Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
Nomogram Based on Platelet–Albumin–Bilirubin for Predicting Tumor Recurrence After Surgery in Alpha-Fetoprotein-Negative Hepatocellular Carcinoma Patients
Authors Yang C, Wu X, Liu J, Wang H, Jiang Y, Wei Z, Cai Q
Received 6 November 2022
Accepted for publication 8 January 2023
Published 13 January 2023 Volume 2023:10 Pages 43—55
DOI https://doi.org/10.2147/JHC.S396433
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Imam Waked
Chengkai Yang,1 Xiaoya Wu,2 Jianyong Liu,3 Huaxiang Wang,1 Yi Jiang,3 Zhihong Wei,3 Qiucheng Cai3
1The Fuzong Clinical Medical College of Fujian Medical University, Fuzhou, 350025, People’s Republic of China; 2Eastern Hospital Affiliated to Xiamen University, Fuzhou, 350025, People’s Republic of China; 3Department of Hepatobiliary Surgery, 900 Hospital of The Joint Logistics Team, Fuzhou, 350025, People’s Republic of China
Correspondence: Qiucheng Cai; Zhihong Wei, Department of Hepatobiliary Surgery, 900 Hospital of The Joint Logistics Team, No. 156 The Second West Ring Road, Fuzhou, Fujian, 350025, People’s Republic of China, Tel +86 13514072408 ; +86 18059055977, Email [email protected]; [email protected]
Purpose: In this study, we developed a nomogram based on the platelet–albumin–bilirubin (PALBI) score to predict recurrence-free survival (RFS) after curative resection in alpha-fetoprotein (AFP)-negative (≤ 20 ng/mL) hepatocellular carcinoma (HCC) patients.
Patients and Methods: A total of 194 pathologically confirmed AFP-negative HCC patients were retrospectively analyzed. Univariate and multivariate Cox regression analyses were performed to screen the independent risk factors associated with RFS, and a nomogram prediction model for RFS was established according to the independent risk factors. The receiver operating characteristic (ROC) curve and the C-index were used to evaluate the accuracy and the efficacy of the model prediction. The correction curve was used to assess the calibration of the prediction model, and decision curve analysis was performed to evaluate the clinical application value of the prediction model.
Results: PALBI score, MVI, and tumor size were independent risk factors for postoperative tumor recurrence (P < 0.05). A nomogram prediction model based on the independent predictive factors was developed to predict RFS, and it achieved a good C-index of 0.704 with an area under the ROC curve of 0.661 and the sensitivity was 73.2%. Patients with AFP-negative HCC could be divided into the high-risk group or the low-risk group by the risk score calculated by the nomogram, and there was a significant difference in RFS between the two groups (P < 0.05). Decision curve analysis (DCA) showed that the nomogram increased the net benefit in predicting the recurrence of AFP-negative HCC and exhibited a wider range of threshold probabilities than the independent risk factors (PALBI score, MVI, and tumor size) by risk stratification.
Conclusion: The nomogram based on the PALBI score can predict RFS after curative resection in AFP-negative HCC patients and can help clinicians to screen out high-risk patients for early intervention.
Keywords: hepatocellular carcinoma, platelet–albumin–bilirubin score, alpha-fetoprotein-negative, recurrence-free survival, nomogram
Introduction
Hepatocellular carcinoma (HCC) is the most common type of liver malignancy worldwide, and it ranks sixth in incidence and fourth in mortality among all types of cancer, thus seriously threatening human health and life.1 Resection is the recommended treatment for HCC, and with advancements in perioperative management, surgical techniques, and postoperative monitoring, the survival rate of HCC has increased. The tumor recurrence rate at 5 years after surgery is 70%, and the long-term prognosis is not satisfactory.2
Alpha-fetoprotein (AFP) is a serum biomarker used to diagnose and postoperatively monitor HCC, with a specificity of 76–96%;3,4 however, its sensitivity is low, with 60–70% of HCC patients having elevated AFP levels and 33–65% of AFP-positive HCC patients having tumors smaller than 3 cm,;5–7 thus, greatly limiting the diagnosis and treatment of AFP-negative HCC patients. In addition, a study has reported that measuring serum AFP levels after resection cannot predict tumor recurrence in AFP-negative HCC patients.8 Therefore, it is important to identify the prognostic indicators of AFP-negative HCC patients after resection.
