Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Nutritional Status Link with Polioseronegativity Among Children from Poliomyelitis Transmission High-Risk Area of the Democratic Republic of the Congo (DRC)
Authors Mwamba GN , Nzaji MK , Hoff NA, Mukadi PK, Musene KK, Gerber SK, Halbrook M, Sinai C , Fuller T, Numbi OL, Wemakoy EO, Tamfum JJM, Mukadi DN, Mapatano MA, Rimoin AW, Dikassa PSL
Received 25 September 2023
Accepted for publication 8 March 2024
Published 19 March 2024 Volume 2024:17 Pages 1219—1229
DOI https://doi.org/10.2147/JMDH.S437351
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Guillaume N Mwamba,1,2 Michel Kabamba Nzaji,1,2 Nicole A Hoff,3 Patrick K Mukadi,4 Kamy Kaminye Musene,5 Sue K Gerber,6 Megan Halbrook,3 Cyrus Sinai,3 Trevon Fuller,3 Oscar Luboya Numbi,7 Emile Okitolonda Wemakoy,8 Jean Jacques Muyembe Tamfum,4 Dalau Nkamba Mukadi,8 Mala Ali Mapatano,8,9,* Anne W Rimoin,3,* Paul-Samson Lusamba Dikassa8,*
1Department of Public Health, Faculty of Medicine, University of Kamina, Kamina, Democratic Republic of the Congo; 2Expanded Program on Immunization, Ministry of Health, Kinshasa, Democratic Republic of the Congo; 3Department of Epidemiology, UCLA Fielding School of Public Health, Los Angeles, CA, USA; 4National Institute of Biomedical Research (INRB), Ministry of Health, Kinshasa, Democratic Republic of the Congo; 5UCLA-DRC Health Research and Training Program, UCLA-DRC, Kinshasa, Democratic Republic of the Congo; 6Polio Eradication program, The Bill and Melinda Gates Foundation, Seattle, WA, 98109, USA; 7Faculty of Medicine, University of Lubumbashi, Lubumbashi, 1825, Democratic Republic of the Congo; 8Department of Epidemiology and Biostatistics, School of Public Health, University of Kinshasa, Kinshasa, Democratic Republic of the Congo; 9Department of Nutrition, School of Public Health, University of Kinshasa, Kinshasa, Democratic Republic of the Congo
*These authors contributed equally to this work
Correspondence: Nicole A Hoff, Field Director for UCLA-DRC Research Program and Researcher at UCLA Fielding School of Public Health, 5345 Av De la Démocratie (Ex Av. Des huileries), Kinshasa, Democratic Republic of the Congo, Tel +1 (240) 409-0578, Email [email protected] Guillaume N Mwamba, Expanded Program on Immunization, 32 Av De la Justice, Kinshasa-Gombe, Democratic Republic of the Congo, Tel +243817975023, Email [email protected]
Background: Malnutrition is identified as a risk-factor for insufficient polioseroconversion in the context of a vaccine-derived polio virus (VDPV) outbreak prone region. To assess the prevalence of malnutrition and its link to poliovirus insufficient immunity, a cross-sectional household survey was conducted in the regions of Haut- Lomami and Tanganyika, DRC.
Methods: In March 2018, we included 968 healthy children aged 6 to 59 months from eight out of 27 districts. Selection of study locations within these districts was done using a stratified random sampling method, where villages were chosen based on habitat characteristics identified from satellite images. Consent was obtained verbally in the preferred language of the participant (French or Swahili) by interviewers who received specific training for this task. Furthermore, participants contributed a dried blood spot sample, collected via finger prick. To assess malnutrition, we measured height and weight, applying WHO criteria to determine rates of underweight, wasting, and stunting. The assessment of immunity to poliovirus types 1, 2, and 3 through the detection of neutralizing antibodies was carried out at the CDC in Atlanta, USA.
Results: Of the study population, we found 24.7% underweight, 54.8% stunted, and 15.4% wasted. With IC95%, underweight (OR=1.50; [1.11– 2.03]), and the non-administration of vitamin A (OR=1.96; [1.52– 2.54]) were significantly associated with seronegativity to polioserotype 1. Underweight (OR=1.64; [1.20– 2.24]) and the non-administration of vitamin A (OR=1.55; [1.20– 2.01]) were significantly associated with seronegativity to polioserotype 2. Underweight (OR=1.50; [1.11– 2.03]), and the non-administration of vitamin A (OR=1.80. [1.38– 2.35]) were significantly associated with seronegativity to polioserotype 3. Underweight (OR=1.68; IC95% [1.10– 2.57]) and the non-administration of vitamin A (OR=1.82; IC95% [1.30– 2.55]) were significantly associated with seronegativity to all polioserotypes.
Conclusion: This study reveals a significant association between underweight and polioseronegativity in children. In order to reduce vaccine failures in high-risk areas, an integrated approach by vaccination and nutrition programs should be adopted.
