Back to Journals » Journal of Inflammation Research » Volume 16
NLR48 is Better Than CRP, and mCTSI, and Similar to BISAP and SOFA Scores for Mortality Prediction in Acute Pancreatitis: A Comparison of 6 Scores
Authors Cazacu SM , Parscoveanu M, Cartu D, Moraru E, Rogoveanu I , Ungureanu BS , Iordache S, Florescu DN, Iovanescu VF, Dragomir MI
Received 18 August 2023
Accepted for publication 10 October 2023
Published 20 October 2023 Volume 2023:16 Pages 4793—4804
DOI https://doi.org/10.2147/JIR.S432408
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Sergiu Marian Cazacu,1,* Mircea Parscoveanu,2,* Dan Cartu,2,* Emil Moraru,2,* Ion Rogoveanu,1,* Bogdan Silviu Ungureanu,1,* Sevastita Iordache,1,* Dan Nicolae Florescu,1,* Vlad Florin Iovanescu,1,* Manuela Iuliana Dragomir3,*
1Gastroenterology Department, University of Medicine and Pharmacy Craiova, Clinical Emergency Hospital Craiova, Craiova, Romania; 2Surgery Department, University of Medicine and Pharmacy Craiova, Clinical Emergency Hospital Craiova, Craiova, Romania; 3Public Health Management Department, University of Medicine and Pharmacy Craiova, Craiova, Romania
*These authors contributed equally to this work
Correspondence: Sevastita Iordache, The University of Medicine and Pharmacy Craiova, Gastroenterology Department, 2-4, Petru Rares Street, Craiova, Dolj County, 200349, Romania, Tel +40722990012, Fax +40251426688, Email [email protected]
Introduction: The neutrophil–lymphocyte ratio (NLR) has been suggested as a reliable marker for predicting inflammation progression and severity of acute pancreatitis, although the role of the NLR stratified by etiology is still insufficiently studied. However, the NLR’s role in mortality prediction was poorly evaluated in the literature.
Patients and Methods: We performed a retrospective, cross-sectional study to analyze the role of NLR0 (at admission) and NLR48 (at 48 hours) in acute pancreatitis as compared with CRP, BISAP, SOFA, and modified CTSI (mCTSI) for the prediction of mortality and severe acute pancreatitis (SAP) in patients admitted into the Emergency Clinical County Hospital of Craiova during 48 months. The primary assessed outcomes were the rate of in-hospital mortality, the rate of persistent organ failure, and ICU admissions. We analyzed mortality prediction for all acute pancreatitis, for biliary, alcoholic, and hypertriglyceridemic acute pancreatitis, for severe forms, and for patients admitted to the ICU.
Results: A total of 725 patients were selected; 42.4% had biliary acute pancreatitis, 27.7% had alcoholic acute pancreatitis, and 8.7% had hypertriglyceridemia-induced acute pancreatitis. A total of 13.6% had POF during admission. The AUC for NLR48 in predicting mortality risk and SAP was 0.81 and 0.785, superior to NLR0, CRP48, and mCTSI but inferior to BISAP and SOFA scores. The NLR48/NLR0 ratio did not add significantly to the accuracy. NLR0 and NLR48 performed poorly for mortality prediction in severe forms and in patients admitted to the ICU. NLR48 has good accuracy in our study for predicting death risk in biliary and alcoholic acute pancreatitis but not in hypertriglyceridemic acute pancreatitis.
Conclusion: NLR48 was a good indicator in predicting mortality risk and severe forms in all patients with acute pancreatitis, but not of death in SAP and in patients admitted to ICU, with good accuracy for predicting death risk in biliary and alcoholic acute pancreatitis but not in hypertriglyceridemic acute pancreatitis.