Previous studies have shown that multiple biomarkers play an important prognostic and predictive value in HCC,9–13 and abnormal liver function has been proved to be an independent factor for predicting recurrence in HCC patients.14,15 In 2015, Johnson et al introduced the albumin–bilirubin (ALBI) score, which is based on two objective laboratory parameters, namely, serum albumin concentration and total bilirubin concentration, to provide a simple and objective method for assessing liver function and prognosis in HCC patients.16,17 In addition, most HCC patients present with cirrhosis as the underlying disease, with portal venous pressure as an indicator of cirrhosis severity. On the basis of the ALBI score, several investigators have proposed using platelet counts to define the severity of portal hypertension and to generate a novel liver function reserve model, that is, the platelet–albumin–bilirubin (PALBI) score.18,19 The PALBI score can predict hepatic complications and overall survival after hepatectomy in HCC patients.20,21 However, no relevant study has reported whether the PALBI score can assess liver function and prognosis in AFP-negative HCC patients. In recent years, prognostic models for diseases based on laboratory data have been established with advantages of objectivity, non-invasive analysis, and convenience.22,23 Therefore, we developed a nomogram prediction model based on the PALBI score to predict the probability of recurrence-free survival (RFS) after curative resection in AFP-negative HCC patients.
Patients and Methods
Patients
A total of 194 AFP-negative HCC patients who underwent curative resection at the 900th Hospital of Chinese People’s Liberation Army Joint Support Force from January 2010 to December 2018 were included. The inclusion criteria were as follows: (1) patients with primary HCC confirmed by two or more imaging modalities (ultrasound, computed tomography, or magnetic resonance imaging) or postoperative histopathologic examination; (2) those treated by resection with the intent to cure, which was defined as negative margins with no residual tumor based on histopathologic examination; and (3) those preoperatively AFP negative (≤20 ng/mL). The exclusion criteria were as follows: (1) patients with other malignant tumors; (2) those treated by transarterial chemoembolization, radiofrequency ablation, or other anti-tumor therapy; (3) those that were lost to death; and (4) those that were lost to follow-up. The study was approved by the Ethics Committee of the 900th Hospital of PLA Joint Support Force. All procedures were in compliance with the relevant guidelines and regulations. All patients signed written informed consent forms, and this study was conducted in accordance with the Declaration of Helsinki.
Data Acquisition
All data were collected from each participant’s electronic medical records and included gender, age, white blood cell count, coagulation time, and platelet count, as well as the levels of hemoglobin, sodium, AFP, albumin, total bilirubin, aspartate aminotransferase, alkaline phosphatase, and alanine aminotransferase. Surgical information and tumor characteristics were also collected. The PALBI score was computed as follows: 2.02 × log10 bilirubin – 0.37 × (log10 bilirubin)2–0.04 × albumin – 3.48 × log10 platelets + 1.01 × (log10 platelets).2
Follow-Up
Postoperatively, patients received standardized treatment and follow-up according to the primary liver cancer diagnosis, and the treatment plan was adjusted in some cases.24 Patients were re-examined every 2 months for the first year after surgery and every 3 months thereafter. At each re-examination, a detailed history was taken, a physical examination was performed, the AFP level and liver function were assessed, and an abdominal ultrasound was performed. Abdominal computed tomography with contrast and/or magnetic resonance imaging were performed every 6 months, and relevant examinations were performed to identify the patients with suspected intrahepatic and extrahepatic recurrence and metastasis. The primary end point was tumor recurrence. Recurrence-free survival was measured from the date of surgery to the date of recurrence or death or the most recent follow-up.
