Back to Journals » Journal of Inflammation Research » Volume 16
Nomogram Based on Preoperative Absolute Lymphocyte Count to Predict Local Recurrence in Patients with Non-Small Cell Lung Cancer After Microwave Ablation
Authors Lv Y , Liu Y, Li K, Liu Z, Zhang T, Duan M, Chen Y, Ma T, Huang G , Huang Z
Received 30 December 2022
Accepted for publication 12 April 2023
Published 21 April 2023 Volume 2023:16 Pages 1761—1770
DOI https://doi.org/10.2147/JIR.S402108
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Yonghui Lv,1 Yuanwei Liu,1 Kaiguo Li,1 Zhiling Liu,1 Tong Zhang,1 Mingguang Duan,1 Yunchao Chen,1 Teng Ma,1 Guanghui Huang,2,* Zhaoqin Huang1,*
1Department of Radiology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, Shandong, 250000, People’s Republic of China; 2Department of Oncology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, Shandong, 250000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Guanghui Huang, Department of Oncology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, No. 9677 Jingshi Road, Lixia District, Jinan, Shandong, 250012, People’s Republic of China, Email [email protected] Zhaoqin Huang, Department of Radiology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, No. 324, Jingwu Road, Huaiyin District, Jinan, Shandong, 250012, People’s Republic of China, Email [email protected]
Purpose: This study aims to investigate the prognostic value of preoperative absolute lymphocyte count (preALC) for non-small cell lung cancer (NSCLC) after microwave ablation (MWA) and build a combined nomograph with clinical features to predict the local recurrence.
Patients and Methods: A total of 118 NSCLC patients who underwent microwave ablation were enrolled in this study. The median local recurrence-free survival (LRFS) was 35.5 months. Independent prognostic factors obtained by multivariate analysis were included in the prediction model. The prognostic value of the model was assessed by the area under the time-dependent receiver operating characteristic curve (T-AUC).
Results: Histological subtype and preALC were independent risk factors for local relapse-free survival. According to the time-dependent receiver operating characteristic curve (T-ROC), the optimal cut-off value of preALC was 1.965× 109/L, the sensitivity was 0.837, and the specificity was 0.594. The area under the T-ROC curve (AUC) of preALC was 0.703. To establish a nomogram to predict the local recurrence rate of NSCLC after MWA based on the prognostic factors revealed by Cox regression.
Conclusion: Preoperative lymphocyte count reduction is associated with poor prognosis of NSCLC. The nomogram model combined with preALC can provide a good individualized prediction of local recurrence after microwave ablation.
Keywords: non-small cell lung cancer, microwave ablation, nomogram, preoperative absolute lymphocyte count
Introduction
Lung cancer is the most common cause of cancer mortality globally.1 Surgical resection is the standard treatment for patients with early NSCLC.2 However, it is estimated that 25% of patients with non-small cell lung cancer (NSCLC) are not suitable for curative resection because of medical comorbidities,3 who need an alternative local treatment, such as stereotactic body radiation therapy (SBRT), radiofrequency ablation (RFA), or microwave ablation (MWA). MWA with higher convection and lower heat deposition effect in the lung can maximize the preservation of normal lung tissue,4 which is suitable for patients with chronic obstructive pulmonary disease and pulmonary fibrosis.5 Prediction of early local recurrence after MWA is very important to improve the prognosis of NSCLC patients. The latest guidelines recommend using a 1 cm frosted glass shadow around the lesion after thermal ablation to determine whether the lesion is completely ablated.6 However, this subjective evaluation method is difficult to make a consistent result due to the impact of bleeding or exudation.
