Back to Journals » Substance Abuse and Rehabilitation » Volume 15
Not Two Sides of the Same Coin: A Qualitative Comparative Analysis of Post-Treatment Abstinence and Relapse
Authors Pars E , Hirzalla F , VanDerNagel JEL , Dijkstra BAG , Schellekens AFA
Received 21 November 2023
Accepted for publication 4 March 2024
Published 16 March 2024 Volume 2024:15 Pages 9—19
DOI https://doi.org/10.2147/SAR.S447560
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rajendra Badgaiyan
Esther Pars,1– 4 Fadi Hirzalla,5 Joanne EL VanDerNagel,2,3,6,7 Boukje AG Dijkstra,2,8,9 Arnt FA Schellekens1,2
1Department of Psychiatry, Radboud University Medical Center, Nijmegen, the Netherlands; 2Nijmegen Institute for Scientist-Practitioners in Addiction (NISPA), Nijmegen, the Netherlands; 3Department of Human Media Interaction, University of Twente, Enschede, the Netherlands; 4Salvation Army, Ugchelen, The Netherlands; 5Department of Public Administration and Sociology, Erasmus University, Rotterdam, the Netherlands; 6Tactus Addiction Care, Deventer, the Netherlands; 7Aveleijn, Borne, the Netherlands; 8Novadic-Kentron, Vught, the Netherlands; 9Behavioral Science Institute, Radboud University, Nijmegen, the Netherlands
Correspondence: Esther Pars, Department of Psychiatry, Radboud University Medical Center, PO Box 9101, Nijmegen, 6500 HB, the Netherlands, Tel +31 24 361 35 13, Email [email protected]
Purpose: Substance use disorder (SUD) can be a chronic relapsing condition with poor treatment outcomes. Studies exploring factors associated with abstinence or relapse after treatment are often quantitative in nature, applying linear statistical approaches, while abstinence and relapse result from non-linear, complex, dynamic and synergistic processes. This study aims to explore these underlying dynamics using qualitative comparative analysis (QCA) as a mixed methods approach to further our understanding of factors contributing to post-treatment abstinence and relapse.
Patients and Methods: In a prospective study, we gathered both qualitative and quantitative data pertaining to post-treatment substance use and the factors linked to substance use outcomes. These factors encompassed psychiatric comorbidity, intellectual disability, social disintegration, post-treatment support, and engagement in activities among patients who had undergone inpatient treatment for severe SUD (n = 58). QCA, a set-theoretic approach that considers the complex interplay of multiple conditions, was applied to discern which factors were necessary or sufficient for the occurrence of either abstinence or relapse.
Results: We found two solutions predicting abstinence, and five for relapse. Post-treatment conditions (support and engagement in activities) were important for retaining abstinence. For relapse, individual baseline characteristics (intellectual disability, social disintegration, psychiatric comorbidity) combined with (post-)treatment factors (post-treatment support, activities) were important.
Conclusion: Although abstinence and relapse represent opposing outcomes, they each exhibit distinct dynamics. To gain a comprehensive understanding of these dynamics, it is advisable to examine them as separate outcomes. For clinical practice, it can be worthwhile to recognize that fostering the conditions conducive to abstinence may differ from preventing the factors that trigger relapse.
Plain Language Summary: This study explores why some people who struggle with addiction stay clean after treatment, while others relapse. Previous studies often used traditional statistical methods, with inconclusive results due to their inability to capture the complexity of this process. To address this, we used a different approach called qualitative comparative analysis (QCA).
We collected information from 58 individuals who received inpatient treatment for their addiction. We looked at different factors like mental health problems, intellectual disability, the support they got from professionals and their social network, and whether they kept themselves busy with activities. We investigated how these factors are related to staying clean or relapse. With the help of QCA, we analyzed how these factors work together to cause either drug-free living or relapse.
We found that staying clean was strongly linked to getting support after treatment and being involved in activities like hobbies or work. On the other hand, relapse was more likely in people with personal problems, like intellectual disabilities and mental health problems, when support and activities were lacking after treatment.
In summary, our study indicates that staying clean and relapse are different processes with different factors at play. Helping someone stay clean may therefore require different strategies than preventing relapse. This insight can guide development of more personalized healthcare for individuals dealing with addiction.