Keywords: acute pancreatitis, severe acute pancreatitis, neutrophil–lymphocyte ratio, BISAP score, SOFA score, C-reactive protein
Introduction
Acute pancreatitis represents a disease with an estimated mortality rate of 1–5%;1–3 10–25% may develop severe complications which require ICU admission,2–4 and mortality rates of up to 30–40% have been noted in hospitalized patients with pancreatic necrosis and organ failure.1,3,4 Biliary gallstones, alcohol consumption, and hypertriglyceridemia (HTG) above 1000 mg/dL represent the three main risk factors for acute pancreatitis; a systematic review and meta-analysis of 127 studies showed that the risk for non-mild acute pancreatitis and for complications is higher in HTG acute pancreatitis (HTGAP) compared with alcoholic acute pancreatitis (AAP) and biliary acute pancreatitis (BAP); a higher mortality rate was noted in HTGAP versus AAP (OR=1.72) and BAP (OR=1.50).4
Several scoring systems are available today, such as the Ranson score, Glasgow score, APACHE II, BISAP, CTSI (Computed Tomography Severity Index), and modified CTSI (mCTSI)2,3 but many complex scores require several parameters not usually sampled at admission in all cases of acute pancreatitis (mostly in ICU admissions). The BISAP score requires only five parameters (BUN>25 mg/dL, impaired mental status, the presence of systemic inflammatory response syndrome or SIRS, age above 60 years, and pleural collection) and has high specificity but limited sensitivity;2,3 a meta-analysis comparing the BISAP score with the Ranson score and APACHE II showed a higher sensitivity but a lower specificity.3
Several biological markers have been proposed for the prediction of the severity and mortality of acute pancreatitis. C-reactive protein (CRP) represents one of the first predicting markers for disease severity, with proposed cut-offs of 150 or 190 mg/dL at 48 h or an interval change of 90 mg/dL at 48 h.5 These results suggest that CRP can be used to select mild cases of acute pancreatitis which can be discharged early and managed in an ambulatory setting. Other proposed markers6 were the white blood cell count, neutrophil number, erythrocyte sedimentation rate, and Hb level.
The neutrophil–lymphocyte ratio (NLR) has been suggested as a reliable marker for predicting inflammation progression and severity of pancreatitis in several studies.7–17 Acute pancreatic inflammation activates inflammatory cytokines and proteolytic enzymes;2 a high neutrophil number indicates an acute inflammatory response and a low lymphocyte number a deterioration in the general health condition combined with physiological stress.10 The NLR can have physiological variations in healthy persons (0.78 to 3.53) and the baseline NLR can therefore influence increased values in acute pancreatitis.18 Most studies were focused on NLR0 (at admission) and some studies evaluated also NLR48 (48 hours after admission); the time interval between the onset of the symptoms and hospitalization can be variable, and the ratio between NLR48 and NLR0 may reflect the trend of increasing or decreasing inflammation and therefore may theoretically overcome the limitations induced by the timing of NLR determination and also of NLR physiological variations. Moreover, the ratio between NLR48 and NLR0 may eliminate the individual variation in the NLR and therefore may be more accurate than NLR0 or NLR48 for prognosis prediction.
Materials and Methods
We performed a retrospective, cross-sectional study in order to analyze the role of the NLR (at admission, NLR0 at 48 hours, NLR48; and the ratio between, NLR48/NLR0) as compared with BISAP and SOFA scores, and also with mCTSI and CRP levels for the prediction of mortality in patients admitted with acute pancreatitis into the Emergency Clinical County Hospital of Craiova during a period of 48 months (January 2018–December 2021). We collected the clinical data of the patients (age, sex, predisposing factors, clinical history, complications), and laboratory data at admission (including serum triglyceride level, serum amylase and lipase, creatinine, bilirubin, ASAT, and ALAT values) and at 48 h (including hemogram and CRP level at 48 hours). The SOFA, BISAP, and mCTSI scores were estimated, as also the APACHE II score for patients admitted to ICU.
