Back to Journals » Clinical Epidemiology » Volume 13
Non-Persistence with Medication as a Mediator for the Social Inequality in Risk of Major Adverse Cardiovascular Events in Patients with Incident Acute Coronary Syndrome: A Nationwide Cohort Study
Authors Boesgaard Graversen C , Brink Valentin J , Lytken Larsen M, Riahi S, Holmberg T, Paaske Johnsen S
Received 19 August 2021
Accepted for publication 19 October 2021
Published 13 November 2021 Volume 2021:13 Pages 1071—1083
DOI https://doi.org/10.2147/CLEP.S335133
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Vera Ehrenstein
Christina Boesgaard Graversen,1 Jan Brink Valentin,2 Mogens Lytken Larsen,3 Sam Riahi,1,3 Teresa Holmberg,4 Søren Paaske Johnsen2
1Department of Cardiology, Aalborg University Hospital, Aalborg, Denmark; 2Danish Center for Clinical Health Services Research, Department of Clinical Medicine, Aalborg University, Aalborg, Denmark; 3Department of Clinical Medicine, The Faculty of Medicine, Aalborg University, Aalborg, Denmark; 4National Institute of Public Health, University of Southern Denmark, Copenhagen, Denmark
Correspondence: Christina Boesgaard Graversen Email [email protected]
Aim: Low socioeconomic status is associated with higher risk of major adverse cardiovascular events (MACE) among patients with incident acute coronary syndrome (ACS). We examined whether non-persistence with antiplatelet and statin therapy mediated the income- and educational-related inequality in risk of MACE.
Methods: Using national registers, all Danish patients diagnosed with incident ACS from 2010 to 2017 were identified. The primary outcome (MACE) comprised all-cause death, cardiac death and cardiac readmission. Risk of MACE was handled by discrete time analyses using inverse probability of treatment weights. The mediator variable comprised non-persistence to a combined 2-dimensional measure of statin and antiplatelet treatment. The mediation analysis was evaluated by population average effects.
Results: The study population was 45,874 patients, of whom 16,958 (37.0%) were non-persistent with medication and 16,365 (35.7%) suffered MACE during the median follow-up of 3.5 years. Compared to patients with low income, the adjusted hazard ratio of MACE was lowered by 33% (HR: 0.67, 95% CI: 0.61– 0.72) in men and by 34% (HR: 0.66, 95% CI: 0.61– 0.72) in women with high income, respectively. Similar results were observed according to level of education. A socioeconomic difference in risk of non-persistence was found in men but not women and only in relation to income. The lower risk of non-persistence observed in high-income men mediated the lower risk of MACE by 12.6% (95% CI: 11.1– 14.1%) compared with low-income men.
Conclusion: Non-persistence with medication mediated some of the income-related inequality in risk of MACE in men, but not women, with incident ACS.
Keywords: acute coronary syndrome, social inequality, major adverse cardiovascular event, non-persistence with medication, register-based cohort study
Introduction
In recent decades risk of mortality following acute coronary syndrome (ACS) has decreased, which is often explained by a combination of a general improvement in cardiovascular risk factors and widespread implementation of invasive treatment and secondary pharmacological and nonpharmacological preventive treatment.1–3 Nonetheless, one year mortality is still approximately 15% and several studies have shown that socioeconomically deprived patients have higher risk of major adverse cardiovascular events (MACE) compared to the more affluent patients.4,5
The existing research attributes the increased risk of MACE to be partly explained by socioeconomic gradients in obtained functional recovery after diagnosis,6 as well as the use of evidence-based secondary preventive measures, including cardiac rehabilitation.7,8 Also, socioeconomic inequality in long-term survival among patients treated with percutaneous coronary interventions or coronary artery bypass grafting have been demonstrated.9–11 The inequality in clinical outcomes appears not to be explained by diverse access to invasive management.12,13 Thus, it has been speculated whether poor clinical outcomes instead could partly be explained by lower utilisation of secondary preventive treatment during follow-up.10 Such low utilisation is considered problematic, as a vast body of evidence reports statin and antiplatelet therapy to lower risk of MACE, and these drugs have long been a cornerstone in the secondary pharmacological treatment following ACS and implemented in clinical guidelines.14,15 Further, any delay in secondary pharmacological treatment will increase risk of MACE, also in females who more often suffer from non-obstructive coronary artery disease.16
Lower levels of income, and to some extent lower levels of education, have been argued to be risk factors for non-persistence with medication.11 Thus, studies have tried to handle the effect of non-persistence with medication by including it as a confounder when exploring the socioeconomic gradient in clinical outcomes.11,17–19 Yet, it is more likely that non-persistence is an intermediate variable that lies within the pathway from socioeconomic factors (SEFs) to MACE; however, it has not been investigated how much the effect of SEFs on MACE is brought about through non-persistence with medication and if this effect differs according to sex. We examined if patients’ level of income and education was associated with risk of MACE and the potential mediating role of non-persistence with secondary preventive treatment. We further evaluated if this mediating role was moderated by sex.
