Back to Journals » Nature and Science of Sleep » Volume 14
Non-Right Handedness is Associated with More Time Awake After Sleep Onset and Higher Daytime Sleepiness Than Right Handedness: Objective (Actigraphic) and Subjective Data from a Large Community Sample
Authors Taubert H, Schroeter ML, Sander C, Kluge M
Received 14 January 2022
Accepted for publication 7 April 2022
Published 5 May 2022 Volume 2022:14 Pages 877—890
DOI https://doi.org/10.2147/NSS.S358352
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Hilde Taubert,1 Matthias L Schroeter,2– 4 Christian Sander,1,4,* Michael Kluge1,*
1Department of Psychiatry and Psychotherapy, University of Leipzig, Leipzig, Germany; 2Department of Neurology, Max Planck Institute for Human Cognitive and Brain Sciences, Leipzig, Germany; 3Clinic for Cognitive Neurology, University Hospital Leipzig, Leipzig, Germany; 4Leipzig Research Center for Civilization Diseases, University of Leipzig, Leipzig, Germany
*These authors contributed equally to this work
Correspondence: Michael Kluge, Department of Psychiatry and Psychotherapy University of Leipzig, Semmelweisstr 10, Leipzig, 04103, Germany, Tel +49 341/97 24673, Fax +49 341/97 24539, Email [email protected]
Purpose: Handedness has been linked to various physiological and pathological phenomena including memory function and psychiatric disorders. Also for sleep, several studies have reported associations. However, large-scale studies including a broad age span of participants and studies analyzing women and men separately are lacking.
Methods: Therefore, objective sleep data were determined using at-home actigraphy from 1764 healthy participants (18 to 80 years, 908 women), averaging five consecutive nights. In addition, subjective sleep-related data were captured by self-report diaries, the Pittsburgh Sleep Quality Index (PSQI), the Epworth Sleepiness Scale (ESS) and the Morningness-Eveningness-Questionnaire (MEQ). Handedness was determined with the Edinburgh Handedness Inventory (EHI) providing information on the direction (left vs right) and the degree of handedness (strong vs weak). To address the potential endocrine effects, premenopausal women (≤ 45 years) and postmenopausal women (≥ 55 years) were analyzed separately. This was also done for men.
Results: The degree and direction of handedness were correlated with “wake after sleep onset” (WASO) in the total sample and all women (the more right-handed/lateralized the shorter WASO). In postmenopausal women, additionally, time in bed (TIB) and total sleep time (TST) were correlated. There were no other significant associations between an objective sleep variable and handedness. In both premenopausal women and > 55-year-old men subjective quality of sleep (PSQI) was correlated with direction and degree of handedness (the more right-handed/lateralized the better). In the total sample and postmenopausal women, the degree and direction of handedness were negatively correlated with daytime sleepiness. The chronotype was not associated with handedness in any group.
Conclusion: While associations were not consistent in all groups, overall, right-handedness tended to be associated with better sleep and less daytime sleepiness. Handedness and sleep seemed to be differentially associated in women and men, being in line with endocrine interactions.
Keywords: handedness, sleep, daytime sleepiness, menopause, actigraphy
Introduction
Restorative and sufficient sleep is essential for human well-being.1 Factors affecting quality and quantity of sleep include sex, age, body mass index (BMI) as well as other health- and lifestyle-related factors.2 Another factor probably affecting sleep is handedness.3 Handedness was formerly used as a dichotomous characteristic labelling individuals as either left- or right-handed (LH or RH).4 Using this concept, about 90% of the human population are RH.5 Research has moved on to see at least three categories: RH, LH, both termed consistently handed (CH) and inconsistent-handed (ICH).6 More modern approaches tend to avoid partitioning altogether and regard handedness as a continuum, which has two qualities: degree, meaning CH vs ICH, as well as direction, meaning RH vs LH.7
So far, handedness was inconsistently and in part contradictory reported being associated with several objective and subjective sleep parameters. Overall, lower degrees of lateralization were associated with objectively better sleep including a shorter sleep onset latency (SOL),8 a higher sleep efficiency (SE)8 and more N-REM sleep.8,9 Elsewhere, left-handedness was associated with longer10 or shorter total sleep time (TST)11 and lower SE.11 In contrast to objective sleep characteristics, lower degrees of lateralization were associated with subjectively impaired sleep, eg a shorter TST12 or more awakenings.13 Similarly, left-handedness was associated with more awakenings4 and lower TST.14 Most studies had limited sample sizes and a small range of ages of the participants, namely college students. Only a single study with solely over 65-year-old participants exists.15 Moreover, the majority of these studies only used self-report for analyses.4,12–14,16 Those using objective measures, ie actigraphy or polysomnography, recorded only a single night or lack of diversity of age or hand preference.8–11
Therefore, rational for our study was to add knowledge on the association between handedness and sleep. Compared to the right-handed majority, altered sleep in non-right-handed individuals could be caused by both, reactively, ie a more stressful life in a world designed for right-handers or a partly differing cortical sleep regulation.
While there is no clear cut lateralization in handedness,17 which is “simply based on a mirrored organization of hand motor areas”,18 the extent of activation of brain regions involved in hand movements has been shown to differ between right and left handers.18 In addition, handedness has been linked to different kinds of brain lateralization, such as language lateralization, eg “more atypical (right hemisphere) lateralization in left handers”.19,20
There is evidence that sex hormones affect lateralization in women (eg during the menstrual cycle21,22 and after estrogen replacement therapy23) as well as in men.24,25 In addition, sex hormones also affect sleep in both women26,27 and men.28 Therefore, we analyzed the association between handedness and sleep separately for men and women, dividing the cohort into ages for pre- and post-menopause.
Thus, the aim of this study was to examine the association between handedness and objective and subjective sleep, addressing potential age and sex differences in a broad cohort of 1764 participants with ages ranging from 18 to 80 years. While the nature of this study has been exploratory, we expected left-handedness to be associated with impaired sleep and more daytime sleepiness. In addition, we expected different associations in pre– and postmenopausal women.
