Back to Journals » Journal of Inflammation Research » Volume 16
New Inflammatory Marker Associated with Disease Activity in Gouty Arthritis: The Systemic Inflammatory Response Index
Authors Jiang Y, Tu X , Liao X, He Y, Wang S, Zhang Q, Qing Y
Received 17 September 2023
Accepted for publication 17 November 2023
Published 24 November 2023 Volume 2023:16 Pages 5565—5573
DOI https://doi.org/10.2147/JIR.S432898
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Yi Jiang,1,2,* Xin Tu,1,3,* Xia Liao,1,2,* Yixi He,1,2 Shunbing Wang,1,2 Quanbo Zhang,1,3 Yufeng Qing1,2
1Research Center of Hyperuricemia and Gout, Affiliated Hospital of North Sichuan Medical College, Nanchong, 637000, People’s Republic of China; 2Department of Rheumatology and Immunology, Affiliated Hospital of North Sichuan Medical College, Nanchong, 637000, People’s Republic of China; 3Department of Geriatrics, Affiliated Hospital of North Sichuan Medical College, Nanchong, 637000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Quanbo Zhang; Yufeng Qing, Research Center of Hyperuricemia and Gout, Affiliated Hospital of North Sichuan Medical College, Nanchong, 637000, People’s Republic of China, Tel/Fax +86 08172282131, Email [email protected]; [email protected]
Background: The systemic immune-inflammatory index (SII) and systemic inflammatory response index (SIRI), as novel non-specific inflammatory markers, have recently drawn attention. At present, no studies have been conducted to investigate the value of SII and SIRI in gouty arthritis (GA), so we explored their possible association with GA disease activity.
Methods: The study enrolled 474 patients with acute gouty arthritis (AG), 399 patients with intercritical gouty arthritis (IG) and 194 healthy controls (HC). The differences in Monocyte-to-lymphocyte ratio (MLR), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), SII, and SIRI levels among different groups were assessed. The changes in the above indicators before and after treatment in the AG and IG groups were evaluated. Multivariate logistic regression analysis was assessed influencing factors for the acute gout attack. ROC curves were plotted to evaluate their diagnostic value for AG.
Results: Compared with the IG group, the erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), PLR, and incidence of hyperlipidemia in the AG group were significantly higher, and the duration of disease was significantly shorter (P < 0.05). The MLR, NLR, SII and SIRI in the AG group were significantly higher than those in the IG and HC groups (P < 0.05). Compared with baseline, decreased MLR, NLR, PLR, SII and SIRI were observed in the AG group after treatment (P < 0.05), while there was no significant difference in the IG group before and after treatment (P > 0.05). SIRI was positively correlated with ESR and CRP (P < 0.05). Multivariate logistic regression analysis result showed that duration of disease, hyperlipidemia, ESR, CRP, and SIRI were influencing factors of acute gout attack (P < 0.05). The AUC of ESR, CRP and SIRI on the diagnosis in AG were 0.664, 0.755, and 0.674, respectively.
Conclusion: SIRI may be used as a new inflammatory marker of disease activity with gouty arthritis.
Keywords: systemic inflammatory response index, complete blood cell count, gouty arthritis, inflammatory marker
Introduction
Gouty arthritis (GA) is an autoinflammatory disease caused by the deposition of MSU crystals in joints and surrounding tissues.1 The clinical symptoms of acute gouty arthritis are abrupt, characterized by redness, swelling, heat, pain, and dysfunction of the affected joint and surrounding tissues.2 Without clinical intervention, repeated attacks of acute gout inflammation can lead to progressive destruction of joint tissues, bone erosion, and cartilage damage, ultimately evolving into chronic gouty inflammation. Many inflammatory factors are involved in the gouty inflammatory response induced by MSU crystals, such as IL-1β, IL-6, TNF-α, and other cytokines, which are crucial in the inflammatory cascade amplification reaction.3 However, serum inflammatory factors such as IL-1β and IL-6 are rarely used as clinical routine testing indicators due to the high cost. Currently, two nonspecific inflammatory biomarkers, Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), are often used to detect disease activity in gouty arthritis. However, they have complex measurements and limited clinical application and still have certain limitations in evaluating gout disease activity. For example, some patients with low disease activity are often overlooked because ESR and CRP are at cutoff thresholds, and the above inflammatory indicators may be significantly increased in some patients with intercritical gout. Therefore, more inflammatory markers related to disease activity need to be identified.
