Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Operation Status of the Mutual Aid Human Milk Bank for Preterm Infants and Data Analysis
Authors Wang H, Hu XL, Li QF, Zhou J, Wu MY
Received 13 September 2023
Accepted for publication 3 November 2023
Published 16 November 2023 Volume 2023:16 Pages 3521—3530
DOI https://doi.org/10.2147/JMDH.S440114
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hua Wang,1 Xiao-Li Hu,2 Qiu-Fang Li,3 Jie Zhou,1 Ming-Yuan Wu1
1Department of NICU, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, 310006, People’s Republic of China; 2Department of Obstetrics, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, 310006, People’s Republic of China; 3Department of Nursing, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, 310006, People’s Republic of China
Correspondence: Ming-Yuan Wu, Department of NICU, Women’s Hospital, Zhejiang University School of Medicine, No. 1 of Xueshi Road, Shangcheng District, Hangzhou, 310006, People’s Republic of China, Tel + 86 13958115502, Email [email protected]
Objectives: This study aimed to investigate the matching degree between the donated supply and demand, clinical characteristics of both donors and recipients, along with the operation cost.
Methods: From January 1, 2018 to December 31, 2021, the data on human milk donation and usage, the clinical characteristics of donors and recipients, and the cost of each operating center were collected from the Manual Donation Registration Form and Information Management System of the selected human milk bank.
Results: During the four years that the human milk bank was in operation, the volume of donated milk was slightly greater than the volume of consumed milk. A total of 1364 donors donated 2434.63 liters of qualified human milk, for RMB 1,791,000 (USD 257, 202), ie, RMB 385.3 (USD 55.3)/L; 97.8% of the donors were preterm puerperae, and 59% of the donors donated between 1 week and 1 month after delivery. All recipients were preterm infants and received donated human milk for a duration of 9.4 days on average. During the four years of operation, the proportion of donors who had previously received donated milk among all donors showed an overall increasing trend, while the incidence of NEC in preterm infants gradually decreased.
Conclusions: The increasingly optimized structure of donors, the more economical operation, and the fact that the use of donated milk may not affect breastfeeding of the recipients have made it a human milk bank operation mode worthy of promotion.
Keywords: donated human milk, human milk bank, NEC, operating cost, preterm infants
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Nurfatimah has been published for this article.
Introduction
Breast milk has unique nutritional and immune activity and is the most ideal food source for infant health. For premature babies, breast milk is a also a preferred food with therapeutic effects.1 Breastfeeding advantages extend beyond the properties of human milk itself, and a complex of nutritional, environmental, socioeconomic, psychological as well as genetic interactions establishes a massive list of benefits of breastfeeding to the health outcomes of the breastfed infant, with added value in premature infants.2 It has several benefits such as reducing the incidence of bronchopulmonary dysplasia, late-onset sepsis, and neonatal necrotizing enterocolitis (NEC) in preterm infants, promoting the development of their neuroimmune system,3 and lowering heavy and long-term social burdens in future related to social assistance and special education that preterm infants may require as they grow, therefore guaranteeing the sustainable development of social productivity.4 Preterm infants in China are cared for in the neonatal intensive care unit (NICU), and due to factors such as maternal separation, immaturity of various systems, diseases suffered by preterm infants, maternal conditions, and the social environment, they are unable to be breastfed,5 hence, the donated human milk from human milk banks is an optimal alternative to maternal breastmilk. Donated human milk is currently recommended by the World Health Organization,6 American Academy of Pediatrics,7 and European Society for Pediatric Gastroenterology, Hepatology, and Nutrition as the preferred alternative to maternal human milk.8
Human milk banks are nonprofit professional organizations that recruit human milk donors, collect donated human milk, and screen, process, store, and distribute human milk.9 Scientific and comprehensive operational guidelines have been developed by the Human Milk Bank Association of North America and Human Milk Bank Association of Europe.10,11 Norway,12 Germany,13 South Korea,14 and Italy15 modified and supplemented the management guidelines of the Association based on their own conditions. Currently, human milk banks abroad rely on corporate and institutional donations.16
Human milk banks in China have developed rapidly, from 2 in 2013 to 14 in 2016, Currently, there are about 20 human milk banks.17 Since 2016, researchers have conducted studies on human milk banks,18–21 and have successively released various specifications, guidelines, and consensus.9,22–25 Human milk banks are currently facing two major challenges.1 Human milk banks are generally established by medical institutions in China, which lack sufficient operational funding, face instability in terms of donors, and have insufficient donated milk. Therefore, we created a mutual aid human milk bank model, which over the course of four years of operation, improved the feasibility and operational efficiency of continuous milk donation, while also providing a reference program with Chinese characteristics for long-term development of human milk banks. It is hereby reported as follows.