Materials and Methods
Participants and Experimental Procedure
For this study, we used data from the “LIFE-Adult” study (Leipzig Research Center for Civilization Diseases); for details see.29 “LIFE-Adult” is a population-based study with 10,000 participating adults (age range: predominantly 40 to 79 years, 400 participants with an age range of 18 to 39 years). Participants were randomly recruited from the city of Leipzig, Germany. The LIFE participants took part in a baseline examination, during which various physical examinations (including blood sampling) were carried out, and interviews and questionnaires on various health topics were completed (including sociodemographics, medical history, medication intake). As part of an optional additional examination, a subgroup took part in a 1-week actigraphy examination to record physical activity and sleep behavior. The LIFE study was conducted according to the Declaration of Helsinki and was approved by the ethics committee of the University of Leipzig (registration number: 263-2009-14122009). All participants gave written informed consent.
For the sub-cohort studied here, inclusion criteria comprised actimetry completed for a minimum of 4 out of 5 nights, recording of subjective sleep characteristics using scales and a sleep diary, as well as questionnaires on daytime sleepiness, chronotype and handedness (see below). The following exclusion criteria were defined, potentially affecting sleep: a medical history of stroke, Parkinson’s disease or multiple sclerosis; current diagnosis of depression or cancer or treatment during the previous year. To address undetected depression, the Centre for Epidemiologic Studies – Depression Scale (CES-D) was measured, and participants with a score higher than 22 were excluded.30 Furthermore, precluded were participants using sleeping drugs more than once per week during the preceding month (according to item 7 of Pittsburgh Sleep Index, PSQI) or taking drugs with sleep-altering effects including hypnotics, tranquilizers, antipsychotics, anxiolytics, opioids and first-generation antihistamines (according to medication anamnesis interview). In addition, in order to minimize the inclusion of participants with otherwise disturbed sleep, only participants who slept more than 4 hours, objectively (according to actigraphy) as well as subjectively (PSQI item 4), were analyzed. In addition, shift workers or participants on parental leave were excluded from analyses.
Sleep was objectively measured using actigraphy (see below) in 2788 participants. Of these, 1024 participants were excluded for not meeting in- or exclusion criteria (see Figure 1). Thus, the resulting study population comprised 1764 persons (908 women and 856 men). Mean (± SD) age was 57.8 (± 12.2) years, mean BMI was 27.1 (± 4.3) kg/m2. Women had a mean age of 56.8 (± 12.1) years, men had a mean age of 58.8 (± 12.2) years. Women had a mean BMI of 26.8 (± 4.8) kg/m2, men had a mean BMI of 27.5 (± 3.7) kg/m2. The most diagnosed and reported illnesses were hypertension, elevated blood lipids, thyroid disease, arthrosis, disc prolapse, acid reflux, herpes zoster, ‘other skin diseases’ (than psoriasis or atopic dermatitis), hay fever and ‘other kidney diseases’ (than renal insufficiency).
Objective Measurement of Sleep Using Actigraphy
Actigraphy recordings were performed using SenseWear Pro 3 devices (BodyMedia Monitoring System, Bodymedia, Pittsburgh, Pennsylvania, USA). Participants were instructed to wear them for a total of seven consecutive days and nights. During this study period, participants were asked to keep a sleep-log, in which they documented their bedtimes and wake-up times, among other things.
Actigraphy data was analyzed using the SenseWear Professional software package version 6.1 (BodyMedia Monitoring System, Bodymedia, Pittsburgh, Pennsylvania, USA), which scores each recording minute as laying down (yes/no) and sleep (wake vs sleep). The algorithms used are based on multiple sensor parameters (galvanic skin response, skin temperature, 2-axis body acceleration, heat flux) with an off-arm detection in place to note the removal of the device. Validated successfully when compared with PSG, the SenseWear was shown to accurately detect total sleep time, wake after sleep onset and sleep efficiency.31–35 Many studies indirectly validated measurements of time in bed, meaning lying duration, by accurately assessing energy expenditure in relation to different activities.36–38 Lying duration assessed via this algorithm has been used in studies before.39,40 It was also shown that the SenseWear armband performs equally well in comparison with another well-established wearable tool called Actiwatch.31,35,41
Afterwards, data was exported to a Microsoft Excel template with customized Visual Basic for Applications (VBA) macros. The Excel tool was used to customize analysis windows to the specific day-night-cycles of each participant, as no fixed time-window was used for night sleep analyses. Based on the bedtime and wake-up information provided in the sleep log, the respective night sleep episodes were identified manually. Then, the following sleep parameters were calculated for each:
Time in bed (TIB = sum of all minutes classified as lying down)
Total Sleep Time (TST = sum of all minutes classified as sleep)
Sleep onset latency (SOL = sum of all minutes classified as lying down before first time falling asleep)
Sleep efficiency (SE = ratio of TST to TIB)
Number of waking episodes (Nwake = amount of nocturnal waking episodes ≥ 5 minutes)
Wake after sleep onset (WASO = sum of all minutes classified as wake between sleep onset and awakening).
For greater reliability, only data from nights during the week was used. Values were averaged across the 5 nights prior to work days (Sunday to Thursday night). Only participants with analyzable data from at least 4 nights were included in the analyses.
Subjective Assessment of Sleep and Sleep Quality
Subjective sleep characteristics and sleep related variables were captured during the baseline visit of the LIFE study using the following self-report questionnaires: The Pittsburgh Sleep Quality Index (PSQI) is a self-rating scale to assess the subjective quality and quantity of sleep during the past four weeks. It consists of 19 individual items, creating 7 components, producing a global score, ranging from 0 to 21 points with higher scores reflecting greater sleep problems.42–44 For the analysis of subjective sleep, we used items 1 (usual bedtime) and 3 (usual get up time) to calculate time in bed (TIBPSQI), item 2 (typical sleep onset latency; SOLPSQI) and 4 (usual sleep duration, SDPSQI) and calculated subjective sleep efficiency (SEPSQI = SDPSQI/TIBPSQI).