The occurrence and development of inflammation played an important role in determining the clinical course and outcome in some solid malignancies and could be used to predict the prognosis of patients with a variety of malignant tumors.7,8 Lymphocytes are the main immune cell and play an important role in host anticancer defense mechanisms.9 Preoperative lymphocytopenia was associated with poor prognosis.10–12 Absolute lymphocyte count (ALC) had been used to evaluate the prognosis of lung cancer.13–15 However, these studies investigated the evaluation of ALC in lung cancer patients who underwent resection15 or chemoradiotherapy.13,14 In addition, numerous studies in recent years have demonstrated that tumor ablation can induce anti-tumor immune responses, primarily by causing tumor cell necrosis, further antigen release, and then antigen presenting cells (APC) to present tumor antigens to effector cells that migrate to other parts of the disease and enhance the immune response.16 This may also be a factor in the influence of pre-ablation lymphocyte count on the recurrence of lung cancer after ablation. As far as we know, there are no study to evaluate the prognostic value of preoperative absolute lymphocyte count (preALC) in lung cancer with MWA therapy.
The study was to explore the predictive value of preALC for local recurrence of lung cancer after MWA and establish a combined nomograph prediction model with clinical information to predict the local recurrence of NSCLC after microwave ablation (MWA) therapy.
Method
Patient Selection
This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Biomedical Research Ethic Committee of Shandong Provincial Hospital (ethics number: 2022–582), informed consent was waived due to the retrospective nature of this study. All personal identification data were anonymized and deidentified before analysis. We retrospectively analyzed 404 patients with confirmed or suspected lung cancer who were treated with MWA in our hospital from January 2010 to June 2018. The patients were screened according to the inclusion and exclusion criteria. The inclusion criteria were as follows: (1) pathological diagnosis as primary non-small cell lung cancer; (2) chest CT scan were performed before MWA within 1 week, and the cTNM stage was classified as T1∼2N0M0 based on CT/MRI imaging; (3) no anticancer therapy before MWA treatment; (4) hematology examination was evaluated within 1 week before MWA (including lymphocytes, white blood cells, neutrophils, monocytes and so on); (5) no infection during peripheral blood collection. The exclusion criteria were as follows: (1) pathological diagnosis: small cell lung cancer or other carcinoma; (2) concomitant other malignancy before MWA; (3) lymph node metastases or distant metastases were present in CT/MRI imaging; (4) incomplete clinical pathological data; (4) patients lost information on follow-up (Figure 1).
 |
Figure 1 Patient selection flowchart. Abbreviations: PLC, primary lung cancer; MWA, microwave ablation; NSCLC, non-small cell lung cancer; SCLC, small cell lung cancer. |
Imaging Analysis
NSCLC tumor staging was determined by the clinical TNM staging system of the International Union for Cancer Control (8th edition).17 All NSCLC patients underwent chest CT (Discovery, GE Healthcare, Chicago, IL) prior to MWA surgery, and all CT imaging was reviewed by two radiologists with more than 5 years of experience in chest radiology to assess tumor location, size, density, presence of lymph nodes, and distant metastases. All laboratory tests were performed within one week prior to MWA.
Patient’s Follow Up
Patients with NSCLC were reexamined with chest enhanced CT 4–6 weeks after MWA and considered as baseline. The follow-up strategy: every 3 months within 2 years and every 6 months after 2 years by chest CT. The primary endpoint was local recurrence-free survival (LRFS), which was defined as the time from MWA surgery to the first occurrence of LR or patient death. When there had no follow-up information on the date of last follow-up, it was considered as lost follow-up. However, lost follow-up patients who met the 1-, 2-, and 3-year LRFS follow-up criteria were included in the study to increase sample size and improve the study results. Local response was assessed by the modified response evaluation criteria in solid tumors (mRECIST 1.1).18
MWA Procedure
All MWA procedures were performed by two radiologists with more than 5 years of experience in CT-guided interventional procedures. The microwave system used (Nanjing Eigao Microwave Research Institute, Nanjing, China) consists of a microwave generator and a hollow water-cooled shaft antenna, a flexible coaxial cable and a microwave generator. The operating frequency is 2450 ± 50 MHz, the maximum output power is 70W. In this study, 18G (diameter) ×180 mm (effective length) water-cooled microwave needle was used to puncture tumors under CT guidance. Preoperative CT was performed to inform the treatment plan, determine the appropriate body position, puncture site location, optimal puncture trajectory, and number of MWA needles. The patient was placed in the supine or oblique position depending on the tumor location. 0.2 g of 2% lidocaine and 37.5 mg bupivacaine were diluted to 50 mL with normal saline, and appropriate amounts were taken for local infiltration anesthesia. The needle was introduced to the planned site, and the location was confirmed by CT. Subsequently, tumor MWA was performed, and the power and duration were adjusted as needed. The procedure was terminated when the ablation zone presented a 5–10 mm edge beyond the lesion boundary. A chest CT scan was performed immediately after ablation to assess the ablation area and detect possible complications. Simultaneous coaxial cannula biopsy was performed in all patients.
