Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Nursing Interventions to Improve Quality of Life Among Children and Adolescents with Thalassemia: A Scoping Review
Authors Mardhiyah A , Panduragan SL, Mediani HS , Yosep I
Received 1 April 2023
Accepted for publication 21 June 2023
Published 23 June 2023 Volume 2023:16 Pages 1749—1762
DOI https://doi.org/10.2147/JMDH.S415314
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ai Mardhiyah,1,2 Santhna Letchmi Panduragan,3 Henny Suzana Mediani,1 Iyus Yosep4
1Department of Pediatric Nursing, Faculty of Nursing, Universitas Padjadjaran, Sumedang, West Java, Indonesia; 2Faculty of Health Science, Lincoln University College, Petaling Jaya, Selangor Darul Ehsan, Malaysia; 3Faculty of Nursing, Lincoln University College, Petaling Jaya, Selangor Darul Ehsan, Malaysia; 4Department of Mental Health, Faculty of Nursing, Universitas Padjadjaran, Sumedang, West Java, Indonesia
Correspondence: Ai Mardhiyah, Department of Pediatric Nursing, Faculty of Nursing, Universitas Padjadjaran, Jl. Raya Ir. Soekarno KM. 21, Hegarmanah, Jatinangor, Sumedang, West Java, 45363, Indonesia, Tel +62 81322629909, Fax +6202287793411, Email [email protected]
Abstract: Thalassemia is an inherited blood disorder affecting hemoglobin synthesis which leads to chronic hemolysis that can reduce the quality of life of children with it due to the disease and the treatment given. However, the intervention still focuses on handling physical problems due to thalassemia. So that an intervention that focuses on improving the quality of life of children with thalassemia is needed. The purpose of this study is to explore interventions that could improve the quality of life of children with thalassemia. A scoping review study design was used in this study. The databases used are CINAHL, PubMed, and Scopus. Articles published from last five years (2018– 2022), open access full-text, in English, and with the type of randomized controlled trial (RCT). The keywords used in English are “thalassemia or beta-thalassemia” AND “quality of life OR Life Quality OR Health-Related Quality of Life” AND “nursing intervention OR nursing care”. From ten articles analyzed, we found five types of nursing intervention: Health Care Instructions, Psychological Program, Educational Program, Counseling Program, and Self-care Model, which were carried out for 1– 7 months. The articles in this study are from Egypt and Iran. The sample in this study is the range of 20– 173 respondents. The thalassemia patients in this study were in the age range of 7– 35 years, but the average age of the patients was in their 20s. Nursing intervention can potentially improve the quality of life in children and adolescents with thalassemia. Nurses need to pay attention to the patient’s age, family and patient knowledge about the disease, length of stay, and the patient’s physical and psychological condition in providing nursing care to patients with thalassemia. Implementation of nursing is given by paying attention to the stages of child development and involving the family. Nursing interventions can be carried out by nurses or nurses teach families to intervene at home. This nursing intervention has the potential to improve the quality of life of patients with thalassemia while still taking into account the conditions of the patient and family in a comprehensive manner.
Keywords: nursing intervention, quality of life, thalassemia
Introduction
Thalassemia is a hereditary blood disorder resulting in chronic hemolytic anemia disease due to defective hemoglobin synthesis. Thus, erythrocytes of patients with thalassemia have a shorter lifespan (less than 120 days).1 It is the most common genetic disease worldwide and has been declared a world health problem.2 According to the World Health Organization (WHO), thalassemia is the most common genetic disease in the world which has now been declared a world health problem.3,4 Approximately 7% of the world’s population has the thalassemia gene. Based on WHO data, about 250 million people in the world (4.5%) carry the thalassemia gene, while 80–90 million of them carry the thalassemia gene.5
Symptoms obtained in patients are general symptoms, namely: anemia, paleness, fatigue, and a decrease in hemoglobin levels, enlargement of the spleen, and Cooley’s Fascies (the marrow produces excessive red blood cells so that the marrow cavity enlarges causing thinning of the bones and protrusion of the forehead).6–8 Another sign in thalassemia patients is enlargement of the spleen (splenomegaly) and cooley’s fascies can be described as signs due to ineffective erythropoiesis where there is sub-optimal production of mature erythrocytes.9 Clinical symptoms have been seen since the child was less than 1 year old, namely: symptomatic anemia at the age of 6–12 months, along with decreased fetal hemoglobin levels.10 Patients with β-thalassemia major generally show symptoms in the form of weakness, fatigue quickly, yellowish skin and sclera (jaundice), dark urine, increased heart rate, shortness of breath, dizziness, headaches, growth retardation, children become thin, stomach distended due to hepatosplenomegaly with a distinctive face (frontal bossing), crooked mouth (rodent like mouth), slightly drawn lips, and dental malocclusion.11
Blood transfusion treatment is the only way to prevent death in children with thalassemia. Blood transfusion aims to maintain a hemoglobin level of 9–10 g/dl.12 For children and their families, the fact that a child is diagnosed with thalassemia is like a nightmare for several reasons, such as the lower life expectancy in non-compliance patients ie transfusion dependent thalassemia patients who do not routinely receive blood transfusion, lifelong blood transfusion treatment, and changes in the child’s physical form that are clearly visible.13 This condition will cause changes both physically and psychologically. Physical problems experienced in the form of changes in skin color to black, pale, thinning hair, and enlarged stomach, while the psychological impact experienced in the form of feeling bored, saturated, and hopeless.14–16 Psychologically, thalassemic children feel different from their group, children feel limited in their activities, academic achievement tends to be low, and self-confidence decreases.17,18
Lifelong treatment and management to reduce complications in children with thalassemia can affect the quality of life of children with thalassemia.19,20 Conditions can affect the chronic conditions experienced by children which affect their quality of life.4,21,22 Thalassemia is a chronic disease that can actually affect the quality of life of the sufferer. The quality of life of children with chronic diseases will be very dependent on the family so that it can cause stress for families, especially parents because children need more attention.22–24 Quality of life is an individual’s perception of his position in life, in the cultural context, the value system in which they are located and their relationship to life goals, expectations, standards, and other related issues that cover a very broad and complex quality of life including physical health problems, psychological status, the level of freedom, social relations and the environment in which they are located.22,25,26
Previous scoping review of family-centered care have shown that family-centered care is effective for improving the quality of life in adolescents with chronic illnesses.27 The sample shows that the study recommends conducting further research on family-centered care in improving the quality of life for adolescents with thalassemia. Another study on nursing interventions showed a significant increase in quality of life in adolescents with chronic illnesses.28 From these two data, some chronic diseases are thalassemia. So based on these data, this study is the first scoping review that describes nursing interventions to improve the quality of life for adolescents with thalassemia.