Statistical Analysis
Measurement data were presented as median or mean ± standard deviation. The Mann–Whitney U-test was used to compare continuous variables. The Chi-square or Fisher exact test was used to compare categorical variables. The Kaplan–Meier method was used to prepare survival curves. Variables with P < 0.05 were included in multivariate and univariate Cox regression analyses, and predictive factors affecting survival were analyzed using Cox regression models. A nomogram prediction model based on independent risk factors from multivariate analysis. The area under the receiver operating characteristic (ROC) curve and the C-index were used to evaluate the accuracy of the model in predicting survival, and the larger the C-index, the higher the accuracy of the model. Each patient was assigned a total risk score (NomoScore: nomogram risk score) for risk stratification of RFS according to the nomogram prediction model. Patients were classified into different risk groups, namely, low or high risk groups to identify statistically significant differences in disease-free survival between the groups. Decision curve analysis (DCA) was conducted to determine the clinical benefit of the nomogram by quantifying the net benefit along with the increase in threshold probabilities. P < 0.05 was considered statistically significant.
Univariate and multivariate Cox regression analyses were performed using SPSS 25.0 software (IBM Corporation, Armonk, NY, USA). The nomogram, ROC curves, and survival figures, as well as DCA, were prepared or performed using R version 3.6.2 (http://www.r-project.org/) with “rms”, “glamet”, “ggDCA”, “rmda” “survival”, “survminer”, and “ggpubr” packages. The KM curves were plotted using Prism 8.0 software (GraphPad, San Diego, CA, USA). P < 0.05 was considered statistically significant.
Results
Patient ‘S Clinical Information
A total of 722 patients underwent curative resection during the study period, and 331 patients who met the inclusion criteria were included in this study. In addition, 137 patients were excluded because of preoperative anticancer therapy (n = 42), history of other malignancies (n = 35), incomplete clinical or follow-up data (n = 55), and perioperative death (n = 5). A flowchart of the patient selection process is shown in Figure 1.
 |
Figure 1 Flow chart of the study design. |
A total of 194 patients diagnosed with AFP-negative HCC were finally included, with a median overall survival (mOS) time of 75.2 months and a median follow-up time of 137 months (range, 1–275 months). After comparing the clinical data of AFP-negative patients without recurrence (n = 92) and AFP-negative patients with recurrence (n = 102), correlation analysis showed that there were significant differences in tumor size (p = 0.022), MVI (p = 0.000), and Barcelona Clinic of Liver Cancer (BCLC) stage (p = 0.000) between the groups. All baseline characteristics of the patients are shown in Table 1.
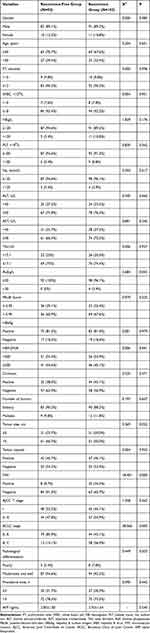 |
Table 1 Baseline and Clinicopathological Characteristics of Alpha-Fetoprotein-Negative Hepatocellular Carcinoma Patients |
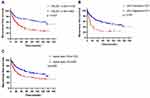
PALBI Score Was an Independent Predictive Factors
In univariate analysis, PALBI score, tumor size, MVI, tumor-node-metastasis (TNM) stage, BCLC stage, and operation time were risk factors for postoperative tumor recurrence (P < 0.05). In multivariate analysis, PALBI score, MVI, and tumor size were independent risk factors for postoperative tumor recurrence (P < 0.05, Table 2). Kaplan–Meier curves suggested that three independent predictive factors could stratify the entire cohort of patients for RFS (P < 0.01 for all, Figure 2).
 |
Table 2 Univariate and Multivariate Cox Analyses for Recurrence-Free Survival of Alpha-Fetoprotein-Negative Hepatocellular Carcinoma Patients |
The Nomogram Showed Good Predictive Value
The nomogram prediction model was developed based on the independent risk factors from multivariate analysis (Figure 3A). The nomogram achieved a good concordance index of 0.704 (95% CI: 0.624–0.784) with 1000 bootstrap samples to measure the discrimination in predicting 1-, 3-, and 5-year RFS rates. The area under the ROC curve was 0.661 (Figure 3B). The calibration curves for 1-, 3- and 5-year RFS rates were largely overlapped with the standard lines (Figure 3C–E). The final nomogram could accurately distinguish the RFS of AFP-negative HCC patients and had better consistency between the predicted probability and the observed probability of RFS.