Materials and Methods
Study Design and Setting
This nationwide prospective register-based cohort study with historical data was conducted in Denmark, whose population of 5.8 million inhabitants are all provided with a Central Person Register (CPR) number that eases linkage between nationwide registers. The Danish healthcare system is tax-financed and provides access for all Danish inhabitants to hospital treatment without additional charge. Further, vast prescribed medication bought at pharmacies are reimbursed with modest co-payment by the patient. The percentage of reimbursement increases with expenditures for reimbursable medication within a period of one year, but co-payment is yearly capped at approximately 570 €.20
Study Population
The National Patient Registry (NPR) was used to identify patients hospitalised with an incident primary or secondary diagnosis of ACS (ICD-10: I200, I21, I24) in the inclusion period from 1/1/2010 to 31/12/2017.18 Eligible patients were ≥18 years of age and registered with a CPR number. Patients were excluded if, within the five preceding years before the inclusion period: (1) they were diagnosed with ischemic heart disease (ICD-10: DI20-25), (2) they had emigrated within five years prior to study inclusion, (3) they had not redeemed prescriptions of both antiplatelets and statins within 180 days following incident ACS hospital discharge, (4) they had a negative five-year mean family equalised income level, or (5) their date of death was equal to hospital discharge. Further, any missing exposure data would cause exclusion from the study as these would not fulfil the requirements of multiple imputation. Accordingly, two study populations were established to minimise loss of data and the selection of study participants is presented in Figure 1.
 |
Figure 1 Selection of study population I and II. Abbreviations: ACS, acute coronary syndrome; IHD, ischemic heart disease. |
Socioeconomic Factors
Levels of income and education were used separately as exposure variables to reflect different aspects of socioeconomic position and were obtained from the Population Education Register and the Income Statistics Registry, respectively.21,22 To account for yearly income variation, the level of income was assessed using the mean equalised family income within five years preceding diagnosis of ACS and categorised by tertiles into low (<22,064 €), medium (22,064–31,945 €), or high (>31,945 €). The level of education was categorised according to the International Standard Classification of Education into low (<10 years), middle (10–12 years), or high (>12 years).
Non-Persistence with Medication
Patients were categorised as non-persistent if they had a break in treatment lasting at least 365 days from expected completion of previous redemption until next redemption. After being identified as non-persistent, the assumed time of break was estimated with an induction period of 90 days following the latest registered redemption. This ensured the variable followed the ABC taxonomy and EMERGE medication adherence guidelines.23,24 Moreover, the joint adherence measure definition was based on European guidelines, that recommend lifelong treatment of statin and aspirin in combination with a P2Y12-inhibitor in the initial 12 months following diagnosis of ACS.14,15 The daily drug dose was assumed to be one tablet for each drug. Patients’ use of antiplatelet and statin therapy was identified in the National Prescription Register and the ATC-codes are presented in Suppl. Table S1.25
Clinical Outcomes
The primary outcome was MACE, which was measured as a composite endpoint comprising all-cause death, cardiac death and hospital readmission due to cardiovascular causes. The secondary outcomes comprised non-persistence with medication and each individual component included in the MACE composite measure. The diagnostic codes of cardiac death and cardiac readmission comprised myocardial infarction, stroke, cardiac arrest, chronic heart failure, and ventricular tachycardia/fibrillation (ICD-10 codes are presented in Suppl. Table S1). All information on readmission was based on diagnoses from inpatient contacts and provided by the NPR.