Keywords: addiction, substance use outcomes, qualitative comparative analysis
Introduction
Substance use disorder (SUD) is a multifaceted public health problem that impacts individuals and communities worldwide.1 High relapse rates pose a significant challenge in the recovery process from SUD, with one-year rates ranging between 40 and 60%.2,3 Relapse can have severe negative health, psychosocial, legal, and economic consequences,4,5 whereas abstinence can facilitate recovery.6,7
Numerous studies have explored biological, genetic, psychological, and environmental factors that may predict post-treatment abstinence or relapse,5,8–16 showing inconclusive results.10 For instance, while most studies link psychiatric co-morbidity to an increased relapse risk,17,18 some studies suggest a reduced risk.10,19 This highlights the inherent complexity of post-treatment substance use outcomes that arise from a dynamic interplay of multiple factors over time.9,20,21
While conventional statistical methods are valuable for assessing the impact of interaction effects on abstinence and relapse, their primary emphasis on average effects presents challenges in comprehending the intricate and synergistic nature of the factors that lead to these outcomes on an individual level.22–24 Qualitative comparative analysis (QCA) is a multi-method set-theoretic approach that differs from conventional statistical methods, as it aims to identify and explain the specific combinations of factors that contribute to particular outcomes.25 QCA examines how multiple conditions interact to produce an outcome, similar to a “causal recipe” (conjunctural causation), and whether different conditions or combinations of conditions can explain the same outcome (equifinality). Further, with QCA, it is possible to determine whether and how conditions operate differently in causing an outcome across different cases. Lastly, QCA enables the identification of causal asymmetry, meaning that the conditions leading to an outcome, like abstinence, are not merely the opposite of the conditions leading to the non-occurrence of an outcome, like relapse. In a service innovation study by Ordanini et al,26 QCA has already demonstrated its ability to identify intricate configuration effects that could not be captured fully by using conventional interaction effects. Through the application of QCA, we aim to explore the (combinations of) conditions that result in abstinence or relapse. By adopting this comprehensive approach, we aim to contribute to a deeper understanding of the complex and interrelated factors influencing post-treatment substance use outcomes.
Methods
Setting and Sample
From September 2020 to October 2022, we collected qualitative and quantitative data at a Salvation Army SUD treatment facility in The Netherlands that tailors to individuals with SUD and comorbidities. Participants were enrolled in an inpatient treatment program based on the Community Reinforcement Approach (CRA), of either 12 or 28 weeks. Intended length of treatment was determined by the availability of financing from the Social Support Act (WMO), not on problem severity.
All patients entering treatment were considered eligible to participate in this study. However, for the purpose of conducting the QCA analysis, only patients with a complete dataset, comprising both baseline and follow-up measurements, were included (see Figure 1). QCA was designed for medium-sized samples,27 and our inclusion process continued until we reached a sufficiently large sample (n = 58) that exhibited variability in both the conditions and outcome measures. This study received approval from the regional ethical board under the reference number 2020–6837.
 |
Figure 1 Inclusion process. |
Outcomes and Conditions
Our outcomes of interest were abstinence and relapse. We defined abstinence by the number of days without (self-reported) substance use during the 30-day period leading up to the three-month follow-up evaluation. A value of 3 out of 30 days with substance use denoted the boundary between a slip (ie, a temporary setback after which abstinence is resumed) and full relapse.
To identify theoretically relevant conditions for our study, we followed the methodology of Goicolea et al28 by conducting a literature review. This resulted in a list of 48 potential conditions, out of which 40 were considered feasible and relevant for our study. Within QCA, it is advised to avoid models with more than seven causal conditions, as these become highly challenging to interpret given the large number of parameters involved.29 Therefore, we aimed to limit our conditions to a maximum of seven, which would also comfortably meet the criteria for sample size. This criterion is linked to the number of conditions, and seven conditions require at least 30 cases to establish a reliable model.30
To refine our selection, we analyzed the data collected from the first ten cases in our study. This allowed us to assess the relevance of each condition in this population. Conditions that were not deemed relevant to our cases were omitted. Through this iterative process, we reduced the number of conditions to seven, balancing individual and contextual factors: psychiatric co-morbidity, mild to borderline intellectual disability (total IQ 50–85, MBID), treatment duration, post-treatment formal (eg, treatment, outpatient support) and informal (social network) support, and engagement in daily activities. We refer to Supplementary Tables 1 and 2 for a more detailed description of the selection process and to Supplementary Table 3 for definitions and measurements of these conditions.
Procedure
All patients entering treatment were approached by the researcher and fully informed. Those willing to participate signed informed consent to (1) complete questionnaires, (2) access their electronic patient files, and (3) participate in a semi-structured interview by phone 3 months post-treatment. Baseline questionnaires were administered to measure psychiatric comorbidity, MBID, and social disintegration (see Supplementary Table 3 for questionnaires). Treatment length was derived from the electronic patient files. Three-month post-treatment, researchers assessed post-treatment informal support, formal support, and daily activities with a questionnaire (see Supplementary Table 3), complemented by a semi-structured interview covering these aspects and other relevant post-treatment experiences, along with an evaluation of substance use frequency over the past 30 days.
