Back to Journals » Cancer Management and Research » Volume 14
Non-Inferiority Study on the Precise Implementation of Multidisciplinary Continuous Nursing Intervention in Patients with Breast Cancer Experiencing Negative Emotions
Authors Shen J, Wang M, Li F, Li Y, Zhou J, Sun W
Received 20 December 2021
Accepted for publication 17 April 2022
Published 20 May 2022 Volume 2022:14 Pages 1759—1770
DOI https://doi.org/10.2147/CMAR.S354214
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Jun Shen, Meng Wang, Fan Li, Yan Li, Jun Zhou, Wenwen Sun
Department of Breast Surgery, The First People’s Hospital of LianYunGang, The First Affiliated Hospital of Kangda College of Nanjing Medical University, LianYunGang, People’s Republic of China
Correspondence: Wenwen Sun, Department of Breast Surgery, The First People’s Hospital of LianYunGang, The First Affiliated Hospital of Kangda College of Nanjing Medical University, No. 6 Zhenhua East Road, High-Tech Square, LianYunGang, 222002, People’s Republic of China, Tel +86-18961325179, Email [email protected]
Objective: To explore the precise implementation methods of multidisciplinary continuous nursing intervention in patients with breast cancer experiencing negative emotions.
Methods: About 30– 40% of breast cancer patients have negative emotions, and negative emotions can increase the risk of breast cancer death. Team psychological intervention is helpful to improve negative emotions. How to effectively and accurately implement the multidisciplinary continuous nursing model needs further research.We designed a retrospective analysis of 750 patients with breast cancer in our hospital was made. Their baseline characteristics and follow-up data, pre-treatment self-rating anxiety scale (SAS) scores, and scores in the follow-up period after the treatment (SAS_A) were included in the analysis to verify the correlation between an SAS_A score and a prognosis. Risk prediction models were established for the SAS_A score, and they were screened and verified. A non-inferiority study was conducted through the models to explore the feasibility of the precise multidisciplinary continuous nursing intervention in patients with breast cancer experiencing negative emotions.
Results: The prognosis could be distinguished with the SAS_A scores; AUC = 0.8306, a p-value of < 0.0001, and cut-off = 53.5. Based on the Kaplan–Meier (K-M) analysis, the rate of no disease progression of the group with relatively high SAS_A scores was significantly lower than that with relatively low SAS_A scores and a p-value of < 0.0001. A regression analysis was conducted to screen variables including income, operation, family, religion, and SAS scores. The fit.select.v1.lrm model was established, and its concordance index (C-index) was 0.676 (0.622, 0.729). Based on the model calibration curve, Prob = 0.4 was selected. In accordance with the non-inferiority design, the minimum 95% confidence interval (CI) of the mean value difference of the two groups should be greater than the cut-off value. If λ = 20%, the cut-off value was 1.316, and 95% CI was (1.198, 1.4336); the possibility of non-inferiority was refused, but their mean value difference was very close.
Conclusion: It is feasible to precisely implement the multidisciplinary continuous nursing intervention in patients with breast cancer experiencing negative emotions based on the prediction model, but further study is required.
Keywords: multidisciplinary continuous nursing intervention, negative emotions, breast cancer, non-inferiority
Introduction
Breast cancer is the most common malignancy among women. It has surpassed lung cancer as the most commonly diagnosed female malignancy in China.1 Breast cancer accounts for one fourth of female malignancies, and 15% of related deaths.2
Patients with cancer consistently experience different degrees of negative emotions during their diagnosis and treatment,3 especially patients with breast cancer,4,5 of whom 30–40% show negative emotions6 including anxiety or depression.7 The negative emotions can impact their prognosis, and about 60% of patients with metastatic breast cancer are complicated by anxiety and depression.8 Due to the complication of negative emotions, the mortality risk of patients with breast cancer is increased by 19%.9 Group psychological intervention is conducive to the psychological adjustment of patients with breast cancer.10 Conventional nursing models usually provide conventional psychological interventions for patients with breast cancer which have given initial results, but the overall effect is not ideal.11 Multidisciplinary continuous model can improve the negative mood and quality of life of cancer patients, there are successful examples in a variety of tumors.12,13 The importance of the multidisciplinary continuous model has been gradually highlighted because it can improve negative emotions and sleep disorders, therefore improving prognosis.14 However, the combination of multiple disciplines is required in the multidisciplinary continuous nursing model, which is quite difficult; it consumes a large amount of manpower and material resources.15 How to effectively and precisely implement the multidisciplinary continuous nursing model requires further in-depth study.
