Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Obesity Concerns and the Future of a Nation’s Health: A Cross-Sectional Study of Physical Activity and Related Awareness of Doctors-in-The-Making, Staff, and Faculty in a Saudi Arabian Medical College
Authors Alzahrani HA , Ahmad MT, Alasmari ZS, Aljarallah FA, Hafiz LM, Almasoudi BA, Alibrahim AA, Abd El Maksoud WM , Bawahab MA , Alsaleem MA
Received 14 February 2023
Accepted for publication 29 March 2023
Published 5 April 2023 Volume 2023:16 Pages 951—962
DOI https://doi.org/10.2147/JMDH.S406712
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hassan A Alzahrani,1 Mohammad Tauheed Ahmad,2 Ziyad S Alasmari,3 Fares A Aljarallah,3 Lubna M Hafiz,3 Basim A Almasoudi,3 Ahmad A Alibrahim,3 Walid M Abd El Maksoud,1 Mohammed A Bawahab,1 Mohammed A Alsaleem4
1Department of Surgery, College of Medicine, King Khalid University, Abha, Saudi Arabia; 2Department of Medical Education, College of Medicine, King Khalid University, Abha, Saudi Arabia; 3Medical Student, College of Medicine, King Khalid University, Abha, Saudi Arabia; 4Department of Family and Community Medicine, College of Medicine, King Khalid University, Abha, Saudi Arabia
Correspondence: Hassan A Alzahrani, Department of Surgery, College of Medicine, King Khalid University, P.O. Box 641, Abha, Saudi Arabia, Email [email protected]
Background: Saudi Arabian population has amongst the highest prevalence of obesity globally. Apart from nutritional measures, physical activity is considered a major modifiable risk factor for the prevention of obesity and its consequences. An insight into the physical activity and awareness parameters of healthcare professionals and those in the making can provide an insight into how prepared we are to deal with the epidemic of non-communicable diseases. The aim of this study is to find out about the degree of physical activity undertaken by the medical students, faculty and staff at the College of Medicine, King Khalid University, as well as their awareness regarding physical activity guidelines.
Methods: This study surveyed 300 adult participants - medical students, faculty and staff - in the College of Medicine, King Khalid University. An international validated questionnaire was used to assess the physical activity profile of participants as well as BMI parameters. Moreover, awareness and knowledge of the recommended physical activity guidelines for adults were also assessed.
Results: The study participants comprised around 83% students, 9% faculty members, and 7% staff members. Around 55% of the participants were male, while the rest were female. More than 65% of participants across all categories reported low levels of physical activity, with only about 4.5% of participants across various age groups reporting high levels of physical activity. There was no significant difference by gender across the group (P value = 0.227). Only 17% of the study participants were knowledgeable of the recommended physical activity guidelines for adults.
Conclusion: We found a low level of physical activity as well as inadequate awareness about the physical activity guidelines amongst our study participants. This study reiterates the urgent need for well-researched and well-funded health promoting interventions to promote physical activity, especially in the context of health professions’ education.
Keywords: obesity, overweight, physical activity, physical activity guidelines
Background
Overweight and obesity are a worldwide health issue and physical activity (PA) is a well-known preventive measure, even in individuals with a genetic predisposition to overweight.1 Different estimates have found the highest obesity prevalence in Saudi Arabia at 35.6%, while the global average is around 13%. Moreover, Saudi Arabia has two times the death rate attributable to obesity as compared to the global average.2 It must be reiterated that obesity has taken the form of a pandemic, encompassing almost all countries and populations.3 According to a 2019 estimate, overweight and obesity have been found to cost Saudi Arabia a total of $3.8 billion in direct costs, which is equivalent to 4.3% of total health expenditures in the country.4 The high prevalence of morbid obesity has compelled an increasing number of people to seek bariatric surgery.5 This increase in the prevalence of obesity reflects the magnitude of this health problem that requires urgent attention and a long-term strategy for its control. Also, among the most studied pointers for the burden of non-communicable diseases in a population is metabolic syndrome, which has been estimated in different populations worldwide. Two population-level estimates of metabolic syndrome among the Saudi Arabian population reveal a prevalence amongst the highest in the world.6,7
PA and its positive impact on different dimensions of health and wellness has been conclusively proven. From the impact of PA in improving general wellness to the extent of its role in post-operative recovery, as evidenced by its being a core component of the Enhanced Recovery After Surgery (ERAS) program, to reduce complications and shorten hospital stays following surgery.8 PA improves health and wellness, prevents many causes of premature death, and improves patient outcomes in many surgical procedures, as proved in bariatric surgery.9–11 Overweight and obesity, which in most cases are direct consequences of a lack of PA, are major health problems and have a direct impact on medical costs, which can be estimated from the fact that 5–10% of US health care spending is spent on the management of overweight and obesity.12