The Nomogram Has Satisfactory Clinical Utility
According to the total risk score calculated from the nomogram prediction model, AFP-negative HCC patients were divided into the high-risk group or the low-risk group. Survival curves were calculated using the Kaplan–Meier method to compare RFS rates between the two groups, and the results showed a significant discriminatory power for risk of relapse in patients based on the nomogram risk score (P < 0.05, Figure 4A). In predicting 1-, 3-, and 5-year tumor recurrence in AFP-negative HCC, DCA showed that the nomogram prediction model increased the net benefit and showed a wider range of threshold probabilities than PALBI score, MVI, and tumor size by risk stratification (Figure 4B–D).
Discussion
Hepatocellular carcinoma is a malignant tumor characterized by insidious onset, invasiveness, recurrence/metastasis, and poor prognosis, which seriously threatens human health and life. With advancements in medical care, HCC can be treated by surgery, transcatheter arterial chemoembolization, radiofrequency ablation, radiotherapy, chemotherapy, immunotherapy, and targeted therapy. However, radical surgical resection and liver transplantation are the preferred methods of treatment because they offer the best chances of survival, although liver transplantation is not always possible due to the lack of liver donors, the cost of the procedure, and the trauma caused to patients.25 Recurrence after HCC resection affects the long-term survival of patients after surgery, and the recurrence rate 5 years after surgery is high at 70%.2 Therefore, improving the efficacy of radical resection will require predicting the population at high risk of postoperative tumor recurrence, taking effective preventive measures, and selecting better treatment plans after recurrence.
Alpha-fetoprotein is mainly secreted by the liver, as well as the gastrointestinal tract and the yolk sac, and it is a serological marker of liver cancer, with higher preoperative AFP levels associated with a poor prognosis in HCC patients.26 However, the regulation of AFP expression stops before post-transcriptional translation, and 30–40% of HCC patients have serum AFP levels ≤20 ng/mL.27,28 The acronym refers to bilirubin, albumin, AFP-L3, AFP and DCP (BALAD) score and the Japan Integrated Staging (JIS) Score are two prognostic models for HCC that apply AFP levels, and the two models can predict the survival rate of HCC patients after resection,29,30 but the value of these two scores for AFP-negative HCC patients is not clear. Several studies have demonstrated that AFP-negative HCC patients have a better prognosis than AFP-positive HCC patients,8,31 so it is important to develop tools that can predict the prognosis of AFP-negative HCC patients.
Currently, there is no agreement on which tool is best for the postoperative prognostic evaluation of HCC. Commonly used staging systems include those proposed by the BCLC and the American Joint Committee on Cancer, which risk stratify HCC patients.32,33 However, these two staging systems only include tumor factors such as tumor number, size, and MVI, and they cannot provide individualized assessments of HCC patients. The postoperative recurrence of HCC is influenced by various factors, including the general condition of patients, the presence of systemic inflammation and surgery-related factors, and the invasive characteristics of tumors, among which inflammatory factors can promote angiogenesis, DNA damage, invasion, and metastasis through the production of cytokines, which play an important role in tumor occurrence, progression, and metastasis.34 Inflammatory indicators, such as the numbers of neutrophils, monocytes, platelets, and lymphocytes, as well as the levels of serum albumin and total bilirubin, are commonly used in clinical settings, and they have been valuable in assessing the inflammatory response and the prognosis of cancer patients.35,36 Furthermore, several studies have demonstrated that prediction models based on the scores of the abovementioned serological markers have high prognostic accuracy in the postoperative prognosis of AFP-negative HCC patients.31,37
Platelets play an important role in inflammation and tumor biology. Platelets are activated when tumor cells invade the circulatory system, and activated platelets can trigger the epithelial–mesenchymal program in cells, protect tumor cells from blood flow shear injury, help tumor cells evade killing by cells of the immune system, and promote tumor recurrence and metastasis.38–40 Serum albumin can reflect the function of the liver and the presence of systemic inflammation. A previous study has shown that serum albumin can regulate the kinetics of tumor progression by regulating the levels of AFP level and kinases, and low albumin levels are closely related to high invasiveness and tumor recurrence.41 Serum bilirubin, on the other hand, is inversely correlated with the risk of inflammatory diseases and autoimmune diseases, and it exerts anti-inflammatory effects by reducing oxidative stress, decreasing inflammatory factor expression, and inhibiting macrophage and neutrophil counts, thereby reducing tumor cell proliferation and invasion.42,43