Potential Confounding Factors
All covariates were recognised a priori by literature search, depicted using directed acyclic graphs (Suppl. Figure S1) and included age, sex, ethnicity, civil status, somatic and psychiatric comorbidities. Information on age (<65, 65–74, ≥75 years), sex (male, women), civil status (cohabiting/married, single-living/widow) and ethnicity (Danish, immigrant/descendant) were obtained from the Central Person Register.26 All comorbidity diagnoses were obtained from NPR, where somatic comorbidities were assessed by the Charlson Comorbidity Index (CCI) and divided into none (0 points), moderate (1–2 points), or high (≥3 points) and psychiatric comorbidities were defined by any hospital diagnosis or >1 redeemed prescription of antidepressant or anxiolytic medication within 10 years prior to hospital admission and categorised into current (<90 days), recent (90–364 days), past (1–10 years), or none. Information on redeemed prescriptions was provided by the National Prescription Register. Information about claimed prescriptions of antiplatelet or statin therapy within one year prior to hospitalisation along with percutaneous coronary intervention during hospitalisation or within 60 days following discharge was included for descriptive purposes. ATC and procedure codes are presented in Suppl. Table S1.
Statistical Methods
Baseline patient characteristics were obtained at time of hospital discharge and presented with absolute numbers, percentages and in means and standard deviations where appropriate. Patients were followed from time of hospital discharge until time of endpoint (event), a censoring event (emigration or end of follow-up (December 31, 2018), or competing event (death) where appropriate. Missing data of potential confounding variables were handled by multiple imputation under the assumption of being missing at random and imputed 10 times using all variables presented in Table 1 and relevant outcome variables.
 |
Table 1 Baseline Characteristics of Entire Cohort and Study Population I (Income as Exposure) Stratified by Sex |
Inverse probability of treatment weight was assigned for each patient to balance risk of confounding in both study populations and thereby obtain population average effects.27
The statistical analyses were performed using a three-step structure in both study populations (income level as exposure and educational level as exposure) and stratified according to sex.
In step one, the association between SEFs and subsequent non-persistence with medication was investigated. First, the Aalen Johansen estimator calculated the cumulative incidence along with number of events and event rates in unweighted and weighted analyses. Next, hazard ratios (HR) were calculated from unadjusted and multiple adjusted discrete time survival analyses using cubic splines for every 90-day intervals tied with 4 knots to handle the time-varying variable (non-persistence with medication). Event rates, cumulative incidence and HR were presented with 95% confidence intervals (CI).
In step two, the association between SEFs and risk of adverse clinical outcomes was investigated with similar methods used in step one. The primary outcome was risk of MACE and secondary outcomes were risk of all-cause death, cardiac deaths or cardiac readmission, respectively.
In step three, the mediating role of non-persistence with medication on the association between SEFs and MACE was investigated. Before performing mediation analysis, the causal pathway was depicted using directed acyclic graph to assess if the mediator lied within the causal pathway between exposure and outcome (Figure 2).28 The indirect effect estimated the combined effect of how SEFs influenced risk of non-persistence with medication and how this change in non-persistence subsequently influenced risk of MACE. The population average mediated proportion (indirect effect) was calculated as the relative difference between the total effect and the direct effect and was bootstrapped with 100 samples to provide 95% CI.28
Several sensitivity analyses were undertaken to evaluate the robustness of the results. First, different grace periods were tested to examine if the chosen time measure of 90 days introduced misclassification of non-persistence with medication (30 and 60 days, respectively). Further analyses evaluated the effect of different time limits for initiation of medication (30, 60, 90 and no time limit, respectively). Finally, it was tested if a different categorisation of income that followed the national definition of relative poverty would alter the results. All analyses were performed using STATA version 16 (StataCorp, College Station, Texas).
Ethics
The study was registered with a data processor agreement (RN j. nr. 2019–033827). Registry-based studies in Denmark are not required to gain further ethical approval; moreover, personal health and social information was gathered and analysed in an anonymised form.