Analysis
Included and excluded individuals were compared on key variables (age, gender, MBID, psychiatric co-morbidity, time in treatment, treatment completion). Subsequently, QCA analyses were performed with the software program fsQCA 3.0.31
Calibration
All cases (ie, patients) were assigned scores ranging from 0 to 1, indicating the degree to which they were associated with each of the conditions and the outcome. This process, called calibration, resulted in a data matrix containing the calibrated scores of all cases on all conditions and the outcome. Supplementary Table 3 gives a detailed account how calibration scores were assigned, and Supplementary Table 4 displays the full calibrated data matrix.
Truth Table
In the calibrated data matrix, each row corresponds to an individual case. To shift our focus from diversity among cases to identifying commonalities, we constructed a truth table (see Supplementary Tables 5 and 6). This truth table lists all possible combinations of conditions (ie, configurations), which cases are represented by each configuration, and how consistently the configurations co-occur with the outcome. Unlike the data matrix, which contains fuzzy scores ranging from 0 to 1, the truth table simplifies each condition and the outcome as either present (coded as 1) or absent (coded as 0). This simplification streamlines the evaluation of a finite number of potential condition combinations. The more detailed fuzzy calibration scores are retained for the development and assessment of the minimal formula (ie, the resulting model). To construct the truth table, the software matched cases with rows that best represented their blend of present and absent conditions. It proceeded to calculate a consistency value for each row, indicating the portion of cases that exhibit both the configuration and the outcome.
Logical Minimization
The truth table was reviewed, and redundant conditions were removed through logical minimization (Quine-McCluskey algorithm). Redundancy occurs when a condition can be both present and absent with the outcome. For example, if informal support can be both present and absent in relation to the outcome abstinence, this condition may be considered redundant.
To make our results more concise, we incorporated theoretically informed directional expectations (similar to hypotheses) into the logical minimization process. This approach considers combinations of conditions that might not be observed in the dataset but are logically and theoretically plausible. Specifically, we expected that the absence of psychiatric co-morbidity, MBID, and/or social disintegration, along with the presence of formal and informal support and/or engagement in daily activities, would promote abstinence. In the case of predicting relapse, we reversed these expectations. We maintained a neutral stance on the condition “long treatment” because we hypothesized that the ideal duration of treatment depends on the severity or complexity of the problem.32 As such, it may contribute to abstinence or relapse in both present and absent form.
Assessing the Solutions
Before tending to the results of logical minimization, we first assessed whether conditions or combinations of conditions were necessary for the outcome (see Figure 2). If a case does not have a necessary condition, it cannot have the outcome. The lower threshold for necessity was set at 0.9 (a score of 1 would indicate presence of the condition at all times when the outcome is present).
 |
Figure 2 Necessity (left) and sufficiency (right). |
We then proceeded to the results from our logical minimization. Logical minimization produces three models – or in QCA terms, solutions: the complex, parsimonious and intermediate solution. In the current paper, we focused on the intermediate solution, as it balances complexity and conciseness.33,34 The solutions resulting from the performed logical minimization indicate which conditions or combinations of conditions are sufficient for (ie, lead to) the outcome abstinence or, respectively, relapse (see Figure 2).
Our solution was further evaluated with two parameters of fit, solution consistency and solution coverage (see Figure 3). Consistency indicates the extent to which the solution or parts of the solution are a consistent subset of the outcome (ie, co-occur with the outcome). As such, it indicates explanatory power. The lower threshold for consistency was set at 0.8. Solution coverage indicates the extent to which the entire solution and its components explain the outcome of interest. As such, it indicates the level of empirical relevance. There is no established lower threshold for coverage, as solutions with low coverage can still be relevant.
 |
Figure 3 Consistency and coverage. (A) Low consistency, low coverage. (B) High consistency, low coverage. (C). High consistency, high coverage. |
The different parts of the solution (solution terms) were also evaluated on their level of consistency, and two types of coverage: raw and unique coverage. Raw coverage indicates the relative importance of a solution term (which proportion of the outcome is covered by the solution term?), and unique coverage controls for overlap (how much of the outcome is uniquely explained by the solution term?).
Results
Participants (n = 58) were on average 44 years old, with 91.4% being male, and the majority having psychiatric comorbidities, MBID and experiencing social disintegration, see Table 1. Included participants were slightly older than excluded participants (t(120) = −3.044, p < 0.003), see Supplementary Table 7.
 |
Table 1 Baseline Characteristics |
Necessity
For both abstinence and relapse, we could not identify single necessary conditions (see Table 2). Nevertheless, we observed near-necessary consistency scores of 0.89 for the presence of informal support and 0.87 for engagement in activities, indicating their importance in achieving abstinence.