Participants and Methods
Data Sources of the Participants and Study Variables
From January 1, 2018 to December 31, 2021, a retrospective analysis was performed on the human milk bank of a Grade A Class 3 Maternity Hospital in Zhejiang Province, involving the clinical characteristics of donors/recipients, supply and demand of the donated milk, operating costs, and NEC incidence in preterm infants. This study complied with the Declaration of Helsinki and was approved by the Medical Research Ethics Committee of Women’s Hospital, Zhejiang University School of Medicine (IRB-20220045-R). The informed consent obtained from the legal guardians of the participants prior to study commencement for the use of their data in this study.
Study Methods
The human milk bank was established in 2017 to receive fresh, refrigerated, or frozen human milk from the neonatology department of our hospital. The bank, which consists of a collection room, a sterilization processing room, and a storage room, is equipped with three pasteurizers, one human milk composition analyzer, two −20 °C refrigerating cabinets, two medical refrigerators, and one hospital-grade breast pump. In terms of personnel, there is one person in charge and one dedicated nurse. The Bank also has an independent electronic information system,23 which is used to save and manage the data about the milk donations and usage of the human milk bank, thus tracing and ensuring the safety of milk use. The donated human milk is preferred for very (ultra-) low birth weight (VLBW) preterm infants, and in principle, it is given until the mother has sufficient milk or the gestational age is corrected to 32–34 weeks.
The human milk bank implements the Hazard Analysis Critical Control Point (HACCP) management system,19 which involves the following four major processes: ① Recruitment: Home promotion, signing of informed consent form, and preliminary health screening. ② Collection: Serological screening, pumping, home storage, human milk transport, reception, and storage at the human milk bank, and donor data entry. ③ Processing and storage: Thawing, mixing and dispensing, pasteurization, bacteriological screening, freezing for future use, or discarding. ④ Distribution: Issuing medical advice, thawing and distributing, recording the usage, and monitoring feeding.
Source of Human Milk Donation
The milk donation comes from stored human milk collected from mothers with preterm infants in our hospital.
Recruitment and Screening
It is necessary to promote breastfeeding among the parents of all ≤ 34-week preterm infants, and fully inform them of the benefits of breast/human milk feeding and the risks of formula milk. Based on the principles of voluntariness, the recipients signed three informed consent forms: ① Informed consent for fresh breastfeeding, which can strongly encourage fresh breastfeeding; ② Informed consent for use of donated human milk, ie, the use of pasteurized donated human milk in the case of insufficient breast milk; ③ Informed consent for non-remunerated human milk donation, ie, the donation of surplus human milk to other preterm infants in need of human milk. The dedicated nurse of the human milk bank performed preliminary health screening of all preterm puerperae during the promotion of colostrum feeding based on their living habits, history of smoking and drinking, history of drug abuse, history of previous diseases, and history of medication. We also promoted incentive measures during the promotion process; for example, anyone who donates more than 800 mL of human milk in a single donation could apply for a 5G+VR remote consultation service.