Complete blood cell count ratio is a novel non-specific inflammatory indicator, including monocyte-to-lymphocyte ratio (MLR), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), systemic immune-inflammatory index (SII) and systemic inflammatory response index (SIRI). These indicators better reflect systemic inflammation and are readily available and inexpensive. They have been used to evaluate the degree of inflammation and efficacy prognosis in rheumatic diseases such as rheumatoid arthritis, ankylosing spondylitis, and systemic lupus erythematosus.4–7 Previous studies have shown that the MLR and NLR are higher in patients with GA than healthy controls and maybe a strong predictive marker for a gout attack.8 However, SII and SIRI have never been investigated in patients with GA. This shall be the first study to be conducted in GA. Therefore, this study aimed to investigate the correlation of SII and SIRI with gout activity.
Materials and Methods
Research Object
The retrospective study was carried out at the Affiliated Hospital of North Sichuan Medical College from March 2018 to May 2023. Eight hundred and seventy-three consecutive male patients with primary gout were enrolled in the study. The classification of gout follows the 2015 ACR/European League Against Rheumatism (EULAR) gout classification criteria. Gout patients were subdivided into acute gout (AG) group (n=474) and intercritical gout (IG) group (n=399) based on whether patients presented with gout flares or not. All gout patients had no history of secondary gout, malignant tumors, serious diseases of major organs, hematopathy, nephropathy, infection or other autoimmune diseases. After standard treatment, 172 patients with AG and 157 patients with IG, respectively, were included in the study. Healthy controls (HC, 194 age-matched men) with no hyperuricemia, metabolic syndrome, and other chronic diseases were recruited from the Physical Examination Center of the Affiliated Hospital of North Sichuan Medical College. The study was approved by the Ethics Committee of the North Sichuan Medical College and was consistent with the principles of the Declaration of Helsinki. All participants gave informed consent.
Research Methods
Age, sex, body mass index (BMI), and pre- and post-treatment laboratory indicators were recorded for enrolled patients. The laboratory indicators included ESR, CRP, white blood cell count (WBC), neutrophil granule count (GR), lymphocyte count (LY), monocyte count (Mo), platelet count (PLT), serum uric acid (sUA) level, and creatinine. All measurements were carried out by the Clinical Laboratory Department of the Affiliated Hospital of North Sichuan Medical College. The MLR is obtained by calculating MO/LY; The NLR is obtained by calculating GR/LY; The PLR is obtained by calculating PLT/LY; The SII is obtained by calculating (GR*PLT)/LY; The SIRI is obtained by calculating (GR*MO)/LY.
Statistical Analysis
All analyses were performed using SPSS 26.0. Quantitative data demonstrating approximately normal distributions were expressed as the mean ± SD and were statistically analyzed by t-test or one-way ANOVA. Quantitative data exhibiting nonnormal distributions were expressed as the median (interquartile range) and were statistically analyzed by Mann–Whitney U-test or Kruskal–Wallis H-test. Multiple or pairwise comparisons were performed using the LSD-t or Mann–Whitney U-tests. Counting data were expressed as a percentage (%) and were statistically analyzed by Chi-squared test. Spearman correlation analysis was used to assess the correlations between disease activity markers and MLR, NLR, PLR, SII, or SIRI. The influencing factors of acute gout attack were analyzed by multivariate logistic regression analysis. Receiver Operating Characteristic (ROC) curves were used to evaluate the diagnostic value of the above variables for AG. The level of significance was set at a two-sided P value of less than 0.05.
Results
Clinical Data and Laboratory Indicators
The general data and clinical characteristics of participants are shown in Table 1 and Figure 1. No significant among‐group differences were observed in age composition (P > 0.05). The duration of disease in the AG group was significantly shorter than that in the IG group, and the incidence of hyperlipidemia in the AG group was significantly higher than in the IG group (P < 0.05). Compared with the HC group: the WBC, GR, MO, PLT, MLR, NLR, SII, SIRI, sUA, and Creatinine of the AG group were significantly higher than the HC group; the WBC, GR, LY, MO, MLR, NLR, SII, SIRI, sUA, and Creatinine of the IG group were higher than the values of the HC group (P < 0.05). Compared with the IG group, the ESR, CRP, WBC, GR, MO, MLR, NLR, PLR, SII, and SIRI were higher in the AG group (P < 0.05).
 |
Table 1 Baseline Clinical Data and Laboratory Indicators |
Changes in MLR, NLR, PLR, SII, and SIRI Before and After Treatment
We evaluated differences in NLR, PLR, MLR, SII and SIRI levels between the AG and IG groups before and after treatment. The MLR, NLR, PLR, SII and SIRI were significantly reduced in the AG group after treatment compared with baseline (P < 0.05), while there was no significant difference between the before and after treatment in the IG group (P > 0.05), as given in Table 2 and Figure 2.