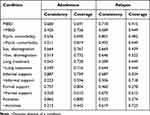 |
Table 2 Results necessity analysis (Single Conditions) |
Additionally, we evaluated the occurrence of necessary combinations of conditions, which resulted in several sets of necessary OR-combinations (see Supplementary Table 8 for an overview). In an OR-combination, the outcome depends on at least one condition; not all conditions need to occur simultaneously. For abstinence, we found necessary OR-combinations consisting of (post)treatment conditions, with the most consistent combination being activities+informal support (consistency 0.956, coverage 0.740). For relapse, we identified combinations involving at least 3 conditions, all consisting of at least two baseline conditions. The most consistent necessary combination included MBID+Psychiatric comorbidity+~Activities (consistency 0.951, coverage 0.429).
Sufficiency
Two combinations of conditions were sufficient for the outcome abstinence, and five for the outcome relapse (Table 3).
 |
Table 3 Intermediate Solution for Abstinence and Relapse |
Abstinence
The intermediate solution for abstinence was a highly consistent subset of the outcome (0.90), indicating that it was firmly supported by the empirical data. The solution accounted for 59% of this outcome (coverage 0.59). The first solution term (A) – presence of baseline social disintegration, post-treatment support (formal and informal), and daytime activities – was the most prevalent (raw coverage 0.51, n = 20), highly consistent (0.90), and showed a unique coverage of 0.30. The second solution (B) – the absence of psychiatric comorbidity and social disintegration at baseline, absence of long treatment, and informal support and activities post treatment – was less prevalent (raw coverage 0.28, n = 4), but still highly consistent (0.87). However, the unique coverage was low (0.08), suggesting it explains a smaller portion of the outcome independently.
The most prevalent solution term for abstinence (A) was best exemplified by case 17 and 28. Both males had SUD for over 30 years, experienced traumatic childhoods, social disintegration and periods of homelessness. Neither had MBID, and both underwent SUD treatment multiple times in the past. Only case 17 scored above the clinical threshold for psychiatric comorbidity. Case 17 spent 36.5 weeks in treatment, and case 28 only 8. After treatment, both men lived in sheltered housing, received intensive professional support, and participated in daily activities. Case 28 expressed a desire for more work opportunities, and case 17 a need for additional formal support from a psychologist. Following treatment, both men received ample informal support, mostly from their families. Case 17, who previously had a (self-proclaimed) “useless” social life, was able to reconnect with his family during treatment. Conversely, case 28 already had a social network and did not require further support in this regard. Both reported that contemplating the consequences of relapse for themselves and their loved ones was enough to avoid substance use.
Relapse
The intermediate solution for relapse was slightly less fitting, compared to the solution for abstinence. Consistency was high (0.87), and the solution explained 45% of the outcome relapse (coverage 0.45). The solution consisted of five solution terms (raw coverage 0.25–0.32, n = 2–5), which showed high levels of overlap, as evidenced by multiple cases being represented in more than one solution term and indicated by low levels of unique coverage (0.01–0.04).
The first two solution terms (A, B) identified that the presence of either MBID or psychiatric comorbidity, combined with the absence of long treatment, support (formal and informal), and activities, was sufficient for relapse. The third solution term (C), which was the most prevalent, indicated that a triple diagnosis (SUD, MBID, psychiatric comorbidity) in conjunction with the absence of long treatment, formal support, and activities, was sufficient for relapse. The fourth solution term (D) showed that the presence of social disintegration and psychiatric comorbidity, along with the absence of post-treatment support (formal and informal) and activities, was sufficient for relapse. Lastly, solution term (E) stated that the presence of social disintegration, MBID, and long treatment, coupled with the absence of post-treatment formal support and activities, was sufficient for relapse.
The solution for relapse is best illustrated by case 12, who is covered by all solution terms. Case 12 had a SUD, spanning over three decades, a history of homelessness, and he scored well above the threshold for psychiatric comorbidity and social disintegration. He began a 28-week treatment program, which was discontinued by the clinic after seven weeks. Relapse occurred two weeks after leaving treatment and soon escalated into daily use. After a few temporary living arrangements, he finally settled into a rented room.
Post-treatment, case 12 reported receiving no formal support, and he was on a waiting list for SUD treatment. He had no daytime activities, often felt bored and had a very small informal social network. Although his sister visited him once a week, he reported feeling lonely most of the time.