The World Health Organization (WHO) and the PA Guidelines for Americans recommend adults do at least 150 minutes to 300 minutes a week of moderate-intensity, or 75 minutes to 150 minutes a week of vigorous-intensity aerobic PA, or an equivalent combination of moderate- and vigorous-intensity aerobic activity.13,14 However, in 2014, a cross-sectional national survey identified that only 36.1% of the adult population reported being aware of government guidelines, and less than 1% correctly identified the moderate-intensity PA guideline (ie, 150 minutes per week).15
Saudi Arabia has one of the highest burdens of non-communicable diseases.16 As stated earlier, very high population estimates of the metabolic syndrome point to a grim picture of the condition of the population’s health. Prevention and control of such population level risk factors require synchronized public health interventions, for which the support of healthcare professionals is critical. Physically active healthcare professionals have been found to be more capable of advising their patients to take care of their health.17 Social accountability in medical education obligates the medical schools to direct their education, research, and service to address the priority health needs of the population.18 With the rapid increase in noncommunicable disease risk factors, medical schools have a greater responsibility to lead prevention and mitigation efforts. Assessing how well healthful behaviors are followed by medical students and doctors is important, as elements of identity formation play a role in molding the doctors-in-the-making as change agents to deal with pressing health problems.19 Hence, we tried to study the state of health of medical students and faculty members pertaining to the PA and related parameters, which are one of the most important determinants of health. The aim of this study was to find out about the kinds of PA that adults who are associated with the College of Medicine at the King Khalid University do as part of their everyday lives. Additionally, we also estimated the proportion of adults from this population who are aware and knowledgeable of the 2018 PA Guidelines.
Methods
Sample Size and Study Population
The required sample size was calculated using the MedCalc statistical software. A previous study carried out by Althumiri et al was used to predict the different measurements in our study.20 The sample size was estimated to be at least 290 subjects in this study. The estimated sample size was made under the assumption of a 95% confidence level and a power of 90%.
We included currently enrolled students as well as faculty members and staff of the College of Medicine at King Khalid University, Abha. A total of 300 completed questionnaires were collected. Participants included in the study were between 18 and 65 years old and provided appropriate consent. To address the issue of vulnerability in our study populations, the questionnaire was anonymous and voluntary. The participants had the right to refuse participation in the study at any stage without penalty. Those faculty and students associated with this study were excluded. Faculty members from the department of family and community medicine were also excluded from the survey, as they are supposed to have a greater awareness of health promotion topics.
Ethical Consideration
Declaration of Helsinki ethical principles were followed in the conduct of this study. Institutional review board of King Khalid University approved the research (ECM #2022-3008). A consent form was attached to elicit the permission of the participants prior to registering their responses.
Study Design
The questionnaires were compiled using Google Form software, and a computer-assisted personal interview (CAPI) survey was adopted for the data collection.
Using a web-based survey offers several advantages, including reduced response time and a low cost of the research as compared with other survey modes.21 Additionally, even measurement errors will be reduced, as the data were spontaneously transferred from the web-based survey into a data file that opens directly into the statistical analysis software rather than being manually entered.22
The questionnaire had three sections. The first section included questions about background factors such as age, gender, height, and weight. The second section included the International Physical Activity Questionnaire (IPAQ), which is a reliable and validated measure, designed in collaboration with top public health agencies such as the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC) and used internationally for such studies.23,24 It is designed for a population group aged between 15 and 65 years and can be used to collect responses either by self-administration or via interview. There are two versions of the IPAQ questionnaire: a short (7-item) and a long (27-item) version. We used the short version that asks about their time spent being physically active in the previous 7 days and includes seven items on four domains: (1) during transportation, (2) at work, (3) during household and gardening tasks, and (4) during leisure time. This version sufficiently serves the objective of this research (Supplementary file). The questionnaire is available in different languages for free download for research purposes (https://sites.google.com/view/ipaq).
In the third section, we assessed the awareness and adherence of participants to the 2018 PA Guidelines. We adopted a questionnaire used in a similar cross-sectional national survey.15 Participants’ awareness was assessed by asking the following: “Have you seen, heard, or read anything about PA guidelines in the last year?” Response options included yes, no, or not sure.