In improving the quality of life of thalassemia patients, interventions are needed to be given to children with thalassemia or their families. Parents need to be equipped with knowledge related to thalassemia, in order to carry out their role as primary caretaker of the pediatric patients.29–32 Lack of parental knowledge about thalassemia disease can result in non-optimal care provided by parents to children with thalassemia.4,25 Research states that the sense of security created by individuals is able to make sick individuals feel comfortable, calm in their environment, not afraid, ashamed, and low self-esteem when dealing with people or other teenagers, through the ability to care independently, sufferers will feel his self-esteem lifted, and feel as if the individual does not feel the slightest pain and assumes that he can be healthy again as usual.4,19,33
The role of nurses in providing nursing care where the first role and function of nurses is promotive where nurses are able to provide health education to parents with hematological disorders, especially in thalassemia.34 The second role and function of the nurse is preventive where the role of the nurse here is being able to take actions that can prevent new problems from occurring, such as infection. The third role and function of the nurse is curative where at this stage the nurse is able to provide nursing services by collaborating with other health teams to provide pain relief, antibiotics to prevent infection.19 The fourth role and function of the nurse is rehabilitative where the nurse is able to make the patient independent so that the patient can recover and be able to do activities as before being admitted to the hospital.
The role of the nurse is to carry out nursing care starting from assessment to nursing evaluation. The nursing assessment carried out must be comprehensive covering physical, psychological, spiritual, cultural, and social aspects.35 Nursing implementation is carried out such as maintaining effective breathing patterns, maintaining peripheral tissue perfusion, increasing activity tolerance, improving body image, preventing infection, and stimulating growth and development according to age.36 So that nurses need to holistically pay attention to the patient’s condition in order to improve the quality of life of patients with thalassemia.
Interventions given by nurses are still focused on physical treatment to reduce symptoms due to thalassemia. In addition to the physical aspect, the quality of life is also influenced by the psychological aspect. So that interventions are needed by nurses to improve the quality of life of children with thalassemia. The purpose of this study was to explore nursing interventions that can be given to improve the quality of life of children with thalassemia.
Materials and Methods
Design
This study used a scoping review design with a scoping review design. Scoping review is a methodological technique that serves to explore new topics today.37 The broad conceptual range of this research framework is an advantage for explaining various relevant findings according to research objectives.38 The framework in this research consists of 5 core stages, namely identification of research questions, identification of relevant study findings, study selection, data mapping, compilation of results, and reporting of analyzed study results.39
Search Methods
This study used a search strategy with PCC’s (Population, Concept, Context) framework:
Population: adolescents with thalassemia
Concept: nursing intervention
Context: improving quality of life
The databases used in the article search are CINAHL, Pubmed, and Scopus. The keywords used are: “thalassemia OR beta thalassemia” AND “quality of life OR life quality OR heathy-quality of life” AND “nursing care OR nursing intervention”. The research questions are: How are nursing interventions to improve the quality of life of children with thalassemia?
Inclusion and Exclusion Criteria
The data search method in this study used PRISMA Extension for Scoping Reviews (PRISMA-ScR) to identify various topics that discussed nursing interventions to improve the quality of life of children with thalassemia (Figure 1). Articles were selected based on inclusion and exclusion criteria. The inclusion criteria for this study were that the patients were children with thalassemia, quasi experiment or randomized control trial, using English, open access full text, and the time setting of the last 10 years (2013–2022). The exclusion criteria in this study were that the sample was not adolescents with thalassemia and was not a nursing intervention.
 |
Figure 1 PRISMA Flow Diagram. Adapted from Page MJ. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Creative Commons.40 |
Data Extraction
After doing a search of articles from three databases. Three authors selected articles using inclusion criteria and screening of titles and abstracts. Then three authors read the article in full-text. The three authors held discussions on the contents of the articles they had read to determine the eligibility of the articles to be included in this scoping review. If there is a debate between authors regarding the contents of the article, the authors conduct deliberations to determine the feasibility of the article. If there is still no agreement between the three authors, the fourth author is invited to read the full-text article and review the article and discuss with the other three authors. After the authors read the articles that match the inclusion and exclusion criteria. The authors read the article in full-text. After that, the authors make a summary of the important aspects according to the research objectives, namely the interventions carried out and the results obtained. The authors then write the results of the analysis into the manual table made by the authors. It aims to make it easier for writers to compare research results. Articles were extracted using a table containing authors, outcome, year, country, study design, sample, intervention, and research results.
Quality Appraisal
Assessment of the quality of the articles in this study aims to obtain articles that are relevant to the research objectives. Assessment of the quality of the article using the Joanna Briggs Institute (JBI) assessment. JBI assessment conducts an assessment by giving a score to the statements provided by JBI. There are 13 statements for articles with a randomized control trial design and 9 statements for articles with a quasi-experimental design. Assessment of articles with discussion of all authors. Each statement is given a score of 1 for the answer option yes and a score of 0 for the answer option no, unclear, and not applicable. Journals were analyzed using the JBI critical assessment method with good article standards to be used if above 75% based on criteria and topic relevance (Table 1).
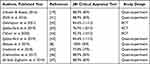 |
Table 1 JBI Critical Appraisal Tool |
Data Analysis
Data analysis in this study was carried out using a qualitative approach. The articles obtained were then read in full and then analyzed comprehensively by the authors. The authors described the findings and also presents them in tabular form. Data analysis was carried out by all authors by comparing findings from articles that match the inclusion criteria and exclusion criteria. After being analyzed, each intervention obtained was classified based on similar interventions and then a description of the intervention and the impact of the intervention was given on children with thalassemia.