Materials and Methods
Subjects
A total of 750 patients newly diagnosed with breast cancer that were admitted and received surgical treatment in our hospital from January 1, 2015 to December 1, 2018 were enrolled in this study. Inclusion criteria were as follows: ① Surgical patients pathologically diagnosed with breast cancer; ② No other treatment before the surgery; ③ Age > 18 years old; ④ Karnofsky performance status score > 70; ⑤ Sound comprehensive and cognitive ability; ⑥ Informed consent to this study; ⑦ Complete medical records and follow-up data. Exclusion criteria were as follows: ① Complicated by other part or visceral metastasis, or expected survival time less than 6 months; ② Complicated by other tumors, or once suffering from other tumors; ③ Complicated by relatively severe heart, liver, and kidney diseases; ④ Lactating and pregnant women. All treatments are developed and performed by the same team, and postoperative adjuvant treatments are formulated according to standard guidelines.
Outcome Measures
The patients’ baseline characteristics and follow-up data were extracted from the medical record data system of our hospital. The following information was collected for each patient: name (ID); age (years old); income; operation; tumor, node, metastasis (TNM) stage; marital status; family support; education; religion; self-rating anxiety scale (SAS) score; SAS score in the follow-up period within 2 weeks of the completion of the planned adjuvant postoperative treatment (such as chemotherapy or radiotherapy, excluding endocrine therapy) (SAS_A); prognosis indicators; and follow-up time. Among them, the income was classified as high income (> 4000 yuan/month, RMB) and low income (< 4000 yuan/month, RMB); the operation was classified as a modified radical mastectomy and breast-conserving surgery; TNM stage was based on 2014 NCCN guidelines; marital status was classified as married or unmarried (including divorced and widowed); Treatment regimens were developed according to the guidelines and included chemotherapy and radiotherapy, with all patients receiving chemotherapy and about 16% (120/750) receiving radiotherapy. Family support was classified as good or average (reported by the patients); religion was classified as yes or no; and the SAS was applied. The SAS score on admission and the SAS_A score in the follow-up period after their treatment within 2 weeks were measured, respectively. The prognosis indicators were disease progression events, including visceral metastasis, local recurrence, and regional lymph node metastasis. The patients were followed up through contact by phone and by consulting their inpatient records and outpatient records, with a median follow-up of 24 months (12–36 months).
Statistical Methods
The R 3.6.3 software was adopted for statistical analysis, and the Pearson test and Fisher’s exact test were applied for the correlation analysis between the clinical characteristics and the prognosis. The Kaplan-Meier (K-M) survival curve and the receiver operating characteristics (ROC) curve were drawn using GraphPad 8.0. The generalized linear regression model was utilized to analyze the influence factors of prognosis, and a p-value of <0.05 indicated that the difference was statistically significant. A nomogram was drawn based on the analysis results with the regression model, while the model was interpreted with concordance index (C-index) and calibration curve, then further judged with clinical decision curve and clinical impact curve, and synchronized and visualized with the R software. The t-test was conducted between independent samples, and its results were expressed as mean value ± standard deviation. A p-value of <0.05 indicated that the difference was statistically significant.