Keywords: children, underweight, polioserotype, malnutrition, seronegativity, DRC
Introduction
Malnutrition, mainly in the forms of micronutrient deficiencies, including but not limited to iron, iodine, vitamin A, copper, zinc, and selenium,1,2 remains a major health challenge worldwide, particularly in low- and middle-income countries (LMIC).3,4 This condition not only stands as a direct health issue but also exacerbates other diseases.5 According to the Integrated Food Security Phase Classification (IPC) Report, around 26.4 million individuals in the Democratic Republic of the Congo (DRC) faced severe acute food insecurity in 2022, with poverty, conflicts, and inadequate agricultural output as primary contributors.6,7
Malnutrition significantly influences mortality in children under five, being a direct or indirect factor in over half of the 10.8 million yearly deaths in this age group, particularly due to infectious diseases. In malnourished children, compromised immune functions lead to a heightened risk of severe infections, perpetuating the malnutrition-infection cycle.8
Poliomyelitis, caused by one of three poliovirus serotypes 1(PV1), 2(PV2), and 3(PV3), primarily affecting children under five, is an infectious disease with potentially severe consequences.9 For every 200 cases of polio, only one results in paralytic symptoms, known as Acute Flaccid Paralysis (AFP), with a mortality rate of 5–10% among these paralytic cases.10
Despite WHO’s African Region being declared free from wild poliovirus in 2020 and the DRC achieving polio-free certification in 2015, the country is still to face outbreaks of vaccine-derived polio virus type 2 (cVDPV2) and type 1 (cVDPV1) cases.11
DRC has had cases of polio caused by vaccine-derived polioviruses (VDPVs) documented since 2004.12 Vaccine-derived poliovirus cases have been documented in the DRC since 2004, with significant outbreaks of various types occurring in recent years. The country’s participation in global polio vaccination strategy shifts, such as the 2016 switch to bivalent oral polio vaccine (OPV), aims at enhancing seroconversion rates and reducing disease incidence,13 and some studies suggest that bOPV leads to significantly higher seroconversion for type 1 and type 3, than tOPV.14 Starting from May 2017, the DRC has been facing continuous outbreaks of vaccine-derived polioviruses. The year 2021 saw 29 confirmed cases of cVDPV215, while 2022 witnessed a significant rise with 290 cases of cVDPV2, 86 cases of cVDPV1, and 11 instances where cVDPV2 was detected through environmental surveillance.11
The Multiple Indicator Cluster Surveys (MICS) from 2017 to 2018 revealed that only 35.0% of children under 12 in the DRC were fully vaccinated, with variations across regions; Haut Lomami had a slightly higher rate of 35.7%, while Tanganyika was at 21.2%. Key factors for incomplete vaccination included parental/caregiver lack of awareness (29.0%), time constraints (18.4%), distrust (16.1%), and service delivery issues (28.7%) such as remote health-care facilities, unsuitable scheduling, and economic hurdles. The country’s nutritional status, evaluated through weight, height, and body mass indices, was notably poor, with negative Z-scores indicating widespread undernutrition16. In the Haut-Lomami region, the nutritional assessment indicated Z-scores below the norm: −1.2 for weight relative to age, −1.8 for height relative to age, and −0.2 for body mass relative to height.16 In contrast, the Tanganyika region showed slightly better but still concerning Z-scores: −0.9 for weight relative to age, −1.6 for height relative to age, and a marginal positive score of 0.1 for body mass relative to height, highlighting nutritional challenges in both areas.16
WHO, to provide guidance for polio eradication activities, has recommended OPV seroprevalence surveys,17 evaluate risk of poliovirus outbreaks, and pinpoint where population immunity is lacking. These surveys have been implemented in the DRC,18 Nigeria,19 India,20 Pakistan21, West Africa,22 and Madagascar23 These activities have prompted adjustments in the approaches to eradicating poliomyelitis. Reduced titers of vaccine-specific antibodies and seroconversion rates have been identified in children with severe wasting, but there is still very little information on the low effectiveness of vaccines in countries with a high prevalence of malnutrition.24,25
To assess the prevalence of malnutrition and its link to poliovirus insufficient immunity in the context of a cVDPV outbreak prone area, a cross-sectional study was carried out in two south-eastern regions of the DRC.
Methods
Study Population
In 2018, a community-based, cross-sectional study was conducted in eight districts across the Haut-Lomami and Tanganyika Regions of the DRC, specifically targeting Butumba, Lwamba, Malemba-Nkulu, Mukanga, Ankoro, Kabalo, Kongolo, and Manono.
The methodology of this survey, which aimed to assess various health indicators, follows the protocols outlined by Halbrook in 2020,26 briefly, the eight districts with highest number of cVDPV2 registered and highest mass campaign responses organized were selected. Within each health zone, five villages were selected by stratified random sampling using settlement feature layers derived from satellite imagery. During the second stage, we selected villages using a GIS point methodology with buffers. The clusters (health areas) were randomly selected using ArcGIS software based on two parameters: 1) not being in the same health area and 2) being separated by at least 500 m. Households in which children aged 6 to 59 months reside formed subgroups of these clusters. Overall, 327 households in Haut-Lomami and 641 in Tanganyika were investigated by simple random sampling. All households in the cluster were given the opportunity to be surveyed until the expected sample size was reached. Households that refused to participate were marked as “refused” in the tablet-based questionnaire.