Results
The total articles obtained from search engines are 684 articles. Then the authors checked for duplication of articles using the Mendeley application, and found 140 duplicate articles. Then the authors eliminated based on the inclusion criteria, and examined the articles by reading the titles and abstracts, and found 17 articles that matched them. After that, the authors read the full-text articles and examined the exclusion criteria, and found 10 articles that fit the research objectives. The 10 articles were then examined for the quality of the articles using the JBI Critical Appraisal Tools, and 10 articles were found to be appropriate and relevant with a JBI score above 75%.
The researcher identified the 5 methods by providing an explanation of the impacts and activities carried out as well as the impact of the interventions carried out. The results of the analysis of the article are presented in tabular form as follows (Table 2):
 |
Table 2 Extraction Data |
There are 10 articles that describe nursing interventions to improve the quality of life of children with thalassemia. In addition, the intervention can also improve mental health such as adaptive coping, increasing self-efficacy, increasing resilience, and reducing stress. This study shows that the articles come from Iran (8 articles) which is a developing country and Egypt (2 articles) which is a developed country. Design articles in this review are quasy experiment (8 articles) and RCT (2 articles). The sample in this study is the range of 20–173 respondents. The age range of patients with thalassemia is between the ages of 7–35 years. The research subjects from the articles analyzed were children with thalassemia. Of the 10 articles analyzed, there are 5 types of nursing interventions, namely through Health Care Instructions, Psychological Programs, Educational Programs, Counseling Programs, and Self-care Models. The following is an explanation of each type of nursing intervention:
Health Care Instructions
Health care instructions are given by nurses to provide instructions for therapy that can be carried out independently by patients and families. In addition, nurses also provide psychological support to patients and families. The therapies trained by nurses are psychological and spiritual therapy, relaxation therapy, nutritional therapy, blood transfusions, and schedule check-ups to health services. Intervention Health Care instructions begins by analyzing the needs of each. The success of this intervention is influenced by the understanding of parents or caregivers about the patient’s disease. The more families and patients understand the instructions given by nurses, the easier the intervention process will be given. So that the level of family education is important to be able to understand the instructions given by nurses. The difficulty in carrying out this intervention is when the family and the patient do not understand the importance of the intervention and the patient and family are getting bored with the routine therapy being carried out. So nurses need to do games so that activities are not boring.
The intervention was carried out as many as 10 sessions for each child and parent with a time of 7 months.19 Health instructions given to participants regarding health needs, namely nutrition, efforts to relieve pain, treatment plans, the importance of blood transfusions, and follow-up plans. In each session there is an evaluation delivery in the form of knowing the feelings and problems that have not been resolved by the participants. Problems that have not been completed by health care instructions is given counseling to resolve the problem. Instructions are adjusted to the stage of development and family environment. The results of the study showed that there was a significant effect in improving the quality of life of children with thalassemia.
The next instruction-based intervention is a nurse-implemented orientation program consisting of three steps, namely introduction, implementation, and closing.41 At the inauguration stage, nurses and participants discuss the patient’s needs, improve the health status of participants, increase the role of participants, and prevent complications, this aims also to build trust between participants and nurses. In the second stage, participants were explained about thalassemia disease and the impact of treatment, also explained about the concept of hemosiderosis and splenectomy and strategies to prevent infection from the treatment provided. Then at this stage it is also explained about diet and treatment regimens as well as strategies for dealing with psychological problems. At the end of the session, a booklet of information about thalassemia was given to serve as an activity guide. So that participants experienced a significant improvement in quality of life after being given the intervention.
Psychological Program
Psychological program is an intervention that focuses on providing psychological support for adolescents with thalassemia. Adolescents and their parents are given psychoeducation about their illness. Then, relaxation therapy exercises are given to be practiced independently by the patient and family. Psychological problems are influenced by the psychological condition of the participants and also the age of the patient with thalassemia. Nurses must also pay attention to the stages of adolescent development so that emotional instability does not occur. So nurses need to pay attention to the patient’s age. In addition, the physical condition of the patient and family also needs to be considered to maintain the overall condition of the patient and family. The patient’s unstable psychological condition sometimes becomes an obstacle for patients and their families in carrying out the program. So that mental nurses need to carry out additional therapy to increase the emotional stability of patients and families such as practicing relaxation and mindfulness techniques.
The form of psychological program is continuous care program (CCM) was carried out individually for 14 weeks.42 The first step in this activity is orientation with a duration of 30–40 minutes per session. Activities in the form of introductory sessions, program contracts, and knowing the quality of life of participants. The second stage is sensitization with a duration of 45 to 60 minutes. The intervention consisted of six training sessions discussing anatomy and physiology related to thalassemia, thalassemia complications and treatment procedures, diet of thalassemia patients and the role of exercise, basic care for thalassemia and side effects of treatment, training in relaxation techniques, and training in social skills. In the last session, participants were given education through booklets, CDs, and self-control checklists so that participants could follow the instructions given. The CCM program has proven to be effective as an intervention in nursing care in improving the quality of life of participants.
The second psychological intervention that can be done is individual psychotherapy (cognitive-behavioral therapy).44 This intervention was opened with an introduction to the program, an assessment of the quality of life and self-efficacy of the participants, interviews with participants related to the fear of disease, and identifying psychological problems. Then participants were given training on the détente method, which is to train muscle relaxation and deep breathing for 15 minutes. Participants were also asked to practice speaking skills in solving problems, as well as practicing self-management. Participants experienced an increase in quality of life and a decrease in anxiety after being given the intervention.
The third psychological intervention is acceptance and commitment therapy.43 This intervention begins with an introduction to the intervention and the task of recording daily experiences. Furthermore, participants were taught strategies, assessment methods, and preventing complications from control therapy. In addition, participants were also trained to solve problems, accept, identify ego, and develop strategies to achieve goals. At the end of the session, participants were asked to reflect on their past experiences. This intervention can significantly reduce stress, increase resilience, and improve the quality of life of participants with thalassemia major.
