Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
Nine-Year Follow-Up of Interleukin 6 in Chronic Obstructive Pulmonary Disease – Complementary Results from Previous Studies
Authors Prudente R , Ferrari R , Mesquita C , Machado L, Franco E, Godoy I, Tanni S
Received 14 July 2021
Accepted for publication 27 September 2021
Published 3 November 2021 Volume 2021:16 Pages 3019—3026
DOI https://doi.org/10.2147/COPD.S328266
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Robson Prudente,1 Renata Ferrari,2 Carolina Mesquita,2 Luiz Machado,2 Estefânia Franco,1 Irma Godoy,2 Suzana Tanni2
1Clinical Hospital of Botucatu Medical School, Department of Internal Medicine, Pneumology Area, Botucatu School of Medicine, São Paulo State University (UNESP), Botucatu, São Paulo, Brazil; 2Department of Internal Medicine, Pneumology Area, Botucatu School of Medicine, São Paulo State University (UNESP), Botucatu, São Paulo, Brazil
Correspondence: Robson Prudente
Clinical Hospital of Botucatu Medical School, Department of Internal Medicine, Pneumology Area, Botucatu School of Medicine, São Paulo State University (UNESP), Botucatu, São Paulo, Brazil
Email [email protected]
Background: Systemic manifestations of chronic obstructive pulmonary disease (COPD) are related to increased systemic inflammatory process; however, it is not entirely clear how much they are related and how the systemic inflammation, in particular interleukin-6 (IL-6), is associated with exacerbation and mortality risk.
Objective: To evaluate the role of IL-6 in COPD patients over nine years.
Study Design and Methods: A total of 133 COPD patients were assessed at baseline between 2004 and 2006 and reassessed after three and nine years through clinical evaluation, comorbidities, hematological blood count and IL-6 analysis.
Results: After nine years, 19 patients lost the follow-up and were not possible to identify the date of death of four patients; 12 refused to participate and 1 could not be involved due to recurrent exacerbations. Therefore, 33 patients were included in the reassessment after nine years of follow-up and 92 patients were included in the Cox mortality analysis with IL-6 as a time-dependent covariate. Regarding the inflammatory profile, in patients who survived after nine years, there was a significant increase in IL-6 [0.4 (0.2– 0.8) vs 5.7 (3.4– 11) pg/mL; p < 0.001] and reduction in lymphocyte count [2.1 (1.6– 2.4) vs 1.4 (1.2– 2.1)10^9/L; p < 0.01] with an increase in the neutrophil/lymphocyte ratio (2.0 ± 0.7 vs 2.7 ± 1.2; p = 0.003). The Cox mortality model did not show a statistical significance influence of IL-6 assessed during the follow-up.
Conclusion: There was a progressive increase in IL-6 during the follow-up, however, without influence on mortality.
Keywords: chronic obstructive pulmonary disease, inflammation, interleukin-6, severity of illness index, mortality
Background
Chronic obstructive pulmonary disease (COPD) is defined as a frequent, preventable, and treatable condition characterized by persistent respiratory symptoms and progressive, not fully reversible airflow obstruction. The etiology is multifactorial and involves genetic aspects, exposure to risk factors and abnormal lungs inflammatory response.3 Local manifestations are characterized by reduction in forced expiratory volume in the first second (FEV1), pulmonary hyperinflation, a decrease in respiratory muscle strength and resistance, together these factors are associated with ventilation decrease and dyspnea increase. These changes are associated with the restriction of activities of daily living (ADLs) and, consequently, worsening quality of life.3–5 Moreover, studies have shown that the condition does not only affect the lungs and respiratory muscles but there is also significant systemic impairment such as protein-energy malnutrition, reduced peripheral muscle strength and endurance, and decreased exercise tolerance, which also have a great impact on the severity of the disease and quality of life.3,5,6
It is known that the systemic manifestations of COPD are related to increase systemic inflammatory process7 despite, it is not fully understood or how much they are related in this process.8 In addition, the most recent studies show that systemic inflammation, especially the activation of interleukin-6 (IL-6), is associated with higher risk of exacerbation, symptom burden and mortality.9–12
IL-6 corresponds to a cytokine that acts on both the innate and adaptive immune responses; it is synthesized by monocytes, endothelial cells, fibroblasts, and other cells in response to microorganisms and stimulation by other cytokines, mainly interleukin-1 (IL-1) and tumor necrosis factor alpha (TNF-α).13 During the differentiation of CD4 T cells, IL-6 promotes the production of IL-17 and IL-21 and suppresses the regulatory function of T cells. The effect generated is precisely the deposition of matrix, antibody complexes and proteases in the target tissue and, consequently, lung parenchyma destruction.14,15 Especially during the period of exacerbation, macrophages are unable to ingest apoptotic cells and bacteria, causing more activation of inflammatory cells and the release of several mediators, including IL-6.