Statistical Analysis
The optimal cutoff values for preALC were calculated based on the maximum Youden index (sensitivity+specificity-1) point on the time-dependent receiver operating characteristic curve (t-ROC) for the prediction of LRFS. Survival curves were plotted using Kaplan-Meier method and compared using logarithmic rank test. Cox’s regression model was used for univariable and multivariable analyses. In the univariate analysis, P values <0.05 was entered into the multivariate Cox regression analysis as a candidate variable. The nomogram was constructed according to the result of the univariate and multivariate analysis. The concordance index (C-index) was applied to measure the discrimination of the model. The identification ability of the model was evaluated by calculating the area under the curve (AUC). Decision curve analysis (DCA) was used to assess the net benefit and clinical performance of the nomogram. The IBM SPSS version 26.0 software (IBM Corp.) and R software version 4.2.1 will be utilized for statistical analyses. All tests of significance were two-tailed, and P values <0.05 were taken to indicate significant differences.
Results
Baseline Characteristics
A total of 118 NSCLC patients (69 males and 49 females) were enrolled, of which 47 patients showed local recurrence and 71 patients did not show local recurrence, with an overall local recurrence rate of 39.8% and the median LRFS was 35.5 months. 94 patients (79.7%) had adenocarcinoma; 52 patients (44.1%) had smoking history.; 13 patients (11.0%) had preoperative CEA ≥ 10 ng/mL. Detailed baseline characteristics are shown in Table 1.
 |
Table 1 Baseline Characteristics of the 118 Patients in This Study |
The Cutoff Values of Absolute Lymphocyte Count (preALC)
According to the t-ROC curve, the optimal cutoff values of the preALC were 1.965 × 109/L, with sensitivity of 0.837 and specificity of 0.594, respectively (Figure 2). The AUCs of the t-ROC curves for the preALC were 0.703. Survival analysis indicated that the difference in LRFS between the high and low preALC groups was statistically significant (Figure 3).
 |
Figure 2 Time-dependent ROC of preALC. |
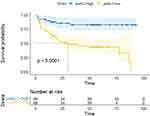 |
Figure 3 Kaplan-Meier survival curve. |
Construction of the Nomogram for LRFS
Univariate analysis showed that histological subtype, CEA level, and preALC were risk factors for poor LRFS in NSCLC patients receiving MWA (p < 0.05). Histological subtype and preALC were included in multivariate analysis to construct a nomogram. Histological subtype (HR = 2.595, 95% CI = 1.412–4.768, P = 0.002), and preALC (HR = 0.221, 95% CI = 0.101–0.482, P ≤ 0.001) were independent prognostic factors of LRFS (Table 2). These indicators were further included in the construction of the nomogram prediction model (Figure 4).
 |
Table 2 Analysis of Prognostic Factors for LRFS |
 |
Figure 4 Nomogram and correction curve. (A) Nomogram for predicting based on preALC. (B) LRFS calibration curves used to predict 1, 2, and 3 years in NSCLC patients after ablation. |
Calibration, Validation and Decision Curve Analysis of the Nomogram
The prediction ability of the model was evaluated by calculating the C index, which was 0.693, indicating that the nomogram had good prediction accuracy. The correction curve showed that the prediction of 1-year, 2-year, and 3-year local recurrence rates with MWA treated NSCLC patients based on pre-ALC and histological subtypes, especially the results within 1 year, were in good agreement with the actual observed results (Figure 4).