Discussion
This study used qualitative comparative analysis (QCA) to explore the baseline, treatment, and post-treatment conditions leading to post-treatment abstinence and relapse in patients with SUD. Necessity analysis revealed no single necessary condition for either abstinence or relapse. However, the presence of informal support and engagement in activities were identified as important (near-necessary) conditions for abstinence. Additional necessity analyses found several necessary OR-combinations. For abstinence, these primarily involved (post-)treatment conditions, with the most consistent combination being activities+informal support. Relapse required at least three conditions, including two or more baseline conditions, with the most consistent combination involving MBID+psychiatric comorbidity+~activities.
Sufficiency analyses revealed seven distinct causal pathways, providing insight into the “causal recipes” leading to either abstinence or relapse. These pathways revealed that socially disintegrated individuals relied on comprehensive post-treatment conditions (formal support, informal support, engagement in activities) to remain abstinent, while those without baseline social disintegration and psychiatric comorbidity (without differentiating between different disorders) benefited from short treatment combined with less comprehensive aftercare (informal support, engagement in activities). For relapse, the pathways consistently showed an absence of formal support and activities, frequently coupled with absent informal support. However, there were considerable variations in baseline and treatment conditions across the different solution terms for relapse.
While previous studies often linked abstinence to the absence of baseline conditions related to relapse,36–40 we only observed this pattern in the least prevalent configuration for abstinence—specifically, among patients without social disintegration and psychiatric comorbidity. Surprisingly, our study found that the most prevalent configuration for achieving abstinence included the presence of social disintegration. This suggests that socially disintegrated individuals can achieve and maintain abstinence if post-treatment conditions are beneficial.
Treatment duration was counterintuitively related to abstinence and relapse. While short treatment duration featured in both the abstinence and relapse solution, long treatment was exclusively related to relapse. Although longer treatment duration predicted sustained abstinence in several other studies,41–45 our study may reflect the interplay between baseline conditions and treatment duration: individuals with less severe baseline issues tended to benefit from shorter treatment durations, whereas those with pre-existing baseline conditions were more prone to relapse after short treatment. This finding aligns with scholars advocating “matched care”, ie, tailoring treatment intensity and duration to the individuals’ problem severity and specific needs.32,46 Nonetheless, it remains interesting that the final solution term (E) for relapse demonstrated that patients with MBID and social disintegration experienced relapse after long treatment duration, particularly in the absence of formal support and engagement in activities. This may underscore the significance of effective aftercare for this particular group, as even an extended treatment duration cannot compensate for its absence. Further research is needed to clarify this.
When evaluating post-treatment conditions (formal support, informal support, and engagement in activities) individually, our findings are in line with previous studies, associating their presence with abstinence and their absence with relapse.8,10,47–50 For individuals with baseline social disintegration, all post-treatment conditions appear to synergistically facilitate abstinence, suggesting that comprehensive aftercare, encompassing both formal and informal support, along with engagement in activities, holds promise as an effective intervention. In contrast, individuals with milder baseline issues no longer rely on formal post-treatment support as a critical factor for achieving abstinence. This implies that they may already derive sufficient benefit from informal support and engagement in activities. Conversely, relapse configurations typically involved one or more baseline conditions, in conjunction with the absence of post-treatment formal support and engagement in activities. This further highlights the significance of individualized and comprehensive care pathways that extend beyond inpatient treatment.
The different causal pathways for abstinence and relapse found in this study illustrate that these outcomes are not two sides of the same coin. This may provide an explanation for the inconclusive results observed in previous studies,10 as this “inconclusiveness’ may arise from causal asymmetry, where conditions cannot be simply reversed to reverse the outcome. Future studies should heed Glaesser”s51 advise and analyze abstinence and relapse outcomes separately. Furthermore, they should consider the intricate interplay of baseline, treatment, and post-treatment conditions, rather than exclusively concentrating on individual conditions. From a clinical perspective, it is crucial to recognize that fostering conditions for abstinence can diverge from preventing factors that trigger relapse. In light of this, McKay52 advises enhancing the appeal and effectiveness of the “recovery journey” by prioritizing abstinence-centered support and incentives. The Community Reinforcement Approach (CRA) is one example of a strategy that emphasizes post-treatment support and engagement in activities to promote sustained abstinence.53
Strengths and Limitations
To our knowledge, this study is the first using QCA methodology to explore post-treatment abstinence and relapse dynamics. QCA, designed to unravel complex causality in medium-sized samples,35 allowed us to shed light on these dynamics with a sample size smaller than what is typically needed for conventional statistical procedures.
It is important to note that data collection occurred amidst the Covid-19 pandemic, which may have impacted our research. Despite the fact that inpatient treatment at the Salvation Army clinic remained largely unaffected by the pandemic, the post-treatment phase for patients might have been more complicated due to restricted social interactions and interruptions in daily activities. Additional limitations include the sample size and the specific (predominantly male) population of the Salvation Army, which limits the generalizability of our findings.
