Back to Journals » Infection and Drug Resistance » Volume 17
Omadacycline for the Treatment of Severe Chlamydia psittaci Pneumonia Complicated with Guillain-Barre Syndrome
Authors Wang J , Dong S, Fang M , Fan Z, Xu Y
Received 28 September 2023
Accepted for publication 29 December 2023
Published 9 January 2024 Volume 2024:17 Pages 81—87
DOI https://doi.org/10.2147/IDR.S437100
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Sandip Patil
Juan Wang, Shuangyong Dong, Mengjuan Fang, Zhiyan Fan, Yuansheng Xu
Department of Emergency, Affiliated Hangzhou First People`s Hospital, School of Medicine, Westlake University, Hangzhou, People’s Republic of China
Correspondence: Yuansheng Xu, Department of Emergency, Affiliated Hangzhou First People`s Hospital, School of Medicine, Westlake University, No. 261 Huansha Road, Hangzhou, Zhejiang Province, 310006, People’s Republic of China, Email [email protected]
Background: Chlamydia psittaci (C. psittaci) is a pathogen that is seldom implicated in community-acquired pneumonia and is rarely linked to severe pneumonia. Reports of severe C. psittaci pneumonia accompanied by Guillain-Barre syndrome (GBS) are scarce. Tetracyclines are the preferred therapeutic approach for psittacosis. Omadacycline, a novel tetracycline, demonstrates strong antibacterial efficacy against typical bacteria and atypical pathogens, including C. psittaci. However, its application in the treatment of psittacosis pneumonia remains constrained.
Case Presentation: A 77-year-old female patient was admitted to the hospital presenting with symptoms of fever, low back pain, and headache. The diagnosis of C. psittaci was established through the utilization of metagenomic next-generation sequencing (mNGS). Initial administration of moxifloxacin, meropenem, piperacillin-tazobactam, and doxycycline proved to be ineffective. Subsequent omadacycline leaded to the successful resolution of fever and dyspnea. However, after the endotracheal tube was removed, the patient experienced a rapid decline in symmetrical limb strength, leading to a diagnosis of GBS based on clinical manifestations, cerebrospinal fluid analysis, and electromyography. Following a 5-day course of immunoglobulin therapy and nutritional nerve treatment, the patient’s condition ameliorated, culminating in an uncomplicated discharge.
Conclusion: This case provides evidence supporting the potential use of omadacycline as a therapeutic option for the treatment of severe C. psittaci pneumonia. The utilization of mNGS technology is of paramount importance in the prompt identification of uncommon pathogens, including C. psittaci. Nevertheless, the occurrence of GBS should be taken into consideration when C. psittaci pneumonia is accompanied by symmetrical limb weakness. These findings have important implications for the diagnosis, treatment, and management of patients with C. psittaci pneumonia.
Keywords: Chlamydia psittaci pneumonia, Guillain-Barre syndrome, omadacycline, metagenomic next‑generation sequencing
Introduction
Chlamydia psittaci (C. psittaci) is classified within the order Chlamydia and is an obligate intracellular parasite within the chlamydia family. This family derives its name from its propensity to parasitize birds belonging to the psittaci family.1 Inhalation serves as the primary mode of infection transmission, while prolonged exposure to infected avian species such as chickens, ducks, geese, and other poultry can also result in infection. The clinical manifestations of psittacosis exhibit a lack of specificity, with various systems of the entire body being susceptible to its effects. These effects can range from mild flu-like symptoms to severe and life-threatening conditions such as acute respiratory distress syndrome, rhabdomyolysis, Guillain-Barre syndrome (GBS), and multiple organ failure.2 GBS, a disease of the peripheral nervous system, is induced by post-infection and autoimmune factors.3 Instances of C. psittaci pneumonia associated with GBS have been rarely documented. While tetracyclines are the preferred treatment for psittacosis, their efficacy may be limited in cases of severe C. psittaci pneumonia complicated by GBS and liver and kidney involvement.