Results
Baseline Characteristics
The inclusion of study participants and their baseline characteristics ware presented in Figure 1 and Table 1. Study population I (exposure: income level) and study population II (exposure: educational level) comprised 45,781 and 44,441 patients, respectively (Figure 1). Overall, the median length of follow-up was 1237 days (25th–75th percentile: 525–2102), the mean age was 65.5 years, about one-third of the patients had reimbursed an antiplatelet or statin within a year prior to study inclusion and almost the entire cohort had a minimum one somatic comorbidity diagnosis (Table 1). Baseline characteristics altered according to level of SEFs and sex (Table 1 and Suppl. Table S2).
SEFs and Risk of MACE
Number of events, event rates and HRs of MACE are presented in Figures 3 and 4. During follow-up, 16,365 patients experienced MACE, corresponding to about one-third of the entire study population. Irrespective of sex, higher levels of income and education, both had beneficial associations with risk of MACE, with significantly lower event rates and HRs in unadjusted and adjusted analyses.
In the regression analyses adjusted for age and ethnicity, male patients with middle and high levels of income had 22% (HR: 0.78, 95% CI: 0.75–0.81) and 33% (HR: 0.67, 95% CI: 0.64–0.70) relative lower risk of MACE, compared to low-income male patients (Figure 3). Additional adjustment for educational level, civil status and somatic as well as psychiatric comorbidities only weakened the association slightly. Similarly, male patients with middle and high levels of education had 9% (HR: 0.91, 95% CI: 0.87–0.94) and 21% (HR: 0.79, 95% CI: 0.75–0.83) relative lower risk of MACE compared to low-educated male patients.
Similar associations were observed among women (Figure 4).
The weighted cumulative incidence of MACE started an almost immediate progressively deviation that favoured the patients with higher income and educational level (Figure 5). The largest deviation was observed when assessing level of income (Figure 5).
 |
Figure 5 Cumulative incidence of primary clinical outcome in weighted study populations I and II according to sex. Abbreviations: MACE, major adverse cardiovascular event; CI, confidence interval. |
SEFs and Risk of Non-Persistence with Medication, All-Cause Death, Cardiac Death and Cardiac Readmission
About one-third (37%) of the patients were non-persistent with the combined measure of drugs; however, when assessing the drugs individually, this proportion of non-persistence was altered to about 24% (Figure 6).
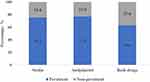 |
Figure 6 Proportion of non-persistence with medication. |
In the unweighted sex-stratified estimates, non-persistence with the joint measure of medication was found in 10,617 (34.2%) men (Figure 3) and 5748 (38.8%) women (Figure 4).
In both unadjusted and adjusted regression analyses, a higher level of income was statistically significantly associated with lower risk of non-persistence with medication among men (Figure 3), but not among women (Figure 4). Further, there was a divergent association between level of education and risk of non-persistence with medication in both sexes; in fact, a higher level of education seemed to increase risk of non-persistence with medication.
Irrespective of sex, a higher level of income had a slightly stronger association with risk of secondary clinical outcomes compared with educational level (Suppl. Figures S2 and S3). The weighted cumulative incidence for all secondary clinical outcomes started to deviate during the initial years and continued to widen in the following years when comparing patients with low vs medium and high levels of SEFs (Suppl. Figures S4 and S5).
Mediating Effect of Non-Persistence with Medication on MACE
Socioeconomic difference in risk of non-persistence was observed in men, but not women, and only in relation to income. Thus, the mediation analysis was restricted to investigating how the income-related gradient in risk of MACE was meditated by non-persistence with medication in men.
Changing a low to a high level of income among men lowered risk of MACE by a factor of 0.67 after adjustment for age and ethnicity. This total effect arose from a direct effect with an HR of 0.71 (95% CI: 0.68–0.74) and an indirect effect with an HR of 0.95 (95% CI: 0.95–0.95) through non-persistence with medication (Table 2). The mediated proportion was 12.6% (95% CI: 11.1–14.1%) among high-income men.
 |
Table 2 The Mediating Effect of Non-Persistence to Medication on the Association Between Income and Risk of MACE Among Men, Adjusted for Age and Ethnicity |
Accordingly, the lower risk of non-persistence observed among high-income men mediated the lower risk of MACE, compared with low-income men. This implied that non-persistence with medication contributed to the income-related inequality in risk of MACE, but only in men.