 |
Table 2 Changes in MLR, NLR, PLR, SII, and SIRI Before and After Treatment in the AG and IG Groups |
Correlation Analysis of MLR, NLR, PLR, SII, and SIRI with Disease Activity Markers in Patients with Gouty Arthritis
ESR and CRP, as inflammatory indicators, are important experimental indexes for evaluating the disease activity of gouty arthritis. Spearman correlation analysis showed that MLR, NLR, PLR, SII and SIRI showed a statistically significant positive correlation with ESR and CRP (P < 0.05), as given in Table 3.
 |
Table 3 Correlation Analysis of MLR, NLR, PLR, SII, and SIRI with Disease Activity Markers in Patients with Gouty Arthritis |
Multivariate Logistic Regression Analysis of Acute Gout Attack in Patients with Gouty Arthritis
The significant indicators (Duration of disease, Hyperlipidemia, ESR, CRP, WBC, GR, LY, MO, PLT, MLR, NLR, PLR, SII, SIRI, sUA and Creatinine) shown in Table 1 were used as independent variable, and the presence or absence of acute gout attack was used as the dependent variable for multivariate logistic regression analysis. The result showed that Duration of disease, Hyperlipidemia, ESR, CRP, and SIRI were influencing factors of acute gout attack (P < 0.05), as given in Table 4.
 |
Table 4 Multivariate Logistic Regression Analysis of Acute Gout Attack in Patients with Gouty Arthritis |
Evaluation of the Diagnostic Efficacy of MLR, NLR, PLR, SII and SIRI for AG Using ROC Curves
ROC curves were plotted to assess the efficiency of MLR, NLR, PLR, SII and SIRI in distinguishing AG patients from IG patients. The AUC of ESR, CRP and SIRI were 0.664 (95% CI: 0.628–0.699), 0.755 (95% CI: 0.724–0.787), and 0.674 (95% CI: 0.639–0.709), respectively. SIRI was found to be superior in diagnosing AG than ESR. At the cutoff value of 1.226, the sensitivity and specificity for the diagnosis of AG were 50.6% and 77.7%, respectively, as given in Table 5 and Figure 3.
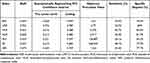 |
Table 5 Evaluation of the Diagnostic Efficacy of MLR, NLR, PLR, SII and SIRI for AG Using ROC Curves |
Discussion
Gouty arthritis, as an autoinflammatory disease, is caused by MSU crystals directly or indirectly triggering cell necrosis and inflammatory reaction.9 MSU crystals released by damaged cells or tissues can be recognized as damage-associated molecular patterns by pattern recognition receptors of innate immune cells, thereby generating immune responses in the initial stage, stimulating the secretion of many pro-inflammatory cytokines, and activating and initiating adaptive immune responses.10 Innate and adaptive immune cells, such as neutrophils, monocytes, lymphocytes, platelets, and pro-inflammatory mediators, play a critical role in the pathogenesis of gouty arthritis. Various inflammatory cells and cytokines synergize and induce the process of gout inflammation occurrence, development and prognosis.11 Therefore, testing various inflammatory indicators and their changes to determine the degree of inflammatory reaction is of great significance for understanding the occurrence and development of patients’ condition.
Inflammation leads to increased neutrophil, monocyte, platelet counts, and decreased lymphopenia counts, making their ratio an essential tool for indirectly evaluating inflammatory status and cell-mediated immunity. Many studies have shown that complete blood cell count and the ratio between them are widely used as markers to evaluate the prognosis, status and progression of inflammatory diseases. For example, NLR and PLR can be used to assess the activity of systemic lupus erythematosus, and MLR and NLR may be useful biomarkers in predicting lupus nephritis.12,13 In addition, NLR and PLR are valuable for evaluating disease activity and the therapeutic efficacy of rheumatoid arthritis.14 SII combined with ferritin proved to be the most powerful assessment tool for diagnosing adult Still’s disease.15 In previous studies, GA patients showed significantly higher MLR and NLR compared with controls, and AG group had higher MLR and NLR than the IG group, which agrees with the finding in the present study.8 Furthermore, our research found that SII and SIRI in the AG and IG groups were significantly higher than in the HC group. In addition, SII and SIRI in the AG group were higher than in the IG group. Moreover, the MLR, NLR, PLR, SII and SIRI in the AG group were significantly decreased after treatment compared with baseline, while the above indicators in the IG group showed no significant difference before and after treatment. To the best of our knowledge, our study is the first to report the levels of SII and SIRI in patients with GA.