Omadacycline is a novel semi-synthetic tetracycline developed by Paratek Pharmaceutical in the United States.4 It has been found to have a broad antibacterial spectrum and has great antibacterial activity against atypical bacteria such as C. psittaci,5 however, there is a scarcity of clinical literature regarding the use of omadacycline in the treatment of psittacosis.6 In this report, we present a case of severe C. psittaci pneumonia accompanied by GBS that was successfully treated with omadacycline, resulting in a favorable prognosis.
Case Presentation
The patient was admitted to the hospital on October 12, 2022, with a fever for 5 days, low back pain, and headache for 3 days. Five days before admission, the patient received no treatment with a fever, chills, and fatigue. Three days ago, the patient developed a high fever, expiratory dyspnea, and experienced back pain and headaches as a result of a fall while walking on level ground, prompting a visit to the local hospital. The patient’s blood routine analysis revealed a white blood cell count (WBC) of 12.5 × 109/L, a neutrophil percentage of 94.2%, a C-reactive protein (CRP) level of 302.4 mg/L, and procalcitonin (PCT) levels of 5.0 ng/mL. Chest computed tomography (CT) (Figure 1A) demonstrated significant consolidation in the left lung along with a minor presence of pleural effusion on the left side. Additionally, head CT (Figure 2A) exhibited the existence of a right subdural hematoma and subarachnoid hemorrhage. Due to the patient’s worsening dyspnea and persistent high fever, she was subsequently transferred to the emergency department of our hospital.
A physical examination on admission indicated a body temperature of 39.8 °C, a respiratory rate of 35 bpm, a pulse of 138 bpm, fingertip pulse oximetry at 95%, and a storage mask providing 10 L/min oxygen. The patient exhibited clear consciousness and normal responsiveness. Additionally, she had shortness of breath, coarse breath sounds in both lungs, and wet rales could be heard in the left lower lung. The muscle strength of the extremities was normal, and bilateral pathological signs were negative.
After admission, the patient was provided with oxygen therapy, specifically a high-flow nasal cannula (HFNC) delivering oxygen at a concentration of 65%. Additionally, a combination of moxifloxacin and meropenem was administered for anti-infection treatment. Nimodipine was administered to alleviate cerebral vasospasm, and there is no surgical reason for the right subdural hematoma. On day 2 (October 13), the patient’s condition worsened, leading to a decline in fingertip oxygen saturation levels to 87–90%. Consequently, immediate endotracheal intubation was performed. Furthermore, she underwent sputum aspiration through fiber bronchoscopy and extracted bronchoalveolar lavage fluid (BALF) for mNGS examination (DIAN Diagnostics, China). The findings from the post-admission assessment are as follows: arterial blood gas analysis demonstrated a pH of 7.367, PaO2 of 72 mmHg (FiO2: 60%), PaCO2 of 31.5 mmHg, and Lac of 1.9 mmol/L. The PCT level was measured at 5.2 ng/mL, while the levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were recorded at 39 U/L and 81 U/L, respectively. Additionally, the albumin level was determined to be 22.8 g/L, and the creatinine level was measured at 91 umol/L. The results of the mNGS of the BALF indicated the presence of C. psittaci, with a corresponding sequence number of 1111 on day 3 (October 14). Upon further investigation into the patient’s medical history, it was revealed that the individual had slaughtered three ducks 10 days prior to the onset of fever. The patient’s diagnosis of C. psittaci pneumonia was determined through the utilization of clinical characteristics and epidemiological investigation. Consequently, the administration of moxifloxacin and meropenem was ceased, and treatment with doxycycline in combination with piperacillin-tazobactam was initiated on day 3 (October 14). Subsequently, in the afternoon, the patient experienced a drop in fingertip oxygen saturation below 90% (PaO2/FiO2 is 145). Based on the assessment of her oxygenation index, respiratory distress, and imaging findings, she was diagnosed with severe acute respiratory distress syndrome. Following multiple lung recruitments and prone ventilation, there was a notable improvement in her oxygen saturation on day 5 (October 16). A subsequent reexamination of the chest CT demonstrated a worsening of lung consolidation compared to previous findings (Figure 1B), while the absorption of the subdural hematoma in the head was observed (Figure 2B). Additionally, her peak body temperature decreased compared to previous measurements, and there was a continuous decline in inflammatory biomarkers, including WBC, CRP, and PCT (Figures 3 and 4). However, on day 8 (October 19), her body temperature continued to rise repeatedly, and she experienced severe gastric retention. As a result, the administration of doxycycline and piperacillin-tazobactam was ceased, and omadacycline (NUZYRA, Paratek Pharmaceutical, US) was initiated as an alternative anti-infective treatment. Initially, a dosage of 200mg intravenous (IV) once daily was administered, which was subsequently reduced to 100mg IV once daily. After 3 days of treatment, the patient’s clinical condition showed improvement, leading to the successful removal of the endotracheal tube. On day 20 (October 31), the omadacycline injection was transitioned to an oral administration of doxycycline at a dosage of 0.1g orally every 12 hours.