Maintaining a follow-up period of only three months could also be considered a limitation, although the literature does indicate that most relapses occur within the first three months after treatment.54 Moreover, akin to more conventional modes of analysis, incorporating all potentially relevant conditions or distinguishing within our conditions was unfeasible. However, the conditions not included, such as type of psychiatric comorbidity or substances used, could also impact the causal pathways to abstinence or relapse,15,16,55 rendering any selection a partial representation of the myriad interactions among factors. Addressing this challenge may be a focus for future research. Finally, while only including participants who completed the follow-up assessment may have introduced selection bias, analysis of key variables between included and excluded participants did not reveal significant differences other than age, suggesting limited bias.
Conclusion
In our sample, post-treatment conditions were important for achieving abstinence, whereas individual baseline conditions combined with (post-)treatment conditions were important factors for relapse. As such, abstinence and relapse may not be two sides of the same coin. Each may have its own underlying unique dynamics, which can differ across contexts. To better understand these dynamics, abstinence and relapse should be studied further as separate outcomes. In clinical practice, it may be relevant to both promote abstinence alongside managing relapse.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Radboudumc (protocol code 2020-6837, August 8th 2020).
Funding
This research was funded by ZonMw, grant number 639003601.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Amundsen EJ, Bretteville-Jensen AL, Rossow I. Patients admitted to treatment for substance use disorder in Norway: a population-based case–control study of socio-demographic correlates and comparative analyses across substance use disorders. BMC Public Health. 2022;22(1):1–12. doi:10.1186/S12889-022-13199-5/FIGURES/2
2. Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: a review. Clin Psychol Rev. 2006;26(2):162–178. doi:10.1016/J.CPR.2005.11.005
3. Reichel C, Bevins R. Forced abstinence model of relapse to study pharmacological treatments of substance use disorder. Curr Drug Abuse Rev. 2009;2(2):184–194. doi:10.2174/1874473710902020184
4. Appiah R, Boakye KE, Ndaa P, Aziato L. “Tougher than ever”: an exploration of relapse prevention strategies among patients recovering from poly-substance use disorders in Ghana. Drugs. 2018;25(6):467–474. doi:10.1080/09687637.2017.1337080
5. Decker KP, Peglow SL, Samples CR, Cunningham TD. Long-term outcomes after residential substance use treatment: relapse, morbidity, and mortality. Mil Med. 2017;182(1):e1589–e1595. doi:10.7205/MILMED-D-15-00560
6. Kaskutas LA, Borkman TJ, Laudet A, et al. Elements that define recovery: the experiential perspective. J Stud Alcohol Drugs. 2014;75(6):999–1010. doi:10.15288/jsad.2014.75.999
7. Kelly JF, Hoeppner B. A biaxial formulation of the recovery construct. Addict Res Theory. 2015;23(1):5–9. doi:10.3109/16066359.2014.930132
8. Barati M, Bashirian S, Mohammadi Y, Moeini B, Mousali A, Afshari M. An ecological approach to exploring factors affecting substance use relapse: a systematic review. J Public Health. 2021. doi:10.1007/s10389-020-01412-x
9. Stillman MA, Sutcliff J Addiction and substance abuse predictors of relapse in alcohol use disorder: identifying individuals most vulnerable to relapse. Addict Subst Abuse. 1; 2020.
10. Sliedrecht W, de Waart R, Witkiewitz K, Roozen HG. Alcohol use disorder relapse factors: a systematic review. Psychiatry Res. 2019;278:97–115. doi:10.1016/J.PSYCHRES.2019.05.038
11. Sharma AK, Upadhyaya SK, Bansal P, Sharma MNDK. A study of factors affecting relapse in substance abuse. Indian J Life Sci. 2012;2(1):31–35.