Determination of Daytime Sleepiness and Chronotype
To determine daytime sleepiness, the Epworth Sleepiness Scale (ESS) questionnaire was used. This self-rating instrument assesses the probability of falling asleep in 8 different everyday situations, thus addressing subjective sleepiness and hypersomnias.45,46 The ESS ranges from 0 to 24 points, with higher scores reflecting greater daytime sleepiness.
The chronotype was assessed using the German version of the 19-item Morningness-Eveningness-Questionnaire (D-MEQ), identifying individual circadian phase and preferences.47,48 The DMEQ ranges from 16 (definitive evening type) to 86 points (definitive morning type).
Determination of Handedness
Handedness was assessed using the Edinburgh Handedness Scale (EHI).49 We used the modified German version of the scale comprising questions regarding hand preference in 10 different motor activities (eg writing, throwing, lighting a match) and additionally 10 questions targeting consistency of hand use regarding each of these 10 activities. The EHI score provides real numbers ranging from −100 (CLH, consistently left-handed) to +100 (CRH, consistently right-handed). As we regarded handedness as a continuum, we used metric values of the score for analyses. The EHI-Score (EHI) was used to determine the direction of handedness. The absolute value of the EHI-Score (absEHI, range 0 to 100) was used to determine the degree of handedness.
Determination of Other Variables
Sex, age, comorbidities, medical history, medication and social economic parameters were assessed via self-report.
Statistical Procedure
Only data recorded during the week was considered for analysis since sleeping patterns on the weekend are less reliant. Then, people engage in different activities, bending their sleeping schedules either to stay up especially late for festivities or to sleep longer to lessen the sleeping debt they may have accumulated during the week.
To control for age and menopausal status, a subgroup-analysis with restricted age ranges was performed. Participants between the ages of 18–45 years were grouped together to constitute a pre-menopausal group, while ≥55 year-olds were grouped together to build a post-menopausal group, considering that the mean age of menopause is about 50 years.50 The cohort was further stratified for sex, leaving four subgroups: young females (N = 190), young males (N = 137), female seniors (N = 511), and male seniors (N = 519).
Subgroups were compared using t-test; if variances were not equal, corrected t-values were used. Correlations between sleep parameters and handedness were calculated using Spearman rank correlations. All statistical testing was performed using SPSS Statistics version 24 (IBM Corp., Armonk, New York, USA). P-values <0.05 were considered to be statistically significant. We did not use the Bonferroni correction for multiple testing in this exploratory study aiming at identifying effects worthy of further being studied. Thereby, we minimized the risk of type 2 errors (ie not detecting a true effect) and accepted the risk of type 1 errors (ie detecting a false effect). Type 2 errors are of particular concern in our sample since the absolute number of predominantly left-handed participants is low despite the large sample due to the small proportion. We believe that this approach is in line with both statistical recommendations51 and current practice.52–54
Results
Objective and Subjective Sleep
Differences between sexes are shown in Table 1. Regarding objective sleep, women spent more time in bed (TIB), slept more (TST) and had a higher sleep efficiency (SE) with fewer awakenings (Nwake) and less time awake (WASO). In contrast, women subjectively reported to sleep less (shorter SDPSQI), to require more time to fall asleep (longer SOLPSQI) and therefore to sleep less efficiently (lower SEPSQI) than men. Also, their subjective quality of sleep (PSQI score) is worse than in men. However, men score higher regarding daytime sleepiness (ESS score).
 |
Table 1 Handedness, Objective and Subjective Sleep Parameters, Daytime Sleepiness and Chronotype Across the Cohort Separated by Sex |
Distribution of Handedness
Mean EHI-Scores were 82.41 (SD = 39.45), with most participants (91.0%) being classified as right-handed (RH), according to their EHI-Score. N = 84 (4.8%) participants were classified as left-handed (LH) and N = 74 (4.2%) were classified as ambidextrous. While most RH showed extremely high lateralization (ie EHI-Score = +100), all other individuals were widely spread in their distribution of hand preferences. Strongly lateralized LH (EHI-Score = −100) were very rare with most LH being only mildly lateralized. It is apparent that handedness is a continuum rather than discrete categories.
Degree and direction of handedness for both men and women are depicted in Figure 2. Handedness scores were comparable for women (EHI = 82.48; absEHI = 90.09) and men (EHI = 82.33, absEHI = 88.59), yet the Mann–Whitney-Test reached significance for absEHI (Z = −2.037, p = 0.042). There were slightly less left-handed men than women (4.1% vs 5.4%), while there were less ambidextrous women than men (3.6% vs 4.8%).
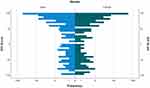 |
Figure 2 Frequency of the Edinburgh Handedness Scale (EHI)-Score in female and male participants. Notes: EHI-Score 100 = consistently right-handed. EHI-Score −100 = consistently left-handed. |
Handedness and Objective Sleep Parameters
In the total sample, time spent awake after sleep onset (WASO) was correlated with handedness. The same was true for the sample of all women (Table 2). In postmenopausal women, in addition to WASO, also time in bed (TIB) and total sleep time (TST) were correlated with handedness. In this subset, right-handedness was associated with longer TIB, longer TST and less WASO (Table 2). Other associations between handedness and objective sleep parameters could not be found. This applies to all other groups looked at: all men, premenopausal women and men stratified for age groups (Table 2). All significant correlations existed for both EHI and absEHI, meaning that direction and degree of lateralization were correlated with sleep parameters in the same way.