The fourth psychological intervention is Resilience and Stress Management (SMART).8 Participants will be asked to raise awareness about stress, the physical signs of stress, and the perceived effects of stress. In addition, participants were also taught about the concept of persistence, how to deal with stress, and progressive muscle training. Participants were also given cognitive distortions, namely identification of negative thoughts, cognitive reconstruction, muscle relaxation, diaphragmatic breathing, training in adaptive coping, building intimacy, and deep breathing meditation. After being given the intervention, participants effectively reduce stress, increase resilience, build adaptive coping, and improve quality of life.
Educational Program
Educational programs are interventions provided by nurses to increase patient and family knowledge about the disease they are suffering from. Nurses act as educators in providing information about the disease, the impact of the disease, and also about the treatment that must be carried out. Providing education to patients is influenced by patient and family education. This can provide a two-way discussion between participants and nurses. In addition, patient compliance to implement education provided by nurses is also important to improve treatment outcomes for thalassemia patients. The length of care for thalassemia patients also influences the patient’s and family’s initial understanding of thalassemia. Providing education to patients sometimes only increases patient understanding, but does not change patient behavior in carrying out independent treatment of thalassemia. So that supervision from nurses is needed to ensure that thalassemia care is carried out by families and patients.
The educational program through Educational Program Therapy is carried out for five sessions. The duration of each session is 20–30 minutes.48 The methods used in providing education are lectures, demonstrations, and group discussions. Participants are given motivation and appreciation after doing the activity. After participants understood their illness through educational programs, participants experienced a significant improvement in their quality of life.
Another educational program is an educational program about iron chelation therapy with a duration of 45–60 minutes.47 Participants were explained about program objectives, content, and procedures. The method given in education is through group discussions and presentations of the results of the discussions. This intervention proved to be effective in improving the quality of life of children with thalassemia.
Counseling Program
Counseling is the process of providing assistance carried out by an expert to individuals who are experiencing a problem to overcome the problems faced by the client. Psychiatric nurses and pediatric nurses play a role in counseling patients and families to solve problems caused by thalassemia. The pediatric nurse’s role is to pay attention to the development of patients with thalassemia so that they can be fulfilled. The implementation of counseling is influenced by the trust that is built between the patient and the nurse. So that efforts to build a trusting relationship usually require a longer time. Patient and family awareness of the problem is important for the counseling process. Counseling takes a long time, so patients can feel bored with repetitive activities. Some of the obstacles to telephone counseling include unstable networks and discrepancies in the counseling schedule. So that initial agreement is needed in counseling so that patients and their families and nurses can adhere to a predetermined schedule.
The counseling program that can be done is through groups. Counseling is given to solve problems with the active participation of participants.46 Participants were given a booklet related to disease, symptoms, complications, and treatment for quality of life in thalassemia and given one month to study it. After that, participants were invited to counseling by telephone for 15–20 minutes regarding the patient’s difficulties, especially regarding his illness. This counseling group has proven to be effective in improving the quality of life of children with thalassemia.
Self-Care Model
The self-care model is nursing care provided to patients and families to improve self-care abilities. Self care is the ability of individuals, families and communities to improve health, prevent disease, maintain health and overcome disease with or without support from health care providers. Participants were given education about self-care. However, nurses still provide self-care services to patients. The implementation of the self-care model is influenced by the length of care that has been carried out by the patient. The longer the treatment has been carried out, the more understanding of self-care methods are carried out in patients with thalassemia. In addition, the patient’s knowledge of the disease and its therapy influences the interventions given. The higher the knowledge possessed by the patient, the easier it is for the patient to understand what self-care should be done.
Orem Self-care Model is one of the self-care interventions through training with interactive presentations and discussions from doctors about thalassemia disease.45 After that, doctors and nurses provided education about self-care for 60 minutes. Participants were given directions regarding self-care that can be done by being given a booklet. Participants are asked to practice independently from the booklet provided. Self-care is believed to increase the client’s confidence and perception to be healthier. Orem Self-care Model is able to significantly improve the quality of life of patients with thalassemia major.
Discussion
This study is the first scoping review that discusses nursing interventions to improve the quality of life for adolescents with thalassemia. The authors found that there were 5 types of interventions that could be carried out, namely Health Care Instructions, Psychological Programs, Educational Programs, Counseling Programs, and Self-care Models. Implementation is carried out by nurses in a comprehensive manner by paying attention to various aspects such as physical and psychological aspects. Interventions also involve families to increase support for children while nursing interventions are given.
This study shows that eight articles are from developing countries. This is in line with previous studies which show that the highest prevalence of thalassemia sufferers comes from developing countries. In line with this study, previous research shows that in 2021 there will be 10,973 adolescents experiencing thalassemia in Indonesia.49 However, the incidence of thalassemia is not influenced by the progress of a country. Other research shows that thalassemia sufferers in the United States of America are as much as 4.5%.22 Another studies also showed that there were 11,000 thalassemia sufferers in Egypt.11,50 This shows that thalassemia sufferers can occur in developed or developing countries.
This study shows that patients with thalassemia are in the range of 7–35 years. Although the average age of the patients shows the figure of 20 years. This shows that most interventions are carried out for children and adolescents. The age of children and adolescents requires monitoring of the developmental stages that occur in them.51 So that nurses who provide interventions must pay attention and help meet the developmental stages of children and adolescents according to their age.52 Fulfillment of these developmental stages collaborate with parents or the patient’s family to get maximum results.53
Parental involvement is also important to improve the quality of life of adolescents with thalassemia. Another study shows that there is a strong relationship between parents and the health status of their members where the role and support of parents is very important for every aspect of health care for family members starting from strategies to the rehabilitation phase.10,27 Previous studies which states that support for assessment is that parents act as a feedback guide, guide and mediate problem solving, as a source and validator of the identity of family members including providing support, appreciation, attention.54,55 This is also supported by previous studies which show that interventions carried out with family can improve the quality of life of adolescents with thalassemia by as much as 10%.6,52,56
The provision of nursing care is carried out comprehensively by nurses to adolescents by involving their parents. In this aspect, nurses must carry out comprehensive patient identification so that the nursing care provided is appropriate and in accordance with the patient’s needs. Adolescents with thalassemia are usually sensitive when discussing their disease and sad about their condition. Thus, various aspects such as physical, psychological, social, cultural, and spiritual are important things that must be considered by nurses.57,58 This is in line with previous studies which show that nurses who pay attention to all aspects that affect patients comprehensively can improve patient satisfaction and quality of life.59,60 In addition, patients also feel that there is hope for carrying out the treatment process.
