Back to Journals » International Journal of General Medicine » Volume 16
Negative Pressure Pneumomediastinum: A Novel Concept of Spontaneous Pneumomediastinum Without Mediastinal Widening Following Weight Loss
Authors Hagiwara H , Kinno Y, Ikegami T
Received 18 December 2022
Accepted for publication 25 March 2023
Published 6 April 2023 Volume 2023:16 Pages 1227—1236
DOI https://doi.org/10.2147/IJGM.S400060
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Luca Testarelli
Hiroaki Hagiwara,1 Yoshinori Kinno,1 Tadashi Ikegami2
1Department of Radiology, Yokohama Minamikyosai Hospital, Yokohama, Japan; 2Department of Diagnostic Imaging, Kanagawa Dental University, Yokosuka, Japan
Correspondence: Hiroaki Hagiwara, Department of Radiology, Yokohama Minamikyosai Hospital, 1-21-1 Mutsuura-higashi Kanazawa-ku, Yokohama, 236-0037, Japan, Tel +81-45-782-2101, Fax +81-45-701-9159, Email [email protected]
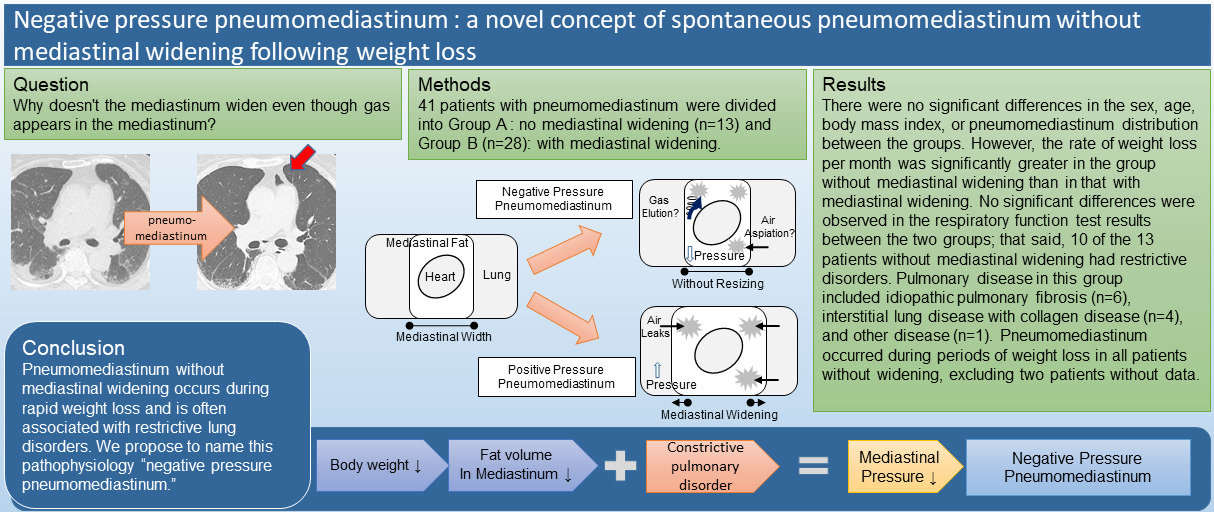
Purpose: Spontaneous pneumomediastinum, supposedly attributed to air leakage from the respiratory tract, is a common complication of interstitial lung disease often resulting in mediastinal widening. However, several cases of pneumomediastinum without mediastinal widening have been observed. This study aimed to investigate the cause of pneumomediastinum in patients without mediastinal widening.
Patients and Methods: This study included 41 patients diagnosed with pneumomediastinum using computed tomography (CT) between July 2011 and September 2021 at Yokohama Minamikyosai Hospital; patients had undergone previous CT showing no gas density. Based on a comparison with previous CT images, the patients were classified into two groups: without mediastinal widening and with mediastinal widening.
Results: Of the 41 patients, 13 and 28 had pneumomediastinum without and with mediastinal widening, respectively. There were no significant differences in the sex, age, body mass index, or pneumomediastinum distribution between the groups. However, the rate of weight loss per month was significantly greater in the group without mediastinal widening than in that with mediastinal widening. No significant differences were observed in the respiratory function test results between the two groups; that said, 10 of the 13 patients without mediastinal widening had restrictive disorders. Pulmonary disease in this group included idiopathic pulmonary fibrosis (n = 6), interstitial lung disease with collagen disease (n = 4), and other disease (n = 1). Pneumomediastinum occurred during periods of weight loss in all patients without widening, excluding two patients without data.