The primary assessed outcomes were the rate of in-hospital mortality, the rate of persistent organ failure, and intensive care unit admissions. The study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all admitted patients and an approval by Local Ethics Committee of the Emergency Clinical County Hospital of Craiova was also obtained (Protocol No 18592/13 April 2023). Patients aged below 18 years, those with other chronic severe diseases (malignancy, chronic severe organ dysfunction, acute or chronic leukemia, acute extrapancreatic infections) which can interfere with the NLR values, and those with insufficient data were excluded from the study.
The diagnosis of acute pancreatitis was based on Atlanta classification and definitions criteria,19 with two of the following three criteria: the symptoms of abdominal pain consistent with acute pancreatitis (acute onset of a persistent, severe, epigastric pain which often radiates to the back), serum lipase/amylase greater than 3 times upper normal limit, and characteristic findings of CT/IRM for acute pancreatitis. The diagnosis of HTG-AP was made by a level above 1000 mg/dL (11.3 mmol/L) or in the case of values between 500 and 1000 mg/dL (5.65–11.3 mmol/L) if other possible etiologies were excluded.17 SAP was diagnosed by the presence of persistent organ dysfunction (respiratory, circulatory, and renal) with a Marshall score of a minimum of 2 points.19 Local collections included acute peripancreatic fluid collections, pancreatic pseudocysts, and necrosis. Patients with acute biliary pancreatitis were admitted to the Surgery Department; those with other etiology were admitted to the Gastroenterology Department and transferred to the Surgery Department when surgical procedures were required.
Statistical analysis was performed using Microsoft Excel (Microsoft Corp., Redmond, WA, USA), together with the XLSTAT 2016 add-on for MS Excel (Addinsoft SARL, Paris, France) and IBM SPSS Statistics 20.0 (IBM Corporation, Armonk, NY, USA) for processing the data. Three categories of patients were analyzed: all acute pancreatitis, acute pancreatitis with POF, and those admitted to the ICU. We constructed the ROC curves for NLR0, NLR48, NLR48 to NLR0 ratio, BISAP and SOFA score, CRP48, mCTSI, and APACHE II score in patients admitted to the ICU; only if the difference from 50% for AUC proved highly significant (p<0.001), we should consider as relevant the cut-off values identified in order to maximize the sensitivity, specificity, and accuracy for that threshold. The results of the study were presented according to the STROBE statement.20
Results
General Characteristics of the Study Group
A total of 725 patients were selected during the analyzed period; 58.9% were male, mean age was 56.8 years. In total, 42.4% had biliary acute pancreatitis, 27.7% had alcoholic acute pancreatitis, and 8.7% had hypertriglyceridemia-induced acute pancreatitis. A total of 8.1% were admitted to the ICU during hospitalization, and 13.6% had POF during admission. Fifty-seven deaths were recorded (7.9% of all cases mortality).
To test the normality of the data for all patients with acute pancreatitis we used the Anderson–Darling test. None of the numerical variables investigated had a normal distribution of data, globally (p<0.0001, except for hematocrit where we found p-value=0.0028); because the data did not follow a normal distribution, results were summarized as the median value and interquartile interval and nonparametric statistical tests should be used. The general characteristics of the selected group are presented in Table 1.
 |
Table 1 Basic Characteristics of Patients with Acute Pancreatitis |
All Patients with Acute Pancreatitis
For mortality prediction, the AUC for all patients with acute pancreatitis was 0.596 for NLR0, 0.809 for NLR48, 0.676 for the ratio between NLR48 and NLR0, 0.529 for CRP48, 0.610 for mCTSI, 0.827 for the BISAP score, and 0.809 for the SOFA score. NLR48 was superior to NLR0 for death prediction; the ratio between NLR48 and NLR0 was superior to NLR0 but inferior to NLR48. The accuracy of BISAP and SOFA scores was similar to NLR48 and superior to NLR0. Both the CRP48 level and mCTSI had an accuracy inferior to BISAP, SOFA, and NLR48 (Figure 1). The sensitivity and specificity were 79.5% and 74.3% for NLR48 (at 7.466 cutoff), 75.7% and 72.7% for BISAP (at 1.000 cutoff), and 63% and 83.9% for SOFA (at 2.000 cutoff). It is remarkable that a simpler score such as the NLR has a sensitivity and specificity similar to some complex scores such as BISAP and SOFA (which require the use of multiple parameters).