Supplementary Analyses
To evaluate the robustness of the mediating variable “non-persistence with medication”, different grace periods (data not shown) were analysed along with different times of initiation (Suppl. Table S3 and S4). Further, a different categorisation of income using the national definition of relative poverty was tested (data not shown). Finally, analyses evaluated if non-persistence with statin and antiplatelet therapy, measured as disjointed variables, differed compared to the main results. The mediating proportions ranged from 16–18% for non-adherence to statin therapy and from 6–12% for non-persistence with antiplatelet therapy in men (Suppl. Figures S6 and S7). Overall, these analyses did not cause major attenuations on the associations observed in the main analyses, apart from the mediating proportions regarding non-persistence with statin and antiplatelet therapy.
Discussion
In the present study, higher levels of income and education were associated with lower risk of MACE, irrespective of sex among patients with incident ACS. Further, non-persistence with medication mediated the income-related gradient in risk of MACE, but only in men.
Non-persistence with medication was evaluated as a joint measure of both antiplatelets and statins and this rather conservative and demanding approach was preferred as clinical guidelines call for lifelong antiplatelet and statin therapy following ACS diagnosis.14,15
Corresponding to our results, studies from the Netherlands,4 Denmark29 and Sweden17 all reported income-related inequality in risk of death after incident AMI hospitalisation. Regarding non-persistence with medication, lower levels of income, but not education, have also been associated with lower adherence to medication but more inconclusive findings have been reported when using area-based aggregated data to measure socioeconomic status.30–32 Such inconsistent results may be caused by differences in socioeconomic markers, which can reflect the individual’s resources or the society structure.33
In the present study, approximately 35% of the patients were categorised as non-persistent with the joint therapy measure, which illustrates an overall acceptable level of persistence despite the rather strict requirements. Moreover, about 24% of the patients were non-persistent with either statin or antiplatelet therapy, which resembles findings in studies from Denmark,34 Sweden17 and Canada.35 However, studies comprising more diverse study populations from different healthcare settings have reported overall non-persistence with statins and antiplatelets to be about 40% and this level increased according to the lowering of a country’s economic position.36,37
The event rate of non-persistence to medication was higher in women compared to men in our study, which corresponds to earlier studies reporting female sex to be a determinant of non-adherence to medication.38,39 This level of non-persistence is problematic as pharmacological treatment reduces risk of MACE, also in females who more often suffer from a non-obstructive coronary artery disease that causes a different ischemic endothelial damage profile compared to men.16
Interestingly, there was no social gradient in women regarding risk of non-persistence with medication and this implied that women’s non-persistence instead was determined by other factors than level of education and income.
In the present study, non-persistence with medication had a mediating role on the income-related inequality in risk of MACE among men. This was largely caused by the mediating role of non-persistence with statin therapy; nevertheless, optimal treatment with both drugs is advocated. A similar mediating role of optimal pharmacological treatment was recently reported in heart failure patients.40 The requirements for mediation analysis was not fulfilled among women in our study; however, we observed a social gradient in risk of MACE irrespective of sex, and future studies should explore possible mediating causes for such a tendency.
We consider it less likely that the higher risk of non-persistence with medication among men with low income is caused by cost-related issues as the prices of antiplatelet and statin therapy are low in Denmark combined with Danish rules of general reimbursement. Instead, we assume that income serves as a proxy measure of wealth and life-resources in this setting and that inequality in adverse clinical outcomes most likely is a result of cumulated poor health.
In summary, findings from present study imply that promotion of good persistence with medication may be a way to lower income-related inequality in risk of MACE, especially among men. Further, women have an overall higher level of non-persistence with medication, but this is not associated with socioeconomic differences.
It could be assumed that the mediating effect of non-persistence with medication may be more prominent if the same study design is implemented in a study population with a higher level of non-persistence with medication.