We reserved the concept “healthy child” to the child who does not present specific signs of serious illness (such as lethargy, unconsciousness, and convulsion),27 cough or difficult breathing, dehydration or persistent diarrhea, fever, oedema of both feet, and palmar pallor at the assessment time. Only 968 children fitted this operational definition.
We reserved the definition of a “healthy child” to exclude those with signs of serious illness (such as lethargy, unconsciousness, and convulsion),27 cough or difficult breathing, dehydration or persistent diarrhea, fever, oedema of both feet, and palmar pallor at the assessment time. Only 968 children fitted this operational definition.
Measurement of this variable, carried out by trained personnel, includes clinical observation of danger signs, measuring respiratory rate and taking temperature.
Data Collection and Study Variables
Trained interviewers obtained informed consent and conducted interviews in the preferred language of the participants (either French or Swahili). The questionnaire, administered orally, gathered essential demographic information, work habits, health status, and vaccination records of those who agreed to participate. In this survey, standard equipment was used to perform anthropometry. Height was measured using a wooden stadiometer, weighted using a SECA 874 digital scale and middle upper arm circumference (MUAC) using MUAC tricolor strips.
Using WHO standards, anthropometric measurements (stunting, wasting, and underweight) were assessed using Emergency Nutrition Assessment (ENA) software. Data on health, anthropometry (height, weight), vaccination knowledge, and immunization usage were collected through a tablet-based questionnaire26 which might be linked to various illnesses. Additionally, to aid in data analysis, dried blood spots (DBSs) obtained via finger prick were cataloged with unique barcode numbers linking them to the questionnaire responses.
We utilized both quantitative and qualitative data, including age, gender, marital status, tribal affiliation, education level, religious beliefs, primary occupation, nutritional status, and seroprevalence. Household size was assumed to average six members, based on prior research findings.28
Z-scores were calculated using the Emergency Nutrition Assessment (ENA) software, applying WHO standards for infants and children to define underweight, wasting, and stunting when their respective Z-scores fell below −2 standard deviations from the WHO Child Growth Standards median.
Laboratory Analysis
Tests for neutralizing antibodies against poliovirus types 1 (PV1), 2 (PV2), and 3 (PV3) were performed by the CDC in Atlanta using a specialized microneutralization assay to evaluate the antibodies’ effectiveness in serum samples. Dried blood spots (DBSs) were transported at room temperature and then stored at −20°C until analysis. The methodology for this testing has been detailed in prior publications.29 About 60 µl of serum were extracted from each card for the poliovirus neutralization test that requires a small volume of sample.
The assay involved diluting the eluted DBS, mixing it with a set amount of virus before introducing it to cells susceptible to poliovirus, and then applying a luminescent reagent after 5 days to identify surviving cells, indicating successful virus neutralization. Neutralizing antibody levels were quantified in log2 titers, with a detection range between 2.5 and 10.5 log2. Titers of 3.0 log2 or higher signify a sufficient immunogenic response.26,30
Statistical Analysis
The study used SPSS 23 for data analysis. Prevalence rates of malnutrition were computed, followed by comparisons of frequencies via the Pearson chi-square test, with significance set at p < 0.05. Univariate analysis results were presented as frequency distributions and percentages. Bivariate analysis employed the chi-square test to explore the relationship between nutritional status and seronegativity.
Ethical Considerations
The ethical clearance was given by the ethics committee of University of California, Los Angeles’ Institutional Review Broad (IRB#18-000303), and the Kinshasa School of Public Health (approval letter No: ESP/CE/164/2021), University of Kinshasa, DRC.
Our study complies with the Declaration of Helsinki and verbal informed consent was acceptable and approved by the ethics committees.
Results
Socio-Demographic Characteristics of Participating Parents or Guardians
In the study, 968 parents or guardians took part, with mothers aged 20 to 35 years representing 71.3% of the participants. Additionally, 25.4% of these participants had completed secondary education or attended university. Regarding the age and level of education of the father, the situation is as follows: 57.1% are between 20 and 35 years old; 22.7% attended secondary school or university. Overall, 92.6% of parents reported that they were employed and 35.3% of households reported having less than 7 members. Biological parents represented 92% of those interviewed.96.5% of respondent were Luba tribe (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Participating Parents or Guardians |
Characteristics of the Child
In 60.4% of households there were 2 or fewer children under 5 years old. A total of 968 children were assessed of which 47.1% were female and 52.9% were male. In terms of anthropometry, 44% of the children were 72.5cm or taller, 28% weight 10.5kg or greater, and 67% have an arm circumference of at least 13.5 cm (Table 2).
 |
Table 2 Sociodemographic and Anthropometric Characteristics of the Targeted Child |
Of the enrolled children, 24.7% suffer from being underweight, 54.8% from stunting and 15.4% from wasting (Table 3). In the Haut-Lomami Region, there was a prevalence of 19.3% for underweight, 66.7% for stunting, and 10.4% for wasting, while in Tanganyika the prevalences were as follows: 27 0.5%; 48.7% and 17.9%, respectively (Table 3).