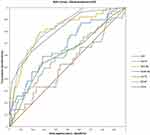 |
Figure 1 AUC for mortality prediction, all patients with acute pancreatitis. |
For the prediction of POF, the AUC for all patients with acute pancreatitis was 0.619 for NLR0, 0.785 for NLR48, 0.635 for the ratio between NLR48 and NLR0, 0.513 for CRP48, 0.565 for mCTSI score, 0.817 for BISAP score, and 0.848 for SOFA score (Figure 2). The accuracy of BISAP and SOFA scores was superior to both NLR48 and NLR0; the ratio between NLR48 and NLR0 was superior to NLR0 but inferior to NLR48 (Table 2).
 |
Table 2 AUC and 95% Confidence Interval (CI) for the Prediction of Death and POF in All Patients with Acute Pancreatitis |
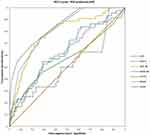 |
Figure 2 AUC for the prediction of persistent organ failure, all patients with acute pancreatitis. |
Patients with Acute Pancreatitis and Persistent Organ Failure/Admitted to the ICU
In patients with POF, the AUC for mortality prediction was 0.453 for NLR0, 0.623 for NLR48, 0.577 for the ratio between NLR48 and NLR0, 0.478 for CRP48, 0.512 for mCTSI, 0.470 for the BISAP score, and 0.561 for the SOFA score (Table 3). All scores had only low or moderate accuracy for mortality in patients with POF (Figure 3).
 |
Table 3 AUC and 95% Confidence Interval (CI) for the Prediction of Death in Patients with Acute Pancreatitis and POF and in Those Admitted to the ICU |
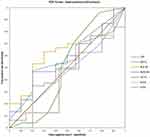 |
Figure 3 AUC for mortality prediction in patients with persistent organ failure. |
Fifty-nine patients were admitted to the ICU Department (8.1%). For mortality prediction in patients admitted to the ICU, the AUC was 0.535 for NLR0, 0.650 for NLR48, 0.524 for the ratio between NLR48 and NLR0, 0.459 for CRP48, 0.546 for mCTSI, 0.650 for the BISAP score, 0.692 for the SOFA score and 0.757 for APACHE II score (Table 3). APACHE II score has had the highest accuracy for predicting mortality in ICU-admitted patients (Figure 4).
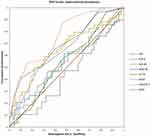 |
Figure 4 AUC for mortality prediction in patients admitted to the ICU. |
We analyzed the accuracy of NLR0, NLR48, NLR48/NLR0, BISAP, mCTSI, and SOFA score for the prediction of mortality stratified by etiology (alcoholic pancreatitis=201 cases, biliary pancreatitis=308 cases, hypertriglyceridemic pancreatitis=63 cases). NLR48 had good accuracy in both alcoholic and biliary pancreatitis (AUC 0.798 and 0.871, respectively) but not in hypertriglyceridemic pancreatitis. NLR48/NLR0 had a moderate accuracy only in biliary pancreatitis (AUC 0.81), inferior to NLR48. BISAP and SOFA scores had both a good accuracy in alcoholic pancreatitis; BISAP performed better in biliary pancreatitis (AUC 0.80 versus 0.68 for SOFA) while the SOFA score performed better in hypertriglyceridemic pancreatitis (AUC 0.87 versus 0.78 for BISAP) and was the only score with statistical significance. The mCTSI score had moderate accuracy in all forms (AUC 0.73 in alcoholic pancreatitis, 0.64 in biliary pancreatitis, and 0.84 in hypertriglyceridemic pancreatitis), although with borderline statistical significance P-values between 0.05 and 0.07 (Table 4).