The time-dependent ROC curve was used to evaluate the prognostic effect of independent prognostic factors in predicting local recurrence. We found that the model had the best predictive performance at 1 year (AUC of 0.688), which was better than that at 2 and 3 years (AUC of 0.606 and 0.612) (Figure 5).
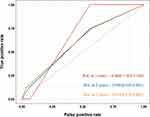 |
Figure 5 Time dependent ROC of nomogram. |
The DCA shows the satisfactory benefit of a line graph under threshold probabilities (Figure 6).
 |
Figure 6 DCA of the nomogram for (A) 1 years, (B) 2 years and (C) 3 years. |
Discussion
Local tumor recurrence is a key problem after MWA of NSCLC. Early identification of risk factors for local recurrence and adjustment of treatment plan can improve the prognosis of NSCLC patients. In this study, the findings showed that early-stage NSCLC patients with reduced absolute lymphocyte value before MWA treatment were more likely to have local recurrence.
Previous studies have shown that the occurrence and progression of most cancers is related to chronic inflammation,19 and ALC was associated with the prognosis of patients with a variety of malignant tumors.10–12 Inflammatory factors have been used to predict the prognosis of some malignant tumors. Different inflammatory cells have both pro-tumor and anti-tumor properties. Rabold’s study proposed that T lymphocytopenia was associated with a poor prognosis in patients with advanced thyroid cancer.20 Teck Seo’s study reported that chemotherapy-related lymphocytopenia was an independent prognostic factor for adjuvant chemotherapy after potentially curative surgery in colorectal cancer patients.21 In our study, multivariate analysis revealed that preoperative ALC and histological subtype were predictive markers of LRFS in NSCLS. Patients with preoperative lymphocytopenia were more likely to have local recurrence than those who exhibited relatively high preoperative ALC. This result suggests that the reduction of peripheral blood lymphocyte count is one of the reasons for the poor prognosis of NSCLC patients, which was consistent with the previous findings.13 However, most previous studies have evaluated the impact of lymphocyte count on distant progression and overall survival of lung cancer patients, few studies have studied the impact on the outcome of simple local recurrence. In this study, combined with preoperative ALC, early local recurrence after early NSCLC MWA was predicted. The diagnosis of simple local recurrence is very important for local recurrence case because MWA ablation can be repeated at the same site,22 which is meaningful to guide the clinical determination of the next treatment plan.
At present, the exact mechanism of the prognostic value of peripheral blood lymphocyte count in cancer patients remains unclear. Several theories could explain this connection. T lymphocytes mediate cellular immunity and play an important role in anti-tumor immune response. T cells can generally be divided into CD4+ T cells, CD8+ T cells, memory T cells and natural killer T cells.23 CD8+ T cells are the core participants of anti-tumor immunity, and their cytotoxic activity against tumor cells can destroy tumor cells. CD4+ T cells, especially Th1 subsets, control cell-mediated antitumor immunity and can assist CD8+ T cells to participate in cellular immune killing or exert direct antitumor activity independent of CD8+T. CD4+ T cells and CD8+ T cells can induce apoptosis of tumor cells through their interaction.24 Low lymphocyte counts are often associated with poorer clinical outcomes, possibly due to a reduced lymphocyte-mediated immune response to the tumor. Meanwhile, previous studies have evaluated the immunogenic changes of thermal ablation in a variety of malignancies, especially liver cancer and breast cancer.25,26 Some studies27 have reported that cold ablation of NSCLC has a strong anti-cancer immune response and distancing effect. We believe that the pre-ablation lymphocyte count of NSCLC may have an impact on the anti-cancer immune response triggered by ablation, and the specific mechanism needs to be further explored.
In addition, previous studies have reported the prognostic role of histological subtypes in lung adenocarcinoma.22 In this study, we found that patients with adenocarcinoma had a lower risk of local recurrence after ablation than those with squamous cell carcinoma, which was consistent with the results of previous relevant studies.