The knowledge was assessed by asking the following: Identify “the minimum amount of moderate-intensity PA the guidelines recommend for adults to get substantial health benefits.” The respondents could choose from the six provided responses: i) 20 minutes a day, 3 or more days a week; ii) 100 minutes spread out over a week; iii) 30 minutes a day, 5 or more days a week; iv) 150 minutes spread out over a week; v) 60 minutes, 7 days a week; vi) Do not know/not sure. As per the guidelines, any respondent who marks “150 minutes spread out over a week” will be categorized as knowledgeable of the moderate-intensity PA guidelines as specified in the 2018 Guidelines. The PA guidelines recommend adults do at least 150 to 300 minutes of moderate-intensity PA over a week’s time, or 75 to 150 minutes of vigorous-intensity aerobic PA over a week’s time, or an equivalent combination of moderate- and vigorous-intensity aerobic activity.16
Data Analysis
The data were collected, reviewed and then fed to Statistical Package for Social Sciences version 21 (SPSS: An IBM CompanyTM). All statistical methods were two-tailed with an alpha level of 0.05, and a P value less than or equal to 0.05 was considered significant. The IPAQ scoring protocol was adopted to categorize PA into low (below 600 MET-min/week), moderate (600–1499 MET-min/week), and high (above 1500 MET-min/week) levels over the previous 7 days (Supplementary file). Descriptive analysis was done by prescribing frequency distribution and percentage for study variables including participants bio-demographic data, PA awareness and knowledge of PA guidelines. Cross-tabulation for showing the distribution of participants’ overall PA level by their personal data and their knowledge regarding PA guidelines using Pearson chi-square test for significance and exact probability test if there were small frequency distributions.
Results
A total of 300 participants completed the study questionnaire, 250 (83.3%) were students, 28 (9.3%) were faculty staff, and 22 (7.3%) were staff members. Of the students, a total of 108 (43.4%) were at level 6 or below and 141 (56.6%) were at level 7 or above. Participants ages ranged from 18 to 65 years with a mean age of 23.9 ± 14.8 years. Around 55% of the participants were male and the rest were female. Around 30% of the participants were classified as overweight and around 17% as obese (Table 1).
 |
Table 1 Personal Data of Study Participants |
Table 2 shows that 46.3% of the study participants reported that “During the last 7 days, they did vigorous physical activities like carrying light loads, bicycling at a regular pace, or doubles tennis” with an average duration of 26.4 ± 36.6 minutes per day. Also, 63.3% of participants reported that “During the last 7 days, they did moderate physical activities like carrying light loads, bicycling at a regular pace, or doubles tennis” with an average duration of 30 ± 39 minutes per day. Additionally, 95% of the study participants walked for at least 10 minutes daily, while the average hours spent on a weekday were 2.41 ±1.02 hours.
 |
Table 2 Physical Activity Among Study Participants |
Figure 1 shows the overall level of PA among study participants based on the IPAQ scoring protocol. Around 65% of the participants had an overall low level of PA, while 89 (29.7%) performed moderate activity and 14 (4.7%) had an overall high PA level.
 |
Figure 1 Level of physical activity among study participants, based on the international physical activity questionnaire scoring protocol. |
In our study, we found that around 31% of participants had seen, heard, or read anything about PA guidelines in the last year. Regarding the minimum amount of moderate-intensity PA, 51 (17%) reported (correctly) PA for 150 minutes spread out over a week, 106 (35.3%) reported doing the same for 30 minutes a day, 5 or more days a week, and 50 (16.7%) for 20 minutes a day, 3 or more days a week while, 73 (24.3%) were not sure (Table 3).
 |
Table 3 Knowledge and Perception of Physical Activity Guidelines, Among Study Participants |
By studying the distribution of PA level among our participants, we found that around 10% of participants aged 46–65 years performed high-level of PA versus 4.5% of others aged 18–25 years with no statistical significance (P=0.921). Furthermore, 38.5% of males performed moderate to high PA compared to 29.1% of females (P=0.227). Moderate to high PA was reported by 37.3% of normal weighted participants in comparison to 22% of the obese group (P=0.360). Additionally, 50% of staff members performed moderate to high PA compared to 33% of students (P=0.563). The PA profile was also examined with respect to the BMI of the participants. Moderate and high levels of PA were lower in the obese and overweight groups as compared to the normal weight groups. However, this difference was not found to be significant (Table 4).