Results
SAS_A Score and Disease Progression Events During the Follow-Up Period
As shown in relevant studies, the prognosis of patients with breast cancer complicated by negative emotions was relatively poor, and among these patients suffering from relapse and metastasis, more than half were complicated by negative emotions. As shown in this study, the SAS_A score and the disease progression events were correlated (Figure 1). The difference of the SAS_A score between patients with disease progression events during the follow-up period and those without disease progression events was statistically significant (p < 0.05). The ROC curve reflected that the disease progression events could be effectively distinguished with the SAS_A score, which was consistent with the conclusions drawn from previous studies.9 In this study, area under the ROC curve (AUC) = 0.8306, Std.Error = 0.02353, 95% confidence interval (CI) = 0.7845 to 0.8767, a p-value of <0.0001, cut-off = 53.5, sensitivity = 66.67% (57.20% to 74.95%), and specificity = 86.51% (83.66% to 88.93%). As distinguished by the SAS_A cut-off value based on the KM analysis, it was found that there was a difference between the group with relatively high SAS_A scores and that with relatively low SAS_A scores, a p-value of <0.0001, the median of no events: SAS_Low: Un; SAS_High: 22 months; HR (high–low): 4.085 (2.582–6.462).
Establishment of an SAS_A Score Grouping Predication Model
The SAS_A score was the SAS score measured in the follow-up period after treatment and was correlated with the disease progression. Previous studies showed that the multidisciplinary continuous nursing model would improve the patients’ negative emotions and lower the SAS_A score. With the reduction of the SAS_A score after the intervention, the patients’ disease progression events were further improved.
Baseline Data and Univariate Analysis
The correlation of observation indicators included with the SAS_A score was studied. As shown in the univariate analysis, the initial indicators such as SAS score, income, operation, marital status, and family were significantly correlated with the SAS_A score (p < 0.05); their OR value was an SAS score of 1.0643, income (low: high) 1.5631, operation (MRM: LUM) 0.3935, marital status (unmarried: married) 0.5033, family (average: good) 0.5963, respectively, which indicated that a high initial SAS score, low income, modified radical mastoidectomy, unmarried status, and average family support were risk factors that affect an SAS_A score (Table 1).
 |
Table 1 Baseline Indicators and Univariate Analysis |
Multivariate Analysis
The observation indicators were included to conduct the multivariate analysis of full independent variables and analyze the correlations between independent variables and the SAS_A grouping (Table 2). It was found in the multiple factor regression analysis that the observation indicators, such as initial SAS score, income, operation, family, and religion, were correlated with the outcome.
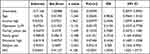 |
Table 2 Multivariate Analysis |
Variable Selection
It was found in the test of every independent variable VIF that the indicators, including age, income, education, and religion, were larger than five, and there was a possibility of collinearity. LASSO analysis could decrease the high-dimensional data by regularization and select relevant factors, which were the best prediction characteristics.16,17 The characteristics with non-zero coefficients were screened with the LASSO regression model18 (Figure 2). When lambda = 0.000432, the model fitting degree was the best option; it was found through regularization scheme that when lambda.1se = 0.06187291 (red dotted line), the scope of variables included was similar to Figure 2A, and when lambda.min = 0.001672241 (blue dotted line), it indicated that the SAS was the most significant indicator in the model.
 |
Figure 2 LASSO regression results (A and B). |
With the combination of multiple factor regression analysis results, three models were respectively established for the three scenarios of LASSO regression. All indicators, including age, income, operation, marital status, family, education, religion, SAS score, etc., were included in the fit.all.lrm model. Income, operation, family, religion, and SAS score were included in the fit.select.v1.lrm model, while operation, family, and SAS score were included in fit.select.v2.lrm model.
Validation of Their Efficiency
The models were assessed and screened respectively based on the AUC, C-index, calibration curve, clinical decision, and benefit curves, etc. The C-index and the AUC of the three models were further calculated to assess the efficiency of the models (Table 3). The ROC curve and the calibration curve (Figure 3) were drawn, and it was found that the fit.all.lrm model and the fit.select.v1.lrm model had better prediction efficiency, with more significance in the fit.select.v1.lrm model, whose curve was closer to the ideal prediction curve. It could be concluded from the Figure 3 that when the prediction probability cut-off = 0.4 and 0.6, the curve deviated from the ideal prediction curve to an underestimated risk (about 10%), providing the basis for the selection of a cut-off value in subsequent studies.