 |
Table 2 Spearman’s Rank Correlation of Direction of Handedness (Mean EHI) and Degree of Handedness (Absolute EHI) with Objective Sleep Parameters Separated by Sex and Age Group |
Handedness and Subjective Sleep Parameters
There was no significant association between handedness and a quantitative sleep parameter as assessed with the PSQI (eg SOL) in any group. In terms of quality of sleep, however, right-handedness was associated with a lower PSQI score in premenopausal women and older men, indicating better sleep quality (Table 3). All significant correlations existed for both EHI and absEHI, meaning that direction and degree of lateralization were correlated with sleep parameters in the same way. In the following groups, neither quantitative nor qualitative PSQI measures were associated with handedness: total group, all women, all men, younger men and postmenopausal women.
 |
Table 3 Spearman's Rank Correlation of Direction of Handedness (Mean EHI) and Degree of Handedness (Absolute EHI) with Subjective Sleep Parameters Separated by Sex and Age Group |
Daytime Sleepiness and Chronotype
In the total group and in postmenopausal women, right-handedness was associated with a lower ESS score, ie less daytime sleepiness (Table 3). The chronotype (D-MEQ score) was not associated with handedness in any group.
Discussion
To our knowledge, this is by far the largest study investigating the association between handedness and objective and subjective sleep. Key findings are:
First, the more right-handed/lateralized the participants were, the less they were awake after sleep onset. This was true for the total sample, all women and postmenopausal women. The latter also spent more time in bed and slept more. Secondly, in contrast to these associations with objective sleep variables, there was no significant association with any subjective quantitative sleep parameter in any group. Thirdly, however, the more right-handed/lateralized premenopausal women and >55-year-old men were, the better their subjective quality of sleep was. Fourthly, the more right-handed/lateralized the participants were, the less sleepy they were at daytime. This applied to the total group and postmenopausal women. Thus, overall, while associations were not consistently found in all groups, right-handedness tended to be associated with better sleep and less daytime sleepiness. Overall, associations were weak, though. The finding that direction (EHI) and degree (absEHI) of handedness showed similar correlations is plausible since the vast majority of participants were right-handed and showed a high degree of lateralization.
So far, there are only 11 studies on the association between handedness and sleep. Four of them used objective measuring techniques (actigraphy8–11 with one study additionally comparing with polysomnography and self-report11) while seven only used self-reports.4,12–16,55
Studies capturing objective sleep variables were rather small (10 to 41 participants) and included only young participants with mean ages ranging from 20.5 to 22.4 years. Results were inconsistent: One study reported right-handedness to be associated with longer total sleep time (TST) and higher sleep efficiency (SE).11 Another study reported left-handedness to be associated with longer sleep duration with no significant differences in sleep onset latency (SOL) or SE.10 Propper et al reported in a first study, investigating sleep depending on the degree of handedness, a higher degree of handedness (ie consistently handed individuals) to be associated with longer SOL and lower SE in women.8 In a second study, addressing direction of handedness, they compared sleep in 5 consistent LH (4 females) and 5 consistent RH (5 females). Here, the only significant finding is a higher number of REM periods in consistent LH.9 Thus overall, no clear picture has arisen from these studies. Our findings also do not show a homogenous picture. Overall, however, direction and degree of handedness (the more right-handed and the more lateralized) were associated with better objective sleep, being roughly in line with the results of one of the studies11 but not of the others.8,10
Research focusing on the association between handedness and subjective sleep is limited as well. Except for one15 out of seven, all studies included young participants with mean ages 16–29 years.4,11–14,16 Two studied the degree of handedness,13,14 two direction4,11 and two both.12,16 The one study in elderly (older than 64 years) included 1277 participants but was (regarding sleep) limited to the question “can get enough rest and sleep” in consistent-handed and non-consistent-handed (mixed-handed) participants.15 A further recent study compared subjective sleep parameters and direction of handedness in 35 gifted and 28 non-gifted children between 8 and 12 years.55
Also, in terms of subjective sleep, findings were not uniform but less contradictory: Among young adults, a higher degree of handedness was found to be associated with longer sleep duration,14 lower SOL,13 less awakenings13 and less “trouble returning to sleep after an awakening”.13 That means overall, a higher degree of handedness tended to be associated with better sleep. A study addressing direction of handedness reported right-handedness to be associated with less sleep problems.4 Another study, mainly addressing dream recall, found that the sleep duration in left-, right- and mixed-handed individuals was comparable.16 In elderly participants, the proportion agreeing on the question “can get enough rest and sleep” did not differ between consistent-handed and non-consistent-handed (mixed-handed) participants.15 Piro et al showed gifted children to be significantly more left-handed, as well as showing a trend towards more sleep disturbances.55 Thus, at least in adults, most studies point to better sleep in right-handed or consistent handed participants. These findings are in line with our result of a better sleep quality in pre-menopausal women and older men as assessed with the PSQI total score. Single subjective sleep measures derived from the PSQI (eg TIB) did not show correlations with handedness in our study, though.
Objectively measured TIB and TST were shorter than subjectively reported in our sample (Table 1), being a well-known finding56 and a possible reason that associations between handedness and objective and subjective sleep, respectively, were not congruent.
In contrast to sleep, we are not aware of reports on the association of handedness and daytime sleepiness. The less right-handed/consistent handed participants were, the higher the daytime sleepiness was. This interesting finding is in line with the concept that it may be more stressful for left-handers or mixed-handers “to cope in a right-handed world”.10 Either, sleepiness could be “directly” induced by the higher effort required to manage the daily routine. Or, sleepiness could be caused by impaired night sleep since stress has been shown to impair sleep.57–59 In line with that, stress reduction was repeatedly associated with improved sleep quality.60,61 In addition or alternatively to those reactive mechanisms (to higher stress levels), higher sleepiness could also be linked to differences in brain structure or function.
While we did not find striking differences between women and men or between pre- and postmenopausal women, there are several indications that might suggest endocrine influences: For example, TIB and TST were positively correlated in postmenopausal women and negatively in premenopausal women. In the smaller premenopausal group, this did not reach significance, though. Of note, we did not analyze sex hormones so that this assumption ultimately remains speculative.