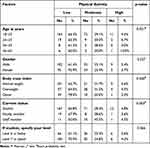 |
Table 4 Distribution of Physical Activity Level Among Study Participants by Their Personal Data |
Distribution of PA level among study participants by their knowledge and perception of PA guidelines. Exact of 28.2% of participants who saw, heard, or read anything about PA guidelines in the last year performed moderate to high PA versus 38.9% of others who did not (P=0.429). Also, 45.1% of participants knowledgeable regarding moderate-intensity PA guidelines performed moderate to high PA compared to 32.4% of others with recorded statistical significance (P=0.049) (Table 5).
 |
Table 5 Distribution of Physical Activity Level Among Study Participants by Their Knowledge and Perception of Physical Activity Guidelines |
Discussion
Saudi Arabia has one of the highest prevalences of obesity, as well as the morbidity and mortality associated with obesity.2 Obesity affects the quality of life of individuals and being a risk factor for many serious chronic illnesses adds substantially to the burden of healthcare expenditure.25 Likewise, Saudi Arabia has amongst the highest burdens of non-communicable diseases as evidenced from different estimates, especially the high prevalence of metabolic syndrome recorded amongst the Saudi Arabian population over the past two to three decades as evidenced from two estimates published in 2005 and 2018.6,7 Metabolic syndrome is a clustering of conditions that predispose an individual to cardiovascular morbidity and mortality. Based on the consensus of experts, three of five risk factors - abdominal obesity, elevated triglycerides, reduced high-density lipoprotein cholesterol, elevated blood pressure, and elevated fasting glucose - constitute a diagnosis of metabolic syndrome.26 PA has been recommended as one of the most important routine measures for physical fitness and weigh control, and the various dimensions of the health benefits of PA for all age-groups are undebatable. Adequate levels of PA can lead to substantial risk reduction for more than 25 common chronic diseases, as well as premature mortality.27 Promoting PA amongst all sections of the population has been an important component of disease prevention and health promotion in the past decades. Right from organizing marathons to observing special days to promote PA28 and the recent emergence of mobile applications29 to estimate and promote PA, there appears to be a sustained interest in promoting PA at the government and civil society levels even as the overall levels of PA at the individual levels as well the chronic diseases linked to lack of PA continue to rise.30 Promoting PA amongst students at the school and college levels has been one of the primary modes of developing this essential habit amongst a vital subset of the population. Promoting PA in educational institutions has been recommended and has a lot of advantages. Apart from developing positive habits toward the prevention of chronic illness, PA has the advantage of promoting mental well-being and efficiency of learning.31,32 In a study of medical students in Saudi Arabia, PA was linked to better academic performance.33 Such a correlation between PA and academic performance has been reported in other studies as well.34–37
Given the vital importance of PA and the significance of the role doctors’ and healthcare professionals’ advice in health promotion amongst patients, it is important that the medical students and medical college faculty are themselves practicing healthy behaviors.38 In this context, we have included medical students and faculty members in our survey. A total of 300 participants completed the study questionnaire, out of which 250 (83.3%) were students, 28 (9.3%) were faculty members, and 22 (7.3%) were staff members. We sought a representative mix of beginning and senior medical students based on their clinical exposure as well as years of familiarity with medicine topics and health promotion. We divided the students into two groups- level 6 and below (up to 3 years of medical schooling) and above level 6 (over 3 years of medical schooling). A total of 108 (43.4%) were at level 6 or below and 141 (56.6%) were at level 7 or above. Participants’ age ranged from 18 to 65 years, with a mean age of 23.9 ± 14.8 years. The survey comprised of 166 males (55.3%) and remaining females. As per the self-report, 89 (29.7%) of the respondents could be classified as overweight, while 50 (16.7%) were classified as obese, which was higher as compared to most other similar studies. Collectively, over 46% of the respondents reported being obese or overweight. In a study of 6773 university students from 22 countries, the prevalence of obesity or overweight was 22%.39 While, in a survey of 610 university students in Jeddah, a total of more than 48% students were found to be obese or over-weight.40 Similar high-levels of obesity/overweight amongst university students (35% to 38%) have been detected in other studies in Saudi Arabia.41,42 Comparable to our study, a higher prevalence of obesity and over-weight (45.2%) was found in a recent survey of medical students in King Abdulaziz University, Jeddah.43 Saudi Arabia has one of the highest rates of over-weight and related chronic conditions globally.44 A high prevalence of obesity/over-weight amongst medical students in Saudi Arabia is a matter of exceptional concern which needs to be addressed urgently.