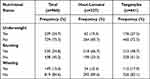 |
Table 3 Prevalence of Malnutrition Among Children 6–59 Months per Province |
Association Between Seronegativity to Polioserotypes and Children Nutritional Status
An association was found between being underweight (OR=1.50; IC95% [1.11–2.03]) and the non-administration of vitamin A supplements (OR=1.96; IC95% [1.52–2.54]) and seronegativity to poliovirus serotype 1. However, no significant correlation was identified between seronegativity to poliovirus serotype 1 and either stunting or wasting.
(Table 4). The association between underweight (OR=1.64; IC95% [1.20–2.24]), and the none-administration of vitamin A (OR=1.55; IC95% [1.20–2.01]) were also significantly noted with seronegativity to polioserotype 2 (Table 4).
 |
Table 4 Seronegativity to Polioserotypes and Nutritional Status of the Child |
We observed a significant association between underweight (OR=1.50; IC95% [1.11–2.03]), and the non-administration of vitamin A (OR=1.80; IC95% [1.38–2.35]) with seronegativity to polioserotype 3 (Table 4). Finally, we observed a significant association between underweight (OR=1.68; IC95% [1.10–2.57]), and the non-administration of vitamin A (OR=1.82; IC95% [1.30–2.55]) with seronegativity to polioserotype in the presence of all polioserotypes (Table 4).
Discussion
Overall, our study revealed a prevalence of 66.7% for stunting, 19.3% for underweight, and 10.4% for wasting in the Haut-Lomami region, and successively of 48.7%, 27.5%, and 17.9%, in Tanganyika Region. Stunting was found to be the most common form of malnutrition, reaching 54.8% of children overall, while one child out of six (15.4%) was considered wasted. The prevalence of underweight represents a quarter of the population studied, with higher rates in Tanganyika Region compared to Haut-Lomami Region. The findings align with the national data from the 2013–2014 Demographic and Health Survey (DHS) of the DRC, which reported that 43% of children under five were stunted, 23% were underweight, and 8% were experiencing wasting,28 as well as the MICS 2017–2018.16
Our results are similar to those of the studies by Luzingu et al in four provinces of the DRC31 and Mbunga et al in children from Popokabaka District in the Kwango Region.
Our study indicates significant association of underweight and non-administration of vitamin A with seronegativity, respectively, to polioserotypes 1, 2, to 3 and in the presence of all three polioserotypes. Studies which explored the association between underweight and polioseronegativity remain very limited with a paucity of recent literature. Our study, describing the same methods, focused on developing and validating a model for predicting polioseronegativity in malnourished children from areas in the Democratic Republic of the Congo where poliomyelitis transmission is highly prevalent, marks a significant contribution to the field.31 Previous studies have examined the causes of the reduced effectiveness of oral vaccines in LIMC without finding a consistent link with malnutrition.24,32–34 Haque et al study is similar to our findings on this single aspect for lower polioserotype 3 antibody titers in Bangladeshi children, they revealed a notable decrease in antibody titers against poliovirus serotype 3 among underweight children (with a weight-for-age Z-score ≤ −2), despite receiving at least three doses of OPV.35,36
Research in India and Pakistan did not identify a correlation between malnutrition and the efficacy of OPV.37–39 Other studies in Bangladesh, Indonesia, and Ghana found that vitamin A supplementation did not markedly influence OPV seroconversion rates.34,40–42
The exact reasons behind these immunological issues remain unclear.43 It has been proposed by some researchers that the disruption is due to insufficient energy and essential amino acids needed for the production of crucial proteins.44 Infections could account for the observed changes, with evidence suggesting a link between infection, malnutrition, and their combined impact on immune responses.45 Even if malnutrition and infections seem to bring many immunological changes, malnutrition appears to be associated with impaired immune system.33
Our study indicated a significant association of the non-administration of vitamin A with seronegativity, respectively, to polioserotype 1, to polioserotype 2, and to polioserotype 3 and in the presence of all three polioserotypes. This association suggests a strong link between nutritional deficiencies and reduced immune response to the polio vaccine. Being underweight may indicate poor nutrition, negatively affecting the immune system’s vaccine response. Vitamin A, essential for immune health, when deficient, can reduce immunity to poliovirus. This highlights the critical role of addressing nutritional shortfalls to boost vaccine effectiveness, especially in high polio risk zones.46 Only one study by James et al in India found that vitamin A supplementation given at 6, 10, and 14 weeks of age modestly enhanced the immune response to the trivalent oral polio vaccine, particularly for the Sabin-1 strain. However, this effect was not deemed significant in further multivariate analysis.47 However, this was not significant in the multivariate analysis.47 However, detection of neutralizing antibody titers is associated with protection against OPV48,49 serum poliovirus IgA assays are necessary for poliovirus infection detection and its control.50–55
Vitamin A has a beneficial effect on immunogenicity especially since it has been proven to increase the number of cytokines and helper T cells. These cells contribute to the differentiation of B cells into cells secreting immunoglobulins.56 However, this effect often appears for antigens, which depend on T-cells.57
While studies revealed an improvement in the immune response to poliovirus when children are supplemented with vitamin A, it is not clear why this benefit was restricted only to type 1 poliovirus in the study conducted by James et al.47
In contrast to the findings of James et al, the study from Indonesia observed a notably higher percentage of children in the placebo group who had antibody titers exceeding 90% for all three poliovirus types.41 The literature review showed that low antibody titer58,59 in infant who received three doses of OPV would not be associated with a weak immune response of the vaccine.60