Conclusion: Pneumomediastinum without mediastinal widening occurs during rapid weight loss and is often associated with restrictive lung disorders. The negative pressure attributed to the decreased plasticity of the lungs, which complements the space where the mediastinal fat has disappeared, is presumably the cause of pneumomediastinum. This pathophysiology is different from that of conventional pneumomediastinum attributed to increased intrapleural space pressure; thus, we propose to name the abovementioned pathophysiology “negative pressure pneumomediastinum”.
Keywords: interstitial lung disease, idiopathic lung fibrosis, restrictive lung disorder
Graphical Abstract:
Introduction
Pneumomediastinum (PM), which is a clinical condition indicated by the presence of gas in the mediastinum, is classified into spontaneous pneumomediastinum (SPM) and secondary PM according to the underlying etiology.1 The pathophysiology of SPM is inferred based on a three-step process that identifies alveolar ruptures, air dissection along bronchovascular sheaths, and the spreading of pulmonary interstitial emphysema into the mediastinum.2 Current studies have not found conclusive evidence concerning the cause of SPM.3 The causes of secondary PM include esophageal injury, tracheal or bronchial injury related to trauma or of iatrogenic origin, and aerogenic infection.
SPM is a well-known complication of various respiratory diseases, including interstitial lung disease (ILD). In some cases, upon the progression of respiratory failure, mediastinal enlargement results from air leaks owing to an increase in the intrapleural pressure and is often associated with pneumothorax. However, a case of a patient with ILD and PM without expansion of the mediastinal width has been reported previously.4 In this case, the mediastinal fat decreased as a result of weight loss, and gas density appeared to replace the space. We presume that there is a decrease in the mediastinal pressure given that the space left following mediastinal fat loss is not substituted by lung expansion owing to low compliance of the lung in patients with ILD. A decrease in the mediastinal pressure may result in the drawing of air from the airway or elution of nitrogen from the tissues, leading to a vacuum phenomenon (VP), in which gas accumulates in the joint spaces or intervertebral discs. No pneumothorax or subcutaneous emphysema was observed in these cases, as they were not caused by air leakage.
We propose that this new pathophysiology should be named “negative pressure PM”, the pathologic characteristic of which is the decrease in the mediastinal pressure. This is distinct from conventional PM, which results from air leakage due to an increase in intrapleural pressure. Thus, the purpose of this study was to further investigate negative pressure PM and elucidate its etiology and clinical presentation.
Materials and Methods
We reviewed a database of PM cases that were radiologically diagnosed on computed tomography (CT) images between July 2011 and September 2021 at Yokohama Minamikyosai Hospital. Of these, upon reviewing the images and clinical records, we excluded the patients without previously recorded CT studies for comparison of the mediastinum volume and those with iatrogenic or traumatic PM; thus, 41 patients were included in the study.
CT images were obtained using a multidetector-row CT scanner (Aquilion, Toshiba, Nasu Japan); images of the lung and mediastinal windows of 5-mm thickness were evaluated. We reviewed the images and identified PM and its distribution. In cases where the mediastinal contour in all the slices did not deviate outward when compared with that in previous CT images, no mediastinal enlargement was considered, and such cases were classified into group A. Other cases were classified into group B since the mediastinum was presumed to have widened. The sites of PM included the (1) anterior mediastinum, which was ventral to the anterior margin of the ascending aorta; (2) posterior mediastinum, which was posterior to the dorsal margin of the trachea; (3) middle mediastinum, which was between the anterior and posterior mediastinum; (4) superior mediastinum, which was cranial to the aortic arch; and (5) hilum, which was the part beyond the lateral side of the mediastinum. Emphysema extending to the cranial side rather than to the apex of the lung was considered subcutaneous emphysema not mediastinal emphysema. Pneumothorax and subcutaneous emphysema were recorded.
We established a diagnosis of respiratory disease based on the patient’s medical history. In order to estimate body weight loss, we used two measurements of body weight, one taken around the time of the present CT and another taken from a previous time point; thus, we calculated the rate of weight loss per month (RWL) using the following equation:
The presence or absence of chest pain and other symptoms was confirmed. We recorded the results of the respiratory function test performed at the time of the CT examination.