The PALBI score is calculated based on three inflammatory markers, namely, the serum albumin level, the total bilirubin level, and the platelet count, and it shows advantages in some aspects of liver function, but not in others, which may reflect the relationship between inflammation and tumor development and predict the outcome after hepatectomy in AFP-negative HCC patients. Lee et al showed that the predictive value of the PALBI score for overall survival in HCC patients was better than the Child–Turcotte–Pugh score and the model for end-stage liver disease (MELD) score.44 Therefore, we developed and validated a nomogram based on the PALBI score to predict the prognosis of AFP-negative HCC patients undergoing curative resection. The area under the ROC curve of the nomogram was 0.661 and the C-index was 0.704, which is similar to HCC prognostic nomograms constructed at other sites,45 indicating that the model had good efficacy and high accuracy in prediction. The calibration curve also showed good correlation between the predicted results and the actual results. The model divided patients into two different risk groups, namely, low risk and high risk, and there was a statistically significant difference in RFS between the two groups. Furthermore, DCA revealed that the model could increase the net benefit in predicting recurrence in AFP-negative HCC patients and showed a wider threshold probability range than PALBI score, MVI, and tumor diameter by risk stratification. Li et al showed that radical resection had a higher long-term survival rate than TACE for BCLC stage B and C hepatocellular carcinoma patients with normal liver function, large solitary tumors, multinodular tumors, macrovascular invasion, or portal hypertension.46 Therefore, our center fully combines the patient ‘s own will and efficacy evaluation, and selects the optimal individualized treatment plan for the patient. In this study, the data set was not randomly divided into training and validation groups. On the contrary, our nomogram was based on a representative sample size and internally validated based on the model, avoiding data waste and inefficiency.47 Therefore, this prediction model has important clinical value in guiding postoperative monitoring, follow-up, and postoperative adjuvant therapy.
In this study, MVI and tumor size were independent risk factors for postoperative tumor recurrence in AFP-negative HCC patients. Multivascular invasion is defined as a cancer cell nest in the lumen of endothelial cell-lined blood vessels, and it can only be observed microscopically, which closely resembles the invasive behavior of HCC. Tumor cells in MVI-positive patients may spread and metastasize to the liver, eventually forming portal vein tumor thrombi, which associate with a higher postoperative recurrence rate and a lower survival rate.48–50 Tumor size is closely related to genetic changes in HCC, and the larger the tumor, the more invasive the behavior of tumor cells, and the higher the risk of postoperative recurrence and metastasis.51
This study has several limitations. First, this was a single-center study, and the sample size was insufficient, which may bias the study results. Second, retrospective studies have selection bias in data collection and postoperative follow-up. Third, there are many factors that affect the treatment effect of patients, which are not included in detail in this study, and we will further improve this work in future studies. Therefore, our results require external validation in different geographical regions. Although the sample size of this study is limited, our results are significant as they are intended to guide clinical practice.
Conclusion
In conclusion, we developed and validated a nomogram based on the PALBI score to predict RFS after curative resection in AFP-negative HCC patients. This predictive model can be used to monitor patients and to design follow-up programs for high-risk patients.
Abbreviations
PALBI, platelet–albumin–bilirubin; RFS, recurrence-free survival; AFP, alpha-fetoprotein; HCC, hepatocellular carcinoma; ROC, receiver operating characteristic; MVI, microvascular invasion; TNM, tumor-node-metastasis BCLC; Barcelona Clinic of Liver Cancer PT, prothrombin time; WBC, white blood cell; HB, hemoglobin; PLT, platelet count, Na, sodium ion; ALT, alanine aminotransferase; AST, aspartate transaminase; TBIL, total bilirubin; ALP, alkaline phosphatase; HBsAg, hepatitis B surface antigen; HBV, hepatitis B virus; AJCC, American Joint Committee on Cancer; BALAD, bilirubin, albumin, AFP-L3, AFP and DCP; JIS, Japan Integrated Staging; MELD, model for end-stage liver disease.