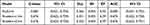 |
Table 3 C-Index and AUC Value of Three Models |
 |
Figure 3 The ROC curve (A) and the calibration curve (B) of three models. |
The clinical decision curve analysis (DCA) is a simple mathematical model for assessing the feasibility and efficiency of a prediction tool. In accordance with relevant literature,19 in the circumstance that the possibility of patients with breast cancer suffering from negative emotions was predicated at 35% (30–40%), the clinical decision advantages were shown in the three models. The clinical impact curve (CIC) helped to judge the degree of clinical benefit. The red curve (number high risk) referred to the number of persons classified as positive (high risk) in the model at each threshold probability; the blue curve (number high risk with outcome) referred to the number of persons classified as true positive at each threshold probability (Figure 4). In the three models, when the prediction probability = 0.4, the two curves became closer, and when the prediction probability = 0.6, they were basically overlapped.
Visualization of the Models
The nomogram is used to summarize and visualize multiple prediction indicators based on the multiple factor regression analysis. With the nomogram, each indicator can be assigned and the line segment with scales can be drawn, which is convenient for clinical application.20 Based on the comparison of the models, the fit.select.v1.lrm model was adopted for the nomogram (Figure 5), as an inclusion criterion in subsequent studies.
 |
Figure 5 Fit.select.v1 nomogram. |
Non-Inferiority Study Design
It was indicated in previous studies that if all patients received the multidisciplinary continuous intervention, the SAS score at the end of the treatment (the SAS_A score) would be lowered to the greatest extent, and the patients’ prognosis would be improved. However, it requires a large amount of manpower and material resources to provide multidisciplinary continuous intervention for all patients, so it is difficult for clinical application.21 Our study showed that after the patients were screened with the models and received the multidisciplinary continuous nursing intervention, their SAS_A score were lowered, so the non-inferiority study was designed to explore whether the precise implementation of the intervention model could be promoted. The positive control group (group 1) was established, and all patients in the group received the multidisciplinary continuous nursing intervention; in the observation group (group 2), all patients were assessed with the models after enrollment, and if in the high-risk predication probability > 0.4, they received the multidisciplinary continuous nursing intervention. There were patients receiving the conventional nursing intervention in group 2, so no negative control group was designed in this study.
Determination of Sample Size and Cut-off Value
The one-tailed test level α = 0.05, and the permitted type II error probability assumed would not exceed β = 0.2. In accordance with the formula N = 2 × [(ua + uβ)·s/δ]2, the sample size was calculated. Based on the mean value change method δ = λ(p − c) (p was the mean value of the positive control group, and c was the mean value of the negative control group), the literature showed that the λ value would be 5%–20%, which depended on the clinical decision and the study design. It could be learned from the previous data and the preliminary study that s = 2.6 and p − c referred to the mean value difference of the SAS_A score after the multidisciplinary continuous nursing intervention and the conventional nursing intervention. The result of our preliminary study was roughly equivalent to five, and it was stabilized with the increase of the p − c value, so it was finally determined that when a = 0.05, β = 0.2, and λ = 0.2, and if the loss rate in the follow-up visits was not larger than 5%, the number of persons enrolled in each group was 90.
Study Process and Baseline Table
The nursing models were divided into the multidisciplinary continuous nursing model group and the conventional nursing model group. According to the previous successful literature and experience combined with the conditions of our hospital,22–24 we set up the multi-disciplinary continuous nursing mode. The routine nursing mode group provided routine nursing, including routine health education, relevant preoperative and postoperative education manuals, postoperative routine rehabilitation, exercise, diet nursing and medication guidance, etc. The multi-disciplinary continuous nursing mode group added multi-disciplinary combined guidance on the basis of conventional nursing, including the following contents: breast specialists judged the postoperative recovery of patients, and decided follow-up treatment plan according to the patient pathology combined with the patient’s own situation; After evaluating patients’ body function status, rehabilitation physicians add rehabilitation exercise for postoperative motor function of breast cancer on the basis of routine rehabilitation exercise, evaluate patients’ rehabilitation efficacy and safety in the implementation process, and guide patients’ postoperative limb function exercise; Psychological practitioner is responsible for all of the patients with psychological status and to evaluate the sleep state, at the same time for multidisciplinary joint group of patients nursing mode in the initial evaluation reflects the psychological problems and sleep disorders were analyzed, and formulate and implement corresponding psychological intervention, so as to further improve the patients’ cognitive level and self-adaptation ability, according to the evaluation results to psychological counseling, For anxiety, fear and other negative emotions, guide patients to have an objective and correct understanding of breast cancer, eliminate inner fear; Under the relaxed and soothing background music, the use of inducing language to help patients relax and relieve their negative psychological state; Nutritional physicians evaluate the nutritional status of patients, provide nutritional adjustment programs, and specialized nursing staff carry out patient education, to further accelerate postoperative rehabilitation of patients and improve immune capacity and carry out telephone follow-up after discharge.The operational staff and the patients were double-blinded and grouped with the random number table method. The patients randomized into group 1 received the multidisciplinary continuous nursing intervention after the baseline assessment, the patients randomized into group 2 were predicted with the predication model after the baseline assessment, and patients with probability > 0.4 received the multidisciplinary continuous nursing intervention; all other patients received conventional nursing. See Table 4 for the detailed baseline conditions. There was no statistical difference in the age, income, operation, family, religion, and SAS score between the two groups of patients.