While handedness appears to be mainly, and sleep partly determined by genetic and epigenetic factors,20,62 there is evidence that both lateralization and handedness as well as sleep are also affected by sex hormones. While sex hormones are ‘likely not initially triggering hemispheric asymmetries’, they have ‘been shown to be able to profoundly shape them.’20 For example in premenopausal women, functional cerebral asymmetry (FCA) constantly changes in dependence of their hormonal cycles as shown by the electroencephalogram (EEG)63 or functional magnetic resonance imaging (fMRI).21,64 During the follicular phase when estradiol levels are rising, FCA is lowest, and during the menses, lateralization is most pronounced.21 Accordingly, the lateralized behavior (figure recognition or spatial attention) changed.20,22 In men, salivary testosterone levels in adult men have been linked to cerebral laterality for language.65 In addition, testosterone has been shown to affect brain asymmetries in terms of language lateralization66 and mental rotation,24 prenatally and during puberty.24 Similarly, androgen exposure in utero has been suggested to influence the development of left-handedness.67,68 A recent study found high prenatal testosterone concentrations in amniotic fluids to predict weak hand skill asymmetry scores and high prenatal estradiol to predict predicted weak hand preference in 15-year-old girls, thus overall also suggesting some influence of sex hormones on handedness.69 An interplay between sex hormones and handedness in females is also suggested by reports that left-handedness is associated with earlier menopause70,71 – yet, here also non-supportive reports exist72,73 – and different sex hormone levels in left- and right-handed menopausal women.74
Sex hormones also affect human sleep. In women, sleep architecture was found to be dependent on luteinizing hormone (LH), follicle stimulating hormone (FSH), progesterone and estrogen, causing more sleep difficulties during the week before and during menses.75 Later in life, reduced sex hormone levels during menopause are associated with sleep difficulties in 40–56% “with 26% experiencing severe symptoms that impact daytime functioning”.76 Consistently, progesterone showed sleep-promoting effects in postmenopausal women.26,77,78 Furthermore, besides progesterone also estradiol contributes to the regulation of sleep stages.27 In men, low testosterone levels were associated with impaired sleep.79,80 While the decreasing sleep efficiency in men during aging has been linked to declining testosterone levels,28 sleep, in turn, plays an important role in endocrine regulation, including maintaining male testosterone levels.28,81
Opposed to a large body of literature reporting non-right handedness to be more common in men, regardless of culture and century,82 we did not find a relevant difference in our cohort in terms of direction. This might be due to our comparatively old study cohort: LH have a shorter life expectancy than RH with the earliest deaths in the group of only little lateralized LH.83 In addition, men die younger than women do. Our finding of better objective sleep in women but better subjective sleep in men is in agreement with current knowledge.56
Strengths and Limitations
The main strength of this study is the large sample size comprising both subjective and objective sleep data. By stratifying the cohort according to sex and age, we controlled for the two main confounding factors in sleep regulation.84 Additionally, we analyzed the mean values of five consecutive nights in their home environment; thus, the setting was as natural as possible.
It is a limitation that the age distribution was uneven since more participants that are elderly were included. Moreover, it would have been interesting to capture polysomnographic data in order to shed light on sleep stages. It is another limitation that participants with undiagnosed sleep disorders, including obstructive sleep apnea (OSA) and sleep movement disorders, could not be excluded because there were neither data from polysomnography nor from appropriate questionnaires allowing us to do so. Therefore, the study results should be interpreted very carefully. In terms of insomnia, at least in severe forms, we excluded those with an objective or subjective sleep duration of less than 4 hours.
Conclusions
While associations between sleep parameters and handedness were not consistent in all groups, overall, right-handedness tended to be associated with better sleep and less daytime sleepiness. Handedness and sleep seemed to be differentially associated in women and men, being in line with endocrine interactions.
Abbreviations
EHI, Edinburgh Handedness Inventory (score); absEHI, absolute value of Edinburgh Handedness Inventory score; BMI, body mass index; RH, right-hander; LH, left-hander; CH, consistently handed; ICH, inconsistently handed; CRH, consistently right-handed; CLH, consistently left-handed; TIB, time in bed; SOL, sleep onset latency; TST, total sleep time; SE, sleep efficiency; Nwake, number of times participants woke for more than 5 min during each night; WASO, amount of time spent awake after sleep onset; PSQI, Pittsburgh Sleep Quality Index; D-MEQ, Morningness-Eveningness-Questionnaire, German version; ESS, Epworth Sleepiness Scale.
Ethics Approval and Informed Consent
The study was conducted according to the Declaration of Helsinki and was approved by the ethics committee of the University of Leipzig (registration number: 263-2009-14122009). All participants gave written informed consent.
Data Sharing Statement
Restrictions are applied to the availability of these data. Data was obtained from the Leipzig Research Center for Civilisation Diseases. All data and samples of LIFE are the property of the University of Leipzig and are subject to the Law for the Protection of Informal Self-Determination in the Free State of Saxony (Saxon Data Protection Act). Use of data can be requested through the LIFE office (https://life.uni-leipzig.de/).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by LIFE – Leipzig Research Center for Civilization Diseases, University of Leipzig. LIFE is funded by means of the European Union, by means of the European Social Fund (ESF), by the European Regional Development Fund (ERDF), and by means of the Free State of Saxony within the framework of the excellence initiative. We acknowledge support from Leipzig University for Open Access Publishing.
Disclosure
All authors declare no conflicts of interest related to this work.
References
1. Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151–161. doi:10.2147/NSS.S134864
2. Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3(5):383–388. doi:10.1016/j.sleh.2017.07.013
3. Christman SD, Propper RE. Dreaming, handedness, and sleep architecture: interhemispheric mechanisms. Int Rev Neurobiol. 2010;92:215–232.