A nomogram is a simple visual statistical model that has been widely used in cancer prognosis.28 Based on the independent prognostic variables identified in Cox regression analyses, we developed and validated a combination nomogram to assess the risk of local recurrence after MWA of NSCLC. The model had the best identification ability in predicting 1-year LRFS, with an AUC of 0.688, while the AUC values of the second and third year decreased. The following reason may explain this trend: 1) most of NSCLC patients received follow-up examination in our hospital within 1 year after surgery, but a few of patients underwent the follow-up examination in local hospitals; 2) NSCLC patients received different adjuvant treatments after MWA. In the study, the calibration plot showed good prediction accuracy and can predict good agreement. We believe that nomogram can provide personalized prediction of local recurrence after MWA of NSCLC and be helpful for patients and clinicians in the treatment decision-making process.
The study has some limitations. First of all, the study was a retrospective analysis, which may introduce some bias. Secondly, the number of patients included in this study was small; a large prospective study is needed to confirm our results. In recent years, it has been reported that artificial intelligence has been used to predict the recurrence of other tumors after ablation, and satisfactory results have been obtained. In the next study, we are working on combining artificial intelligence to predict local recurrence after MWA for NSCLC.
In conclusion, preoperative lymphocyte count reduction is associated with poor prognosis of NSCLC. The nomogram model combined with preALC can provide a good individualized prediction of local recurrence after MWA.
Funding
The Natural Science Foundation of Shandong [Grant Number NO. ZR2020MH289] and the Academic promotion program of Shandong First Medical University [Grant Number 2019QL023].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bray F, Ferlay J, Soerjomataram I, et al. Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer. Chest. 2013;143(5):e278S–e313S. doi:10.1378/chest.12-2359
3. Ricardi U, Badellino S, Filippi AR. Stereotactic body radiotherapy for early stage lung cancer: history and updated role. Lung Cancer. 2015;90(3):388–396. doi:10.1016/j.lungcan.2015.10.016
4. Crocetti L, Bozzi E, Faviana P, et al. Thermal ablation of lung tissue: in vivo experimental comparison of microwave and radiofrequency. Cardiovasc Intervent Radiol. 2010;33(4):818–827. doi:10.1007/s00270-010-9869-z
5. Vogl TJ, Naguib NN, Lehnert T, et al. Radiofrequency, microwave and laser ablation of pulmonary neoplasms: clinical studies and technical considerations – review article. Eur J Radiol. 2011;77(2):346–357. doi:10.1016/j.ejrad.2009.07.034
6. Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria – a 10-year update. J Vasc Interv Radiol. 2014;25(11):1691–705e4. doi:10.1016/j.jvir.2014.08.027
7. Lang C, Egger F, Alireza Hoda M, et al. Lymphocyte-to-monocyte ratio is an independent prognostic factor in surgically treated small cell lung cancer: an international multicenter analysis. Lung Cancer. 2022;169:40–46. doi:10.1016/j.lungcan.2022.05.010
8. Li Q, Kong F, Ma J, et al. Nomograms based on fibrinogen, albumin, neutrophil-lymphocyte ratio, and carbohydrate antigen 125 for predicting endometrial cancer prognosis. Cancers (Basel). 2022;14(22):5632. doi:10.3390/cancers14225632
9. Kim J, Kwon J, Kim M, et al. Low-dielectric-constant polyimide aerogel composite films with low water uptake. Polymer J. 2016;48(7):829–834. doi:10.1038/pj.2016.37