In that regard, there are few studies which evaluated the influence of IL-6 in a long time of follow-up and its association with mortality in COPD patients.2,16 Furthermore, we did not find many data from nearly a decade of follow-up related to IL-6 in Brazilian COPD patient.10,17–24 In this sense, better understanding the role of IL-6 over time, helps in a more effective search for inflammation control and, consequently, minimizes its related outcomes, such as reduced physical capacity, greater occurrence of exacerbations and increased mortality.9–12 Thus, our hypothesis is that IL-6 is associated to COPD mortality over nine years of follow-up and the objective of our study was to assess the association of IL-6 in mortality risk in patients with COPD over nine years, as well as verify the variation of IL-6 in survivals over nine years.
Study Design and Methods
Settings
This is the third of three studies that evaluated patients with COPD over nine years, approved by Botucatu School of Medicine Research Ethics Committee (approval number: 1.527.377) and was conducted in accordance with the principles of the Declaration of Helsinki. All subjects involved in the research agreed to participate signing the informed consent form after objectives and methods of the research have been clarified. The applied methodology was the same used in this previous study, where further details can be found.22,24
Participants
In general, between 2004 and 2006, 133 COPD patients from the Pulmonology outpatient clinic of Botucatu Medical School were invited to participate in this study. Inclusion criteria were patients diagnosed with COPD, clinical stability, and optimized drug therapy. Exclusion criteria were patients with diagnoses of other respiratory diseases, noncompliance with treatment, myocardial infarction four months before the beginning of the study, unstable angina, and congestive heart failure class III and IV.
Outcomes Measurements
The regular follow-up of these patients was performed by medical appointments at least every six months and by telephone contact with the survivors who had stopped outpatient medical follow-up. A protocol of telephone contact was also used to confirm the cause of death from family members and to confirm clinical condition, frequency of exacerbations, hospitalizations and use of non-programed health-care attendance. For data collection in clinical reassessment, we considered the following periods: baseline, after three and nine years of follow-up.18,19,22
At baseline, all recruited patients were assessed by pulse oximetry, pulmonary function, nutritional evaluation, exercise tolerance, sensation of dyspnea, and presence of comorbidities. Clinical assessment, arterial blood sample, pulse oximetry and spirometry (pre- and post-bronchodilator) were performed on the first day, and venous blood sample, nutritional status, six-minute walking distance (6MWD), quality of life and dyspnea perception were assessed on another day. These assessments were reapplied to survivors after three and nine years and more details are available in previous studies.18,19,22,24
Laboratory Assessments
Laboratory evaluation included complete hematological blood count and biochemical examinations. And the analysis was performed according to the criteria and methods routinely used by the Technical Section of Botucatu School of Medicine Laboratory and Clinical Analysis.
To IL-6 analysis, blood was collected in a 10mL vacutainer tube with heparin and was centrifuged in a refrigerated centrifuge (Eppendorf 5403®) at 1000rpm for 5 minutes. The plasma from the top of the tubes was removed and centrifuged again to obtain clear plasma. The samples were stored in 1.5 mL eppendorf tubes in a refrigerator at −80°C until analysis.
The IL-6 cytokine assays were performed in duplicates by means of commercially available immunoenzymatic assays (ELISA) (Biosource International, Inc, CA, USA). For serum measurements, 0.16 to 10.0pg/mL ultra-sensitive ELISA were used for IL-6 (Human IL-6 US – Cytoscreen). The sequence of cytokines dosing followed the recommendations from the kits supplier company.