Strengths and Limitations
Major strengths of the present cohort study include the use of register-based exposure, covariates and outcome measures as well as the large sample size due to linkage to nationwide registers, which also limited the risk of loss to follow-up and selection bias. The evaluation of social inequality using both level of income and education increased the understanding of latent socioeconomic association. All confounding variables were further selected a priori by literature search and depictured by directed acyclic graphs, which limited risk of over- and under-adjustment. The thorough statistical approach using mediation analysis robustly displayed the impact of non-persistence with medication and the abundant numbers of supplementary analyses all confirmed the findings of the main results. The findings are assumed to have high external validity as they most likely are more pronounced in other countries with different settings of healthcare structures and higher proportions of patients being non-persistent with medication.
Nonetheless, some limitations must be considered when interpreting the findings of the present study. First, restricting the study population to patients initiating both antiplatelet and statin therapy could introduce selection bias due to opening an otherwise blocked path in the relation between exposure and outcome (please see directed acyclic graph in Suppl. Figure S1). However, results from sensitivity analyses using different time limits for initiation of pharmacological treatment other than the original 180 days all supported the main findings.
Second, estimation of socioeconomic status is a challenge and each socioeconomic variable is an indicator of different social stratification; however, these are only pseudo-markers of a greater picture.41 It should be considered that salary for the same job role is often unequal between sexes, which may bias the role of income. Moreover, there is a risk of introducing gender bias as the social role within a family often differs among males and females. Consequently, research finds females to be less prone to follow the advised lifestyle, eg due to their income level and social role.42 In the present study, this gender bias, along with the pathophysiological sex-difference in coronary artery disease that could act as a background bias, was handled by stratification but the biases should be considered when interpreting the importance of socioeconomic disparity in clinical outcomes.
Third, the most approachable way to measure persistence with medication in large-scale cohort studies is by using register-based prescription data. It was estimated that, due to the medium to long follow-up time, non-persistence would be best addressed using risk of discontinuation in the present study.
Fourth, there may always be a risk of residual or unmeasured confounding despite gathering of covariate information through linkage to national registers.43 Further, the definition of non-persistence with medication in register-based cohort studies relies on assumptions and it may therefore be reasonable to assume that the mediating variable used involved some form of residual confounding caused by misclassification. Consequently, the potential role of non-persistence with medication may be even larger than observed in the present study as any presence of random misclassification in covariates leads the adjusted results towards results obtained in unadjusted analyses.
Therefore, understanding reasons for barriers that facilitate social inequality in risk of MACE ought to be a priority in secondary cardiovascular prevention. Findings from the present study call for further research that investigates the potential mediating mechanisms that influence the socioeconomic gradient in clinical outcomes. These may comprise risk factors including smoking, hypertension, BMI and physical inactivity, which all have been argued as mediators of the association between educational level and risk of primary coronary event.44,45
Conclusion
In this nationwide large-scale cohort study, patients’ level of income and education were significantly associated with risk of MACE during follow-up. We found evidence that non-persistence with medication contributed to the income-related gradient in MACE, but only in men. Further research that investigates the mediating role of non-persistence with medication in different study populations, including those with higher levels of non-persistence, is warranted to understand its potential to reduce the socioeconomic gradient in clinical outcomes.
Data Sharing Statement
Data underlining this article cannot be shared publicly due to Danish law on data protection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Danish Heart Foundation (grant number: 18-R123-A8283-22081).
Disclosure
SPJ has provided consultancy work for Bayer, Bristol Myers Squibb, Pfizer and Sanofi and has participated in advisory board meetings for Bayer, Bristol Myers Squibb and Pfizer. The authors report no other conflicts of interest in this work.
References
1. Mensah GA, Wei GS, Sorlie PD, et al. Decline in cardiovascular mortality: possible causes and implications. Circ Res. 2017;120(2):366–380. doi:10.1161/CIRCRESAHA.116.309115
2. Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356(23):2388–2398. doi:10.1056/NEJMsa053935
3. Joensen AM, Joergensen T, Lundbye-Christensen S, et al. Explaining Trends in Coronary Heart Disease Mortality in Different Socioeconomic Groups in Denmark 1991–2007 Using the IMPACT SEC Model. PLoS One.2018;13(4):e0194793.