4. Coren S, Searleman A. Left sidedness and sleep difficulty: the alinormal syndrome. Brain Cogn. 1987;6(2):184–192. doi:10.1016/0278-2626(87)90119-9
5. Papadatou-Pastou M, Ntolka E, Schmitz J, et al. Human handedness: a meta-analysis. Psychol Bull. 2020;146(6):481–524. doi:10.1037/bul0000229
6. Christman SD. Handedness. In: Ramachandran VS, editor. Encyclopedia of Human Behavior.
7. Christman SD, Prichard EC, Corser R. Factor analysis of the Edinburgh handedness inventory: inconsistent handedness yields a two-factor solution. Brain Cogn. 2015;98:82–86. doi:10.1016/j.bandc.2015.06.005
8. Propper RE, Lawton N, Przyborski M, Christman SD. An assessment of sleep architecture as a function of degree of handedness in college women using a home sleep monitor. Brain Cogn. 2004;54(3):186–197. doi:10.1016/j.bandc.2004.01.004
9. Propper RE, Christman SD, Olejarz S. Home-recorded sleep architecture as a function of handedness II: consistent right- versus consistent left-handers. J Nerv Ment Dis. 2007;195(8):689–692. doi:10.1097/NMD.0b013e31811f44b8
10. Lehnkering H, Strauss A, Wegner B, Siegmund R. Actigraphic investigations on the activity-rest behavior of right- and left-handed students. Chronobiol Int. 2006;23(3):593–605. doi:10.1080/07420520600724094
11. Killgore WD, Lipizzi EL, Grugle NL, Killgore DB, Balkin TJ. Handedness correlates with actigraphically measured sleep in a controlled environment. Percept Mot Skills. 2009;109(2):395–400. doi:10.2466/pms.109.2.395-400
12. Hicks RA, Pellegrini RJ, Hawkins J. Handedness and sleep duration. Cortex. 1979;15(2):327–329. doi:10.1016/S0010-9452(79)80036-2
13. Hicks RA, DeHaro D, Inman G, Hicks GJ. Consistency of hand use and sleep problems. Percept Mot Skills. 1999;89(1):49–56. doi:10.2466/pms.1999.89.1.49
14. Propper RE. Handedness differences in self-assessment of sleep quantity: non-right versus strong right handers. Sleep Biol Rhythms. 2004;2(1):99–101. doi:10.1111/j.1479-8425.2003.00067.x
15. Porac C, Searleman A. The relationship between hand preference consistency, health, and accidents in a sample of adults over the age of 65 years. Laterality. 2006;11(5):405–414. doi:10.1080/13576500600677823
16. Violani C, De Gennaro L, Solano L. Hemispheric differentiation and dream recall: subjective estimates of sleep and dreams in different handedness groups. Int J Neurosci. 1988;39(1–2):9–14. doi:10.3109/00207458808985687
17. Tzourio-Mazoyer N, Zago L, Cochet H, Crivello F. Development of handedness, anatomical and functional brain lateralization. Handb Clin Neurol. 2020;173:99–105.
18. Tzourio-Mazoyer N, Labache L, Zago L, Hesling I, Mazoyer B. Neural support of manual preference revealed by BOLD variations during right and left finger-tapping in a sample of 287 healthy adults balanced for handedness. Laterality. 2021;26(4):398–420. doi:10.1080/1357650X.2020.1862142
19. Bruckert L, Thompson PA, Watkins KE, Bishop DVM, Woodhead ZVJ. Investigating the effects of handedness on the consistency of lateralization for speech production and semantic processing tasks using functional transcranial Doppler sonography. Laterality. 2021;26:1–26.
20. Güntürkün O, Ströckens F, Ocklenburg S. Brain lateralization: a comparative perspective. Physiol Rev. 2020;100(3):1019–1063. doi:10.1152/physrev.00006.2019
21. Weis S, Hausmann M, Stoffers B, Vohn R, Kellermann T, Sturm W. Estradiol modulates functional brain organization during the menstrual cycle: an analysis of interhemispheric inhibition. J Neurosci. 2008;28(50):13401–13410. doi:10.1523/JNEUROSCI.4392-08.2008
22. Hausmann M. Hemispheric asymmetry in spatial attention across the menstrual cycle. Neuropsychologia. 2005;43(11):1559–1567. doi:10.1016/j.neuropsychologia.2005.01.017
23. Doty RL, Kisat M, Tourbier I. Estrogen replacement therapy induces functional asymmetry on an odor memory/discrimination test. Brain Res. 2008;1214:35–39. doi:10.1016/j.brainres.2008.04.017
24. Beking T, Geuze RH, van Faassen M, Kema IP, Kreukels BPC, Groothuis TGG. Prenatal and pubertal testosterone affect brain lateralization. Psychoneuroendocrinology. 2018;88:78–91. doi:10.1016/j.psyneuen.2017.10.027
25. Hollier LP, Maybery MT, Keelan JA, Hickey M, Whitehouse AJ. Perinatal testosterone exposure and cerebral lateralisation in adult males: evidence for the callosal hypothesis. Biol Psychol. 2014;103:48–53. doi:10.1016/j.biopsycho.2014.08.009
26. Schüssler P, Kluge M, Adamczyk M, et al. Sleep after intranasal progesterone vs. zolpidem and placebo in postmenopausal women – a randomized, double-blind cross over study. Psychoneuroendocrinology. 2018;92:81–86. doi:10.1016/j.psyneuen.2018.04.001
27. Copinschi G, Caufriez A. Sleep and the ovarian axis. Curr Opin Endocr Metab Res. 2021;17:38–45. doi:10.1016/j.coemr.2021.01.001