Statistical Analysis
Descriptive statistics were used to describe the features of all participants. Means, ± standard deviation or medians and interquartile range (25–75%) were used depending on the data distribution. Categorical variables were expressed as percentages. The Chi-square test was used to compare the values of categorical variables.
The comparison between two independent groups was performed by means of the Student’s t-test for variables with normal distribution and Mann–Whitney test for variables with non-normal distribution. The tool to compare two dependent groups, was paired Student’s t-test for variables with normal distribution and Wilcoxon test for non-normal distribution. Chi-square tests were used to compare qualitative variables with a frequency higher than five and Fisher’s exact test for frequency less than five.
IL-6 cutoff points were determined by 90th and 95th percentile of sample distribution. These cutoff points were used to assess associations with mortality over nine years. The Kaplan–Meier curve followed by the Log rank test was used to evaluate mortality rate related to categorization of IL-6 cut-off points.
IL-6 as a time dependent covariate was used in the Cox regression analysis to analyze the association of variation of IL-6 over time and the risk of mortality including all subjects evaluated at baseline, adjusted by baseline data of age, male gender, BODE index, Charlson Comorbidities index, number of exacerbations in the first three years of follow-up and SpO2.
The significance level was set at p < 0.05. All data were analyzed using SPSS version 17.0 (IBM Software, Dallas, TX, USA) and SAS (USA).
Results
Among the 133 patients initially evaluated (69% male, 65±9.5 years old, and FEV1: 59.7±24.9%) nineteen lost the follow-up, four did not have their cause of death identified, twelve refused to participate in the last follow-up, and one could not be included due to recurrent exacerbations. Therefore, 33 patients who survived (54.5% male, 61±8.6 years old, and FEV1: 64.2±26.6%) completed nine years follow-up assessment and 110 patients [67% male, 65±9 years old, and FEV1: 52.5 (40–73%)] were included in the mortality analysis. However, only 92 were included in Cox regression due to missing data.
Regarding the causes of death, 41 were attributed to respiratory failure, 9 to cancer, 5 to cardiovascular disease, and 9 to other causes. Four patients were excluded from the analyses due to a lack of information concerning date and cause of death. Demographic and clinical characteristics of the involved patients in the survival analysis, and the evolution of other markers at baseline, after three and nine years can be consulted in a previous publication and in Supplemental Material.22,24
In relation to the IL-6 of survival patients (n = 33), after nine years there was a significant increase in IL-6 values [0.4 (0.2–0.8) vs 5.7 (3.4–11) pg/mL; p < 0.001], reduction in lymphocyte count [2.1 (1.6–2.4) vs 1.4 (1.2–2.1)10^9/L; p < 0.001] and increased neutrophil/lymphocyte (N/L) ratio (2.0±0.7 vs 2.7±1.2; p = 0.003). The other peripheral blood cells showed no variation at baseline and after nine years. In addition, when analyzed those who had a reduction in FEV1 > 40mL after nine years (n = 14) was observed an increase in IL-6 after nine years when compared to baseline [0.4 (0.23–0.88) vs 5.73 (3.67–10.47) pg/mL; p < 0.001], and a reduction in lymphocyte count (1.8±0.41 vs 1.6±0.6 10^9/L; p = 0.01) at the final moment.
The comparison of IL-6 at baseline between patients who survived or not after nine years showed that the survivors had statistically significant lower IL-6 values at baseline [0.49 (0.2–0.8) vs 1.29 (0.6–1.9) pg/mL; p < 0.001]. The comparison of the lymphocyte count of these groups did not show statistically significant differences (p = 0.20), whereas the N/L ratio was higher in patients who died [2.0 (1.5–2.3) vs 2.4 (1.9–3.5); p = 0.006]. The evolution of inflammatory profile at baseline, after three and nine years can be seen in Table 1.
 |
Table 1 Evolution of Inflammatory Profile at Baseline, After Three and Nine Years |
The IL-6 distribution of the population at baseline can be seen in Figure 1 and, to evaluate the association of the 90th (≥2.3pg/mL) and 95th (≥3.1pg/mL) percentiles of IL-6 baseline with the mortality of all patients, the Kaplan–Meier curve followed by the Log Rank test showed a statistically significant difference between the groups when categorized as <3.1pg/mL or ≥3.1pg/mL. Patients with higher values of IL-6 at baseline showed higher death risk during nine years. However, it is noteworthy that the sample ≥3.1pg/mL consisted only of five individuals (Figure 2). A similar result was observed using the cutoff point of 90th of the sample, with seven being the number of individuals categorized with IL-6 ≥2.3pg/mL (Figure 3).