Collection
The working staff of the human milk bank collected the relevant laboratory results of the puerperae during hospitalization through the HIS system, which could replace the need for serological tests of the donors for at least 3 months. After including the eligible puerperae, the dedicated nurse collected the human milk in two ways: ① Fractional donation: If the distance was short, the puerpera or a family member would deliver fresh or frozen breast milk for the infant once a day; the dedicated nurse would calculate the volume of human milk to be fed on that day based on medical advice, and the excess volume would be frozen and stored. After the preterm infant is discharged from the hospital, the pre-stored human milk would be summarized and officially stored in the bank. On the same day, the human milk would be dissolved, divided, and pasteurized for future use. ② Discharge donation: In case of long distance, the puerpera or family member would deliver the frozen human milk at least every 2–3 days. No donations were allowed in the initial stage, to ensure maternal breastfeeding. After a preterm infant was discharged from the hospital, the remaining human milk pre-stored in the refrigerating cabinet of the human milk bank would be donated and sterilized for future use.
Cost and Financial Compensation
The total operating cost of the human milk bank involve four cost centers—promotion and recruitment, collection, processing, and storage, and distribution, including the costs of consumables, labor, office supplies, energy consumption, equipment depreciation (including depreciation and maintenance of housing), and testing, all of which are currently borne by the hospital. The human milk bank of our hospital is currently operating on a “free donation, free use, and moderate compensation” model. At the distribution stage, donated human milk is thawed and delivered to the neonatology department, where the specialized nurses dispense and feed the infants based on medical advice. Our hospital has set a reasonable human milk processing fee of RMB 50/day, which is stipulated to be charged once regardless of the number/volume of donations received on one day by calculating the costs of sanitary materials (sterilized gloves, collection bottles, syringes/disposable bottles, milk storage bottles) and salary (staff consumption and time consumption) in this process, and as approved by the relevant department.
Study Variables and Evaluation Indexes
(1) The age, gestational week, mode of delivery, educational background, time of first donation, donation volume, and number of donations by the donor. Gestational age, birth weight, days of donation of the recipient. (2) Total and unit costs: In this study, a four-step process model was used to divide all operations into four cost centers (recruitment, collection, storage, and distribution), involving direct and indirect cost elements related to human milk donation; the annual cost and unit cost of operating and managing the milk bank of our hospital were calculated based on the operation-based costing process of Chinese human milk banks developed by Cun.26 Cost of each cost center = Direct cost of operation+Σ (Standard unit price of each resource × Consumption of the resource). Total human milk bank operating costs = Σ (Cost of cost center). Compensation cost = Σ (Number of recipients per day × Single human milk disposal fee). Unit cost of 1 L donated milk = (Total operating cost of the human milk bank in the same period - Compensation cost in the same period)/Total volume of eligible donated human milk in the same period (L). (3) Incidence of NEC in preterm infants = Number of preterm infants in the same period/Total number of preterm infants in the same period × 100%. The modified Bell-NEC grading criteria in the fifth edition of Practical Neonatology was used to make the diagnosis of NEC,27 and the preterm infants were determined to have NEC based on the clinical features and radiographic evidence.
Data Collection Method
From 2018 to 2021, the dedicated nurse at the human milk bank collected and acquired the relevant data of both donors and recipients, as well as the cost of each cost center, through the Manual Donation Registration Form and the Human Milk Bank Information Management System; the data was later entered into the database, and checked by the head of the human milk bank. The NICU physicians calculated the NEC incidence in preterm infants.
Statistical Method
SPSS26.0 statistical software was used to process the data. The measurement data conforming to a normal distribution were expressed by mean ± standard deviation, and those not conforming to normal distribution were expressed as median and interquartile range. The counting data were expressed as cases, percentage, and percent.