28. Andersen ML, Tufik S. The effects of testosterone on sleep and sleep-disordered breathing in men: its bidirectional interaction with erectile function. Sleep Med Rev. 2008;12(5):365–379. doi:10.1016/j.smrv.2007.12.003
29. Loeffler M, Engel C, Ahnert P, et al. The LIFE-Adult-Study: objectives and design of a population-based cohort study with 10,000 deeply phenotyped adults in Germany. BMC Public Health. 2015;15(1):691. doi:10.1186/s12889-015-1983-z
30. Radloff LS, The CES-D. Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi:10.1177/014662167700100306
31. Alsaadi SM, McAuley JH, Hush JM, et al. Assessing sleep disturbance in low back pain: the validity of portable instruments. PLoS One. 2014;9(4):e95824. doi:10.1371/journal.pone.0095824
32. O’Driscoll DM, Turton AR, Copland JM, Strauss BJ, Hamilton GS. Energy expenditure in obstructive sleep apnea: validation of a multiple physiological sensor for determination of sleep and wake. Sleep Breath. 2013;17(1):139–146. doi:10.1007/s11325-012-0662-x
33. Peterson BT, Chiao P, Pickering E, et al. Comparison of actigraphy and polysomnography to assess effects of zolpidem in a clinical research unit. Sleep Med. 2012;13(4):419–424. doi:10.1016/j.sleep.2011.12.003
34. Sharif MM, Bahammam AS. Sleep estimation using BodyMedia’s SenseWear™ armband in patients with obstructive sleep apnea. Ann Thorac Med. 2013;8(1):53–57. doi:10.4103/1817-1737.105720
35. Shin M, Swan P, Chow CM. The validity of Actiwatch2 and SenseWear armband compared against polysomnography at different ambient temperature conditions. Sleep Sci. 2015;8(1):9–15. doi:10.1016/j.slsci.2015.02.003
36. Casiraghi F, Lertwattanarak R, Luzi L, et al. Energy expenditure evaluation in humans and non-human primates by SenseWear Armband. Validation of energy expenditure evaluation by SenseWear Armband by direct comparison with indirect calorimetry. PLoS One. 2013;8(9):e73651. doi:10.1371/journal.pone.0073651
37. Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ. Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc. 2010;42(11):2134–2140. doi:10.1249/MSS.0b013e3181e0b3ff
38. Welk GJ, McClain JJ, Eisenmann JC, Wickel EE. Field validation of the MTI Actigraph and BodyMedia armband monitor using the IDEEA monitor. Obesity. 2007;15(4):918–928. doi:10.1038/oby.2007.624
39. Madden KM, Ashe MC, Lockhart C, Chase JM. Sedentary behavior and sleep efficiency in active community-dwelling older adults. Sleep Sci. 2014;7(2):82–88. doi:10.1016/j.slsci.2014.09.009
40. Włodarek D, Gląbska D, Rojek-Trębicka J. Physical activity of predialysis patients with chronic kidney disease measured using SenseWear Armban. J Sports Med Phys Fitness. 2011;51(4):639–646.
41. van Wouwe NC, Valk PJ, Veenstra BJ. Sleep monitoring: a comparison between three wearable instruments. Mil Med. 2011;176(7):811–816. doi:10.7205/MILMED-D-10-00389
42. Hinz A, Glaesmer H, Brähler E, et al. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med. 2017;30:57–63. doi:10.1016/j.sleep.2016.03.008
43. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
44. Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53(3):737–740. doi:10.1016/S0022-3999(02)00330-6
45. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi:10.1093/sleep/14.6.540
46. Sauter C, Popp R., Danker-Hopfe H, et al. Normative values of the German Epworth Sleepiness Scale. Somnologie. 2007;11,272-278. doi:10.1007/s11818-007-0322-8
47. Griefahn B, Künemund C, Bröde P, Mehnert P. Zur Validität der deutschen Übersetzung des Morningness-Eveningness-Questionnaires von Horne und Östberg. Somnologie. 2001;5(2):71–80. doi:10.1046/j.1439-054X.2001.01149.x
48. Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4(2):97–110.
49. Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9(1):97–113. doi:10.1016/0028-3932(71)90067-4
50. Team IS. Variations in reproductive events across life: a pooled analysis of data from 505 147 women across 10 countries. Hum Reprod. 2019;34(5):881–893. doi:10.1093/humrep/dez015
51. Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34(5):502–508. doi:10.1111/opo.12131
52. Al-Rashed F, Sindhu S, Al Madhoun A, et al. Short sleep duration and its association with obesity and other metabolic risk factors in Kuwaiti urban adults. Nat Sci Sleep. 2021;13:1225–1241. doi:10.2147/NSS.S311415
53. Sabil A, Bignard R, Gervès-Pinquié C, et al. Risk factors for sleepiness at the wheel and sleep-related car accidents among patients with obstructive sleep apnea: data from the French Pays de la Loire sleep cohort. Nat Sci Sleep. 2021;13:1737–1746. doi:10.2147/NSS.S328774
54. Yang Y, Li C, Zhao L, Li J, Han F, Xiao F. Factors Associated with Depression and Sub-Dimension Symptoms in Adolescent Narcolepsy. Nat Sci Sleep. 2021;13:1075–1082. doi:10.2147/NSS.S312000
55. Piro JM, Ortiz C, Manouvrier L. Sleep behaviors and handedness in gifted and non-gifted children. Dev Neuropsychol. 2021;46:1–10.