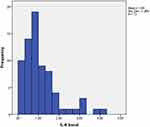 |
Figure 1 IL-6 distribution of the population studied at baseline. |
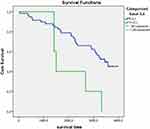 |
Figure 2 Kaplan–Meier mortality curve in relation to patients with IL-6 ≥ or < 3.1pg/mL. |
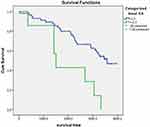 |
Figure 3 Kaplan–Meier mortality curve in relation to patients with IL-6 ≥ or < 2.3pg/m. |
Cox’s regression analysis showed no association between the IL-6 variation over time and the mortality rate over nine years (n = 92) (Table 2). When imputing the missing data by using multiple imputation of covariates and IL-6 as a time dependent covariate, of IL-6 influence could not be assessed, and only BODE index was a predictor of mortality [Hazard ratio (HR): 1.4 (95% HR Confidential interval: 1.1–1.7); p = 0.003].
 |
Table 2 Assessment of IL-6 as a Time Dependent Covariate in Cox Regression Analysis |
Discussion
The present study aimed to evaluate the role of IL-6 in patients with COPD over nine years. Previous studies have already shown that patients with stable COPD have higher serum IL-6 concentrations compared to healthy controls, however, our findings indicate that the increase in IL-6 is gradual over time, according to the evolution of the disease itself.25,26 The increase in inflammation, even in patients with less FEV1 variation, draws attention to the fact that the systemic inflammation is a persistent and progressive process, even in those who maintain pulmonary function unchanged or with small loss, suggesting that an isolated analysis of COPD prognostic markers requires some caution.
FEV1 has already been shown to be closely related to chronic respiratory symptoms in the general population.27 Tantucci and Modina28 have also warned that would be more logical to undertake efforts for early detection of COPD based on risk factors, rather than just symptoms. Thus, based on this assumption and our findings, we can infer that the association of evaluation of the disease markers, such as prognostic and inflammatory markers, may be more appropriate in the assessment of these patients over long periods.
In addition, we also found that the IL-6 analysis showed that patients who survived after nine years of follow-up had less inflammation at baseline compared to those who were known to have died, showing a better prognosis for those with lower cytokine values. We also found that when considering the individuals with highest IL-6 values (90th and 95th percentiles of the sample) there was a higher risk of death, nevertheless, in the latter case, we should consider the small number of subjects categorized in these groups. Similar findings were observed in the study conducted by Mehrotra et al29 where IL-6 was a significant predictor of mortality in 268 individuals with obstructive airway disease, however, for some years now, prospective studies have shown that elevated IL-6 has been a useful marker for predicting worse outcomes in COPD.9,10,30,31 The population of this study has already demonstrated in the three-year follow-up, that a significant increase in IL-6 was associated with higher mortality.10
On the other hand, other studies have found no major link between IL-6 and worse outcomes in COPD. The ECLIPSE study,16 for example, found no association between IL-6 with a greater number of exacerbations in three years and, similarly, the Fermont et al32 meta-analysis showed associations between high levels of IL-6 with the hospitalization rate of patients with COPD, it also did not indicate associations with the number of exacerbations and mortality of these patients. Likewise, our model with serial analysis of IL-6 in three moments also did not show influence of IL-6 on the mortality rate of these individuals during the follow-up period. However, we cannot affirm that our results show a true relationship between IL-6 and mortality, since we have no power in relation to the sample size. There is no consensus in the literature about the influence of IL-6 on mortality of patients COPD and, in this sense, although some authors such as Celli et al30 have shown that IL-6, by itself, improves the ability to predict mortality in COPD, the authors themselves claim that the association of biomarkers further improves this ability, which corroborates with the idea that the combination of inflammatory markers assessment and other COPD markers (such as FEV1, for example) may be more accurate.