Health Care Instructions is an intervention given to adolescents with thalassemia by following instructions given by nurses. This intervention is carried out so that adolescents and parents are able to independently improve the quality of life of adolescents with thalassemia. Previous studies have shown that instructions from nurses and assistance to parents regarding the care of adolescents with thalassemia can improve the quality of life of adolescents.19,61 Other studies also show that parents need directions from nurses to carry out self-care for children with thalassemia.62,63 This is supported by previous studies which show that parents lack knowledge about thalassemia care, so directions from nurses are needed to increase the role of parents and adolescents themselves in providing care.60,64,65
Psychological Programs are assistance from nurses to improve psychological aspects in adolescents with thalassemia. Psychological aspects have decreased in adolescents with thalassemia. So that interventions to improve psychological aspects are important efforts to be given by nurses. Previous studies have shown that adolescents who are given meditation therapy can manage the anxiety they experience.66 In addition, mindfulness therapy methods also function to increase hope and quality of life in adolescents with thalassemia.67,68 Adolescents are focused on increasing positive psychological aspects so as to reduce negative thoughts about their illness. In line with this, previous research also shows that adolescents who focus on the positive aspects they have have a higher quality of life.69,70
Educational Programs are educational programs to increase knowledge and quality of life in adolescents with thalassemia. Good knowledge about thalassemia can improve the quality of life of adolescents. This is in line with previous studies which show that education about chronic diseases in adolescents can improve the self-care process so that there is an increase in quality of life.65,71 In addition, other studies also show that there is a relationship between knowledge and quality of life for adolescents with thalassemia.48,64 Health Education is provided by nurses regarding various information such as definitions, factors, and independent efforts made in care. These various educations can increase patient confidence in caring for themselves. So that patients have a high quality of life.
Counseling Programs are nurses’ efforts to provide counseling to parents and adolescents with thalassemia. Counseling was carried out by a nurse for one hour to find out the feelings of adolescents and the problems they face. Problem solving in adolescents can improve the quality of life of adolescents with thalassemia. This is because the source of stress and anxiety for patients has decreased. Previous studies have shown that counseling is effective in improving the quality of life for adolescents with thalassemia.72,73 Counseling aims to reduce the anxiety and fear experienced by parents and adolescents with thalassemia. Other studies also show that counseling by nurses and psychologists for adolescents with thalassemia and their parents can increase hope and quality of life.74,75 In addition, adolescents with thalassemia have low self-esteem. So that counseling makes teenagers and parents more open about the problems they face.
Self-care Models are interventions that focus on increasing the ability to care independently for adolescents with thalassemia. Adolescents and parents are taught and directed to carry out care for people with thalassemia. Previous studies have shown that adolescents with thalassemia who perform self-care have a higher quality of life compared to adolescents who are unable to perform self-care.44,65 This is supported by other studies which show that adolescents who are able to carry out independent care have a high quality of life.56,76 In addition, other studies also show that there is a relationship between self-care and quality of life in adolescents with thalassemia.18,63 Directions from nurses also involve parents so that teenagers and parents are able to accompany their children during the treatment process.
Nursing intervention is an important aspect to be given to adolescents with thalassemia and their parents. Thalassemia adolescents are at risk of experiencing hopelessness and other psychological problems, and are even at risk of committing suicide. The nurse is the person in charge of the patient in the room who interacts a lot with the patient. So that nurses’ understanding of nursing care must be comprehensive to improve the quality of life of adolescents with thalassemia.
Limitation
This study is limited by the design of the articles reviewed, namely randomized control trials and quasi-experiments, this causes the authors to be unable to show the results of studies with other designs as a comparison in providing nursing care to adolescents with thalassemia. In addition, this study is also limited because it cannot assess the effectiveness of nursing interventions from all the articles reviewed. This is due to the limitations of the research design in this study, namely scoping review. Then this study also has limitations from the database used, namely three databases, so a comprehensive discussion is needed for further research using more article databases.
Conclusions
Nursing interventions based on improving the quality of life of children with thalassemia consist of 5 types, namely Health Care Instructions, Psychological Programs, Educational Programs, Counseling Programs, and Self-care Models. The intervention was carried out by the nurse and independently by the family at home. Nurses as educators play a role in providing education about thalassemia and also the psychological impact of thalassemia. Nurses also act as counselors to help solve problems that are owned by families and patients with their illness. Then nurses as well as instructors can provide modules for self-therapy for thalassemia. These five interventions can be effective in improving the quality of life of children with thalassemia. Implementation of nursing must pay attention to the stages of child and adolescent development to improve the quality of life of children optimally. In addition, nurses must also involve parents to provide comprehensive care according to the needs and habits of children.
The implication in this study is that there is a reference for nurses in providing types of nursing interventions to improve the quality of life of adolescents with thalassemia according to the characteristics of adolescents. Then another implication is that there is a basis for hospitals to formulate policies for nurses in providing nursing care to improve the quality of life for adolescents with thalassemia. In addition, families or caregivers of patients with thalassemia have an overview of providing care to children and adolescents with thalassemia, so they can ask for help from health services for treatments that cannot be done independently. Recommendations for further research are further research on systematic review and meta-analysis to assess the effectiveness of nursing interventions in adolescents with thalassemia.
Acknowledgments
All authors thank to Universitas Padjadjaran, Bandung, West Java, Indonesia, who has facilitated the database for us in this study.
Funding
There was no external funding in this research.
Disclosure
The authors report no conflicts of interest in this research.