Results
General Operating Data of the Human Milk Bank
(1) Donor clinical characteristics: The mean age was 30.52±4.65 years old, the mean gestational week was 31.13±2.62 weeks, 55.79% had an education background of junior college and below, 68.55% had cesarean section, 2.20% had full-term delivery, and 68.18% were primiparae (Table 1). Furthermore, the average number of donations was 6.44±1.26 times, the average time to first donation was 4.04±2.43 days, and the individual donations ranged from 130 mL to 37,300 mL, with the median of 2125 mL. The proportion of total donors who had previously received donated human milk among all donors was 63.49% (313/493) in 2018, 65.58% (242/369) in 2019, 69.35% (172/248) in 2020, and 87.40% (222/254) in 2021, showing an increasing trend.
 |
Table 1 Clinical Signs of the Donors |
(2) Clinical characteristics of the recipients: As shown in Table 2, the mean gestational age was 31.23±2.39 weeks, the mean birth weight was 1508.01±504.25 g, the mean days of receiving donated human milk was 9.39±9.24 days, and the mean hospital stay was 42.34±23.80 days.
 |
Table 2 Duration of Breast Donation Therapy for Recipients |
(3) The annual milk donation to the human milk bank of our hospital was slightly greater than consumption, which can ultimately meet the basic demand of the hospital. Due to the impact of COVID-19, the number of infants in the NICU decreased in 2019 and 2020, as well as the volume of milk donation and the number of donors and recipients. After the decline in the intensity of the epidemic, the operation of the human milk bank gradually returned to normal, and in 2022, the number of recipients and volume of eligible milk donation significantly increased, as shown in Table 3.
 |
Table 3 Quality of Donated Human Milk in the Human Milk Bank and Its Usage from 2018 to 2021 |
Calculation of the Operating Cost
Table 4 shows the proportion of each cost center in the total cost of operation. The processing and storage costs accounted for the highest percentage, followed by the distribution cost, and the collection and recruitment costs. Over a 4-year period, the total cost of the human milk bank of our hospital was RMB 1,790,872, and the human milk disposal fee was RMB 852,790 (Table 5). The processing cost of 1 L of donated human milk decreased from RMB 735.58 (USD 102.19) to RMB 385.31 (USD 54.15).
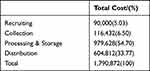 |
Table 4 Cost Allocation Among Different Cost Centers of the Human Milk Bank from 2018 to 2021 |
 |
Table 5 Breakdown of Reimbursement for the Human Milk Bank from 2018 to 2021 |
NEC Incidence in Preterm Infants
NEC incidence in preterm infants was 66/775=8.5% in 2018, 58/767=7.5% in 2019, 44/733=6.0% in 2020, and 38/740=5.1% in 2021, revealing an overall decreasing trend, as shown in Figure 1.
 |
Figure 1 Incidence of necrotizing enterocolitis in preterm infants from 2018 to 2021. |
Discussion
Mutual Aid Human Milk Bank for Preterm Infants Optimized the Donor Structure
One of the important conditions for normal operation of a human milk bank is the availability of healthy human milk donors. Currently, most donors are volunteers recruited from society; however, the costs of serological testing, and human milk preservation and transportation reduces the interest of donors and creates difficulty in donation.28 Furthermore, as the targeted lactation of mothers of the preterm infants target lactation on Day 7 after delivery is >190 mL/d,29 the excess human milk from mothers of VLBW preterm infants is discarded. The Mutual Aid Human Milk Bank for Preterm Infants acquires the excess human milk for preterm infants during hospitalization, thereby preventing wastage and achieving redistribution of this valuable resource.
The composition of preterm human milk differs from that of full-term human milk, making its nutritional value and biological functions more suitable for preterm infants.30,31 In the human milk bank of our hospital, 97.8% of the donors were preterm puerperae, which is significantly higher than that reported in domestic and international literature.17,32–34 Since many preterm infants were recipients, their mothers understood the importance of human milk donation and were more willing to be donors. In this study, the proportion of all donors who previously received donated milk among all donors increased year after year. When human milk became abundant, the mothers of the recipients would actively donate their milk out of empathy and gratitude, creating a virtuous circle. Simultaneously, the previous receipt of the donated human milk increased the donors’ awareness of the formal donation, creating a good compliance in the process of human milk collection and storage, thus increasing the qualification rate (qualified milk donation/total milk donation) year after year. It is worth noting that during the four years of operation of the human milk bank, the mean gestational age of donors was close to that of recipients (around 31 weeks, with a standard deviation of about 2 weeks), indicating that the human milk bank of our hospital provided preterm infants with the most appropriate human milk, rather than human milk of any gestational age. Another characteristic of the human milk bank of our hospital is that most donors began donating between 1 week and 1 month after delivery, which was earlier than the time to first donation reported in relevant literature.17,32,33 The composition of human milk varies with birth age, and donated human milk generally comes from the later stages of lactation, so the composition is similar to that of mature milk with relatively low nutrient content.35 The donors of our human milk bank can provide preterm infants with human milk that contains more calories, fat, and protein concentration.36,37 The number of donors who began donating human milk 3 months after delivery decreased rapidly, most likely due to the fact that most Chinese women only have 4–6 months of maternity leave and their free time and lactation volume would decrease significantly upon returning to work.