Acknowledgments
We thank the patients who participated in this study and the staff at the Department of Hepatobiliary Surgery of the 900th Hospital of the Chinese People’s Liberation Army Joint Support Force for their support and cooperation.
Funding
Our research was supported by the grants from Fujian Natural Science Foundation (2020Y0078), General project of the 900th Hospital Research Project of the Joint Logistic Support Force (2021MS21).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Hepatocellular carcinoma. % J Nature reviews. Dis Primers. 2021;7(1):7. doi:10.1038/s41572-021-00245-6
3. Yang SL, Liu LP, Yang S, et al. Preoperative serum α-fetoprotein and prognosis after hepatectomy for hepatocellular carcinoma. Br J Surg. 2016;103(6):716–724. doi:10.1002/bjs.10093
4. Okuda K, Kubo Y, Obata H. Serum alpha-fetoprotein in the relatively early stages of hepatocellular carcinoma and its relationship to gross anatomical types. Ann N Y Acad Sci. 1975;259:248–252.
5. She S, Xiang Y, Yang M, et al. C-reactive protein is a biomarker of AFP-negative HBV-related hepatocellular carcinoma. Int J Oncol. 2015;47(2):543–554.
6. Taketa K. Alpha-fetoprotein: reevaluation in hepatology. Hepatology. 1990;12(6):1420–1432.
7. Agopian VG, Harlander-Locke MP, Markovic D, et al. Evaluation of patients with hepatocellular carcinomas that do not produce α-fetoprotein. JAMA Surg. 2017;152(1):55–64.
8. Zhang XF, Qi X, Meng B, et al. Prognosis evaluation in alpha-fetoprotein negative hepatocellular carcinoma after hepatectomy: comparison of five staging systems. Eur J Surg Oncol. 2010;36(8):718–724.
9. Kurokawa T, Ohkohchi N. Platelets in liver disease, cancer and regeneration. World J Gastroenterol. 2017;23(18):3228–3239.
10. Wang ZX, Jiang CP, Cao Y, Zhang G, Chen WB, Ding YT. Preoperative serum liver enzyme markers for predicting early recurrence after curative resection of hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2015;14(2):178–185. doi:10.1016/S1499-3872(15)60353-8
11. Nagel T, Klaus F, Ibanez IG, Wege H, Lohse A, Meyer B. Fast and facile analysis of glycosylation and phosphorylation of fibrinogen from human plasma-correlation with liver cancer and liver cirrhosis. Anal Bioanal Chem. 2018;410(30):7965–7977. doi:10.1007/s00216-018-1418-7
12. Oldenhuis CN, Oosting SF, Gietema JA, de Vries EG. Prognostic versus predictive value of biomarkers in oncology. Eur J Cancer. 2008;44(7):946–953. doi:10.1016/j.ejca.2008.03.006
13. Moldogazieva NT, Zavadskiy SP, Sologova SS, Mokhosoev IM, Terentiev AA. Predictive biomarkers for systemic therapy of hepatocellular carcinoma. Expert Rev Mol Diagn. 2021;21(11):1147–1164. doi:10.1080/14737159.2021.1987217
14. Ang SF, Ng ES, Li H, et al. The Singapore Liver Cancer Recurrence (SLICER) Score for relapse prediction in patients with surgically resected hepatocellular carcinoma. PLoS One. 2015;10(4):e0118658. doi:10.1371/journal.pone.0118658
15. Chan AWH, Zhong J, Berhane S, et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol. 2018;69(6):1284–1293. doi:10.1016/j.jhep.2018.08.027
16. Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-The ALBI grade. J clin Oncol. 2015;33(6):550–558. doi:10.1200/JCO.2014.57.9151
17. Pinato DJ, Sharma R, Allara E, et al. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J Hepatol. 2017;66(2):338–346. doi:10.1016/j.jhep.2016.09.008