References
1. Adam S, Afifi H, Thomas M, Magdy P, El-Kamah G. Quality of life outcomes in a pediatric thalassemia population in Egypt. Hemoglobin. 2017;41(1):16–20. doi:10.1080/03630269.2017.1312434
2. Telfer P, Constantinidou G, Andreou P, Christou S, Modell B, Angastiniotis M. Quality of life in thalassemia. Ann N Y Acad Sci. 2005;1054(1):273–282. doi:10.1196/annals.1345.035
3. Sheikh KA, El-setouhy M, Yagoub U, Alsanosy R, Ahmed Z. Khat chewing and health related quality of life: cross-sectional study in Jazan region, Kingdom of Saudi Arabia. Health Qual Life Outcomes. 2014;12(1):44. doi:10.1186/1477-7525-12-44
4. Dhirar N, Khandekar J, Bachani D, Mahto D. Thalassemia Major: how do we improve quality of life? Springerplus. 2016;5(1):1895. doi:10.1186/s40064-016-3568-4
5. Apidechkul T, Yeemard F, Chomchoei C, Upala P, Tamornpark R. Epidemiology of thalassemia among the hill tribe population in Thailand. PLOS ONE. 2021;16(2):1–16. doi:10.1371/journal.pone.0246736.
6. Wacharasin C, Phaktoop M, Sananreangsak S. Examining the usefulness of a family empowerment program guided by the illness beliefs model for families caring for a child with thalassemia. J Fam Nurs. 2015;21(2):295–321. doi:10.1177/1074840715585000
7. Zinati F, Khashaninia Z, Rahgoi A, Rezasoltani P, Babamahmodi F. The effect of partnership caring model on quality of life of adolescents with major thalassemia. Iran J Rehabil Res. 2016;2(2):57–67.
8. Babaei MR, Askarizadeh G, Towhidi A. The effectiveness of Stress Management and Resilience Training (SMART) on psychological well-being in patients with thalassemia major. Prev Care Nurs Midwifery J. 2019;8(4):8–15. doi:10.29252/pcnm.8.4.8
9. Ribeil JA, Arlet JB, Dussiot M, Cruz Moura I, Courtois G, Hermine O. Ineffective erythropoiesis in β-thalassemia. Sci World J. 2013;2013:394295. doi:10.1155/2013/394295
10. Khanna AK, Prabhakaran A, Patel P, Ganjiwale JD, Nimbalkar SM. Social, psychological and financial burden on caregivers of children with chronic illness: a cross-sectional study. Indian J Pediatr. 2015;82(11):1006–1011. doi:10.1007/s12098-015-1762-y
11. Elzaree FA, Shehata MA, El Wakeel MA, El-Alameey IR, AbuShady MM, Helal SI. Adaptive functioning and psychosocial problems in children with beta thalassemia major. Open Access Maced J Med Sci. 2018;6(12):2337–2341. doi:10.3889/oamjms.2018.367
12. Hellström Y, Persson G, Hallberg IR. Quality of life and symptoms among older people living at home. J Adv Nurs. 2004;48(6):584–593. doi:10.1111/j.1365-2648.2004.03247.x
13. Sadek EH, Elsayh KI, Mohammed FZ, Mohamed NT, Faheem S. Effect of an educational program on self-efficacy of adolescents with thalassemia major. Assiut Sci Nurs J. 2020;8(22):72–85. doi:10.21608/asnj.2020.87263
14. Borimnejad L, Parvizy S, Haghaani H, Sheibani B. The effect of family-centered empowerment program on self-efficacy of adolescents with thalassemia major: a randomized controlled clinical trial. Int J Community Based Nurs Midwifery. 2018;6(1):29–38.
15. Kim S, Tridane A. Thalassemia in the United Arab Emirates: why it can be prevented but not eradicated. PLoS One. 2017;12(1):e0170485. doi:10.1371/journal.pone.0170485
16. Bazi A, Sargazi-aval O, Safa A, Miri-moghaddam E. Health-related quality of life and associated factors among thalassemia major patients, southeast of Iran. J Pediatr Hematol Oncol. 2017;39(7):513–517. doi:10.1097/MPH.0000000000000963
17. Wang M, Huang M, Hong Y. Psychological intervention in children with transfusion-dependent β-thalassaemia. Vox Sang. 2022;117(3):386–392. doi:10.1111/vox.13201
18. Pouraboli B, Abedi HA, Abbaszadeh A, Kazemi M. Self-care in Patient with Major Thalassemia: a Grounded Theory. J Caring Sci. 2017;6(2):127–139. doi:10.15171/jcs.2017.013
19. Hassan SME, Azzab Seshi E. Study of the health instructions effect on quality of life and psychological problems among children with thalassemia. Int J Stud Nurs. 2016;1(1):16. doi:10.20849/ijsn.v1i1.92
20. Sawicki GS, Ostrenga J, Petren K, et al. Risk factors for gaps in care during transfer from pediatric to adult cystic fibrosis programs in the United States. Ann Am Thorac Soc. 2018;15(2):234–240. doi:10.1513/AnnalsATS.201705-357OC
21. Manwani D, Doyle MH, Davidson L, et al. Transition navigator intervention improves transition readiness to adult care for youth with sickle cell disease. Acad Pediatr. 2022;22(3):422–430. doi:10.1016/j.acap.2021.08.005
22. Manwani D, Doyle MH, Davidson L, et al. Health-related quality of life in adults with transfusion-independent thalassaemia intermedia compared to regularly transfused thalassaemia major: new insights. Am J Hematol. 2017;43(4):848–850. doi:10.1186/s40064-016-3568-4
23. Lapp V, Chase SK. How do youth with cystic fibrosis perceive their readiness to transition to adult healthcare compared to their Caregivers’ views? J Pediatr Nurs. 2018;43:104–110. doi:10.1016/j.pedn.2018.09.012
24. Hunt WR, Linnemann RW, Middour-Oxler B. Transition planning for chronic illnesses in the time of COVID-19. J Patient Exp. 2020;7(6):848–850. doi:10.1177/2374373520978875
25. Akcalı A, Yıldız MS, Akcalı Z, et al. Periodontal condition of patients with Thalassemia Major: a systematic review and meta-analysis. Arch Oral Biol. 2019;102(2):113–121. doi:10.1016/j.archoralbio.2019.04.004
26. Saha R, Misra R, Saha I. Health related quality of life and its predictors among Bengali thalassemic children admitted to a tertiary care hospital. Indian J Pediatr. 2015;82(10):909–916. doi:10.1007/s12098-014-1670-6
27. Mardhiyah A, Panduragan SL, Mediani HS. Reducing psychological impacts on children with chronic disease via family empowerment: a scoping review. Healthcare. 2022;10(10):2034. doi:10.3390/healthcare10102034