56. Kocevska D, Lysen TS, Dotinga A, et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: a systematic review and meta-analysis. Nat Hum Behav. 2021;5(1):113–122. doi:10.1038/s41562-020-00965-x
57. Lipert A, Musiał K, Rasmus P. Working mode and physical activity as factors determining stress and sleep quality during COVID-19 pandemic lockdown in Poland. Life. 2021;12(1):28. doi:10.3390/life12010028
58. Bernburg M, Hetzmann MS, Mojtahedzadeh N, et al. Stress perception, sleep quality and work engagement of German outpatient nurses during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;19(1):313. doi:10.3390/ijerph19010313
59. Zhao X, Lan M, Li H, Yang J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: a moderated mediation model. Sleep Med. 2021;77:339–345. doi:10.1016/j.sleep.2020.05.021
60. Chen TL, Chang SC, Hsieh HF, Huang CY, Chuang JH, Wang HH. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: a meta-analysis. J Psychosom Res. 2020;135:110144. doi:10.1016/j.jpsychores.2020.110144
61. Stächele T, Domes G, Wekenborg M, Penz M, Kirschbaum C, Heinrichs M. Effects of a 6-week internet-based stress management program on perceived stress, subjective coping skills, and sleep quality. Front Psychiatry. 2020;11:463. doi:10.3389/fpsyt.2020.00463
62. Garfield V. Sleep duration: a review of genome-wide association studies (GWAS) in adults from 2007 to 2020. Sleep Med Rev. 2021;56:101413. doi:10.1016/j.smrv.2020.101413
63. Cacioppo S, Bianchi-Demicheli F, Bischof P, Deziegler D, Michel CM, Landis T. Hemispheric specialization varies with EEG brain resting states and phase of menstrual cycle. PLoS One. 2013;8(4):e63196. doi:10.1371/journal.pone.0063196
64. Thimm M, Weis S, Hausmann M, Sturm W. Menstrual cycle effects on selective attention and its underlying cortical networks. Neuroscience. 2014;258:307–317. doi:10.1016/j.neuroscience.2013.11.010
65. Papadatou-Pastou M, Martin M. Cerebral laterality for language is related to adult salivary testosterone levels but not digit ratio (2D:4D) in men: a functional transcranial Doppler ultrasound study. Brain Lang. 2017;166:52–62. doi:10.1016/j.bandl.2016.12.002
66. Lust JM, Geuze RH, Van de Beek C, Cohen-Kettenis PT, Groothuis AGG, Bouma A. Sex specific effect of prenatal testosterone on language lateralization in children. Neuropsychologia. 2010;48(2):536–540. doi:10.1016/j.neuropsychologia.2009.10.014
67. Galaburda AM, LeMay M, Kemper TL, Geschwind N. Right-left asymmetrics in the brain. Science. 1978;199(4331):852–856. doi:10.1126/science.341314
68. Nass R, Baker S, Speiser P, et al. Hormones and handedness: left-hand bias in female congenital adrenal hyperplasia patients. Neurology. 1987;37(4):711–715. doi:10.1212/WNL.37.4.711
69. Richards G, Beking T, Kreukels BPC, Geuze RH, Beaton AA, Groothuis T. An examination of the influence of prenatal sex hormones on handedness: literature review and amniotic fluid data. Horm Behav. 2021;129:104929. doi:10.1016/j.yhbeh.2021.104929
70. Leidy LE. Early age at menopause among left-handed women. Obstet Gynecol. 1990;76(6):1111–1114.
71. Dane S, Reis N, Pasinlioğu T. Left-handed women have earlier age of menopause. J Basic Clin Physiol Pharmacol. 1999;10(2):147–150. doi:10.1515/JBCPP.1999.10.2.147
72. Pavia M, Hsieh CC, Ekbom A, Adami HO, Trichopoulos D. Handedness, age at menarche, and age at menopause. Obstet Gynecol. 1994;83(4):579–582. doi:10.1097/00006250-199404000-00015
73. Fallahzadeh H. Age at natural menopause in Yazd, Islamic Republic Of Iran. Menopause. 2007;14(5):900–904. doi:10.1097/gme.0b013e318032b2e6
74. Negrev N, Nikolova P, Nikolova R. Serum levels of female sex hormones in left-handed and right-handed menopausal women. Laterality. 2000;5(1):69–75. doi:10.1080/713754352
75. Suh S, Cho N, Zhang J. Sex Differences in Insomnia: from Epidemiology and Etiology to Intervention. Curr Psychiatry Rep. 2018;20(9):69. doi:10.1007/s11920-018-0940-9
76. Baker FC, de Zambotti M, Colrain IM, Bei B. Sleep problems during the menopausal transition: prevalence, impact, and management challenges. Nat Sci Sleep. 2018;10:73–95. doi:10.2147/NSS.S125807
77. Nolan BJ, Liang B, Cheung AS. Efficacy of micronized progesterone for sleep: a systematic review and meta-analysis of randomized controlled trial data. J Clin Endocrinol Metab. 2021;106(4):942–951. doi:10.1210/clinem/dgaa873
78. Schüssler P, Kluge M, Yassouridis A, et al. Progesterone reduces wakefulness in sleep EEG and has no effect on cognition in healthy postmenopausal women. Psychoneuroendocrinology. 2008;33(8):1124–1131. doi:10.1016/j.psyneuen.2008.05.013
79. Patel P, Shiff B, Kohn TP, Ramasamy R. Impaired sleep is associated with low testosterone in US adult males: results from the National Health and Nutrition Examination Survey. World J Urol. 2019;37(7):1449–1453. doi:10.1007/s00345-018-2485-2
80. Schiavi RC, Schreiner-Engel P, White D, Mandeli J. The relationship between pituitary-gonadal function and sexual behavior in healthy aging men. Psychosom Med. 1991;53(4):363–374. doi:10.1097/00006842-199107000-00002
81. Su L, Zhang SZ, Zhu J, Wu J, Jiao YZ. Effect of partial and total sleep deprivation on serum testosterone in healthy males: a systematic review and meta-analysis. Sleep Med. 2021;88:267–273. doi:10.1016/j.sleep.2021.10.031
82. Papadatou-Pastou M, Martin M, Munafò MR, Jones GV. Sex differences in left-handedness: a meta-analysis of 144 studies. Psychol Bull. 2008;134(5):677–699. doi:10.1037/a0012814
83. Ellis L, Engh T. Handedness and age of death: new evidence on a puzzling relationship. J Health Psychol. 2000;5(4):561–565. doi:10.1177/135910530000500412
84. Grandner MA. Sleep, Health, and Society. Sleep Med Clin. 2020;15(2):319–340. doi:10.1016/j.jsmc.2020.02.017
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