 |
Table 4 Baseline at Enrollment |
Non-Inferiority Conclusion
Between the group with the multidisciplinary continuous nursing intervention model and the group with the conventional nursing, the SAS_A score of the intervention group was significantly lower, the mean value difference of the two groups was 6.58 ± 0.298, 95% CI was 5.992 to 7.168, and p < 0.0001. In the comparison between group 1 and group 2, the statistical difference was found, p = 0.0042, the mean value difference of the two groups was 1.284 ± 0.4821, and 95% CI was 0.2293 to 2.339. In the comparison between group 2 and the conventional nursing group, there was a statistical difference, p < 0.0001, the mean value difference was 4.675 ± 0.6754, and 95% CI was 3.339 to 6.011. In group 1 and group 2, the SAS score and SAS_A score before and after the intervention indicated that the patients in the two groups were benefited as a whole (p < 0.0001). In further analysis, compared with the persons classified as low risk in the prediction model, the persons classified as high risk in the prediction model and receiving the multidisciplinary continuous nursing intervention showed better results, and their difference had statistical significance (p < 0.0001) (Figure 6). Based on the design, the minimum 95% CI value of the mean value difference between group 1 and group 2 should be larger than the cut-off value. If λ = 20%, the cut-off value was 1.316, and 95% CI was (1.198, 1.4336); the possibility of non-inferiority was refused, so this study did not demonstrate the non-inferiority of the model that patients are screened based on the prediction model and then receive the multidisciplinary continuous nursing intervention and the model that all patients receive the multidisciplinary continuous nursing intervention.
Discussion
Breast cancer, a high-incidence disease in China, has exceeded lung cancer, ranking first among malignancies in females, and severely affecting female patients’ health. Negative emotions, including anxiety and depression, may lower the patients’ immunity and further impact their prognosis. The multidisciplinary continuous nursing intervention model includes the continuous nursing intervention conducted in and out of the hospital through psychological intervention, nutritional support, rehabilitation training, etc. to effectively improve the patients’ negative emotions. The multidisciplinary continuous nursing intervention model for all patients with breast cancer can effectively improve their negative emotions, but the multidisciplinary continuous nursing intervention model requires the combination of multiple disciplines with large-scale manpower and material resources. This study aims to explore a new nursing model for the precise implementation of multidisciplinary continuous nursing, and thus achieve the expected results.