28. Lappalainen P, Pakkala I, Strömmer J, Sairanen E, Kaipainen K, Lappalainen R. Supporting parents of children with chronic conditions: a randomized controlled trial of web-based and self-help ACT interventions. Internet Interv. 2021;24:100382. doi:10.1016/j.invent.2021.100382
29. Blake H, Yildirim M, Wood B, et al. Covid-well: evaluation of the implementation of supported wellbeing centres for hospital employees during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(24):1–22. doi:10.3390/ijerph17249401
30. Elliott T, Tong I, Sheridan A, Lown BA. Beyond convenience: patients’ perceptions of physician interactional skills and compassion via telemedicine. Mayo Clin Proc Innov Qual Outcomes. 2020;4(3):305–314. doi:10.1016/j.mayocpiqo.2020.04.009
31. Forni GL, Puntoni M, Boeri E, Terenzani L, Balocco M. The influence of treatment in specialized centers on survival of patients with thalassemia major. Am J Hematol. 2009;84(5):317–318. doi:10.1002/ajh.21398
32. Musallam KM, Khoury B, Abi-Habib R, et al. Health-related quality of life in adults with transfusion-independent thalassaemia intermedia compared to regularly transfused thalassaemia major: new insights. Eur J Haematol. 2011;87(1):73–79. doi:10.1111/j.1600-0609.2011.01623.x
33. Cramm JM, Strating MMH, Sonneveld HM, Nieboer AP. The longitudinal relationship between satisfaction with transitional care and social and emotional quality of life among chronically ill adolescents. Appl Res Qual Life. 2013;8(4):481–491. doi:10.1007/s11482-012-9209-3
34. Elsayed LA. Nursing guidelines for children suffering from beta thalassemia. Int J Nurs Sci. 2015;5(4):131–135. doi:10.5923/j.nursing.20150504.02
35. Az-zahra WF, Mardhiyah A, Nurhidayah I. The depression categories of adolescent with beta-thalassemia major. J Nurs Care. 2019;2(1). doi:10.24198/jnc.v2i1.20162
36. Madmoli Y, Majin SA, Rahmati P, Khodadadi M. Health-related Quality of Life of Young Adult with beta-Thalassemia. Sci J Nurs. 2019;4(4):66–75.
37. Peterson J, Pearce PF, Ferguson LA, Langford CA. Understanding scoping reviews: definition, purpose, and process. J Am Assoc Nurse Pract. 2017;29(1):12–16. doi:10.1002/2327-6924.12380
38. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi:10.7326/M18-0850
39. Bradbury-Jones C, Aveyard H, Herber OR, Isham L, Taylor J, O’Malley L. Scoping reviews: the PAGER framework for improving the quality of reporting. Int J Soc Res Methodol. 2021;00(00):1–14. doi:10.1080/13645579.2021.1899596
40. Page MJ. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021. doi:10.1136/bmj.n71
41. Rafii Z, Ahmadi F, Nourbakhsh SMK. The effects of an orientation program on quality of life of patients with thalassemia: a quasi-experimental study. J Caring Sci. 2016;5(3):223–229. doi:10.15171/jcs.2016.024
42. Salehipour S, Ghaljeh M, Navidian A, Sarani H. Impact of continuous care model on the quality of life of patients with Thalassemia major: a clinical trial study. Evid Based Care J. 2021;10(4):59–66. doi:10.22038/ebcj.2021.56920.2488
43. Jabbarifard F, Sharifi T, Solati K, Ghazanfari A. The effectiveness of acceptance and commitment therapy on perceived stress, resilience, and the quality of life in thalassemia major patients. J Shahrekord Univ Med Sci. 2019;21(2):91–97. doi:10.34172/jsums.2019.16
44. Taheri P, Nooryan K, Karimi Z, Zoladl M. Effect of individual psychotherapy with a focus on self-efficacy on quality of life in patients with thalassemia major: a clinical trial. J Clin Care Skin. 2020;1(2):49–54. doi:10.52547/jccs.1.2.49
45. Madmoli Y, Akhaghi Dezfuli SM, Adavi A, Maraghi E, Heidari-Soureshjani R, Madmoli M. The effect of orem self-care on mental health of patients with thalassemia major. J Clin Nurs Midwifery. 2018;7(2):108–115.
46. Dehnoalian A, Madadkar S, Alaviani M, Motamedi Z, Ahmadpour S, Banan-Sharifi M. The impact of educational counseling program on quality of life of thalassemia patients. Jundishapur J Chronic Dis Care. 2017. doi:10.5812/jjcdc.55980
47. El-Said Zaghamir D, Hanie El-Kazaz R, Ahmed Khalil Morsy A, Ahmed Elmazahy M. Impact of educational program about iron chelation therapy on the quality of life for thalassemic children. Port Said Sci J Nurs. 2019;6(3):33–49. doi:10.21608/pssjn.2019.66511
48. Abu Samra O, Auda W, Kamhawy H, Al-Tonbary Y. Impact of educational programme regarding chelation therapy on the quality of life for B-thalassemia major children. Hematology. 2015;20(5):297–303. doi:10.1179/1607845414Y.0000000197
49. Tarım HŞ, Öz F. Thalassemia Major and Associated Psychosocial Problems: a Narrative Review. Iran J Public Health. 2022;51(1):12–18. doi:10.18502/ijph.v51i1.8287
50. Nassim MS, Mahmoud MA, Abu Shady H, Mohammed EAER. Assessment of disease knowledge gaps among beta thalassemia major patients and their caregivers. Egypt Pediatr Assoc Gaz. 2022;70(1):49. doi:10.1186/s43054-022-00143-w
51. Agarwal PK, Xie H, Sathyapalan Rema AS, et al. Evaluation of the ages and stages questionnaire (ASQ 3) as a developmental screener at 9, 18, and 24 months. Early Hum Dev. 2020:147. doi:10.1016/j.earlhumdev.2020.105081
52. Septyana G, Mardhiyah A, Widianti E. The mental burden of parents of children with thalassemia. J Keperawatan Padjadjaran. 2019;7(1):93–100. doi:10.24198/jkp.v7i1.1154
53. Miri-Aliabad G, Fadaee M, Khajeh A, Naderi M. Marital status and fertility in adult Iranian patients with β-thalassemia major. Indian J Hematol Blood Transfus. 2016;32(1):110–113. doi:10.1007/s12288-015-0510-9
54. Borhani F, Najafi MK, Rabori ED, Sabzevari S. The effect of family-centered empowerment model on quality of life of school-aged children with thalassemia major. Iran J Nurs Midwifery Res. 2011;16(4):292–298.