12. Daughters SB, Magidson JF, Anand D, Seitz-Brown CJ, Chen Y, Baker S. The effect of a behavioral activation treatment for substance use on post-treatment abstinence: a randomized controlled trial. Addiction. 2018;113(3):535–544. doi:10.1111/ADD.14049
13. Wahler EA, Otis MD. Social stress, economic hardship, and psychological distress as predictors of sustained abstinence from substance use after treatment. Subst Use Misuse. 2014;49(13):1820–1832. doi:10.3109/10826084.2014.935789
14. Mohannan SC, Finney JW. Explaining abstinence rates following treatment for alcohol abuse: a quantitative synthesis of patient, research design and treatment effects. Addiction. 1996;91(6):787–805. doi:10.1046/j.1360-0443.1996.9167876.x
15. Marquez-Arrico J, Río-Martínez L, Navarro J, Prat G, Forero D, Adan A. Coping strategies in male patients under treatment for substance use disorders and/or severe mental illness: influence in clinical course at one-year follow-up. J Clin Med. 2019;8(11):1972. doi:10.3390/jcm8111972
16. Marquez-Arrico JE, Navarro JF, Adan A. Health-related quality of life in male patients under treatment for substance use disorders with and without major depressive disorder: influence in clinical course at one-year follow-up. J Clin Med. 2020;9(10):3110. doi:10.3390/jcm9103110
17. Schellekens AFA, de Jong CAJ, Buitelaar JK, Verkes RJ. Co-morbid anxiety disorders predict early relapse after inpatient alcohol treatment. Eur Psychiatry. 2015;30(1):128–136. doi:10.1016/j.eurpsy.2013.08.006
18. Trocchio S, Chassler D, Storbjörk J, Delucchi K, Witbrodt J, Lundgren L. The association between self-reported mental health status and alcohol and drug abstinence 5 years post-assessment for an addiction disorder in U.S. and Swedish samples. J Addict Dis. 2013;32(2):180–193. doi:10.1080/10550887.2013.795468
19. Tómasson K, Vaglum P. Antisocial addicts: the importance of additional axis I disorders for the 28-month outcome. Eur Psychiatry. 2000;15(8):443–449. doi:10.1016/S0924-9338(00)00518-6
20. Drake RE, Wallach MA, McGovern MP. Special section on relapse prevention: future directions in preventing relapse to substance abuse among clients with severe mental illnesses. Psychiatric Serv. 2005;56(10):1297–1302. doi:10.1176/appi.ps.56.10.1297
21. Durazzo TC, Meyerhoff DJ. Psychiatric, demographic, and brain morphological predictors of relapse after treatment for an alcohol use disorder. Alcohol Clin Exp Res. 2017;41(1):107–116. doi:10.1111/acer.13267
22. Fiss PC. A set-theoretic approach to organizational configurations. Acad Manage Rev. 2007;32(4):1180–1198. doi:10.5465/amr.2007.26586092
23. Fiss PC, Sharapov D, Cronqvist L. Opposites attract? Opportunities and challenges for integrating large-N QCA and econometric analysis. Polit Res Q. 2013;66(1):191–198.
24. Schneider CQ, Wagemann C. Qualitative Comparative Analysis (QCA) and fuzzy-sets: agenda for a research approach and a data analysis technique. Comp Sociol. 2010;9(3):376–396. doi:10.1163/156913210X12493538729838
25. Vis B. The comparative advantages of fsQCA and regression analysis for moderately large-N analyses. Sociol Methods Res. 2012;41(1):168–198. doi:10.1177/0049124112442142
26. Ordanini A, Parasuraman A, Rubera G. When the recipe is more important than the ingredients: a Qualitative Comparative Analysis (QCA) of service innovation configurations. J Serv Res. 2014;17(2):134–149. doi:10.1177/1094670513513337
27. Ragin CC. Fuzzy-Set Social Science. The University Of Chicago Press; 2000.
28. Goicolea I, Hultstrand Ahlin C, Waenerlund AK, et al. Accessibility and factors associated with utilization of mental health services in youth health centers. A qualitative comparative analysis in northern Sweden. Int J Ment Health Syst. 2018;12(1). doi:10.1186/s13033-018-0249-4
29. Fainshmidt S, Witt MA, Aguilera RV, Verbeke A. The contributions of qualitative comparative analysis (QCA) to international business research. J Int Bus Stud. 2020;51(4):455–466. doi:10.1057/s41267-020-00313-1
30. Marx A. Towards More Robust Model Specification in QCA; Results from a Methodological Experiment; 2006.
31. Ragin CC, Davey S Fuzzy-set/qualitative comparative analysis 3.0; 2016.
32. De Leon G, Melnick G, Cleland CM. Client matching: a severity-treatment intensity paradigm. J Addict Dis. 2008;27(3):99–113. doi:10.1080/10550880802122703
33. Cooper BR, Hill LG, Parker L, Jenkins GJ, Shrestha G, Funaiole A. Using qualitative comparative analysis to uncover multiple pathways to program sustainment: implications for community-based youth substance misuse prevention. Implement Sci Commun. 2022;3(1):1–12. doi:10.1186/S43058-022-00303-4
34. Ragin CC, Sonnett J. Between complexity and parsimony: limited diversity, counterfactual cases, and comparative analysis. In: Vergleichen in Der Politikwissenschaft. VS Verlag für Sozialwissenschaften; 2005:180–197. doi:10.1007/978-3-322-80441-9_9