Our study contributes to the existing knowledge regarding the association between underweight status and polioseronegativity and highlights the potential value of incorporating weight assessment into routine vaccination sessions to improve our understanding of OPV-related seroconversion. By identifying underweight children, health-care providers can provide counseling and additional information to caregivers on how to improve the child’s weight, which could in turn improve their response to polio vaccination. Vitamin A supplementation has been shown to be a significant intervention for improving polioseroconversion in association with improved weight for age. Vitamin A insufficiency along with protein-energy malnutrition, iron deficiency, and anemia.61 Supplementation with these essential nutrients has been found to significantly improve specific antibody responses.62
This study provides evidence to suggest that eradicating all three types of malnutrition in children under five may not be necessary to improve polio seroconversion, as proposed by Habyarimana.63 Instead, targeting a single type of malnutrition, specifically underweight, which affects approximately a quarter of children in the studied population, may be a cost-effective approach to enhance immunogenicity against polio and promote overall child health. Such an approach could have important implications for public health programs aimed at improving child immunization coverage and reducing the burden of vaccine-preventable diseases.
Maintaining high herd immunity against WPV is crucial for achieving global eradication of poliomyelitis. The effectiveness of OPV varies from one area to another depending on living conditions. Malnutrition has been linked to reduced immunogenicity to poliovirus.
Our study has some limitations. The design of the cross-sectional study limits our ability to deduce the exact reasons for the variations in seroconversion rates. Laboratory methods we used did not allow us to know whether the neutralizing antibodies are of vaccine or infectious origin. Several vaccination campaigns in response to cVDPV2 epidemics could negatively influence our findings. Insufficient vaccination cards possessed by 13.1% of participants did not facilitate an in-depth analysis. Only children accompanied by their parents or guardians at the time of sample collection constituted our study population, which may have unintentionally biased our sample and underestimated the target population. Finally, information such as hemoglobin levels, serum retinol levels, place of birth, and early life disease history was not collected.
Our research outcomes have important clinical relevance. They suggest that ensuring adequate nutritional status, particularly regarding weight and vitamin A levels, is crucial for effective immunization against polio.64 This emphasizes the need for integrated health strategies that combine vaccination programs with nutritional support, especially in areas where polio is a risk.61 Health-care providers should be aware of the potential impact of malnutrition on vaccine efficacy and consider nutritional assessment and intervention as part of immunization campaigns. This approach could improve vaccine response rates and ultimately contribute to more effective control of polio.
Conclusion
The results of our research highlight a notable link underweight-polioseronegativity among children under five. In high-risk regions, a comprehensive approach that incorporates both vaccination and nutrition programs may be necessary to address vaccine failures and enhance immunogenicity against all polioserotypes. In undernourished settings, weight gain tailored to the age of children, in conjunction with vitamin A supplementation, constitutes critical factors in reducing immune deficiency and expediting the global eradication of poliomyelitis. Such an integrated approach may prove valuable in overcoming the challenges posed by poliovirus transmission in areas with poor environments and suboptimal health systems.
Acknowledgments
The authors express their gratitude to the Division of Viral Diseases team at the CDC in Atlanta, specifically acknowledging William C. Weldon and his team for testing all samples. Appreciation is also extended to UCLA students Skylar Martin and Sydney Merritt for their editorial contributions, as well as to the DRC Ministry of Public Health, Hygiene and Prevention, regional health officials, and all survey interviewers and data collectors for their pivotal roles in this research. Thanks to Arie Voorman for his contribution on the methods, study design, and implementation of this study.
Author Contributions
All authors contributed significantly to the research reported, from the initial concept and design to execution, data collection, analysis, and interpretation. They were involved in writing, reviewing, and editing the manuscript, approved the final draft for publication, consented to the chosen journal for submission, and agreed to be responsible for all aspects of the work. Additionally, all authors have reviewed and consented to the manuscript’s published version.
Funding
This work was funding from the Bill and Melinda Gates Foundation investment. OPP106684 (PI Anne W. Rimoin).
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Mbunga BK, Mapatano MA, Strand TA, et al. Prevalence of anemia, iron-deficiency anemia, and associated factors among children aged 1–5 years in the rural, malaria-endemic setting of popokabaka, democratic Republic of Congo: a cross-sectional study. Nutrients. 2021;13(3):1–13. doi:10.3390/nu13031010
2. Mbunga BK, Engebretsen IMS, Strand TA, et al. Distribution and determinants of serum zinc, copper, and selenium levels among children under five years from popokabaka, democratic republic of Congo: a cross-sectional study. Nutrients. 2022;14(3):683. doi:10.3390/nu14030683
3. Müller O, Krawinkel M. Malnutrition and health in developing countries. Cmaj. 2005;173(3):279–286. doi:10.1503/cmaj.050342
4. Faber M, Berti C, Smuts M. Prevention and control of micronutrient deficiencies in developing countries: current perspectives. Nutr Diet. 2014;2(Suppl 6):41–57.