4. Stirbu I, Looman C, Nijhof GJ, et al. Income inequalities in case death of ischaemic heart disease in the Netherlands: a national record-linked study. J Epidemiol Community Health. 2012;66(12):1159–1166. doi:10.1136/jech-2011-200924
5. Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes. Circulation. 2018;137(20):2166–2178. doi:10.1161/CIRCULATIONAHA.117.029652
6. Alter DA, Franklin B, Ko DT, et al. Socioeconomic status, functional recovery, and long-term mortality among patients surviving acute myocardial infarction. PLoS One. 2013;8(6):e65130. doi:10.1371/journal.pone.0065130
7. Rasmussen JN, Gislason GH, Rasmussen S, et al. Use of statins and beta-blockers after acute myocardial infarction according to income and education. J Epidemiol Community Health. 2007;61(12):1091–1097. doi:10.1136/jech.2006.055525
8. Pedersen M, Egerod I, Overgaard D, et al. Social inequality in Phase II cardiac rehabilitation attendance: the impact of potential mediators. Eur J Cardiovasc Nurs. 2018;17(4):345–355. doi:10.1177/1474515117746011
9. Jakobsen L, Niemann T, Thorsgaard N, et al. Dimensions of socioeconomic status and clinical outcome after primary percutaneous coronary intervention. Circ Cardiovasc Interv. 2012;5(5):641–648. doi:10.1161/CIRCINTERVENTIONS.112.968271
10. Dalen M, Ivert T, Holzmann MJ, et al. Household disposable income and long-term survival after cardiac surgery. J Am Coll Cardiol. 2015;66(17):1888–1897. doi:10.1016/j.jacc.2015.08.036
11. Nielsen S, Karlsson M, Björklund E, et al. Socioeconomic factors, secondary preventive medication, and long-term Survival after coronary artery bypass grafting: a population-based cohort study from the SWEDEHEART registry. J Am Heart Assoc. 2020;9(5):e015491. doi:10.1161/JAHA.119.015491
12. Hagen TP, Häkkinen U, Iversen T, et al. Socio-economic inequality in the use of procedures and mortality among AMI patients: quantifying the effects along different paths. Health Econ. 2015;24:102–115. doi:10.1002/hec.3269
13. Mårtensson S, Gyrd-Hansen D, Prescott E, et al. Socio-economic position and time trends in invasive management and case fatality after acute myocardial infarction in Denmark. Eur J Public Health. 2016;26(1):146–152. doi:10.1093/eurpub/ckv156
14. Collet J, Thiele H, Germany C, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2020;5:1–79.
15. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39:119–177.
16. Khandelwal A, Bakir M, Bezaire M, et al. Managing Ischemic heart disease in women: role of a women’s heart center. Curr Atheroscler Rep. 2021;23(10). doi:10.1007/s11883-021-00956-x
17. Ohm J, Skoglund PH, Discacciati A, et al. Socioeconomic status predicts second cardiovascular event in 29,226 survivors of a first myocardial infarction. Eur J Prev Cardiol. 2018;25(9):985–993. doi:10.1177/2047487318766646
18. Bernheim SM, Spertus JA, Reid KJ, et al. Socioeconomic disparities in outcomes after acute myocardial infarction. Am Heart J. 2007;153:313–319.