The prediction model combining multiple indicators has been widely applied in clinical practice, and the nomogram has been deemed as a tool that can be more easily and accurately applied in clinical assessment, and is conducive to consideration from many aspects, thus making better clinical decisions.25 The patients with newly diagnosed breast cancer receiving treatment in our hospital were collected and analyzed, confirming the correlation between the negative emotions and the prognosis. In the multivariate analysis, the initial SAS score, income, operation, family, religion, and SAS_A score were significantly correlated. The initial SAS score showed the baseline state of negative emotions; income, family, and religion reflected the basic change of negative emotions; operation reflected the impact of surgical stress on negative emotions. The comparison and verification of different models were visualized with a nomogram, providing the basis for subsequent studies. In the design of the non-inferiority study, λ = 20%, α = 0.05 (single-tailed), and β = 0.2 (with the confidence of 80%). Compared with the conventional nursing group (hereinafter referred to as the conventional group), the group with the multidisciplinary continuous nursing intervention model (hereinafter referred to as the intervention group) had a significantly lower SAS_A score, the mean value difference of the two groups was 6.58 ± 0.298, and 95% CI was 5.992 to 7.168 (it was set as P). In the comparison of the randomized group 1 and group 2, the mean value difference of the two groups was 1.284 ± 0.4821, and 95% CI was 0.2293 to 2.339 (it was set as T). The mean value difference of Group 2 and the conventional group was 4.675 ± 0.6754, and 95% CI was 3.339 to 6.011 (it was set as C). P was used as the positive intervention control, T was used as the control between groups, and C was used as the negative control. When T − C > −(1 − λ)(C − P), the non-inferiority was established. If λ = 20%, the critical value was 1.316, and 95% CI was (1.198, 1.4336). Based on 1.284 ± 0.4821, and 95% CI (0.2293, 2.339), the possibility of non-inferiority was refused. This study did not demonstrate the non-inferiority of the model in which the patients were screened based on the prediction model and then received the precision multidisciplinary continuous nursing intervention and the model in which all patients received the multidisciplinary continuous nursing intervention. The reason might be that when the prediction value probability > 0.4 was selected, the persons classified as high risk in group 2 accounted for about 50%, which means that about half of the patients in group 2 did not receive the intervention. Although it was found in the subsequent analysis that compared with the persons classified as low risk in the prediction model, those classified as high risk in the prediction model and receiving the multidisciplinary continuous nursing intervention showed better results, and their difference was statistically significant (p < 0.0001); such advantage could not balance the impact caused by the reduction of persons receiving the intervention. Instead, the following aspects should be taken into consideration. First, the intervention of all patients can effectively lower the SAS_A score, but if the patients are divided into high-risk patients and low-risk patients, and given specific intervention, the high-risk patients will obtain more benefits from the intervention, and the intervention benefits are more easily transferred to clinical prognosis benefits; whether the intervention given to the low-risk patients will be effectively transferred to clinical prognosis benefits requires further studies. Second, their mean value difference was 1.316 vs 1.284, which is very close. If the input of manpower and material resources is taken into consideration, this method did not receive the evidence of a statistical difference, but it can be used as an option for the implementation of early intervention.
Conclusion
Based on the retrospective study data, this study rediscussed the correlation between negative emotions and disease progression and further verified that negative emotions had an impact on the patients’ prognosis. Models were established based on regression and visualized with a nomogram for the purpose of providing guidance for clinical decisions and precisely implementing the multidisciplinary continuous nursing model. The reason the non-inferiority statistical difference was not obtained from its subsequent clinical verification might be related to the selection of the predication cut-off value, but its potential advantages are exciting, and further studies are expected based on large-scale clinical observation. Based on the characteristics of retrospective studies and limitations of researchers, more further studies are expected.
Ethics Approval
This study was conducted with approval from the Ethics Committee of The First People’s Hospital of LianYunGang. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi:10.3322/caac.21262
3. Yi JC, Syrjala KL. Anxiety and depression in cancer survivors. Med Clin North Am. 2017;101(6):1099–1113. doi:10.1016/j.mcna.2017.06.005
4. Keeling M, Bambrough J, Simpson J. Depression, anxiety and positive affect in people diagnosed with low-grade tumours: the role of illness perceptions. Psychooncology. 2013;22(6):1421–1427. doi:10.1002/pon.3158
5. Ahmadian M, Samah AA, Saidu MB. An outline of the need for psychology knowledge in health professionals: implications for community development and breast cancer prevention. Asian Pac J Cancer Prev. 2014;15(12):5097–5105. doi:10.7314/APJCP.2014.15.12.5097
6. Li L, Li X, Han D, et al. A longitudinal study of psychological distress and its influencing factors in breast cancer patients. Chin J Nurs. 2020;55(08):1140–1146.