 |
Table 4 AUC and 95% Confidence Interval (CI) for the Prediction of Death in Patients with Acute Pancreatitis by Etiology |
Discussion
Early prediction of complications and mortality in acute pancreatitis represents an important factor for therapeutic decisions including ICU admissions and aggressive early treatment in potentially severe cases. Several predictive scores have been proposed, the most used being Ranson, Glasgow–Imrie, SOFA, and BISAP scores; Balthazar and later mCTSI scores have been proposed for CT evaluation of pancreatitis severity, and APACHE II score is generally used in ICU-admitted patients. Ranson and Glasgow–Imrie scores are the first proposed predictive scores but require many parameters and also further evaluation of several parameters at 48 h after admission.
A simplified score or a single, high predictive parameter may represent an attractive approach to predict the severity, the risk of persistent organ failure, the risk of ICU admission, and the risk of mortality. CRP represents one of the most used biological parameters for evaluating the prognosis in acute pancreatitis; a study has shown that CRP at 48 h has an AUC of 0.70 (inferior to mCTSI) and, at a cut-off value of 150 mg/dL, a positive predictive value (PPV) of only 30% was reached, with a negative predictive value (NPV) of 87.39% at 150 mg/dL and 88.81% at 190 mg/dL.5
The NLR reflects an altered inflammatory ratio between activator (neutrophils) which promotes inflammation by activating pro-inflammatory cytokines (IL-1, 6, TNF-α) and proteolytic enzymes (myeloperoxidase, elastase, collagenase) and regulators (lymphocytes) which are related to the regulation of the immune system pathway. Persistent lymphopenia correlates with progressive inflammation in emergency admission and ICU patients, while higher neutrophil counts and pro-inflammatory-activated mediators are related to SIRS and progression toward multiple organ dysfunctions.17 In acute pancreatitis, a high ratio between neutrophils and lymphocytes may be associated with higher local and systemic inflammation and a lower specific immune response, and higher values of the NLR at admission (NLR0) and at 48 h (NLR48) were more frequent in severe cases.10,14 In published studies, NLR values at admission (NLR0), in days 1 and 2, and at 48 h (NLR48) were higher in severe acute pancreatitis (SAP) than in those with mild disease,10,14 and a meta-analysis of 10 papers showed a combined sensitivity of 79% and specificity of 71%, with an AUC of 0.82.2 Some studies compared the NLR with the BISAP score11–13 or with mCTSI,11 with similar accuracy.
In our study, the accuracy for mortality prediction in all patients with acute pancreatitis was highest for the BISAP score (AUC 0.827), followed by NLR48 and the SOFA score (both with AUC 0.809), while for NLR48/NLR0 (AUC 0.676), mCTSI (AUC 0.610), NLR0 (AUC 0.596), and CRP48 (AUC 0.529) the accuracy was low. At calculated best cutoff points, the sensitivity was best for NLR48 (79.5%), while the specificity was best for the SOFA score (83.9%). For POF prediction in all acute pancreatitis, the highest accuracy was noted for the SOFA score (0.848), followed by the BISAP score (AUC 0.817) and NL48 (AUC 0.785), while for NLR48/NLR0 (AUC 0.635), NLR0 (0.619), mCTSI (AUC 0.565), and CRP48 (0.513) the accuracy was low. The accuracy of the NLR in predicting mortality in acute pancreatitis, in severe forms, or in patients admitted to the ICU department was less studied, and most published papers were focused on predicting severe cases with persistent organ failure. The AUC for NLR0 for POF prediction for all-causes acute pancreatitis in the literature was estimated between 0.681 and 0.915,8,10–14 and a combined AUC of 0.82 was noted in a meta-analysis.10 NLR48 was evaluated in a few studies and a meta-analysis for accuracy in predicting severe acute pancreatitis and AUCs between 0.739 and 0.93 were found.8,10,13 For BISAP, the AUC was 0.82 for mortality and 0.87 for SAP, for the Ranson score the AUC was 0.92 for mortality and 0.83 for SAP, while for APACHE II the AUC was 0.83 for mortality and 0.82 for SAP; the pooled sensitivity and specificity for mortality was 81% and 70% for BISAP, 93% and 69% for the Ranson score, and 95% and 68% for APACHE II.3