In our study, around 53% of the respondents reported not taking partin any vigorous activity in their typical week, while only 18.4% reported to be participating in any vigorous activity on 3 or more days of a typical week. In response to the question related to participation in moderate PA, 46.7% reported not participating in any moderate activity in a typical week, while around 21% reported participating in moderate PA on 3 or more days of a typical week. Likewise, on the question asking about the number of days the respondents walked 10 minutes or more per week, 59.7% reported one such instance in a typical week, while 5% reported that they did not walk for 10 minutes even once per week. As per the IPAQ score, 65.7% had a low level of PA while 29.7% had moderate and 4.7% had high PA level. There was no significant difference in PA in different age-groups. More persons amongst the staff members performed moderated to high PA as compared to the students, but this was not found to be statistically significant (P=0.563). Abha, a mountain city in the southwest region, where this study is conducted enjoys a moderate to slightly cold weather all-round the year, with provision of numberless parks and walking tracks, which is quite conducive to any outdoor activity unlike the weather in most other places in Saudi Arabia such as Jeddah, Riyadh or Dammam, etc. In this context, the lack of PA, including walking, assumes greater significance and adds to the seriousness of this public health concern.
Over the past 2–3 decades, several studies and estimates have reported the level of PA amongst different population groups globally. A WHO document published in 2002 reported physical inactivity among 71% of the youth in Saudi Arabia.45 In another national survey conducted in Saudi Arabia in 2005, the overall physical inactivity amongst all age groups was found to be 60.1% for males and 72.9% for females.46 In another study comparing PA and related correlates amongst youth (15–17 years of age) in Al-Ahsa (Saudi Arabia) with two British towns (Birmingham and Coventry), physical inactivity was reported in 34.5% of males and 81.4% of the females amongst the studied Saudi Arabian population, which was 6–8 times higher as compared to the studied British youth.47 Some of the recent studies also point to a very high prevalence of inactivity amongst all age-groups, especially youth in Saudi Arabia.48 A similar study comparing physical inactivity amongst Saudi Arabian and Egyptian medical students found that physical inactivity was much higher among Saudi Arabian medical students (41%) as compared to Egyptian medical students (15.4%).49 Another study compared in Malaysia compared the levels of physical inactivity amongst medical students versus non-medical students, reporting that physical inactivity was more common amongst medical students vs non-medical students (49% vs 35%).50 In the Saudi Arabian context, with a high burden of non-communicable diseases and risk factors, physical inactivity, especially amongst medical students and faculty, is a matter of serious concern, which needs to be studied in more detail and addressed urgently. Promoting participation in sporting events and raising the awareness of youth and students from a health promotion point of view is urgently needed. For better health promotion at the population level, it is important that medical students and doctors are sensitized to this important issue.
As our study participants were medical students and faculty, we also tried to elicit responses regarding the study participants’ awareness of PA guidelines. Around 30% of the participants reported having seen, heard, or read about PA guidelines. When further asked to identify the correct duration of the minimum recommended amount of moderate-intensity PA, 17% answered, correctly choosing the option, “150 minutes spread out over a week”. This was higher as compared to other such studies. In a survey of medical students of Delhi, India, 9.3% of the students correctly stated the recommended duration of PA.51 Also, in a survey of National Health Service doctors in UK, around 13% of the doctors were able correctly state the recommended duration.52 This could be because of the style of question as in both the studies in Delhi and UK, open-ended questions were asked regarding this query, while in our study we asked this question in a multiple-choice format. A study of primary health care physicians in Jeddah, published in 2006 and cited in the paper by Alahmed and Lobelo53 points to a low awareness amongst the studied physicians regarding PA guidelines.
Though there was a positive correlation between knowledge about PA guidelines and PA, this association was not found to be significant (Table 5). This could be in part because of the multiple-choice format in which the question about PA guidelines was asked in our survey and many of the correct answers could be just a random guess. Moreover, PA as with any other health promoting behavior, is influenced by several factors and plain knowledge may not have a big role to play as exemplified in the high rates of unhealthy behaviors amongst doctors and medical students reported in different studies across the world.
One of the strengths of this study is that it was conducted amongst participants at a medical college located in Abha, which is a hill town with weather conducive to outdoor activities such as walking and sports all round the year. This is a rarity in Saudi Arabia, which has mostly extremely hot weather during a greater part of any year. Abha also has good public facilities for sports and walking. Hence, a deficiency in physical activity amongst the participants is even more alarming.