Statistical comparisons of age, body mass index (BMI), RWL, predicted vital capacity (%VC), and forced expiratory volume % in 1 s (FEV1.0%) were performed using paired-samples t-tests; sex, pneumothorax, and subcutaneous emphysema with chi-square tests; and the distribution of PM with a chi-square test for goodness-of-fit using SPSS v. 21.0 for Windows (IBM, Armonk, NY, USA). Statistical significance was set at p<0.05.
Results
Of the included 41 patients, 13 patients (9 men, 4 women) had no mediastinal widening (group A), and 28 patients (21 men, 7 women) had mediastinal widening in their CT images upon comparison with previous CT images (group B) (Table 1). The average age of the 13 patients in group A was 71.8 (range: 29–90) years, while that of the 28 patients in group B was 76.9 (range: 30–87) years. There were no significant differences in the sex or age of the two patient groups.
 |
Table 1 Patient Characteristics |
The average BMI of group A and B were not significantly different between the two groups. However, the average RWL was significantly greater in the group without mediastinal widening (group A) than it was in the group with mediastinal widening (group B) (p=0.037). There was no significant difference in the distribution of PM between the two groups.
Patients without mediastinal widening had no subcutaneous emphysema or pneumothorax, except for one patient (case 8).
The diagnoses of pulmonary disease in the 13 patients in group A included idiopathic pulmonary fibrosis (IPF; n = 6), ILD with collagen disease (n = 4), and other diseases (Table 2).
 |
Table 2 Patient Characteristics of the Group A with No Mediastinal Widening |
The diagnoses of pulmonary disease in the 28 patients in group B included idiopathic pulmonary fibrosis (IPF; n = 9), ILD with collagen disease (n = 10), and other diseases (Table 3).
 |
Table 3 Patient Characteristics of Group B with Mediastinal Widening |
Among the 13 patients in group A, except for two patients without data, the CT examination revealed gas densities in the mediastinum that corresponded to the time when they lost weight. No complaints of chest pain were noted, with the exception of one patient. The respiratory function test revealed a restrictive disorder with a %VC of <80% in the 13 patients in group A except in 3 patients with IPF, gastric cancer, and ulcerative colitis. There were no significant differences in the %VC and FEV1.0% between groups A and B.
Representative Cases
Case 1
Case 1 included a 75-year-old woman who was admitted to the hospital with a history of cough, dyspnea, and slight fever for 3 months. Her body temperature was 37.1°C, and a fine crackle was detected in the dorsum on auscultation. Chest CT revealed reticular opacities and consolidation, which suggested a nonspecific interstitial pneumonia pattern on the bases of both lungs (Figure 1A).
She was diagnosed with systemic lupus erythematosus with Sjogren syndrome based on the presence of facial eruptions for several years, intraoral drying, antinuclear antibodies identified by blood tests, high levels of CH50, and anti-ribonucleoprotein antibodies.
The patient was treated with prednisolone and mycophenolate mofetil. The dyspnea gradually improved. A CT scan performed 1 month later to evaluate the effect of nonspecific interstitial pneumonia treatment revealed PM (Figure 1B).
Case 4
Case 4 included an 89-year-old man with IPF. Lung fibrosis was identified by CT 1 year prior to presentation (Figure 2A). He was admitted to the hospital with a 1-week history of productive cough, dyspnea, and fever. His body temperature was 38.2°C, and a fine crackle was detected in the dorsum on auscultation. Chest CT revealed reticular opacities and honeycombing, suggesting a usual interstitial pneumonia pattern in both peripheral lungs, which were exacerbated relative to those noted during CT performed 1 year earlier (Figure 2B). PM appeared around the pulmonary artery; however, no enlargement of the mediastinum was observed. Subcutaneous fat was no longer visible on the CT images, consistent with his weight loss from 43.5 kg to 33.0 kg over the course of 1 year.
Discussion
SPM is presumably caused by the leakage of air from the respiratory tract. Our study aimed to elucidate the reason for the absence of expansion of the mediastinum in certain cases despite the additional volume of increased air.