Regarding the predictive role stratified by etiology, in our study NLR48 had a good predictive value for mortality in alcoholic and biliary pancreatitis (AUC 0.798 and 0.871, respectively) but not in hypertriglyceridemic pancreatitis (AUC 0.544). For mortality prediction, there was no added value of NLR48/NLR0 ratio stratified by etiology of acute pancreatitis. Several studies have analyzed the predictive value of the NLR for severity in correlation with the etiology of acute pancreatitis;9,15–17 the most frequent causes of acute pancreatitis are biliary stones, alcoholic pancreatitis, and HTA-AP.1 HTG-AP has gradually increased during the last decades17 and represents the third cause of AP with 2–5% of total cases in the USA;17 several studies in China found an even higher rate than for alcohol-induced pancreatitis.21,22 The mechanism of HTG-AP17,21 is related to the hydrolyzation of excessive TG by pancreatic lipase into free fatty acids; when the binding capacity of serum albumin is surpassed, the activation of protein kinase can induce an inflammatory response, pancreatic capillary damage, and also increased blood viscosity, pancreatic ischemia, and local acidosis. HTG-AP can be more severe than other forms,17,21,22 with more systemic complications, and SIRS, but with no differences regarding mortality, hospitalization, and fewer infected necrosis.22–24 Studies published in the literature have shown that in acute biliary pancreatitis the NLR had an AUC of 0.663 for predicting severe forms, while in acute hypertriglyceridemic pancreatitis, an AUC of 0.673 was noted in one study and an OR of 1.314 (95% CI 1.161–1.488, P<0.001) was also noted in multivariate analysis in another study.17 The NLR has been shown to predict the severity of gallstone acute pancreatitis but not of alcoholic acute pancreatitis,9 and another study showed the predictive value for severity only in HTG-AP but not in gallstone or alcohol-induced acute pancreatitis;15 the OR for high NLR in severe acute pancreatitis was 1.34 (p<0.001).17 The AUC for predicting the severity of HTG-AP was 0.706 in one study,15 and 0.673 in another study.16
The NLR may have significant individual variations and therefore the accuracy regarding the prognosis may be altered because of that. Although, in theory, the evolution of the NLR may be a more specific indicator for the prognosis and an increase in the NLR over time may suggest an increased systemic inflammation and therefore a higher risk of complications, severe pancreatitis, and death, in our study the ratio between NLR48 and NLR0 had higher accuracy than NLR0, but the accuracy was lower than NLR48, BISAP, and SOFA scores for the prediction of death risk.
All studied scores had only mild accuracy for death prediction in the subgroup including persistent organ failure patients (AUC between 0.45 and 0.63). In patients admitted into the ICU, moderate accuracy was obtained only for APACHE II (AUC 0.757), while for the SOFA score, BISAP score, NLR48, NLR48/NLR0 mCTSI, NLR0, and CRP48 the predictive value was less accurate (AUC 0.692 for SOFA, 0.650 for BISAP and NLR48, 0.546 for mCTSI, 0.535 for NLR0, and 0.459 for CRP48).
The NLR48 score has been superior to CRP48h in all predicted outcomes and therefore may substitute the determination of CRP at 48 hours as a predictive parameter for mortality and persistent organ failure.
There were some limitations of the study related to the patients not included because of the missing data, especially in case of the patients who died shortly before admission and in patients not included into the study because no NLR48 and CRP48 was obtained; the relatively small group of patients with HTG-AP (63 cases) can also influence the performance of analyzed scores.