Therefore, it can be said that the systemic impairment caused by COPD, not directly related to the inflammatory aspect, is also capable of influencing the mortality of these individuals, given that the patients who are known to have died, both at baseline and after three years of follow-up, still had low IL-6 values. In a previous study carried out with these individuals, we observed that were predictive of mortality in nine years the number of exacerbations in the first three years of follow-up, greater severity by the BODE index, higher scores on the Charlson index and lower BMI.22 We observed that in the imputation of the missing data in Cox’s regression analysis, the BODE index predicted the mortality of this population in nine years, considering IL-6 as a time-dependent covariate. However, the limitations related to the imputation of data require that these results should be analyzed with greater caution to prevent wrong conclusions.33 Specifically, in relation to the BODE index and IL-6, Khan et al34 demonstrated that serum IL-6 concentrations exhibited significant correlation with BODE index, thus, future studies with these variables can be considered to assess these patients.
Regarding the reduction in the number of lymphocytes, we observed a decrease in the cell count with a significant increase in N/L ratio. It is known that low lymphocyte count is associated with poor prognosis in acute and chronic conditions, and factors such as age and deficient nutritional status35 and with agreement of that, Acanfora et al36 in a three-year prospective study with 218 patients with COPD and age around 75 years, observed that the relative reduction in cell count was associated with higher mortality. Besides that, Xiong et al37 found that neutrophils and lymphocytes independently correlate with mortality, but with less relevance compared to the N/L ratio. A study conducted by Lee et al38 demonstrated a correlation of FEV1 in COPD patients only with N/L ratio and not with the cells count alone, in accordance with our findings which demonstrated that only the lymphocyte count in patients who died was no different at baseline from those who survived, whereas the N/L ratio was significantly higher in those who died over the nine years of follow-up. However, further analysis should be performed despite these findings for better conclusions.
The present study has limitations that need to be clarified. During the follow-up, we had about 17% of loss, which may have interfered in our findings. Nevertheless, longitudinal population studies show that the loss of follow-up is greater in longer periods and the percentage presented in the literature is like our findings.20 In addition, we emphasize that the present study does not aim to identify cause and effect, so we can only affirm the possible associations between IL-6 and the mortality of patients with COPD in nine years, thus, more robust studies are encouraged for confirm these findings.
Conclusion
When outlining the role of IL-6 in COPD patients over nine years, it was seen that there was a progressive increase in cytokine during the follow-up period, even though, without influence on mortality. It is suggested, therefore, that in longitudinal segments with longer periods, for prognostic evaluation and mortality of this population, both inflammatory markers and other COPD markers should be analyzed together.
Acknowledgment
The manuscript is part of a PhD thesis of São Paulo State University. After the thesis defense, the full thesis is temporarily made available on-line.1 Besides that, the abstract of this paper has been presented at the ERS International Congress 2018 as a poster presentation. The poster’s abstract was published in the European Respiratory Journal 2020 56: 2471; DOI: 10.1183/13993003.congress-2020.2471.2
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Prudente RA, Tanni SE. Interleucina 6 de pacientes com DPOC em nove anos; 2020.
2. Prudente R, Mesquita C, Franco E, Ferrari R, Godoy I, Tanni S. Role of interleukin 6 in COPD patients over nine years. Eur Respir J. 2020;56:2471. doi:10.1183/13993003.congress-2020.2471.
3. Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164. doi:10.1183/13993003.00164-2019
4. Wouters EFM. Local and systemic inflammation in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005;2(1):26–33. doi:10.1513/pats.200408-039MS
5. Dourado VZ, Tanni SE, Vale SA, Faganello MM, Sanchez FF, Godoy I. Manifestações sistêmicas na doença pulmonar obstrutiva crônica. J Bras Pneumol. 2006;32(2):161–171. doi:10.1590/S1806-37132006000200012
6. Rabe KF, Beghé B, Luppi F, Fabbri LM. Update in chronic obstructive pulmonary disease 2006. Am J Respir Crit Care Med. 2007;175(12):1222–1232. doi:10.1164/rccm.200704-586UP
7. Ahmadi-Abhari S, Kaptoge S, Luben RN, Wareham NJ, Khaw KT. Longitudinal association of C-reactive protein and lung function over 13 years: the EPIC-Norfolk Study. Am J Epidemiol. 2014;179(1):48–56. doi:10.1093/aje/kwt208
8. MacNee W. Pulmonary and systemic oxidant/antioxidant imbalance in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005;2:50–60. doi:10.1513/pats.200411-056SF.
9. Agustí A, Edwards LD, Rennard SI, et al. Persistent systemic inflammation is associated with poor clinical outcomes in COPD: a novel phenotype. PLoS One. 2012;7(5):e37483. doi:10.1371/journal.pone.0037483
10. Ferrari R, Tanni SE, Caram LMO, Corrêa C, Corrêa CR, Godoy I. Three-year follow-up of Interleukin 6 and C-reactive protein in chronic obstructive pulmonary disease. Respir Res. 2013;14(1):24. doi:10.1186/1465-9921-14-24
11. Smith BM, Jensen D, Brosseau M, Benedetti A, Coxson HO, Bourbeau J. Impact of pulmonary emphysema on exercise capacity and its physiological determinants in chronic obstructive pulmonary disease. Sci Rep. 2018;8(1). doi:10.1038/s41598-018-34014-5
12. Garudadri S, Woodruff PG, Han MLK, et al. Systemic markers of inflammation in smokers with symptoms despite preserved spirometry in SPIROMICS. Chest. 2019;155(5):908–917. doi:10.1016/j.chest.2018.12.022
13. Souza JRM, Oliveira RT, Blotta MHSL, Coelho OR. Níveis séricos de interleucina-6 (IL-6), interleucina-18 (IL-18) e proteína C reativa (PCR) na síndrome coronariana aguda sem supradesnivelamento do ST em pacientes com diabete tipo 2. Arq Bras Cardiol. 2008;90(2):94–99. doi:10.1590/S0066-782X2008000200004
14. Shapiro SD. Evolving concepts in the pathogenesis of chronic obstructive pulmonary disease. Clin Chest Med. 2000;21(4):621–632. doi:10.1016/S0272-5231(05)70172-6
15. Barnes PJ, Shapiro SD, Pauwels RA. Chronic obstructive pulmonary disease: molecular and cellular mechanisms. Eur Respir J. 2003;22(4):672–688. doi:10.1183/09031936.03.00040703
16. Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. doi:10.1056/nejmoa0909883
17. Menezes AMB, Jardim JR, Pérez-Padilla R, et al. Prevalence of chronic obstructive pulmonary disease and associated factors: the PLATINO Study in São Paulo, Brazil. Cad Saude Publica. 2005;21(5). doi:10.1590/S0102-311X2005000500030
18. Faganello MM, Tanni SE, Sanchez FF, Pelegrino NRG, Lucheta PA, Godoy I. BODE index and GOLD staging as predictors of 1-year exacerbation risk in chronic obstructive pulmonary disease. Am J Med Sci. 2010;339(1):10–14. doi:10.1097/MAJ.0b013e3181bb8111
19. Ferrari R, Tanni SE, Faganello MM, Caram LMO, Lucheta PA, Godoy I. Three-year follow-up study of respiratory and systemic manifestations of chronic obstructive pulmonary disease. Braz J Med Biol Res. 2011;44(1):46–52. doi:10.1590/S0100-879X2010007500150
20. Moreira GL, Manzano BM, Gazzotti MR, et al. PLATINO, estudo de seguimento de nove anos sobre DPOC na cidade de São Paulo: o problema do subdiagnóstico. J Bras Pneumol. 2014;40(1):30–37. doi:10.1590/S1806-37132014000100005