The interaction between monocyte/macrophage and MSU crystals is the main link in acute gout attack.16 MSU crystals first react directly with synovial cells and monocyte/macrophage, causing increased monocyte activity, neutrophil chemotactic response and an explosive cascade expansion reaction.17 In the initial stage of inflammation, neutrophils engulf MSU crystals and produce ROS through the NADPH enzyme and release multiple neutrophil chemoattractants. Many recruited and activated neutrophils promote the release of massive inflammatory mediators and exacerbate the joint inflammatory response. Neutrophils can also increase blood viscosity by enhancing the interaction between platelets and endothelium, resulting in a hypercoagulable state.18 Platelets adhere to endothelial cells and increase inflammation by leading white blood cells to migrate to the area and adhere.19 In systemic inflammation, an increase in neutrophil count is accompanied by a corresponding decrease in lymphocyte count.20 Low lymphocyte counts have been reported in GA patients and play an essential role in the resolution and repair of inflammation.8 The above mechanisms may explain the association of various inflammatory markers developed based on complete blood cell count with gouty arthritis. Of note, our study observed no differences in lymphocyte counts between GA patients and HC group. Therefore, due to the simplicity of the structure, inflammatory markers of a single-cell subtype may not be sufficient to reflect the complexity and severity of immune-inflammatory states. The index and ratio obtained by combined multiple cell counts may be more reliable inflammatory markers, with advantages such as convenient detection, strong repeatability, and economy. Based on the integration of neutrophils, lymphocytes and monocytes, SIRI can reflect the state of three inflammatory cells simultaneously, which more comprehensively reflects the inflammatory state and immune balance of the body than MLR, NLR or PLR alone.21 It is considered to be a new inflammatory index superior to MLR and NLR.22 High SIRI status reflects strong pro-inflammatory reactions mediated by monocytes and neutrophils and weak or suppressed lymphocyte-mediated anti-inflammatory reactions, which may aggravate the pathophysiological process of gouty arthritis and induce the occurrence of acute gout.23 One of the most critical differences between SIRI and SII is that SIRI uses Monocyte counts, whereas SII uses platelets. Since monocytes play an important role in the mechanism of acute gout inflammation, this may lead to significant differences in the results obtained. For example, SII is not an influencing factor of acute gout attack and is less valuable for the diagnosis of AG than SIRI. In this study, SIRI showed a statistically significant positive correlation with ESR and CRP in patients with gouty arthritis. Multivariate logistic regression analysis result indicated that the duration of disease, hyperlipidemia, ESR, CRP, and SIRI were all influencing factors of acute gout attack. Additionally, ROC curve analysis showed that CRP remains a high Sensitivity and specificity indicator in assessing gout disease activity. Compared with ESR, SIRI had the more effective value in diagnosing AG.
However, our study has some limitations. First, all enrolled patients were from a single centre; Second, the sample size in our study was modest. Therefore, multi-centre clinical trials with larger sample sizes are necessary to confirm our conclusions.
Conclusion
In conclusion, this study is the first to evaluate the association between gouty arthritis and SIRI, and the obtained results suggest that the SIRI can serve as a new index capable of assessing disease activity.
Acknowledgments
Yi Jiang, Xin Tu, and Xia Liao are co-first authors for this study. This work was supported by funding from the National Natural Science Foundation of China (81974250); Science and Technology Project of Nanchong City (20SXCXTD0002, 20SXQT0308). The study was approved (NO: [2023]024) by the Ethics Committee of the Northern Sichuan Medical College and was conducted in accordance with the ethical norms of the 1975 Helsinki Declaration.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dalbeth N, Gosling AL, Gaffo A, et al. Gout. Lancet. 2021;397(10287):1843–1855. doi:10.1016/S0140-6736(21)00569-9
2. Singh JA, Gaffo A. Gout epidemiology and comorbidities. Semin Arthritis Rheum. 2020;50(3S):S11–S16. doi:10.1016/j.semarthrit.2020.04.008