Conclusions
In all patients with acute pancreatitis, the AUC for NLR48 in predicting mortality risk and severe forms was superior to NLR0, CRP48, and mCTSI and similar to BISAP and SOFA scores; the ratio between NLR48 and NLR0 did not add significantly to the accuracy. Both NLR0 and NLR48 performed poorly for mortality prediction in severe forms and in patients admitted to ICU. NLR48 has good accuracy in our study for predicting death risk in biliary and alcoholic acute pancreatitis but not in hypertriglyceridemic acute pancreatitis.
Acknowledgments
Naina Popescu and Robert Godeanu (resident physicians) contributed to the data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The Article Processing Charges were funded by the University of Medicine and Pharmacy of Craiova, Romania.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Iannuzzi JP, King JA, Leong JH, et al. Global incidence of acute pancreatitis is increasing over time: a systematic review and meta-analysis. Gastroenterology. 2022;162(1):122–134. PMID: 34571026. doi:10.1053/j.gastro.2021.09.043
2. Kong W, He Y, Bao H, Zhang W, Wang X. Diagnostic value of neutrophil-lymphocyte ratio for predicting the severity of acute pancreatitis: a meta-analysis. Dis Markers. 2020;2020:9731854. PMID: 32454909; PMCID: PMC7232731. doi:10.1155/2020/9731854
3. Gao W, Yang HX, Ma CE, Sastre J. The value of BISAP score for predicting mortality and severity in acute pancreatitis: a systematic review and meta-analysis. PLoS One. 2015. 10(6):e0130412. Erratum in: PLoS One. 2015; 10(10): e0142025. PMID: 26091293; PMCID: PMC4474919. doi:10.1371/journal.pone.0130412
4. Bálint ER, Fűr G, Kiss L, et al. Assessment of the course of acute pancreatitis in the light of aetiology: a systematic review and meta-analysis. Sci Rep. 2020;10(1):17936. PMID: 33087766; PMCID: PMC7578029. doi:10.1038/s41598-020-74943-8
5. Ahmad R, Bhatti KM, Ahmed M, et al. C-reactive protein as a predictor of complicated acute pancreatitis: reality or a myth? Cureus. 2021;13(11):e19265. PMID: 34900460; PMCID: PMC8648202. doi:10.7759/cureus.19265
6. Chen X, Ning J, Li Q, Kuang W, Jiang H, Qin S. Prediction of acute pancreatitis complications using routine blood parameters during early admission. Immun Inflamm Dis. 2022;10(12):e747. PMID: 36444624; PMCID: PMC9695081. doi:10.1002/iid3.747
7. Azab B, Jaglall N, Atallah JP, et al. Neutrophil-lymphocyte ratio as a predictor of adverse outcomes of acute pancreatitis. Pancreatology. 2011;11(4):445–452. PMID: 21968329. doi:10.1159/000331494
8. Suppiah A, Malde D, Arab T, et al. The prognostic value of the neutrophil-lymphocyte ratio (NLR) in acute pancreatitis: identification of an optimal NLR. J Gastrointest Surg. 2013;17(4):675–681. PMID: 23371356. doi:10.1007/s11605-012-2121-1
9. Cho SK, Jung S, Lee KJ, Kim JW. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio can predict the severity of gallstone pancreatitis. BMC Gastroenterol. 2018;18(1):18. PMID: 29370777; PMCID: PMC5785858. doi:10.1186/s12876-018-0748-4
10. Kokulu K, Günaydın YK, Akıllı NB, et al. Relationship between the neutrophil-to-lymphocyte ratio in acute pancreatitis and the severity and systemic complications of the disease. Turk J Gastroenterol. 2018;29(6):684–691. PMID: 30381275; PMCID: PMC6284671. doi:10.5152/tjg.2018.17563