This study has some limitations. First, the results were based on a CAPI, which may have increased the chance of selection bias or interviewer bias. Second, our study was conducted at a single center, which might make the results less generalizable. Lastly, in our survey, we did not make any assessment of the nutritional profile of the participants, which is an important determinant of overweight and obesity apart from physical activity.
Conclusions
In our study, more than 46% of the respondents were classified as obese or overweight as per the body weight and height information provided by them. Though this prevalence is high as compared to other countries, it is comparable to other similar studies within Saudi Arabia in the past 2–3 decades. A deficient level of PA as well as lack of awareness regarding the PA guidelines amongst the medical students and staff points to a deficiency in addressing preventive medicine and health promotion topics. This study reiterates the urgent need for well-researched and well-funded health promoting interventions to close the competency gap in education and promote PA, especially amongst health professions students and practitioners, to combat the obesity problem in Saudi Arabia.
Data Sharing Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The research was performed in accordance with the Helsinki Declaration of 1964 and subsequent amendments and approved by the research ethics committee of King Khalid University (ECM#2022-3008). Informed consent was obtained from all participants prior to enrollment.
Acknowledgments
We would like to thank Dr. Shehata F. Shehata for his efforts in the data analysis and Prof. Ahmed Mahfouz for editing the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors extend their appreciation to the Deanship of Scientific Research at King Khalid University for funding this work through Small Research Groups under grant number (RGP.1/62/43).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mustelin L, Silventoinen K, Pietiläinen K, Rissanen A, Kaprio J. Physical activity reduces the influence of genetic effects on BMI and waist circumference: a study in young adult twins. Int J Obes. 2009;33(1):29–36. doi:10.1038/ijo.2008.258
2. Salem V, AlHusseini N, Abdul Razack HI, Naoum A, Sims OT, Alqahtani SA. Prevalence, risk factors, and interventions for obesity in Saudi Arabia: a systematic review. Obes Rev. 2022;23(7):e13448. doi:10.1111/obr.13448
3. Meldrum DR, Morris MA, Gambone JC. Obesity pandemic: causes, consequences, and solutions—but do we have the will? Fertil Steril. 2017;107(4):833–839. doi:10.1016/j.fertnstert.2017.02.104
4. Malkin JD, Baid D, Alsukait RF, et al. The economic burden of overweight and obesity in Saudi Arabia. PLoS One. 2022;17(3):e0264993. doi:10.1371/journal.pone.0264993
5. Inocian EP, Nolfi DA, Felicilda-Reynaldo RF, Bodrick MM, Aldohayan A, Kalarchian MA. Bariatric surgery in the Middle East and North Africa: narrative review with focus on culture-specific considerations. Surg Obes Relat Dis. 2021;17(11):1933–1941. doi:10.1016/j.soard.2021.06.015
6. Al-Nozha M, Al-Khadra A, Arafah MR, et al. Metabolic syndrome in Saudi Arabia. Saudi Med J. 2005;26(12):1918–1925. PMID: 16380773.
7. Al-Rubeaan K, Bawazeer N, Al Farsi Y, et al. Prevalence of metabolic syndrome in Saudi Arabia-a cross sectional study. BMC Endocr Disord. 2018;18:1–9. doi:10.1186/s12902-018-0244-4
8. Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606–617. doi:10.1093/bja/78.5.606
9. Bond DS, Vithiananthan S, Thomas JG, et al. Bari-active: a randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surg Obes Relat Dis. 2015;11(1):169–177. doi:10.1016/j.soard.2014.07.010
10. Bond DS, Thomas JG, Vithiananthan S, et al. Intervention-related increases in preoperative physical activity are maintained 6-months after bariatric surgery: results from the bari-active trial. Int J Obes. 2017;41(3):467–470. doi:10.1038/ijo.2016.237
11. Marcon ER, Baglioni S, Bittencourt L, Lopes CL, Neumann CR, Trindade MR. What is the best treatment before bariatric surgery? Exercise, exercise and group therapy, or conventional waiting: a randomized controlled trial. Obes Surg. 2017;27(3):763–773. doi:10.1007/s11695-016-2365-z
12. Tsai AG, Williamson DF, Glick HA. Direct medical cost of overweight and obesity in the USA: a quantitative systematic review. Obes Rev. 2011;12(1):50–61. doi:10.1111/j.1467-789X.2009.00708.x
13. World Health Organization T. Global Recommendations on Physical Activity for Health. World Health Organization; 2010.
14. Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. doi:10.1001/jama.2018.14854
15. Kay MC, Carroll DD, Carlson SA, Fulton JE. Awareness and knowledge of the 2008 physical activity guidelines for Americans. J Phys Act Health. 2014;11(4):693–698. doi:10.1123/jpah.2012-0171
16. Hazazi A, Wilson A. Noncommunicable diseases and health system responses in Saudi Arabia: focus on policies and strategies. A qualitative study. Health Res Policy Syst. 2022;20(1):63. doi:10.1186/s12961-022-00872-9
17. Lobelo F, de Quevedo IG. The evidence in support of physicians and health care providers as physical activity role models. Am J Lifestyle Med. 2016;10(1):36–52. doi:10.1177/1559827613520120
18. Boelen C, Dharamsi S, Gibbs T. The social accountability of medical schools and its indicators. Educ Health. 2012;25(3):180. doi:10.4103/1357-6283.109785
19. McDermott C, Shank K, Shervinskie C, Gonzalo JD. Developing a professional identity as a change agent early in medical school: the students’ voice. J Gen Intern Med. 2019;34(5):750–753. doi:10.1007/s11606-019-04873-3
20. Althumiri NA, Basyouni MH, AlMousa N, et al. Obesity in Saudi Arabia in 2020: prevalence, distribution, and its current association with various health conditions. Healthcare. 2021;9(3):311. doi:10.3390/healthcare9030311
21. Berrens RP, Bohara AK, Jenkins-Smith H, Silva C, Weimer DL. The advent of internet surveys for political research: a comparison of telephone and internet samples. Polit Anal. 2003;11(1):1–22. doi:10.1093/pan/11.1.1
22. Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Questions and answers in surveys. In: Survey Methodology. New Jersey: John Wiley and Sons; 2004:201–213.
23. Booth M. Assessment of physical activity: an international perspective. Res Q Exerc Sport. 2000;71(sup2):114–120. doi:10.1080/02701367.2000.11082794
24. Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB
25. Warburton DE, Bredin SS. Reflections on physical activity and health: what should we recommend? Can J Cardiol. 2016;32(4):495–504. doi:10.1016/j.cjca.2016.01.024
26. Bahijri SM, Al Raddadi RM. The importance of local criteria in the diagnosis of metabolic syndrome in Saudi Arabia. Ther Adv Endocrinol Metab. 2013;4(2):51–59. doi:10.1177/2042018813483165
27. Powers KA, Rehrig ST, Jones DB. Financial impact of obesity and bariatric surgery. Med Clin North Am. 2007;91(3):321–338. doi:10.1016/j.mcna.2007.01.001
28. Bauman A, Murphy N, Lane A. The role of community programmes and mass events in promoting physical activity to patients. Br J Sports Med. 2009;43(1):44–46. doi:10.1136/bjsm.2008.054189
29. Coughlin SS, Whitehead M, Sheats JQ, Mastromonico J, Smith S. A review of smartphone applications for promoting physical activity. Jacobs J Community Med. 2016;2(1):1. PMCID: PMC4811195.
30. Ozemek C, Lavie CJ, Rognmo Ø. Global physical activity levels-need for intervention. Prog Cardiovasc Dis. 2019;62(2):102–107. doi:10.1016/j.pcad.2019.02.004
31. Lapa TY. Physical activity levels and psychological well-being: a case study of university students. Procedia Soc Behav Sci. 2015;186:739–743. doi:10.1016/j.sbspro.2015.04.122
32. Erwin H, Fedewa A, Beighle A, Ahn S. A quantitative review of physical activity, health, and learning outcomes associated with classroom-based physical activity interventions. J Appl Sch Psychol. 2012;28(1):14–36. doi:10.1080/15377903.2012.643755
33. Al-Drees A, Abdulghani H, Irshad M, et al. Physical activity and academic achievement among the medical students: a cross-sectional study. Med Teach. 2016;38(sup1):S66–S72. doi:10.3109/0142159X.2016.1142516
34. Nayak SB, Miranda SA, Bin Fitzrol OJ, Anthony L, Gowrish SR, Aithal AP. The impact of physical activities on the academic performance of medical students. Online J Health Allied Sci. 2016;15(2):1–5.