Our donors ranged from 25 to 35 years, and approximately 70% of the donors were primiparae, which is similar to the characteristics of the donor population reported in literature.17,32–34 As our hospital is a referral center for high-risk pregnancies in Hangzhou and surrounding areas, donors undergoing cesarean section accounted for a high proportion (up to 68.55%), which differed from what was reported in Mainland China,17 but is similar to what was reported in Vietnam (up to 57%).33 Most donors had a junior college education or below, which is similar to a study in India,38 indicating that women with low education levels can also be motivated to donate human milk.
Mutual Aid Human Milk Bank for Preterm Infants Did Not Affect Maternal Breastfeeding for Recipients
The recipients of the donated human milk in this study were preterm infants, and 84.7% received donated human milk for less than 15 days (9.4 days on average), which was longer than the duration reported in Nanjing Maternal and Child Health Care Hospital and Da Nang Hospital in Vietnam,33,34 but much shorter than that reported in Scotland and Taiwan,32,39 most likely because most of the mothers could produce sufficient human milk for feeding after a certain point in time. In this study, we also discovered that the duration of receiving the donated human milk was no more than 25% of the total hospital stay, indicating that the donated human milk provided temporary support in case of insufficient maternal milk, and could give the corresponding mothers time to establish their own milk supply. In the absence of maternal breastfeeding, the donated human milk could be a critical “bridge” for the infants.40 The proper use of donated human milk as a transition prior to maternal breastfeeding can enable mothers to initiate and maintain breastfeeding during separation, without using infant formula as a supplement. To avoid potential overuse and misuse of the donated human milk, most preterm infants should take donated human milk as a brief alternative in the process of promoting breastfeeding, rather than being the entirety of their feeding regimen. Therefore, it is important to reduce the duration and volume of donated human milk consumption, accelerate maternal breastfeeding, and encourage these mothers to become donors.
Mutual Aid Human Milk Bank for Preterm Infants Reduced the Cost
It is critical to seek financial backing for constructing human milk banks. In foreign countries, the cost of donated human milk per infant in the NICU ranged from USD 27 to USD 590/L.41 In China, Cun26 calculated the unit cost of processing 1 mL of donated human milk in Chinese public hospital human milk banks based on the activity-based costing method, ie, RMB 0.80–1.14, with little difference across regions. Daili et al42 investigated the costs of human milk banks in China with mature operating systems, and found that the human milk bank of Guangzhou Women and Children’s Medical Center had an operating cost of USD 141/L, the human milk bank of Nanjing Maternity and Child Health Care Hospital had an operating cost of USD 117/L, and the human milk bank of Shanghai Children’s Hospital had an operating cost of USD 168/L. As for the Mutual Aid Human Milk Bank for Preterm Infants, during the collection process, the serological test was replaced with the serological report of the donors (hospitalized puerperae) during delivery, and no repeated test was required within 3 months, reducing the cost of donor screening and ensuring the standardization of donation. The cost of collection was significantly reduced, far below the percentage reported by the human milk bank of Shanghai Children’s Hospital.26 In the process of recruitment, we saved the costs of transportation, telephone consultation, promotion, and reception. Furthermore, we proposed a reasonable compensation policy for charging the human milk disposal fee, which can further reduce the cost.