SPM is a well-known complication of various ILDs, including IPF and connective tissue disorders,5–7 with increased intrapleural pressure owing to cough and constrained respiration, which are thought to produce alveolar rupture. One report suggested that corticosteroids, which are administered to treat primary disease, damage the interstitial tissues of the lungs,8 and that PM frequently occurs when the condition worsens if steroids and immunosuppressive drugs are not administered.9 These studies mainly focused on the clinical characteristics of lung diseases that result in air leaks. However, our study focused on the relative pressure of the mediastinum and not on the cause of the air leaks. We hypothesized that PM is caused by the pressure gradient between the intrapleural space and mediastinum (Figure 3). The pressure in the intrapleural space and mediastinum is balanced in the normal chest; however, when the intrapleural pressure rises, this balance is disrupted, resulting in a pressure gradient, and an air leak is produced to balance the pressure. This conventional PM is referred to as positive pressure PM because it is attributed to the positive pressure in the intrapleural space. Similarly, negative pressure PM occurs to eliminate the pressure differences during decreased mediastinal pressure.
The conditions involving decrease in the mediastinal pressure are very limited. In positive pressure PM, air leaks from the respiratory tract increase the mediastinal pressure and mediastinal widening (Figure 4). When body weight loss occurs and mediastinal fat is reduced in normal lungs, the capacity of the lungs is increased and the space is replaced resulting in narrowing of the mediastinum; thus, the pressure remains unaltered. However, in patients with restrictive lung disorders attributed to ILD, remodeling and replacement do not occur owing to the decreased plasticity of the lung. This reduces the mediastinal pressure and causes negative pressure PM without mediastinal resizing. The greater RWL in group A also supports this hypothesis.
There are two possible pathophysiological mechanisms for gas collection. One is by air leaks from the intrathoracic airway, similar to conventional SPM, and the other is by the VP. The VP is a pathological condition in which gas is retained in the synovial joints or intervertebral discs. The VP is most frequently associated with degenerative joint diseases but has also been associated with other pathologies, such as osteonecrosis and compression fracture; therefore, its etiology is still under deliberation.10–13 The gas within the intervertebral discs contains at least 90% nitrogen combined with oxygen, carbon dioxide, and other trace gases.14 Unlike oxygen, nitrogen collected in the dead space is not metabolized and is thus thought to accumulate in the tissue. The VP adequately explains the gas collection isolated from the airways and hilum.
All the cases of PM of unknown cause were previously classified as SPM. However, our results show evidence of the existence of negative pressure PM; therefore, we propose that SPM should be classified into the following two categories (Figure 5): positive pressure PM, which represents conventional SPM, and a new additional category of negative pressure PM. During lung disease treatment interventions, PM should be distinguished from positive pressure PM attributed to the exacerbation of lung disease and negative pressure PM attributed to weight loss.
This study has certain limitations. First, this was a retrospective study, and CT scans and body weight measurements were not performed simultaneously; thus, the precise RWL could not be calculated. However, these measurements allowed us to estimate the weight loss based on the decrease in the subcutaneous and mediastinal fat compared to that in the initial CT before gas density identification. Similarly, the respiratory function test did not reflect the respiratory function at the precise time of CT. Second, the presence or absence of mediastinal enlargement was manually judged by a radiologist; therefore, accurate classification was not possible in cases with a small amount of PM. Third, the sampling and component analysis of gas that accumulated in the mediastinum were not performed. These tests can be used to determine whether the accumulated gas originates from the respiratory tract or is caused by the VP.
Conclusion
In a certain number of cases of PM included in this study, the mediastinum was not enlarged. These cases were not caused by air leaks owing to an increase in the intrapleural pressure, but by a decrease in the mediastinal pressure owing to mediastinal fat volume loss combined with lung plasticity reduction in ILD. Given that the cause of PM is presumed to be associated with disruption of the relative pressure balance between the intrapleural space and mediastinum, SPM can be divided into positive pressure PM, which increases intrapleural space pressure, and negative pressure PM, which decreases mediastinal pressure.
Abbreviations
%VC, predicted vital capacity; CT, computed tomography; BMI, body mass index; FEV1.0%, forced expiratory volume % in 1 s; ILD, interstitial lung disease; IPF, idiopathic pulmonary fibrosis; PM, pneumomediastinum; RWL, rate of weight loss per month; SPM, spontaneous pneumomediastinum; VP, vacuum phenomenon.