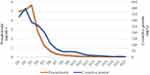 |
Figure 3 Changes of white blood cell count and Neutrophil predominance during hospitalization. |
 |
Figure 4 Changes of Procalcitonin and C-reactive protein during hospitalization. |
Following extubation, the patient promptly experienced stridor and respiratory distress, which were subsequently alleviated through the administration of repeated epinephrine nebulization and intravenous dexamethasone. On day 10 (October 21), the patient presented with symmetrical limb weakness, dysarthria, and a coughing episode following water ingestion. Physical examination revealed a level 2 upper limb strength, level 1 lower limb strength, tendon hyporeflexia, slurred speech, impaired cheek pouching, and diminished pharyngeal reflex. On day 14 (October 25th), the patient underwent a series of diagnostic procedures, including a lumbar puncture, electromyography, and magnetic resonance imaging, with the aim of excluding potential pathologies associated with muscle weakness, such as intracranial infections, cerebral infarction, and myelopathy, among others. There were no obvious abnormalities in brain and cervical magnetic resonance imaging. Analysis of the cerebrospinal fluid (CSF) demonstrated protein levels of 40.7 mg/dl and a white blood cell count of 1/ul. The presence of partial peripheral nerve damage, motor and sensory involvement, and prominent axonal damage was detected through an electromyogram. When considering the patient’s clinical manifestations, electromyogram findings, cerebrospinal fluid results, and the expert opinions of neurologists, a diagnosis of secondary GBS was established.
Following the implementation of nutritional nerve and rehabilitation exercises, a dosage of 20 g (0.4 g·kg−1·d−1) of human immunoglobulin intravenously was administered on day 16 (October 27). After 5 days of immunotherapy, a noticeable improvement in the patient’s muscle strength and mental state was observed. Specifically, the patient exhibited a level 4 distal upper limb muscle strength and a level 3 lower limb muscle strength. Furthermore, the patient exhibited a commanding vocal presence and demonstrated proficiency in constructing coherent sentences. On day 22 (November 2), a chest computed tomography scan (Figure 1C) revealed evident resolution of infection in both lungs. She was transferred to a local rehabilitation hospital for neurological rehabilitation exercises to prevent disuse, muscular atrophy, and joint contracture on day 24 (November 4). Two months after discharge, the patient’s limb muscle strength was level 5.
Discussion
In the past 20 years, several outbreaks of psittacosis in humans have occurred in the United States, Japan, and other countries.7,8 Although the number of reported cases of psittacosis is increasing worldwide, it is still a rare respiratory disease. A meta-analysis revealed that C. psittaci pneumonia constituted approximately 1% of community-acquired pneumonia cases.9 The typical incubation period for C. psittaci pneumonia spans from one to two weeks. Following infection, the systemic system may experience notable impacts, manifesting as temporary flu-like symptoms alongside liver insufficiency and gastrointestinal manifestations such as vomiting, and diarrhea. Additionally, the heart and central nervous system may be subject to involvement, presenting as endocarditis, myocarditis, and encephalitis.2 In this instance, the patient initially suffered from high fever and severe dyspnea, subsequently exhibiting extrapulmonary symptoms including symmetrical limb weakness. Research findings indicate that the majority of patients display either normal or heightened levels of white blood cells and procalcitonin, along with an elevated C-reactive protein.10 In this case, the initial observation revealed elevated levels of the patient’s white blood cells, CRP, PCT. Subsequently, following the administration of anti-infection treatment, a reduction in these inflammatory markers was observed. However, on the 8th day, a subsequent increase in white blood cell count occurred, potentially attributable to the patient’s dysphagia, ultimately resulting in the development of aspiration pneumonia.
