sirili N, Kiwara A, Nyongole O, Frumence G, Semakafu A, Hurtig AK. Addressing the human resource for health crisis in Tanzania: the lost in transition syndrome. Tanzan J Health Res. 2014;16(2). doi:10.4314/thrb.v16i2.6
37. Sirili N, Frumence G, Kiwara A, Mwangu M, Goicolea I, Hurtig AK. “Doctors ready to be posted are jobless on the street…” the deployment process and shortage of doctors in Tanzania. Hum Resour Health. 2019;17(1):1. doi:10.1186/s12960-019-0346-8
38. Sirili N, Anaeli A, Mselle L, Nyongole O, Massawe S. we were like tourists in the theatre, the interns assisted almost all procedures…” Challenges facing the assistant medical officers training for the performance of caesarean section delivery in Tanzania. BMC Med Educ. 2021;21(1):1. doi:10.1186/s12909-020-02480-z
39. Bidabadi NS, Isfahani AN, Rouhollahi A, Khalili R. Effective teaching methods in higher education: requirements and barriers. J Adv Med Educ Professionalism. 2016;4(4):170.
40. Maksymchuk B, Matviichuk T, Solovyov V, et al. Developing healthcare competency in future teachers. Revista Romaneasca Pentru Educ Multidimensionala. 2020;12(3):24–43. doi:10.18662/rrem/12.3/307
41. Rizvi NF, Gulzar S, Nicholas W, Nkoroi B. Barriers in adopting blended learning in a private university of Pakistan and East Africa: faculty members’ perspective. Mhealth. 2017;3:3. doi:10.21037/mhealth.2017.01.01
42. Foley AR, Masingila JO. Building capacity: challenges and opportunities in large class pedagogy (LCP) in Sub-Saharan Africa. Higher Educ. 2014;67(6):797–808. doi:10.1007/s10734-013-9697-6
43. Caverzagie KJ, Nousiainen MT, Ferguson PC, et al. Overarching challenges to the implementation of competency-based medical education. Med Teach. 2017;39(6):588–593. doi:10.1080/0142159X.2017.1315075
44. Edwards RA, Venugopal S, Navedo D, Ramani S. Addressing needs of diverse stakeholders: twelve tips for leaders of health professions education programs. Med Teach. 2019;41(1):17–23. doi:10.1080/0142159X.2017.1396307
45. Kiguli-Malwadde E, Olapade-Olaopa EO, Kiguli S, et al. Competency-based medical education in two Sub-Saharan African medical schools. Adv Med Educ Practice. 2014;5:483. doi:10.2147/AMEP.S68480
46. Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Information. 2004;22(2):63–75. doi:10.3233/EFI-2004-22201
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