35. Jose J, Sruthi MV. Role of physical activity on mental health and academic performance among medical students: a cross-sectional study. Int J Community Med Public Health. 2019;6(11):4789–4793. doi:10.18203/2394-6040.ijcmph20195056
36. Hou Y, Mei G, Liu Y, Xu W. Physical fitness with regular lifestyle is positively related to academic performance among Chinese medical and dental students. Biomed Res Int. 2020;2020:1–10. doi:10.1155/2020/5602395
37. Satti MZ, Khan TM, Azhar MJ, et al. Association of physical activity and sleep quality with academic performance among fourth-year MBBS students of Rawalpindi Medical University. Cureus. 2019;11(7). doi:10.7759/cureus.5086
38. Carlos S, Rico-Campà A, de la Fuente-Arrillaga C, et al. Do healthy doctors deliver better messages of health promotion to their patients? Data from the SUN cohort study. Eur J Public Health. 2020;30(3):438–444. doi:10.1093/eurpub/ckaa019
39. Peltzer K, Pengpid S, Samuels TA, et al. Prevalence of overweight/obesity and its associated factors among university students from 22 countries. Int J Environ Res Public Health. 2014;11(7):7425–7441. doi:10.3390/ijerph110707425
40. Baig M, Gazzaz ZJ, Gari MA, et al. Prevalence of obesity and hypertension among University students’ and their knowledge and attitude towards risk factors of Cardiovascular Disease (CVD) in Jeddah, Saudi Arabia. Pak J Med Sci. 2015;31(4):816. doi:10.12669/pjms.314.7953
41. Al-Rethaiaa AS, Fahmy AE, Al-Shwaiyat NM. Obesity and eating habits among college students in Saudi Arabia: a cross sectional study. Nutr J. 2010;9(1):1. doi:10.1186/1475-2891-9-39
42. Syed NK, Syed MH, Meraya AM, et al. The association of dietary behaviors and practices with overweight and obesity parameters among Saudi university students. PLoS One. 2020;15(9):e0238458. doi:10.1371/journal.pone.0238458
43. Alzahrani SH, Malik AA, Bashawri J, et al. Health-promoting lifestyle profile and associated factors among medical students in a Saudi university. SAGE Open Med. 2019;7:2050312119838426. doi:10.1177/2050312119838426
44. DeNicola E, Aburizaiza OS, Siddique A, Khwaja H, Carpenter DO. Obesity and public health in the Kingdom of Saudi Arabia. Rev Environ Health. 2015;30(3):191–205. doi:10.1515/reveh-2015-0008
45. World Health Organization. The World Health Report 2002: Reducing Risks, Promoting Healthy Life. World Health Organization; 2002.
46. Al-Zalabani AH, Al-Hamdan NA, Saeed AA. The prevalence of physical activity and its socioeconomic correlates in Kingdom of Saudi Arabia: a cross-sectional population-based national survey. J Taibah Univ Med Sci. 2015;10(2):208–215. doi:10.1016/j.jtumed.2014.11.001
47. Al-Nakeeb Y, Lyons M, Collins P, et al. Obesity, physical activity and sedentary behavior amongst British and Saudi youth: a cross-cultural study. Int J Environ Res Public Health. 2012;9(4):1490–1506. doi:10.3390/ijerph9041490
48. Al-Hazzaa HM. Physical inactivity in Saudi Arabia revisited: a systematic review of inactivity prevalence and perceived barriers to active living. Int J Health Sci. 2018;12(6):50.
49. El-Gilany A, El-Masry R. Physical inactivity among Egyptian and Saudi medical students. TAF Prev Med Bull. 2011;10(1):35–44. doi:10.5455/pmb.20101018022143
50. Naim Z, Anwar K, Rahman A, Zuliani N. Physical inactivity among medical and non-medical students: a cross sectional study. Int J Public Health Clin Sci. 2016;3(5):48–58.
51. Anand T, Tanwar S, Kumar R, Meena G, Ingle G. Knowledge, attitude, and level of physical activity among medical undergraduate students in Delhi. Indian J Med Sci. 2011;65(4):133. doi:10.4103/0019-5359.104776
52. Cuthill JA, Shaw M. Questionnaire survey assessing the leisure-time physical activity of hospital doctors and awareness of UK physical activity recommendations. BMJ Open Sport Exerc Med. 2019;5(1):e000534. doi:10.1136/bmjsem-2019-000534
53. Alahmed Z, Lobelo F. Physical activity promotion in Saudi Arabia: a critical role for clinicians and the health care system. J Epidemiol Glob Health. 2018;7:S7–S15. doi:10.1016/j.jegh.2017.10.005
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