Chlamydia psittaci is an intracellular parasite that poses challenges in its detection through conventional cultures.11 Moreover, these conventional methods are time-consuming and need to be equipped with P3 experimental facilities. In contrast, mNGS serves as a highly efficient detection technique capable of identifying intricate and unforeseeable pathogens within a brief timeframe.12 Furthermore, the utilization of antibiotics minimally affects the detection rate of these pathogens and has gained widespread adoption in clinical settings.13 No pathogenic bacteria were found in our patient’s routine culture, but C. psittaci was detected within 24 hours through mNGS. This finding highlights the utility of mNGS analysis of alveolar lavage fluid in identifying the causative agent of pneumonia cases with unknown etiology.
The preferred treatment for psittacosis is tetracyclines, and other effective drugs include macrolides and quinolones for at least 2 weeks.14 This patient was treated with moxifloxacin after admission, but the efficacy was not significant, which may be related to the low intracellular activity of quinolones in C. psittaci.15 Currently, the resistance rate of macrolides is increasing exponentially, and it was reported that macrolides had poor therapeutic effects on severe C. psittaci pneumonia and generally require the combination of other drugs.16 The gastrointestinal tract is considered a vulnerable organ within the human body due to its heightened susceptibility to damage and comparatively slower rate of recuperation when compared to other organs. In a prior study,17 4 patients (a total of 13 cases) with severe C. psittaci pneumonia made a full recovery after treatment with tetracyclines. As we all know, doxycycline is only available in oral preparations in most hospitals, which are insufficiently absorbed in severe patients with poor gastrointestinal function. After the diagnosis of psittacosis, our patient underwent treatment with nasal feedings of doxycyclin. However, this patient suffered from profound gastric retention at the time, and had intermittent high fever, which may be related to the low drug absorption and utilization rate caused by the administration method.
Omadacycline, a novel class of tetracycline medications, is accessible in oral and intravenous formulations. Initially employed for the treatment of acute bacterial skin infections and community-acquired bacterial pneumonia,5 it has been shown to exhibit favorable antibacterial efficacy against chlamydia, surpassing that of doxycycline.18 Furthermore, there is no need to adjust the dosage of omadacycline in patients with liver and kidney insufficiency.19 There were limited instances of omadacycline utilization for the management of psittacosis. Fang et al reported a patient with severe C. psittaci pneumonia complicated with multiple organ failure who improved after treatment with omadacycline.6 Liu et al also reported a case of successful treatment of severe C. psittaci pneumonia with awake prone ventilation combined with omadacycline.20 The aforementioned reports have demonstrated that omadacycline exhibits favorable antibacterial efficacy against C. psittaci, rendering it a promising therapeutic option for severe cases of C. psittaci pneumonia, particularly among elderly individuals with multiple organ dysfunction. In this study, patients experienced a normalization of body temperature within 24 hours of commencing omadacycline treatment, and after a duration of 12 days, chest CT scans revealed substantial resolution of lung consolidation. After discharge, there was no recurrence. Whether omadacycline gets a jump on other traditional drugs in critical patient needs further a quantity of clinical researches.