21. Tanni SE, Zamuner ATS, Coelho LS, Vale SA, Godoy I, Paiva SAR. Are metabolic syndrome and its components associated with 5-year mortality in chronic obstructive pulmonary disease patients? Metab Syndr Relat Disord. 2015;13(1):52–54. doi:10.1089/met.2014.0100
22. Prudente R, Franco EAT, Mesquita CB, Ferrari R, De godoy I, Tanni SE. Predictors of mortality in patients with COPD after 9 years. Int J COPD. 2018;13:3389–3398. doi:10.2147/COPD.S174665
23. Marchioro J, Gazzotti MR, Moreira GL, et al. Anthropometric status of individuals with COPD in the city of São Paulo, Brazil, over time-analysis of a population-based study. J Bras Pneumol. 2019;45(6). doi:10.1590/1806-3713/e20170157
24. Prudente R, Ferrari R, Mesquita CB, et al. Peripheral blood eosinophils and nine years mortality in COPD patients. Int J COPD. 2021;16:979–985. doi:10.2147/COPD.S265275
25. Wei J, Xiong XF, Lin YH, Zheng BX, Cheng DY. Association between serum interleukin-6 concentrations and chronic obstructive pulmonary disease: a systematic review and meta-analysis. PeerJ. 2015;2015(8):e1199. doi:10.7717/peerj.1199
26. Garcia-Rio F, Miravitlles M, Soriano JB, et al. Systemic inflammation in chronic obstructive pulmonary disease: a population-based study. Respir Res. 2010;11(1):1–5. doi:10.1186/1465-9921-11-63
27. Jakeways N, McKeever T, Lewis SA, Weiss ST, Britton J. Relationship between FEV1 reduction and respiratory symptoms in the general population. Eur Respir J. 2003;21(4):658–663. doi:10.1183/09031936.03.00069603
28. Tantucci C, Modina D. Lung function decline in COPD. Int J COPD. 2012;(7):95. doi:10.2147/COPD.S27480
29. Mehrotra N, Freire AX, Bauer DC, et al. Predictors of mortality in elderly subjects with obstructive airway disease: the PILE Score. Ann Epidemiol. 2010;20(3):223–232. doi:10.1016/j.annepidem.2009.11.005
30. Celli BR, Locantore N, Yates J, et al. Inflammatory biomarkers improve clinical prediction of mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(10):1065–1072. doi:10.1164/rccm.201110-1792OC
31. Pinto-Plata V, Casanova C, Müllerova H, et al. Inflammatory and repair serum biomarker pattern. Association to clinical outcomes in COPD. Respir Res. 2012;13(1):71. doi:10.1186/1465-9921-13-71
32. Fermont JM, Masconi KL, Jensen MT, et al. Biomarkers and clinical outcomes in COPD: a systematic review and meta-analysis. Thorax. 2019;74(5):439–446. doi:10.1136/thoraxjnl-2018-211855
33. Nunes LN, Klück MM, Fachel JMG. Multiple imputations for missing data: a simulation with epidemiological data. Cad Saude Publica. 2009;25(2):268–278. doi:10.1590/s0102-311x2009000200005
34. Khan NA, Daga MK, Ahmad I, et al. Evaluation of BODE index and its relationship with systemic inflammation mediated by proinflammatory biomarkers in patients with COPD. J Inflamm Res. 2016;9:187–198. doi:10.2147/JIR.S108783
35. Sørensen AK, Holmgaard DB, Mygind LH, Johansen J, Pedersen C. Neutrophil-to-lymphocyte ratio, calprotectin and YKL-40 in patients with chronic obstructive pulmonary disease: correlations and 5-year mortality - A cohort study. J Inflamm. 2015;12(1):1–2. doi:10.1186/s12950-015-0064-5
36. Acanfora D, Scicchitano P, Carone M, et al. Relative lymphocyte count as an indicator of 3-year mortality in elderly people with severe COPD. BMC Pulm Med. 2018;18(1):1–8. doi:10.1186/s12890-018-0685-6
37. Xiong W, Xu M, Zhao Y, Wu X, Pudasaini B, Liu JM. Can we predict the prognosis of COPD with a routine blood test? Int J COPD. 2017;12:615–625. doi:10.2147/COPD.S124041
38. Lee H, Um SJ, Kim YS, et al. Association of the neutrophil-to-lymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016;11(6):e0156511. doi:10.1371/journal.pone.0156511
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