5. Pierar M Facteurs liés à la dénutrition chez les enfants de moins de 5 ans au Nigéria: analyse des données de l’étude National Nutrition Health Survey (NNHS) 2018. Université catholique de Louvain; 2018.
6. INS RDC. Democratic Republic of the Congo: acute Malnutrition Situation July - December 2022 and Projection for January - June 2023; 2022. Available from: https://www.ipcinfo.org/ipc-country-analysis/details-map/en/c/1155974/.
7. Akilimali A, Banga S, Oduoye MO, et al. Malnutrition among under-five children in Democratic Republic of the Congo: a plague of the health system. Ann Med Surg. 2022;82:20–22. doi:10.1016/j.amsu.2022.104260
8. Rodríguez L, Cervantes E, Ortiz R. Malnutrition and gastrointestinal and respiratory infections in children: a public health problem. Int J Environ Res Public Health. 2011;8(4):1174–1205. doi:10.3390/ijerph8041174
9. Opare JKL, Akweongo P, Afari EA, Odoom J Poliovirus neutralizing antibody levels among individuals in three regions of Ghana Study design; 2019:170–180.
10. Roberts L. Polio Outbreak Breaks the Rules. Science. 2010;330(6012):1730–1731. doi:10.1126/science.330.6012.1730
11. GPEI. DRC 2022 Status: affected by circulating vaccine-derived poliovirus type 1 (cVDPV1) and type 2 (cVDPV2). The Global Polio Eradication Initiative; 2022. Available from: https://polioeradication.org/where-we-work/democratic-republic-of-The-congo/.
12. Mbaeyi C. Update on vaccine-derived poliovirus outbreaks – democratic Republic of the Congo, Horn of Africa, 2017 – 2018 Le point sur les flambées de poliovirus dérivés d “une souche vaccinale – république démocratique du Congo, Corne de l” Afrique, 2017-2018; 2018:580–588.
13. GPEI. Global eradication of wild poliovirus type 2 declared; 2015.
14. Sutter RW, John TJ, Jain H, et al. Immunogenicity of bivalent types 1 and 3 oral poliovirus vaccine: a randomised, double-blind, controlled trial. Lancet. 2010;376(9753):1682–1688. doi:10.1016/S0140-6736(10)61230-5
15. Alfonso VH, Voorman A, Hoff NA, et al. Poliovirus immunity among adults in the Democratic Republic of the Congo: a cross-sectional serosurvey. BMC Infect. Dis. 2022;22(1). doi:10.1186/s12879-021-06951-6
16. INS RDC. Enquête par grappes à indicateurs multiples, 2017-2018, rapport de résultats de l’enquête; 2018. Available from: https://www.unicef.org/drcongo/media/3646/file/COD-MICS-Palu-2018.pdf.
17. Deshpande JM, Bahl S, Sarkar BK, et al. Assessing population immunity in a persistently high-risk area for wild poliovirus transmission in India: a serological study in Moradabad, Western Uttar Pradesh. J Infect Dis. 2014;210(suppl 1):S225–S233. doi:10.1093/infdis/jiu204
18. Congo (Democratic Republic). Ministère du plan. Enquête Démographique et de Santé, RDC 2007. Calverton, Maryland, USA: Ministère du Plan Macro Int; 2008:1–499.
19. Craig KTO, Verma H, Iliyasu Z, et al. Role of serial polio seroprevalence studies in guiding implementation of the polio eradication initiative in Kano, Nigeria: 2011-2014. J Infect Dis. 2016;213(suppl 3):S124–S130. doi:10.1093/infdis/jiv774
20. Bahl S, Estívariz CF, Sutter RW, et al. Cross-sectional serologic assessment of immunity to poliovirus infection in high-risk areas of Northern India. J Infect Dis. 2014;210(suppl_1):S243–S251. doi:10.1093/infdis/jit492
21. Gamage D, Palihawadana P, Mach O, et al. Achieving high seroprevalence against polioviruses in Sri Lanka — results from a serological survey, 2014. J Epidemiol Glob Health. 2015;5(S1):S67–S71. doi:10.1016/j.jegh.2015.06.004
22. Guindo O, Mach O, Doumbia S, et al. Assessment of poliovirus antibody seroprevalence in polio high risk areas of West Africa. Vaccine. 2018;36(8):1027–1031. doi:10.1016/j.vaccine.2018.01.022
23. Razafindratsimandresy R, Mach O, Heraud J-M, et al. Assessment of poliovirus antibody seroprevalence in high risk areas for vaccine derived poliovirus transmission in Madagascar. Heliyon. 2018;4(3):e00563. doi:10.1016/j.heliyon.2018.e00563
24. Prendergast AJ. Malnutrition and vaccination in developing countries. Philos Trans R Soc B Biol Sci. 2015;370(1671):20140141. doi:10.1098/rstb.2014.0141
25. Olofin I, Mcdonald CM, Ezzati M, Flaxman S, Black RE Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: a pooled analysis of ten prospective studies; 2013:8.