11. Tahir H, Rahman S, Habib Z, Khan Y, Shehzad S. Comparison of the accuracy of modified CT Severity Index Score and neutrophil-to-lymphocyte ratio in assessing the severity of acute pancreatitis. Cureus. 2021;13(8):e17020. PMID: 34522501; PMCID: PMC8425492. doi:10.7759/cureus.17020
12. Gezer NS, Bengi G, Baran A, et al. Comparison of radiological scoring systems, clinical scores, neutrophil-lymphocyte ratio and serum C-reactive protein level for severity and mortality in acute pancreatitis. Rev Assoc Med Bras. 2020;66(6):762–770. PMID: 32696885. doi:10.1590/1806-9282.66.6.762
13. Dancu GM, Popescu A, Sirli R, et al. The BISAP score, NLR, CRP, or BUN: which marker best predicts the outcome of acute pancreatitis? Medicine. 2021;100(51):e28121. PMID: 34941057; PMCID: PMC8702250. doi:10.1097/MD.0000000000028121
14. Han C, Zeng J, Lin R, et al. The utility of neutrophil to lymphocyte ratio and fluid sequestration as an early predictor of severe acute pancreatitis. Sci Rep. 2017;7(1):10704. PMID: 28878366; PMCID: PMC5587690. doi:10.1038/s41598-017-10516-6
15. Huang L, Chen C, Yang L, Wan R, Hu G. Neutrophil-to-lymphocyte ratio can specifically predict the severity of hypertriglyceridemia-induced acute pancreatitis compared with white blood cell. J Clin Lab Anal. 2019;33(4):e22839. PMID: 30737845; PMCID: PMC6528595. doi:10.1002/jcla.22839
16. Lu Z, Chen X, Ge H, et al. Neutrophil-lymphocyte ratio in patients with hypertriglyceridemic pancreatitis predicts persistent organ failure. Gastroenterol Res Pract. 2022;2022:8333794. PMID: 35340692; PMCID: PMC8942680. doi:10.1155/2022/8333794
17. Yu S, Wu D, Jin K, et al. Low serum ionized calcium, elevated high-sensitivity C-reactive protein, neutrophil-lymphocyte ratio, and Body Mass Index (BMI) are risk factors for severe acute pancreatitis in patients with hypertriglyceridemia pancreatitis. Med Sci Monit. 2019;25:6097–6103. PMID: 31413252; PMCID: PMC6707096. doi:10.12659/MSM.915526
18. Forget P, Khalifa C, Defour JP, Latinne D, Van Pel MC, De Kock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes. 2017;10(1):12. PMID: 28057051; PMCID: PMC5217256. doi:10.1186/s13104-016-2335-5
19. Banks PA, Bollen TL, Dervenis C, et al. Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–111. PMID: 23100216. doi:10.1136/gutjnl-2012-302779
20. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Available from: https://www.equator-network.org/reporting-guidelines/strobe/.
21. Guo YY, Li HX, Zhang Y, He WH. Hypertriglyceridemia-induced acute pancreatitis: progress on disease mechanisms and treatment modalities. Discov Med. 2019;27(147):101–109. PMID: 30939294.
22. Li X, Ke L, Dong J, et al. Significantly different clinical features between hypertriglyceridemia and biliary acute pancreatitis: a retrospective study of 730 patients from a tertiary center. BMC Gastroenterol. 2018;18(1):89. PMID: 29914404; PMCID: PMC6007076. doi:10.1186/s12876-018-0821-z
23. Bosques-Padilla FJ, Vázquez-Elizondo G, González-Santiago O, et al. Hypertriglyceridemia-induced pancreatitis and risk of persistent systemic inflammatory response syndrome. Am J Med Sci. 2015;349(3):206–211. PMID: 25545390. doi:10.1097/MAJ.0000000000000392
24. Wang Y, Fuentes HE, Attar BM, Jaiswal P, Demetria M. Evaluation of the prognostic value of neutrophil to lymphocyte ratio in patients with hypertriglyceridemia-induced acute pancreatitis. Pancreatology. 2017;17(6):893–897. PMID: 29030078. doi:10.1016/j.pan.2017.10.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