35. Ragin CC. Redesigning Social Inquiry: Fuzzy Sets and Beyond. University of Chicago Press; 2008.
36. Braatveit K, Torsheim T, Hove O. The prevalence and characteristics of intellectual and borderline intellectual disabilities in a sample of inpatients with substance use disorders: preliminary clinical results. J Ment Health Res Intellect Disabil. 2018;11(3):203–220. doi:10.1080/19315864.2018.1469701
37. Copersino ML, Slayter E, McHugh RK, Shedlack KJ, Lukas SE, Weiss RD. Clinical utility of a hybrid secondary and relapse prevention program in adults with mild intellectual disability or borderline intellectual functioning in community residential and day habilitation settings. Disabil Health J. 2022;15(2). doi:10.1016/j.dhjo.2022.101293
38. Dixit S. Social support and treatment outcome in alcohol dependence syndrome in armed forces. J Clin Diagn Res. 2015. doi:10.7860/JCDR/2015/14142.6739
39. Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002;59(4):375. doi:10.1001/archpsyc.59.4.375
40. Ritsher JB, McKellar JD, Finney JW, Otilingam PG, Moos RH. Psychiatric comorbidity, continuing care and mutual help as predictors of five-year remission from substance use disorders. J Stud Alcohol. 2002;63(6):709–715. doi:10.15288/jsa.2002.63.709
41. Andersson HW, Wenaas M, Nordfjærn T. Relapse after inpatient substance use treatment: a prospective cohort study among users of illicit substances. Addict Behav. 2019;90:222–228. doi:10.1016/j.addbeh.2018.11.008
42. Broers B, Giner F, Dumont P, Mino A. Inpatient opiate detoxification in Geneva: follow-up at 1 and 6 months. Drug Alcohol Depend. 2000;58:85–92. doi:10.1016/S0376-8716(99)00063-0
43. Brunette MF, Drake RE, Woods M, Hartnett T. A comparison of long-term and short-term residential treatment programs for dual diagnosis patients. Psychiatric Serv. 2001;52(4):526–528. doi:10.1176/appi.ps.52.4.526
44. Greenfield L, Burgdorf K, Chen X, Porowski A, Roberts T, Herrell J. Effectiveness of long‐term residential substance abuse treatment for women: findings from three national studies. Am J Drug Alcohol Abuse. 2004;30(3):537–550. doi:10.1081/ADA-200032290
45. Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychol Addict Behav. 1997;ll:261.
46. Finney JW, Moos RH, Wilbourne PL. Effects of treatment setting, duration, and amount on patient outcomes. In: Ries RK, Fiellin DA, Miller SC, editors. Principles of Addiction Medicine.
47. Magidson JF, Andersen LS, Satinsky EN, et al. “Too much boredom isn’t a good thing”: adapting behavioral activation for substance use in a resource-limited South AfricanHIV care setting. Psychotherapy. 2020;57(1):107–118. doi:10.1037/pst0000257
48. Nolte-Troha C, Roser P, Henkel D, Scherbaum N, Koller G, Franke AG. Unemployment and substance use: an updated review of studies from North America and Europe. Healthcare. 2023;11(8):1182. doi:10.3390/healthcare11081182
49. Rollins AL, O’Neill SJ, Davis KE, Devitt TS. Special section on relapse prevention: substance abuse relapse and factors associated with relapse in an Inner-City Sample of patients with dual diagnoses. Psychiatric Serv. 2005;56(10):1274–1281. doi:10.1176/appi.ps.56.10.1274
50. Xie H, McHugo GJ, Fox MB, Drake RE. Special section on relapse prevention: substance abuse relapse in a ten-year prospective follow-up of clients with mental and substance use disorders. Psychiatric Serv. 2005;56(10):1282–1287. doi:10.1176/appi.ps.56.10.1282
51. Glaesser J. Analysing causal asymmetry: a comparison of logistic regression and Qualitative Comparative Analysis (QCA). Int J Soc Res Methodol. 2023. doi:10.1080/13645579.2022.2163106
52. McKay JR. Making the hard work of recovery more attractive for those with substance use disorders. Addiction. 2017;112(5):751–757. doi:10.1111/ADD.13502
53. Meyers RJ, Roozen HG, Smith JE. The community reinforcement approach: an update of the evidence. Alcohol Res Health. 2011;33(4):380.
54. Nordfjærn T. Relapse patterns among patients with substance use disorders. J Subst Use. 2011;16(4):313–329. doi:10.3109/14659890903580482
55. Calabria B, Degenhardt L, Briegleb C, et al. Systematic review of prospective studies investigating “remission” from amphetamine, cannabis, cocaine or opioid dependence. Addict Behav. 2010;35(8):741–749. doi:10.1016/j.addbeh.2010.03.019
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