10. Clark EJ, Connor S, Taylor MA, et al. Preoperative lymphocyte count as a prognostic factor in resected pancreatic ductal adenocarcinoma. HPB (Oxford). 2007;9(6):456–460. doi:10.1080/13651820701774891
11. Mehrazin R, Uzzo RG, Kutikov A, et al. Lymphopenia is an independent predictor of inferior outcome in papillary renal cell carcinoma. Urol Oncol. 2015;33(9):388e19–25. doi:10.1016/j.urolonc.2014.06.004
12. Oh SY, Heo J, Noh OK, et al. Absolute lymphocyte count in preoperative chemoradiotherapy for rectal cancer: changes over time and prognostic significance. Technol Cancer Res Treat. 2018;17:1533033818780065. doi:10.1177/1533033818780065
13. Punjabi A, Barrett E, Cheng A, et al. Neutrophil-lymphocyte ratio and absolute lymphocyte count as prognostic markers in patients treated with curative-intent radiotherapy for non-small cell lung cancer. Clin Oncol. 2021;33(8):e331–e338. doi:10.1016/j.clon.2021.03.019
14. Song X, Chen D, Yuan M, et al. Total lymphocyte count, neutrophil–lymphocyte ratio, and platelet–lymphocyte ratio as prognostic factors in advanced non–small cell lung cancer with chemoradiotherapy. Cancer Manag Res. 2018;10:6677–6683. doi:10.2147/CMAR.S188578
15. Zhang J, Huang SH, Li H, et al. Preoperative lymphocyte count is a favorable prognostic factor of disease-free survival in non-small-cell lung cancer. Med Oncol. 2013;30(1):352. doi:10.1007/s12032-012-0352-3
16. Senders ZJ, Martin RCG. Intratumoral immunotherapy and tumor ablation: a local approach with broad potential. Cancers (Basel). 2022;14(7):1754. doi:10.3390/cancers14071754
17. Lim W, Ridge CA, Nicholson AG, et al. The 8(th) lung cancer TNM classification and clinical staging system: review of the changes and clinical implications. Quant Imaging Med Surg. 2018;8(7):709–718. doi:10.21037/qims.2018.08.02
18. Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–247. doi:10.1016/j.ejca.2008.10.026
19. Singh R, Mishra MK, Aggarwal H. Inflammation, immunity, and cancer. Mediators Inflamm. 2017;2017:1. doi:10.1155/2017/6027305
20. Rabold K, Gielen PR, Kers-Rebel ED, et al. T-cell lymphopenia in patients with advanced thyroid carcinoma is associated with poor prognosis. Oncologist. 2019;24(3):e106–e110. doi:10.1634/theoncologist.2018-0422
21. Shibutani M, Maeda K, Nagahara H, et al. Lymphopenia associated with adjuvant chemotherapy after potentially curative surgery for colorectal cancer correlates with recurrence. Int Surg. 2016;105(1–3):146–151. doi:10.9738/intsurg-d-14-00236.1
22. Nance M, Khazi Z, Kaifi J, et al. Computerized tomography-guided microwave ablation of patients with stage I non-small cell lung cancers: a single-institution retrospective study. J Clin Imaging Sci. 2021;11:7. doi:10.25259/JCIS_224_2020
23. Jiang S, Dong C. A complex issue on CD4(+) T-cell subsets. Immunol Rev. 2013;252(1):5–11. doi:10.1111/imr.12041
24. Rosenberg SA. Progress in human tumour immunology and immunotherapy. Nature. 2001;411(6835):380–384. doi:10.1038/35077246
25. Leuchte K, Staib E, Thelen M, et al. Microwave ablation enhances tumor-specific immune response in patients with hepatocellular carcinoma. Cancer Immunol Immunother. 2021;70(4):893–907. doi:10.1007/s00262-020-02734-1
26. Zhou W, Yu M, Mao X, et al. Landscape of the peripheral immune response induced by local microwave ablation in patients with breast cancer. Adv Sci (Weinh). 2022;9(17):e2200033. doi:10.1002/advs.202200033
27. Katzman D, Wu S, Sterman DH. Immunological aspects of cryoablation of non-small cell lung cancer: a comprehensive review. J Thorac Oncol. 2018;13(5):624–635. doi:10.1016/j.jtho.2018.01.017
28. Iasonos A, Schrag D, Raj GV, et al. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–1370. doi:10.1200/JCO.2007.12.9791
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