26. Halbrook M. Population and Geospatial Risks of Vaccine-Derived Poliovirus Type-2 in theDemocratic Republic of the Congo. Los Angeles: University of California; 2021.
27. Benguigui Y. Integrated management of childhood illness (IMCI): an innovative vision for child health care. Rev Bras Saúde Matern Infant. 2001;1(3):223–236. doi:10.1590/S1519-38292001000300003
28. MiniSanté-Rdc. Enquête Démographique et de Santé 2013-2014 Rapport de synthèse République Démocratique du Congo; 2014:1–24.
29. Weldon WC, Oberste MS, Pallansch MA. Standardized Methods for Detection of Poliovirus Antibodies. Methods Mol Biol. 2016;1387:145–176.
30. Gamougam K, Jeyaseelan V, Jones KAV, et al. A Survey to assess serological prevalence of poliovirus antibodies in areas with high-risk for vaccine-derived poliovirus transmission in Chad. J Pediatric Infect Dis Soc. 2022;2022(2):55–64. doi:10.1093/jpids/piab103
31. Mwamba GN. Prediction model with validation for polioseronegativity in malnourished children from poliomyelitis transmission high-risk area of the Democratic Republic of the Congo (DRC); 2023:155–165.
32. Parker EPK, Ramani S, Lopman BA, et al. Causes of impaired oral vaccine efficacy in developing countries. Future Microbiol. 2018;13(1):97–118. doi:10.2217/fmb-2017-0128
33. Rytter MJH, Kolte L, Briend A, Friis H, Christensen VB. The immune system in children with malnutrition - A systematic review. PLoS One. 2014;9:2.
34. Savy M, Edmond K, Fine PE, et al. Landscape analysis of interactions between nutrition and vaccine responses in children. J Nutr. 2009;139(11):2154S–2218S. doi:10.3945/jn.109.105312
35. Pan WK, Seidman JC, Ali A, et al. Oral polio vaccine response in the MAL-ED birth cohort study: considerations for polio eradication strategies. Vaccine. 2019;37(2):352–365. doi:10.1016/j.vaccine.2018.05.080
36. Hoest C, Seidman JC, Pan W, et al. Evaluating associations between vaccine response and malnutrition, gut function, and enteric infections in the MAL-ED cohort study: methods and challenges. Clin Infect Dis. 2014;59(suppl_4):S273–S279. doi:10.1093/cid/ciu611
37. Saleem AF, Mach O, Quadri F, et al. Immunogenicity of poliovirus vaccines in chronically malnourished infants: a randomized controlled trial in Pakistan. Vaccine. 2015;33(24):2757–2763. doi:10.1016/j.vaccine.2015.04.055
38. Chopra K, Kundu S, Chowdhury DS. Antibody response of infants in tropics to five doses of oral polio vaccine. J Trop Pediatr. 1989;3(35):19–23. doi:10.1093/tropej/35.1.19
39. Greenwood BM, Bradley-Moore AM, Bradley AK, Kirkwood BR, Gilles HM. The immune response to vaccination in undernourished and well-nourished Nigerian children. Ann Trop Med Parasitol. 1986;80(5):537–544. doi:10.1080/00034983.1986.11812062
40. Rahman MM, Alvarez JO, Mahalanabis D, et al. Effect of vitamin A administration on response to oral polio vaccination. Nutri Res. 1998;18(7):1125–1133. doi:10.1016/S0271-5317(98)00094-3
41. Semba RD, Mohgaddam NEG. Integration of vitamin A supplementation with the expanded program on immunization does not affect seroconversion to oral poliovirus vaccine in infants. J Nutr. 1999;129(12):2203–2205. doi:10.1093/jn/129.12.2203
42. Newton S, Cousens S, Owusu-Agyei S, et al. Vitamin A supplementation does not affect infants’ immune responses to polio and tetanus vaccines. J Nutr. 2005;135(11):2669–2673. doi:10.1093/jn/135.11.2669
43. Gaayeb L, Pinçon C, Ndiath MO, et al. Effects of malnutrition on children’s immunity to bacterial antigens in northern Senegal. Am J Trop Med Hyg. 2014;90(3):566–573. doi:10.4269/ajtmh.12-0657
44. El-Sayed N, Al-Jorf S, Hennessey KA, et al. Survey of poliovirus antibodies during the final stage of polio eradication in Egypt. Vaccine. 2007;25(27):5062–5070. doi:10.1016/j.vaccine.2007.04.022
45. Di Cesare M, Bhatti Z, Soofi SB, et al. Geographical and socioeconomic inequalities in women and children’s nutritional status in Pakistan in 2011: an analysis of data from a nationally representative survey. Lancet Glob Heal. 2015;3(4):e229–e239. doi:10.1016/S2214-109X(15)70001-X
46. Rayman MP, Calder PC. Optimising COVID-19 vaccine efficacy by ensuring nutritional adequacy. Br. J. Nutr. 2021;126(12):1919–1920. doi:10.1017/S0007114521000386