GBS is an infrequent extrapulmonary manifestation of C. psittaci infection, with numerous microorganisms being linked to GBS, notably Campylobacter jejuni, followed by the Epstein-Barr virus and cytomegalovirus.21 However, C. psittaci is an uncommon pathogen that exhibits a close association with GBS. In this particular case, despite the infection being effectively managed, there has been a progressive escalation in limb weakness. Consequently, the patient has been reliant on rehabilitative exercises to facilitate limb movement for an extended duration. Fang et al reported the first case of C. psittaci pneumonia combined with GBS, whose clinical symptoms was consistent with our patient.22 By incorporating cervical spine, head MRI, and CSF culture, potential confounding factors such as myelitis, acute cerebral infarction, and intensive care-unit acquired weakness (ICU-AW) were ruled out. Therefore, the patient was clinical diagnosed with GBS. Nevertheless, the pathogenesis of C. psittaci pneumonia complicated with GBS is still unclear. Certain scholars posit that certain elements of C. psittaci bear resemblance to peripheral nerve tissue, thereby causing the immune system to erroneously identify them and subsequently mount an immune response against peripheral nerves. This immune response ultimately results in the demyelination and/or axonal impairment of peripheral nerves.21,23 Compared to plasma exchange, the administration of intravenous immunoglobulin (IVIg) is more convenient and yields minimal adverse reactions, rendering it the preferred therapeutic approach for GBS. This patient showed noticeable improvement with the use of IVIg and she was discharged without any complications.
Conclusion
The clinical manifestations of pneumonia caused by C. psittaci are nonspecific and pose challenges in terms of diagnosis. The utilization of mNGS technology enables rapid identification of the pathogen, thereby playing a crucial role in diagnosing cases of community-acquired pneumonia that lack a clear etiology. In instances of pneumonia accompanied by unexplained symmetrical limb weakness, GBS should be considered as a potential underlying condition. Omadacycline, a novel tetracycline antibiotic, exhibits notable efficacy and reliable safety in the treatment of severe C. psittaci pneumonia.
Ethical Statement and Informed Consent
The study was approved by the Ethics Committee of Hangzhou First People’s Hospital, affiliated with the School of Medicine at West Lake University. The patient provided informed consent for publication of this case.
Acknowledgments
The authors would like to thank the neurology specialists for their guidance and the patient’s family for their consent to publication.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Construction Fund of Medical Key Disciplines of Hangzhou (OO20200485), University-Industry Collaborative Education Program (220705078263507) and Zhejiang Provincial Traditional Chinese Medicine Science and Technology Project (2022ZB269).
Disclosure
None of the authors has any conflict of interest.
References
1. Ojeda Rodriguez JA, Modi P, Brady MF. Psittacosis Pneumonia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. PMID: 30252261.
2. Vande Weygaerde Y, Versteele C, Thijs E, et al. An unusual presentation of a case of human psittacosis. Respir Med Case Rep. 2018;23:138–142. doi:10.1016/j.rmcr.2018.01.010
3. Webb S, Wallace VC, Martin-Lopez D, et al. Guillain-Barré syndrome following COVID-19: a newly emerging post-infectious complication. BMJ Case Rep. 2020;13(6):e236182. doi:10.1136/bcr-2020-236182
4. Durães F, Sousa E. Omadacycline: a newly approved antibacterial from the class of tetracyclines. Pharmaceuticals. 2019;12(2):63. doi:10.3390/ph12020063
5. Zhanel GG, Esquivel J, Zelenitsky S, et al. Omadacycline: a novel oral and intravenous aminomethylcycline antibiotic agent. Drugs. 2020;80(3):285–313. doi:10.1007/s40265-020-01257-4