NEC Incidence Showed a Decreasing Trend During the Operation of the Mutual Aid Human Milk Bank for Preterm Infants
As per domestic and foreign research, the maternal breastfeeding quality improvement program can significantly reduce NEC incidence.43–46 The results of this study showed that donated human milk was equally effective, as it could avoid the direct toxic effects of formula on intestinal epithelial cells, and decrease intestinal permeability, lowering NEC incidence,47 while possessing bioactive substances. Follow-up large sample studies need to be conducted to determine whether maternal breastfeeding reduces NEC incidence and severity better than donated human milk.
Conclusion
The Mutual Aid Human Milk Bank for Preterm Infants of our hospital could achieve self-sufficiency based on the steady flow of human milk provided by premature mothers, thus creating a satisfactory trickle-down effect. The continuous operation of our human milk bank mainly relied on funds and sources of donated human milk, and the four-year successful operation proved the sustainable model of the construction and maintenance of the Mutual Aid Human Milk Bank for Preterm Infants. It is imperative to actively expand the methods and means of milk donation, seek funding compensation, ensure the good circulation of the management of the human milk bank, and provide a more evidence-based foundation for the development of human milk banks.
We must realize the importance not only of promoting maternal breastfeeding but ensuring we do all we can to support it, hence providing counsellors also in the NICU where women maybe able to breastfeed directly also their preterm babies. In 2021, fifteen national departments, including the National Health Commission of the People’s Republic of China, collaborated to create the Breastfeeding Promotion Action Plan (2021–2025), to further promote breastfeeding. Human milk (especially fresh maternal milk) can provide preterm infants with the most natural and optimal nutrition. It is the only and the most effective method for reducing the incidence and severity of NEC. It is imperative to take multiple measures to promote fresh maternal breastfeeding for preterm infants, followed by refrigerated human milk, frozen human milk, and pasteurized donated human milk. The Mutual Aid Human Milk Bank of our hospital helped preterm infants by bridging, supplementing, and facilitating breastfeeding.
Funding
This study was supported by Medical and health technology program of Zhejiang Province (Award number 2022RC041, 2021KY769).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Han SP. Problems and future development of human milk bank in China. Chin J Perinatal Med. 2022;25(7):488–493. doi:10.3760/cma.j.issn113909-20220429-00426
2. Shamir R. The Benefits of Breast Feeding. Nestle Nutr Inst Workshop Ser. 2016;86:67–76. doi:10.1159/000442724
3. Li YW, Yan CY, Yang L, et al. Effect of breastfeeding versus formula milk feeding on preterm infants in the neonatal intensive care unit. Zhongguo Dang Dai Er Ke Za Zhi. 2017;19(5):572–575. doi:10.7499/j.issn.1008-8830.2017.05.019
4. Feng Q. “The 8th international breastfeeding and lactation symposium”summary. Chin J Perinatal Med. 2013;16(7):402–403. doi:10.3760/cma.j.issn.1007-9408.2013.07.006
5. Xu L, Cao XM, Mei H, et al. Challenges and countermeasures of breastfeeding for preterm infants in neonatal intensive care units in China. Chin Pediatr Emerg Med. 2021;28(12):1111–1114. doi:10.3760/cma.j.issn.1673-4912.2021.12.014
6. World Health Organization. Feeding of low-birth-weight infants in low- and middle-income countries[DB/OL]; 2011. Available from: https://www.who.int/publications-detail-redirect/9789241548366.