Data Sharing Statement
All relevant data are available from the Open Science Framework (https://osf.io/https://osf.io/vzds9/).
Ethics Approval and Informed Consent
This study was approved by the institutional review board of Yokohama Minamikyosai Hospital (29-1-10) which waived the need for informed consent owing to the retrospective nature of the study; the information concerning the patients’ identities was kept confidential. The patient in representative case 1 was informed about the study and written consent was obtained for publication of case details and accompanying images. The patient in Case 4 died 7 years ago, and it was difficult to contact the bereaved relatives; therefore, documented informed consent for publication of case details and accompanying images was waived by the review board. The study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
We would like to thank Dr. T. Iwasawa for useful discussions. We would like to thank Editage for English language editing.
Author Contributions
All the authors made a significant contribution to the work reported. All the authors were involved in the conception, study design, execution, data acquisition, analysis and interpretation, took part in drafting, revising, and critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
The authors received no specific funding for this work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sahni S, Verma S, Grullon J, Esquire A, Patel P, Talwar A. Spontaneous pneumomediastinum: time for consensus. N Am J Med Sci. 2013;5(8):460–464. doi:10.4103/1947-2714.117296
2. Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine. 1944;23(4):281–358. doi:10.1097/00005792-194412000-00001
3. Al-Mufarrej F, Badar J, Gharagozloo F, Tempesta B, Strother E, Margolis M. Spontaneous pneumomediastinum: diagnostic and therapeutic interventions. J Cardiothorac Surg. 2008;3:59. doi:10.1186/1749-8090-3-59
4. Hagiwara H, Torii I. Mediastinal vacuum phenomenon: atypical pneumomediastinum caused by gas replacement of diminished fat. Int Med Case Rep J. 2015;8:283–286. doi:10.2147/IMCRJ.S93664
5. Fujiwara T. Pneumomediastinum in pulmonary fibrosis. Detection by computed tomography. Chest. 1993;104(1):44–46. doi:10.1378/chest.104.1.44
6. Kono H, Inokuma S, Nakayama H, Suzuki M. Pneumomediastinum in dermatomyositis: association with cutaneous vasculopathy. Ann Rheum Dis. 2000;59(5):372–376. doi:10.1136/ard.59.5.372
7. Franquet T, Giménez A, Torrubia S, Sabaté JM, Rodriguez-Arias JM. Spontaneous pneumothorax and pneumomediastinum in IPF. Eur Radiol. 2000;10(1):108–113. doi:10.1007/s003300050014
8. Yamanishi Y, Maeda H, Konishi F, et al. Dermatomyositis associated with rapidly progressive fatal interstitial pneumonitis and pneumomediastinum. Scand J Rheumatol. 1999;28(1):58–61. doi:10.1080/03009749950155805
9. Matsuoka S, Kurihara Y, Yagihashi K, Okamoto K, Niimi H, Nakajima Y. Thin-section CT assessment of spontaneous pneumomediastinum in interstitial lung disease: correlation with serial changes in lung parenchymal abnormalities. Respir Med. 2006;100(1):11–19. doi:10.1016/j.rmed.2005.04.016
10. Resnick D, Niwayama G, Guerra J, Vint V, Usselman J. Spinal vacuum phenomena: anatomical study and review. Radiology. 1981;139(2):341–348. doi:10.1148/radiology.139.2.7220878
11. Libicher M, Appelt A, Berger I, et al. The intravertebral vacuum phenomenon as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol. 2007;17(9):2248–2252. doi:10.1007/s00330-007-0684-0
12. Lafforgue P, Chagnaud C, Daumen-Legré V, Daver L, Kasbarian M, Acquaviva PC. The intravertebral vacuum phenomenon (‘vertebral osteonecrosis’). Migration of intradiscal gas in a fractured vertebral body? Spine. 1997;22(16):1885–1891. doi:10.1097/00007632-199708150-00015
13. Patten RM. Vacuum phenomenon: a potential pitfall in the interpretation of gradient-recalled-echo MR images of the shoulder. AJR Am J Roentgenol. 1994;162(6):1383–1386. doi:10.2214/ajr.162.6.8192004
14. Ford LT, Gilula LA, Murphy WA, Gado M. Analysis of gas in vacuum lumbar disc. AJR Am J Roentgenol. 1977;128(6):1056–1057. doi:10.2214/ajr.128.6.1056
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.