18. Elshaarawy O, Alkhatib A, Elhelbawy M, et al. Validation of modified albumin-bilirubin-TNM score as a prognostic model to evaluate patients with hepatocellular carcinoma. World J Hepatol. 2019;11(6):542–552. doi:10.4254/wjh.v11.i6.542
19. Hansmann J, Evers MJ, Bui JT, et al. Albumin-bilirubin and platelet-albumin-bilirubin grades accurately predict overall survival in high-risk patients undergoing conventional transarterial chemoembolization for hepatocellular carcinoma. J Vasc Interv Radiol. 2017;28(9):1224–1231.e1222. doi:10.1016/j.jvir.2017.05.020
20. Liu PH, Hsu CY, Hsia CY, et al. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD Era. J Gastroenterol Hepatol. 2017;32(4):879–886. doi:10.1111/jgh.13608
21. Wu B, Hu X, Jin H, et al. Albumin-bilirubin and platelet-albumin-bilirubin grades for hepatitis B-associated hepatocellular carcinoma in Child-Pugh A patients treated with radical surgery: a retrospective observational study. Medicine. 2019;98(43):e17394. doi:10.1097/MD.0000000000017394
22. Zhang LX, Lv Y, Xu AM, Wang HZ. The prognostic significance of serum gamma-glutamyltransferase levels and AST/ALT in primary hepatic carcinoma. BMC Cancer. 2019;19(1):841. doi:10.1186/s12885-019-6011-8
23. Sylman JL, Mitrugno A, Atallah M, et al. The predictive value of inflammation-related peripheral blood measurements in cancer staging and prognosis. Front Oncol. 2018;8:78. doi:10.3389/fonc.2018.00078
24. Department of Medical Administration, National Health and Health Commission of the People’s Republic of China. 中国原发性肝癌诊疗指南(2019版) [Guidelines for diagnosis and treatment of primary liver cancer in China (2019 edition)]. Zhonghua Gan Zang Bing Za Zhi. 2020;28(2):112–128. Chinese. doi:10.3760/cma.j.issn.1007-3418.2020.02.004
25. Dhir M, Melin AA, Douaiher J, et al. A review and update of treatment options and controversies in the management of hepatocellular carcinoma. Ann Surg. 2016;263(6):1112–1125. doi:10.1097/SLA.0000000000001556
26. Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter. 2017;22(Suppl 1):e12403. doi:10.1111/hel.12403
27. Li J, Cheng ZJ, Liu Y, et al. Serum thioredoxin is a diagnostic marker for hepatocellular carcinoma. Oncotarget. 2015;6(11):9551–9563. doi:10.18632/oncotarget.3314
28. Toyoda H, Kumada T, Tada T, et al. Clinical utility of highly sensitive Lens culinaris agglutinin-reactive alpha-fetoprotein in hepatocellular carcinoma patients with alpha-fetoprotein <20 ng/mL. Cancer Sci. 2011;102(5):1025–1031. doi:10.1111/j.1349-7006.2011.01875.x
29. Toyoda H, Kumada T, Osaki Y, et al. Staging hepatocellular carcinoma by a novel scoring system (BALAD score) based on serum markers. Clin Gastroenterol Hepatol. 2006;4(12):1528–1536. doi:10.1016/j.cgh.2006.09.021
30. Kitai S, Kudo M, Minami Y, et al. Validation of a new prognostic staging system for hepatocellular carcinoma: a comparison of the biomarker-combined Japan integrated staging score, the conventional Japan integrated staging score and the BALAD score. Oncology. 2008;75(Suppl 1):83–90. doi:10.1159/000173428
31. Li S, Xu W, Liao M, et al. The significance of gamma-glutamyl transpeptidase to lymphocyte count ratio in the early postoperative recurrence monitoring and prognosis prediction of AFP-negative hepatocellular carcinoma. J Hepatocell Carcinoma. 2021;8:23–33. doi:10.2147/JHC.S286213
32. Chun YS, Pawlik TM, Vauthey JN. AJCC cancer staging manual: pancreas and hepatobiliary cancers. Ann Surg Oncol. 2018;25(4):845–847. doi:10.1245/s10434-017-6025-x
33. Galle PR, Forner A, Llovet JM, Mazzaferro V, Piscaglia F, Raoul JL. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi:10.1016/j.jhep.2018.03.019
34. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503. doi:10.1016/S1470-2045(14)70263-3
35. Chechlinska M, Kowalewska M, Nowak R. Systemic inflammation as a confounding factor in cancer biomarker discovery and validation. Nat Rev Cancer. 2010;10(1):2–3. doi:10.1038/nrc2782
36. Liao R, Peng C, Li M, et al. Comparison and validation of the prognostic value of preoperative systemic immune cells in hepatocellular carcinoma after curative hepatectomy. Cancer Med. 2018;7(4):1170–1182. doi:10.1002/cam4.1424
37. Mao S, Yu X, Shan Y, Fan R, Wu S, Lu C. Albumin-Bilirubin (ALBI) and monocyte to lymphocyte ratio (MLR)-based nomogram model to predict tumor recurrence of AFP-negative hepatocellular carcinoma. J Hepatocell Carcinoma. 2021;8:1355–1365. doi:10.2147/JHC.S339707
38. Haemmerle M, Stone RL, Menter DG, Afshar-Kharghan V, Sood AK. The platelet lifeline to cancer: challenges and opportunities. Cancer Cell. 2018;33(6):965–983.
39. Asghar S, Parvaiz F, Manzoor S. Multifaceted role of cancer educated platelets in survival of cancer cells. Thromb Res. 2019;177:42–50.
40. Labelle M, Begum S, Hynes RO. Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell. 2011;20(5):576–590.
41. Bağırsakçı E, Şahin E, Atabey N, Erdal E, Guerra V, Carr BI. Role of albumin in growth inhibition in hepatocellular carcinoma. Oncology. 2017;93(2):136–142.
42. Fujiwara R, Haag M, Schaeffeler E, Nies AT, Zanger UM, Schwab M. Systemic regulation of bilirubin homeostasis: potential benefits of hyperbilirubinemia. Hepatology. 2018;67(4):1609–1619.
43. Yao Q, Jiang X, Zhai YY, et al. Protective effects and mechanisms of bilirubin nanomedicine against acute pancreatitis. J Control Release. 2020;322:312–325.
44. Lee SK, Song MJ, Kim SH, Park M. Comparing various scoring system for predicting overall survival according to treatment modalities in hepatocellular carcinoma focused on Platelet-albumin-bilirubin (PALBI) and albumin-bilirubin (ALBI) grade: a nationwide cohort study. PLoS One. 2019;14(5):e0216173.
45. Kong J, Wang T, Shen S, Zhang Z, Yang X, Wang W. A genomic-clinical nomogram predicting recurrence-free survival for patients diagnosed with hepatocellular carcinoma. PeerJ. 2019;7:e7942.
46. Zhong JH, Ke Y, Gong WF, et al. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma. Ann Surg. 2014;260(2):329–340.
47. Moons KG, Kengne AP, Woodward M, et al. Risk prediction models: i. Development, internal validation, and assessing the incremental value of a new (bio)marker. Heart. 2012;98(9):683–690.
48. Kim JM, Joh JW, Yi NJ, et al. Predicting hepatocellular carcinoma recurrence beyond Milan criteria after liver resection for solitary hepatocellular carcinoma. J Gastrointest Surg. 2020;24(10):2219–2227.
49. Kim M, Kim T, Lee HY, Hong SY, Wang HJ, Kim BW. Risk factors for beyond Milan recurrence after hepatic resection for single hepatocellular carcinoma no larger than 5 centimeters. Liver Transpl. 2021;27(8):1116–1129.
50. Wang L, Jin YX, Ji YZ, Mu Y, Zhang SC, Pan SY. Development and validation of a prediction model for microvascular invasion in hepatocellular carcinoma. World J Gastroenterol. 2020;26(14):1647–1659.
51. Wu G, Wu J, Wang B, Zhu X, Shi X, Ding Y. Importance of tumor size at diagnosis as a prognostic factor for hepatocellular carcinoma survival: a population-based study. Cancer Manag Res. 2018;10:4401–4410.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.