7. Von Ah D, Habermann B, Carpenter JS, Schneider BL. Impact of perceived cognitive impairment in breast cancer survivors. Eur J Oncol Nurs. 2013;17(2):236–241. doi:10.1016/j.ejon.2012.06.002
8. Koopman C, Nouriani B, Erickson V, et al. Sleep disturbances in women with metastatic breast cancer. Breast J. 2002;8(6):362–370. doi:10.1046/j.1524-4741.2002.08606.x
9. Li DG, LeCompte G, Golod L, et al. Dermal carotenoid measurement is inversely related to anxiety in patients with breast cancer. J Investig Med. 2018;66(2):329–333. doi:10.1136/jim-2017-000546
10. Weis JB, Gschwendtner K, Giesler JM, Adams L, Wirtz MA. Psychoeducational group intervention for breast cancer survivors: a non-randomized multi-center pilot study. Support Care Cancer. 2020;28(7):3033–3040. doi:10.1007/s00520-019-05076-6
11. Brown T, Cruickshank S, Noblet M. Specialist breast care nurses for support of women with breast cancer. Cochrane Database Syst Rev. 2021;2:CD005634. doi:10.1002/14651858.CD005634.pub3
12. Borras JM, Albreht T, Audisio R, et al.; European Partnership Action Against Cancer consensus group. Policy statement on multidisciplinary cancer care. Eur J Cancer. 2014;50(3):475–480. doi:10.1016/j.ejca.2013.11.012
13. Harris RE, Ichesco E, Cummiford C, et al. Brain connectivity patterns dissociate action of specific acupressure treatments in fatigued breast cancer survivors. Front Neurol. 2017;8:298. doi:10.3389/fneur.2017.00298
14. Casellas-Grau A, Font A, Vives J. Positive psychology interventions in breast cancer. A systematic review. Psychooncology. 2014;23(1):9–19. doi:10.1002/pon.3353
15. Tsai CH, Hsieh HF, Lai TW, Kung PT, Kuo WY, Tsai WC. Effect of multidisciplinary team care on the risk of recurrence in breast cancer patients: a national matched cohort study. Breast. 2020;53:68–76. doi:10.1016/j.breast.2020.07.001
16. Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw. 2010;33(1):1–22. doi:10.18637/jss.v033.i01
17. Sauerbrei W, Boulesteix AL, Binder H. Stability investigations of multivariable regression models derived from low- and high-dimensional data. J Biopharm Stat. 2011;21(6):1206–1231. doi:10.1080/10543406.2011.629890
18. Kidd AC, McGettrick M, Tsim S, et al. Survival prediction in mesothelioma using a scalable Lasso regression model: instructions for use and initial performance using clinical predictors. BMJ Open Respir Res. 2018;5(1):e000240. doi:10.1136/bmjresp-2017-000240
19. Bao G, Mi Y. Effects of fear, discharge preparation and family function on quality of life in breast cancer patients undergoing chemotherapy. Chin J Pract Nurs. 2019;37(10):721–726.
20. Chen L, Wen Y, Zhang J, et al. Prediction of radiotherapy response with a 5-microRNA signature-based nomogram in head and neck squamous cell carcinoma. Cancer Med. 2018;7(3):726–735. doi:10.1002/cam4.1369
21. Liu Y, Yao C, Chen Q, Su B. Sample size estimation and statistical inference in noninferiority/equiavalence trials. Chin J N Drugs. 2003;12(5):371–376.
22. Victoria Cerezo M, Ortiz-Tallo M, Cardenal V, De la Torre-luque A. Positive psychology group intervention for breast cancer patients: a randomised trial. Psychol Rep. 2014;115(1):44–64. doi:10.2466/15.20.PR0.115c17z7
23. Rui A, Xu Q, Yang X. Effect of multidisciplinary cooperative continuous nursing on the depression, anxiety and quality of life in gastric cancer patients. Am J Transl Res. 2021;13(4):3316–3322.
24. Han D, Wang D, Yang J, Li X. Effect of multidisciplinary collaborative continuous nursing on the psychological state and quality of life of patients with cervical cancer. Am J Transl Res. 2021;13(6):6654–6661.
25. Wei L, Champman S, Li X, et al. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: a cross-sectional study in China. BMJ Open. 2017;7(10):e017293. doi:10.1136/bmjopen-2017-017293
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