6. Fang C, Xu L, Tan J, Tan H, Lin J, Zhao Z. Omadacycline for the treatment of severe chlamydia psittaci pneumonia complicated with multiple organ failure: a case report. Infect Drug Resist. 2022;15:5831–5838. doi:10.2147/IDR.S384296
7. Shaw KA, Szablewski CM, Kellner S, et al. Psittacosis outbreak among workers at chicken slaughter plants, Virginia and Georgia, USA, 2018. Emerg Infect Dis. 2019;25(11):2143–2145. doi:10.3201/eid2511.190703
8. Matsui T, Nakashima K, Ohyama T, et al. An outbreak of psittacosis in a bird park in Japan. Epidemiol Infect. 2008;136(4):492–495. doi:10.1017/S0950268807008783
9. Hogerwerf L, Gier DE, Baan B, et al. Chlamydia psittaci (psittacosis) as a cause of community-acquired pneumonia: a systematic review and meta-analysis. Epidemiol Infect. 2017;145(15):3096–3105. doi:10.1017/S0950268817002060
10. Shi Y, Chen J, Shi X, et al. A case of chlamydia psittaci caused severe pneumonia and meningitis diagnosed by metagenome next-generation sequencing and clinical analysis: a case report and literature review. BMC Infect Dis. 2021;21(1):621. doi:10.1186/s12879-021-06205-5
11. Yang M, Yang DH, Yang H, et al. Clinical characteristics of chlamydia psittaci pneumonia infection in Central South China. Infect Dis Ther. 2022;11(4):1631–1647. doi:10.1007/s40121-022-00662-4
12. Grumaz S, Stevens P, Grumaz C, et al. Next-generation sequencing diagnostics of bacteremia in septic patients. Genome Med. 2016;8(1):73. doi:10.1186/s13073-016-0326-8
13. Tang J, Tan W, Luo L, et al. Application of metagenomic next-generation sequencing in the diagnosis of pneumonia caused by chlamydia psittaci. Microbiol Spectr. 2022;10(4):e0238421. doi:10.1128/spectrum.02384-21
14. Wang L, Shi Z, Chen W, et al. Extracorporeal membrane oxygenation in severe acute respiratory distress syndrome caused by chlamydia psittaci: a case report and review of the literature. Front Med. 2021;8:731047. doi:10.3389/fmed.2021.731047
15. Cillóniz C, Torres A, Niederman M, et al. Community-acquired pneumonia related to intracellular pathogens. Intensive Care Med. 2016;42(9):1374–1386. doi:10.1007/s00134-016-4394-4
16. Rybarczyk J, Versteele C, Lernout T, et al. Human psittacosis: a review with emphasis on surveillance in Belgium. Acta Clin Belg. 2020;75(1):42–48. doi:10.1080/17843286.2019.1590889
17. Wu HH, Feng LF, Fang SY. Application of metagenomic next-generation sequencing in the diagnosis of severe pneumonia caused by Chlamydia psittaci. BMC Pulm Med. 2021;21(1):300. doi:10.1186/s12890-021-01673-6
18. Karlowsky JA, Steenbergen J, Zhanel GG. Microbiology and preclinical review of omadacycline. Clin Infect Dis. 2019;69(Suppl 1):S6–S15. doi:10.1093/cid/ciz395
19. Chopra T, Sandhu A, Theriault N, et al. Omadacycline: a therapeutic review of use in community-acquired bacterial pneumonia and acute bacterial skin and skin structure infections. Future Microbiol. 2020;15(14):1319–1333. doi:10.2217/fmb-2020-0182
20. Liu X, Yang H, Lai X, et al. A case of severe Chlamydia psittaci pneumonia treat with awake prone position ventilation. Chin Med Case Reposit. 2023:e00334. doi:10.3760/cma.j.cmcr.2023
21. Shahrizaila N, Lehmann HC, Kuwabara S. Guillain-Barré syndrome. Lancet. 2021;397(10280):1214–1228. doi:10.1016/S0140-6736(21)00517-1
22. Fang C, Xu L, Tan J, et al. Case Report: chlamydia psittaci pneumonia complicated by Guillain-Barré syndrome detected using metagenomic next-generation sequencing. Front Cell Infect Microbiol. 2023;12:1070760. doi:10.3389/fcimb.2022.1070760
23. Jasti AK, Selmi C, Sarmiento-Monroy JC, et al. Guillain-Barré syndrome: causes, immunopathogenic mechanisms and treatment. Expert Rev Clin Immunol. 2016;12(11):1175–1189. doi:10.1080/1744666X.2016.1193006
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