55. Thiyagarajan A, Bagavandas M, Kosalram K. Assessing the role of family well-being on the quality of life of Indian children with thalassemia. BMC Pediatr. 2019;19(1):1–6. doi:10.1186/s12887-019-1466-y
56. Yosep I, Hikmat R, Mardhiyah A. Types of digital-based nursing interventions for reducing stress and depression symptoms on adolescents during COVID-19 pandemic: a scoping review. J Multidiscip Healthc. 2023;16:785–795. doi:10.2147/JMDH.S406688
57. Mohammadi S, Tajvidi M, Ghazizadeh S. The relationship between spiritual well-being with quality of life and mental health of young adults with beta-thalassemia major. Sci J Iran Blood Transfus Organ. 2014;11:1.
58. Klaassen RJ. Introducing the tran qol: a new disease-specific quality of life measure for children and adults with thalassemia major. J Blood Disord Transfus. 2013;4(4). doi:10.4172/2155-9864.1000150
59. Roche M, Diers D, Duffield C, Catling-Paull C. Violence toward nurses, the work environment, and patient outcomes. J Nurs Scholarsh. 2010;42(1):13–22. doi:10.1111/j.1547-5069.2009.01321.x
60. Yosep I, Hikmat R, Mardhiyah A. Nursing intervention for preventing cyberbullying and reducing its negative impact on students: a scoping review. J Multidiscip Healthc. 2023;16:261–273. doi:10.2147/JMDH.S400779
61. Tajvidi M, Zeighmi Mohammadi S. The level of loneliness, hopelessness and self-esteem in major thalassemia adolescents. Sci J Iran Blood Transfus Organ. 2012;9(1):36–43.
62. Ghaljeh M, Salarzehi FK, Salehipour S. The effect of benson relaxation technique on anxiety and quality of life in patients with thalassemia major: a clinical trial. Indian J Hematol Blood Transfus. 2023. doi:10.1007/s12288-023-01633-6
63. Razzazan N, Ravanipour M, Jahanpour F, Zarei AR, Motamed N, Hosseini S. Investigating challenges facing self-management empowerment education in adolescents and youths with major thalassemia. Jundishapur J Chronic Dis Care. 2015;3(4). doi:10.17795/jjcdc-23366
64. Rashid MA, Ul H, Abbasi SURS. Theorizing beta thalassemia major: an overview of health sociology. Int Multidiscip J Soc Sci. 2020;9(1 SE–Articles):51–75. doi:10.17583/rimcis.2020.5113
65. Kharyal R, Kumari V, Mrunalini VT, Naik M, Joshi P, Seth T. Disease knowledge and general self-efficacy among adolescents with thalassemia major and their parents’ perspective. Indian J Hematol Blood Transfus. 2021;37(2):280–286. doi:10.1007/s12288-020-01335-3
66. Yang E, Schamber E, Meyer RML, Gold JI. Happier healers: randomized controlled trial of mobile mindfulness for stress management. J Altern Complement Med. 2020;24(5):505–513. doi:10.1089/acm.2015.0301
67. Arch JJ, Mitchell JL, Genung SR, Fisher R, Andorsky DJ, Stanton AL. A randomized controlled trial of a group acceptance-based intervention for cancer survivors experiencing anxiety at re-entry (‘Valued Living’): study protocol. BMC Cancer. 2019;19(1):89. doi:10.1186/s12885-019-5289-x
68. Farb NAS, Anderson AK, Segal ZV. The mindful brain and emotion regulation in mood disorders. Can J Psychiatry. 2012;57(2):70–77. doi:10.1177/070674371205700203
69. Morris JH, Kelly C, Joice S, et al. Art participation for psychosocial wellbeing during stroke rehabilitation: a feasibility randomised controlled trial. Disabil Rehabil. 2019;41(1):9–18. doi:10.1080/09638288.2017.1370499
70. Tagai EK, Miller SM, Hudson V, et al. Improved cancer coping from a web-based intervention for prostate cancer survivors: a randomized controlled trial. Psychooncology. 2021;30(9):1466–1475. doi:10.1002/pon.5701
71. Şahın H, Naz İ, Karadeniz G, Süneçlı O, Polat G, Ediboğlu O. Effects of a home-based pulmonary rehabilitation program with and without telecoaching on health-related outcomes in COVID-19 survivors: a randomized controlled clinical study. J Bras Pneumol Publicacao da Soc Bras Pneumol e Tisilogia. 2023;49(1):e20220107. doi:10.36416/1806-3756/e20220107
72. Behdani F, Badiee Z, Hebrani P, et al. Psychological aspects in children and adolescents with major thalassemia: a case-control study. Iran J Pediatr. 2015;25(3):0–7. doi:10.5812/ijp.25(3)2015.322
73. Gupta J, Falb KL, Ponta O, et al. A nurse-delivered, clinic-based intervention to address intimate partner violence among low-income women in Mexico City: findings from a cluster randomized controlled trial. BMC Med. 2017;15(1):128. doi:10.1186/s12916-017-0880-y
74. Eren R, Karışmaz A, Aslan C, et al. Beta thalassemia minor: patients are not tired but depressed and anxious. Med Princ Pract Int J Kuwait Univ Heal Sci Cent. 2021;30(1):69–72. doi:10.1159/000508981
75. Seyedifar M, Dorkoosh FA, Hamidieh AA, et al. Health-related quality of life and health utility values in beta thalassemia major patients receiving different types of iron chelators in Iran. Int J Hematol Stem Cell Res. 2016;10(4):224–231.
76. Boonchooduang N, Louthrenoo O, Choeyprasert W, Charoenkwan P. Health-related quality of life in adolescents with thalassemia. Pediatr Hematol Oncol. 2015;32(5):341–348. doi:10.3109/08880018.2015.1033795
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