47. Church JA, Rukobo S, Govha M, et al. Neonatal Vitamin A supplementation and immune responses to oral polio vaccine in Zimbabwean infants. Trans R Soc Trop Med Hyg. 2019;113(3):110–115. doi:10.1093/trstmh/try126
48. Simhon A, Lifshitz A, Abed Y, Lasch EE, Schoub B, Morag A. How to predict the immune status of poliovirus vaccinees? A comparison of virus neutralization at a very low serum dilution versus ELISA in a cohort of infants. Int J Epidemiol. 1990;19(1):164–168. doi:10.1093/ije/19.1.164
49. Ivanov AP, Dragunsky EM. ELISA as a possible alternative to the neutralization test for evaluating the immune response to poliovirus vaccines. Expert Rev Vaccines. 2005;4(2):167–172. doi:10.1586/14760584.4.2.167
50. Hashido M, Horie H, Abe S, et al. Evaluation of an enzyme-linked immunosorbent assay based on binding inhibition for type-specific quantification of poliovirus neutralization- relevant antibodies. Microbiol Immunol. 1999;43(1):73–77. doi:10.1111/j.1348-0421.1999.tb02375.x
51. Faden H, Duffy L, Sun M, Shuff C. Long-term immunity to poliovirus in children immunized with live attenuated and enhanced-potency inactivated trivalent poliovirus vaccines. J Infect Dis. 1993;168(2):452–454. doi:10.1093/infdis/168.2.452
52. Herremans T, Kimman TG, Conyn–van Spaendonck MAE, et al. Immunoglobulin a as a serological marker for the (silent) circulation of poliovirus in an inactivated poliovirus-vaccinated population. Clin Infect Dis. 2002;34(8):1067–1075. doi:10.1086/339489
53. Wright PF, Wieland-Alter W, Ilyushina NA, et al. Intestinal immunity is a determinant of clearance of poliovirus after oral vaccination. J Infect Dis. 2014;209(10):1628–1634. doi:10.1093/infdis/jit671
54. Smith DJ, Gahnberg L, Taubman MA, Ebersole JL. Salivary antibody responses to oral and parenteral vaccines in children. J Clin Immunol. 1986;6(1):43–49. doi:10.1007/BF00915363
55. Hird TR, Grassly NC, Andino R. Systematic review of mucosal immunity induced by oral and inactivated poliovirus vaccines against virus shedding following oral poliovirus challenge. PLoS Pathog. 2012;8(4):e1002599. doi:10.1371/journal.ppat.1002599
56. Mcbean AM, Thoms ML, Albrecht P, Cuthie JC, Bernier R. Serologic response to oral polio vaccine and enhanced-potency inactivated polio vaccines. Am J Epidemiol. 1988;128(3):615–628. doi:10.1093/oxfordjournals.aje.a115009
57. Bowman TA, Goonewardene IM, Pasatiempo AMG, Ross AC, Taylor CE. Vitamin A deficiency decreases natural killer cell activity and interferon production in rats. J Nutr. 1990;120(10):1264–1273. doi:10.1093/jn/120.10.1264
58. Modlin JF, Halsey NA, Thoms ML, Meschievitz CK, Patriarca PA. Humoral and mucosal immunity in infants induced by three sequential inactivated poliovirus vaccine-live attenuated oral poliovirus vaccine immunization schedules. J Infect Dis. 1997;175(Supplement 1):S228–S234. doi:10.1093/infdis/175.Supplement_1.S228
59. Crawt L, Atkinson E, Tedcastle A, et al. Differences in antigenic structure of inactivated polio vaccines made from sabin live-attenuated and wild-type poliovirus strains: impact on vaccine potency assays. J Infect Dis. 2020;221(4):544–552. doi:10.1093/infdis/jiz076
60. Bahl R, Bhandari N, Kant S, et al. Effect of vitamin A administered at expanded program on immunization contacts on antibody response to oral polio vaccine. Eur J Clin Nutr. 2002;56(4):321–325. doi:10.1038/sj.ejcn.1601325
61. Ravi SJ, Vecino-Ortiz AI, Potter CM, Merritt MW, Patenaude BN. Group-based trajectory models of integrated vaccine delivery and equity in low- and middle-income countries. Int J Equity Health. 2024;23(1):1–26. doi:10.1186/s12939-023-02088-x
62. Penkert RR, Rowe HM, Surman SL, et al. Influences of Vitamin A on vaccine immunogenicity and efficacy. Front Immunol. 2019;10:1–9. doi:10.3389/fimmu.2019.01576
63. Habyarimana F. Key determinants of malnutrition of children under five years of age in Rwanda: simultaneous measurement of three anthropometric indices. African Popul Stud. 2016;30:2328–2340.
64. Berger MM, Amrein K, Barazzoni R, et al. The science of micronutrients in clinical practice – report on the ESPEN symposium. Clin Nutr. 2024;43(1):268–283. doi:10.1016/j.clnu.2023.12.006
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