7. American Academy of Pediatrics (AAP) Committee on Nutrition, AAP Section on Breastfeeding, AAP committee on Fetus and Newborn. Donor human milk for the high-risk infant: preparation, safety, and usage options in the United States. Pediatrics. 2017;139(1):e20163440. doi:10.1542/peds.2016-3440
8. Arslanoglu S, Corpeleijn W, Moro G, et al. Donor human milk for preterm infants: current evidence and research directions. J Pediatr Gastroenterol Nutr. 2013;57(4):535–542. doi:10.1097/MPG.0b013e3182a3af0a
9. Board E. Operation guidance of Chinese human milk banking. Zhonghua er ke za zhi. 2017;55(8):573–576. doi:10.3760/cma.j.issn.0578-1310.2017.08.005
10. Spatz DL. Pasteurized donor human milk and milk banking through the human milk banking association of North America. J Obstet Gynecol Neonatal Nurs. 2018;47(4):545–546. doi:10.1016/j.jogn.2018.02.004
11. Haiden N, Ziegler EE. Human milk banking. Ann Nutr Metab. 2016;69(Suppl. 2):8–15. doi:10.1159/000452821
12. Grøvslien AH, Grønn M. Donor milk banking and breastfeeding in Norway. J Hum Lact. 2009;25(2):206–210. doi:10.1177/0890334409333425
13. Springer S. News about human milk banking in Germany. Adv Exp Med Biol. 2000;478(47):441–442. doi:10.1007/0-306-46830-1_67
14. Jang HL, Cho JY, Kim MJ, et al. The experience of human milk banking for 8 Years: Korean perspective. J Korean Med Sci. 2016;31(11):1775–1783. doi:10.3346/jkms.2016.31.11.1775
15. Arslanoglu S, Bertino E, Toneto P, et al. Amendment to 2010 Italian guidelines for the establishment and operation of a donor human milk bank. J Biol Reg Homeos Ag. 2012;26(3 Suppl):61–64.
16. Dai CL. Human milk bank operation and management mode. Inter J Pediatrics. 2019;46(2):123–126. doi:10.3760/cma.j.issn.1673-4408.2019.02.013
17. Liu XH, Han SP, Wei QF, et al. The data and characteristics of the human milk banks in mainland China. World J Pediatr. 2019;15(2):190–197. doi:10.1007/s12519-019-00226-6
18. Chen XH, Yu ZB, Han SP. Outcomes of very low birth weight infants and extremely low birth weight infants fed either with human donors’ milk or formula. Chin J Appl. 2016;31(19):1464–1467. doi:10.3760/cma.j.issn.2095-428X.2016.19.007
19. Li QF, Wang H, Xu XF. Application of hazard analysis and critical controI system in the safety management of NICU human milk. Chin J Pract Nurs. 2018;34(29):2297–2300. doi:10.3760/cma.j.issn.1672-7088.2018.29.013
20. Chu X, Xu H, Han SP, et al. Evaluation on the operation and quality improvement of milk bank in Nanjing maternity and child health care hospital. Shanghai Nur. 2020;20(8):8–12. doi:10.3969/j.issn.1009-8399.2020.08.003
21. Wu B, Li QF, Yi SY, et al. The construction and application of intelligent information management system for donor human milk bank. Chin J Nur. 2021;56(2):189–193. doi:10.3761/j.issn.0254-1769.2021.02.005
22. Board E. Expert advice on quality and safety management of Chinese human milk banking. Zhonghua er ke za zhi. 2017;55(8):577–579. doi:10.3760/cma.j.issn.0578-1310.2017.08.006
23. Chinese Nutrition Society. Establishment and management of human milk bank in medical institutions:T/CNSS 2020-003[S/OL]; 2020. Available from: https://www.cnsoc.org/notice/files/@CmsXh_1646ee69-066d-4f76-be2b-3eldbb8cb3de.pdf.
24. Beijing Municipal Bureau of Market Supervision and Administration. Announcement of Beijing Local Standards No. 12, 2021 (General No. 287)[A/OL]; 2021. Available from: http://scjgj.beijing.gov.cn/zwxx/gs/dfbzgg/202112/t20211231_2579564.html.
25. Hangzhou Health Promotion Association. Management specification for premature infant breast milk bank:T/HHPA 005—2020[S/OL]; 2022. Available from: http://www.ttbz.org.cn/StandardManage/Detail/38918/.
26. Cun DL. Cost analysis and compensation policy research of human milk banks in China. Shanghai: Shanghai Jiao Tong University; 2020.