3. Wu M, Tian Y, Wang Q, et al. Gout: a disease involved with complicated immunoinflammatory responses: a narrative review. Clin Rheumatol. 2020;39(10):2849–2859. doi:10.1007/s10067-020-05090-8
4. Xu Y, He H, Zang Y, et al. Systemic inflammation response index (SIRI) as a novel biomarker in patients with rheumatoid arthritis: a multi-center retrospective study. Clin Rheumatol. 2022;41(7):1989–2000. doi:10.1007/s10067-022-06122-1
5. Zinellu A, Mangoni AA. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio and disease activity in rheumatoid arthritis: a systematic review and meta-analysis. Eur J Clin Invest. 2023;53(2):e13877. doi:10.1111/eci.13877
6. Al-Osami MH, Awadh NI, Khalid KB, et al. Neutrophil/lymphocyte and platelet/lymphocyte ratios as potential markers of disease activity in patients with Ankylosing spondylitis: a case-control study. Adv Rheumatol. 2020;60(1):13. doi:10.1186/s42358-020-0113-5
7. Qin B, Ma N, Tang Q, et al. Neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) were useful markers in assessment of inflammatory response and disease activity in SLE patients. Mod Rheumatol. 2016;26(3):372–376. doi:10.3109/14397595.2015.1091136
8. Kadiyoran C, Zengin O, Cizmecioglu HA, et al. Monocyte to lymphocyte ratio, neutrophil to lymphocyte ratio, and red cell distribution width are the associates with gouty arthritis. Acta Medica. 2019;62(3):99–104. doi:10.14712/18059694.2019.132
9. Desai J, Steiger S, Anders HJ. Molecular Pathophysiology of Gout. Trends Mol Med. 2017;23(8):756–768. doi:10.1016/j.molmed.2017.06.005
10. Rose DM, Liu-Bryan R. Innate immunity in triggering and resolution of acute gouty inflammation. Curr Rheumatol Rep. 2006;8(3):209–214. doi:10.1007/s11926-996-0027-1
11. Chen J, Wu M, Yang J, et al. The immunological basis in the pathogenesis of gout. Iran J Immunol. 2017;14(2):90–98.
12. Wu Y, Chen Y, Yang X, et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were associated with disease activity in patients with systemic lupus erythematosus. Int Immunopharmacol. 2016;36:94–99. doi:10.1016/j.intimp.2016.04.006
13. Liu P, Li P, Peng Z, et al. Predictive value of the neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-neutrophil ratio, and neutrophil-to-monocyte ratio in lupus nephritis. Lupus. 2020;29(9):1031–1039. doi:10.1177/0961203320929753
14. Sargin G, Senturk T, Yavasoglu I, et al. Relationship between neutrophil-lymphocyte, platelet-lymphocyte ratio and disease activity in rheumatoid arthritis treated with rituximab. Int J Rheum Dis. 2018;21(12):2122–2127. doi:10.1111/1756-185X.13400
15. Kim JW, Jung JY, Suh CH, et al. Systemic immune-inflammation index combined with ferritin can serve as a reliable assessment score for adult-onset Still’s disease. Clin Rheumatol. 2021;40(2):661–668. doi:10.1007/s10067-020-05266-2
16. Galozzi P, Bindoli S, Doria A, et al. Autoinflammatory features in gouty arthritis. J Clin Med. 2021;10(9):1880. doi:10.3390/jcm10091880
17. So AK, Martinon F. Inflammation in gout: mechanisms and therapeutic targets. Nat Rev Rheumatol. 2017;13(11):639–647. doi:10.1038/nrrheum.2017.155
18. Li X, Ji Y, Kang J, et al. Association between blood neutrophil-to-lymphocyte ratio and severity of coronary artery disease: evidence from 17 observational studies involving 7017 cases. Medicine. 2018;97(39):e12432. doi:10.1097/MD.0000000000012432
19. Cure MC, Cure E, Kirbas A, et al. The effects of Gilbert’s syndrome on the mean platelet volume and other hematological parameters. Blood Coagul Fibrinolysis. 2013;24(5):484–488. doi:10.1097/MBC.0b013e32835e4230
20. Karhade AV, Shah KC, Shah AA, et al. Neutrophil to lymphocyte ratio and mortality in spinal epidural abscess. Spine J. 2019;19(7):1180–1185. doi:10.1016/j.spinee.2019.02.005
21. Li J, Yuan Y, Liao X, et al. Prognostic significance of admission systemic inflammation response index in patients with spontaneous intracerebral hemorrhage: a propensity score matching analysis. Front Neurol. 2021;12:718032. doi:10.3389/fneur.2021.718032
22. Zhang Y, Xing Z, Zhou K, et al. The predictive role of Systemic Inflammation Response Index (SIRI) in the prognosis of stroke patients. Clin Interv Aging. 2021;16:1997–2007. doi:10.2147/CIA.S339221
23. Geng Y, Zhu D, Wu C, et al. A novel systemic inflammation response index (SIRI) for predicting postoperative survival of patients with esophageal squamous cell carcinoma. Int Immunopharmacol. 2018;65:503–510. doi:10.1016/j.intimp.2018.10.002
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