19. Kelli HM, Mehta A, Tahhan AS, et al. Low educational attainment is a predictor of adverse outcomes in patients with coronary artery disease. J Am Heart Assoc. 2019;8(17):e013165. doi:10.1161/JAHA.119.013165
20. Danish Medicines Agency. Reimbursement thresholds. https://laegemiddelstyrelsen.dk/en/reimbursement/calculate-reimbursement/reimbursement-thresholds/
21. Jensen VM, Rasmussena AW. Danish education registers. Scand J Public Health. 2011;39(7_suppl):91–94. doi:10.1177/1403494810394715
22. Baadsgaard M, Quitzau J. Danish registers on personal income and transfer payments. Scand J Public Health. 2011;39(7_suppl):103–105. doi:10.1177/1403494811405098
23. Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. doi:10.1111/j.1365-2125.2012.04167.x
24. De GS, Zullig LL, Dunbar-Jacob J, et al. ESPACOMP Medication Adherence Reporting Guideline (EMERGE). Ann Intern Med. 2018;169(1):30–35. doi:10.7326/M18-0543
25. Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39(7_suppl):38–41. doi:10.1177/1403494810394717
26. Schmidt M, Pedersen L, Sørensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
27. Fewell Z, Hernan MA, Wolfe F, et al. Controlling for time-dependent confounding using marginal structural models. Stata J. 2004;4(4):402–420. doi:10.1177/1536867X0400400403
28. Lange T, Hansen KW, Sørensen R, et al. Applied mediation analyses: a review and tutorial. Epidemiol Health. 2017;39:e2017035. doi:10.4178/epih.e2017035
29. Rasmussen JN, Rasmussen S, Gislason GH, et al. Mortality after acute myocardial infarction according to income and education. J Epidemiol Community Health. 2006;60(4):351–356. doi:10.1136/jech.200X.040972
30. Shimony A, Zahger D, Ilia R, et al. Impact of the community ’ s socioeconomic status on characteristics and outcomes of patients undergoing percutaneous coronary intervention. Int J Cardiol. 2010;144(3):379–382. doi:10.1016/j.ijcard.2009.04.033
31. Biswas S, Andrianopoulos N, Duffy SJ, et al. Impact of socioeconomic status on clinical outcomes in patients with ST-segment-elevation myocardial infarction. Circ Cardiovasc Qual Outcomes. 2019;12(1):e004979. doi:10.1161/CIRCOUTCOMES.118.004979
32. King W, Lacey A, White J, et al. Socioeconomic inequality in medication persistence in primary and secondary prevention of coronary heart disease – a population-wide electronic cohort study. PLoS One. 2018;13(3):1–12. doi:10.1371/journal.pone.0194081
33. Avlund K, Holstein BE, Osler M, et al. Social position and health in old age: the relevance of different indicators of social position. Scand J Public Health. 2003;31(2):126–136. doi:10.1080/14034940210134130
34. Gislason GH, Rasmussen JN, Abildstrøm SZ, et al. Long-term compliance with beta-blockers, angiotensin-converting enzyme inhibitors, and statins after acute myocardial infarction. Eur Heart J. 2006;27(10):1153–1158. doi:10.1093/eurheartj/ehi705
35. Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. J Am Med Assoc. 2007;297(2):177–186. doi:10.1001/jama.297.2.177
36. Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013;34(38):2940–2948. doi:10.1093/eurheartj/eht295
37. Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. 2011;378:1231–1243.
38. Mann DM, Woodward M, Muntner P, et al. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44(9):1410–1421. doi:10.1345/aph.1P150
39. Barrett E, Paige E, Welsh J, et al. Differences between men and women in the use of preventive medications following a major cardiovascular event: Australian prospective cohort study. Prev Med Reports. 2021;22:101342. doi:10.1016/j.pmedr.2021.101342
40. Andersen J, Gerds TA, Hlatky MA, et al. The mediating role of effective treatments in the relationship between income level and survival in patients with heart failure: a sex- and cohabitation-stratified study. Eur J Prev Cardiol. 2021;28:78–86.
41. Galobardes B, Shaw M, Lawlor DA, et al. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7–12. doi:10.1136/jech.2004.023531
42. Sciomer S, Moscucci F, Maffei S, et al. Prevention of cardiovascular risk factors in women: the lifestyle paradox and stereotypes we need to defeat. Eur J Prev Cardiol. 2019;26(6):609–610. doi:10.1177/2047487318810560
43. Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish National patient registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi:10.2147/CLEP.S91125
44. Carter AR, Gill D, Davies NM, et al. Understanding the consequences of education inequality on cardiovascular disease: Mendelian randomisation study. BMJ. 2019;365:1–12.
45. Nordahl H, Rod NH, Frederiksen BL, et al. Education and risk of coronary heart disease: assessment of mediation by behavioral risk factors using the additive hazards model. Eur J Epidemiol. 2013;28(2):149–157. doi:10.1007/s10654-012-9745-z
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