27. Shao XM, Ye HM, Qiu XS. Practical Neonatology.
28. Tian C, Li Y, Soowon L, et al. Lactating women’s knowledge and attitudes about donor human milk in China. J Hum Lact. 2021;37(1):52–61. doi:10.1177/0890334420939057
29. Dong D, Ru X, Huang X, et al. A prospective cohort study on lactation status and breastfeeding challenges in mothers giving birth to preterm infants. Int Breastfeed J. 2022;17(1):6. doi:10.1186/s13006-021-00447-4
30. Underwood MA.Human milk for the premature infant. Pediatr Clin North Am. 2013;60(1):189–207. doi:10.1016/j.pcl.2012.09.008
31. Gila-Diaz A, Arribas SM, Algara A, et al. A review of bioactive factors in human breastmilk: a focus on prematurity. Nutrients. 2019;11(6):1307. doi:10.3390/nu11061307
32. Chang FY, Cheng SW, Wu TZ, Fang LJ. Characteristics of the first human milk bank in Taiwan. Pediatr Neonatol. 2013;54(1):28–33. doi:10.1016/j.pedneo.2012.11.004
33. Tran HT, Nguyen TT, Barnett D, et al. Trends and dynamics in the first four years of operation of the first human milk bank in Vietnam. Nutrients. 2021;13(4):1107. doi:10.3390/nu13041107
34. Xiaoshan H, Xue C, Jun Z, et al. Eight-year operation status and data analysis of the first human milk bank in East China. Int Breastfeed J. 2022;17(1):65. doi:10.1186/s13006-022-00502-8
35. Tong XM, Feng ZC. Preterm breastfeeding.
36. Gidrewicz DA, Fenton TR. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 2014;14(1):216. doi:10.1186/1471-2431-14-216
37. Lamb RL, Haszard JJ, Little HMJ, et al. Macronutrient composition of donated human milk in a New Zealand population. J Hum Lact. 2021;37(1):114–121. doi:10.1177/0890334420963666
38. Katke RD, Saraogi MR. Socio-economic factors influencing milk donation in milk banks in India: an institutional study. Int J Rep Contracept Obstet Gynecol. 2014;3(2):389–393. doi:10.5455/2320-1770.ijrcog20140621
39. Simpson J. Who gets donated human milk in Glasgow. In:
40. Shenker N, Staff M, Vickers A, et al. Maintaining human milk bank services throughout the COVID-19 pandemic: a global response. Matern Child Nutr. 2021;17(3):e13131. doi:10.1111/mcn.13131
41. Carroll K, Herrmann KR. The cost of using donor human milk in the NICU to achieve exclusively human milk feeding through 32 weeks postmenstrual age. Breastfeed Med. 2013;8(3):286–290. doi:10.1089/bfm.2012.0068
42. Daili C, Kunkun Z, Guangjun Y. Cost analysis of operating a human milk bank in China. J Hum Lact. 2020;36(2):264–272. doi:10.1177/0890334419894551
43. Zhu HD. Jiang YJ. A quality improvement program to facilitate breastfeeding for very low birth weight infants. Chin J Perinatal Med. 2019;22(9):637–640. doi:10.3760/cma.j.issn.1007-9408.2019.09.007
44. Talavera MM, Bixler G, Cozzi C, et al. Quality improvement initiative to reduce the necrotizing enterocolitis rate in premature infants. Pediatrics. 2016;137(5):e20151119. doi:10.1542/peds.2015-1119
45. Nathan AT, Ward L, Schibler K, et al. A quality improvement initiative to reduce necrotizing enterocolitis across hospital systems. J Perinatol. 2018;38(6):742–750. doi:10.1038/s41372-018-0104-0
46. Goddard GR, McNelis K, Poindexter A, et al. Quality improvement efforts reduce incidence of surgical necrotizing enterocolitis and related deaths. Am J Perinatol. 2021;38(13):1386–1392. doi:10.1055/s-0040-1712967
47. Meier P, Patel A, Esquerra-Zwiers A. Donor human milk update: evidence, mechanisms, and priorities for research and practice. J Pediatr. 2017;180:15–21. doi:10.1016/j.jpeds.2016.09.027
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
