Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Neck Health Metrics and Quality of Life: A Comparative Study in Bike Drivers with and without Neck Pain
Authors Aafreen A , Khan AR , Khan A , Ahmad A , Alzahrani AH , Alhusayni AI, Alameer AH, Alajam RA, Mondey Ganesan BB, Shaphe MA
Received 30 August 2023
Accepted for publication 10 November 2023
Published 23 November 2023 Volume 2023:16 Pages 3575—3584
DOI https://doi.org/10.2147/JMDH.S437826
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Aafreen Aafreen,1 Abdur Raheem Khan,1 Ashfaque Khan,1 Ausaf Ahmad,2 Abdullah Hussain Alzahrani,3 Abdullah Ibrahim Alhusayni,3 Abdulaziz H Alameer,4 Ramzi Abdu Alajam,4 Bhuvanesh Babu Mondey Ganesan,4 Mohammad Abu Shaphe4
1Department of Physiotherapy, Integral University, Lucknow, India; 2Department of Community Medicine, Integral University, Lucknow, India; 3Department of Health Rehabilitation Sciences, College of Applied Medical Sciences, Shaqra University, Shaqra, Saudi Arabia; 4Department of Physical Therapy, College of Applied Medical Sciences, Jazan University, Jazan, Saudi Arabia
Correspondence: Abdur Raheem Khan, Department of Physiotherapy, Integral University, Lucknow, India, Tel +9616739965, Email [email protected]
Purpose: Neck pain is a prevalent musculoskeletal issue among bike drivers, often resulting from extended static postures, repetitive head movements, and exposure to vibrations. This study aims to assess the connection between cervical ROM, neck proprioception, CVA, and QOL in bike drivers with neck pain compared to those without neck pain so that the targeted interventions can be developed to enhance their well-being.
Methods: A cross-sectional study involving 100 bike drivers aged 20– 50 years was conducted, split into two groups: those with neck pain (n=50) and those without neck pain (n=50). Cervical ROM was measured using a smartphone, neck proprioception was assessed through a head repositioning test, and CVA was determined using lateral-view photographs with a plumb line. The Short Form-36 (SF-36) questionnaire was employed to evaluate QOL. Data analysis was conducted using independent t-tests and Pearson’s correlation coefficient.
Results: Bike drivers with neck pain exhibited significantly reduced cervical ROM (p-value=< 0.001), impaired neck proprioception (p-value=< 0.001), and decreased CVA (p-value=< 0.001) compared to their counterparts without neck pain. A strong negative correlation was found between neck pain and QOL, with lower scores in all eight domains of the SF-36. Cervical ROM, neck proprioception, and CVA showed moderate correlations with various QOL domains (p-value=< 0.05).
Conclusion: Neck pain in bike drivers is linked to decrease cervical ROM, compromised neck proprioception, and reduced CVA. These factors correlate with a lower quality of life, both physical and mental domains. Interventions addressing these aspects may enhance the quality of life for bike drivers experiencing neck pain.
Keywords: cervical range of motion, neck proprioception, craniovertebral angle, quality of life, neck pain, bike drivers
Introduction
Neck pain, a prevalent musculoskeletal issue among professionals whose jobs require extended periods of static postures, is particularly common among bike drivers.1 This condition in bike drivers is often a result of various occupational factors such as prolonged static postures, repetitive head movements, and continued exposure to whole-body vibrations.2 Notably, these factors influence the crucial aspects of neck health, namely the cervical range of motion (ROM), neck proprioception, and craniovertebral angle (CVA).3 Our study aims to quantify these effects and establish the extent to which they contribute to the incidence and severity of neck pain in bike drivers.
The cervical ROM is a measure of the flexibility and mobility of the neck, which is essential for performing daily tasks and activities. Any reduction in cervical ROM can lead to discomfort, limitations in activity, and may contribute to the development and persistence of neck pain.4 It is, therefore, necessary to assess cervical ROM in bike drivers, as it provides an insight into the physical capacity of the neck and the potential risk of neck-related issues.
Neck proprioception, another crucial aspect of neck health, refers to the body’s ability to perceive the position and movement of the neck.5 This sensory feedback mechanism is vital for maintaining balance, coordinating movements, and preventing injuries. Any impairment in neck proprioception can lead to a lack of precision in movements, increase the risk of injury, and exacerbate existing neck pain.6 Considering the demanding nature of bike driving, where precise head and neck movements are required, evaluating neck proprioception is of considerable importance.
The CVA, a measure of the alignment between the head and the neck, is another factor that is affected by the occupational demands of bike driving.7 It is an indicator of the posture of the head and neck, with a decrease in CVA often associated with a forward head posture, a common postural deviation seen in individuals with neck pain.8 This deviation not only increases the strain on the neck muscles but also leads to musculoskeletal pain and discomfort over time.9 Therefore, assessing CVA can offer valuable information about postural habits and their potential role in the development of neck pain.
The presence of neck pain and the associated limitations in physical activity can significantly impact the quality of life (QOL) of bike drivers.10 QOL, a comprehensive measure of an individual’s physical, psychological, and social well-being, tends to be lower in individuals experiencing chronic pain conditions.11 Chronic neck pain, for instance, can lead to functional impairments, reduced productivity, increased healthcare utilization, and psychological distress, all of which can severely compromise an individual’s QOL.12 As such, it is crucial to evaluate QOL in bike drivers with neck pain, to understand the broader impact of this condition on their overall well-being.
In light of the above, this study aims to provide a comprehensive assessment of the cervical ROM, neck proprioception, CVA, and QOL in bike drivers with neck pain as compared to those without neck pain. Our objective is to highlight not only the occupational risks but also the more comprehensive health and economic implications of neck pain among bike drivers, offering a foundation for subsequent interventions and policy-making.
In conclusion, neck pain in bike drivers is a complex issue that demands a holistic approach for its management. Through this study, we aim to shed light on the multifaceted nature of neck pain among bike riders, its occupational origins, and its pervasive effects on everyday life, thereby justifying the need for our focused research on this group. By examining the relationship between neck health metrics and QOL, this study hopes to contribute to a better understanding of this condition and pave the way for more effective strategies to improve the well-being of bike drivers.
Methods
Study Design and Participants
This study was a cross-sectional study conducted from September to December 2022, within the physiotherapy division of the Integral Hospital and Research Centre, a constituent of Integral University, located in Lucknow, Uttar Pradesh, India that aimed to investigate the relationship between neck pain and various factors such as cervical range of motion (ROM), neck proprioception, craniovertebral angle (CVA), and quality of life (QOL) in bike drivers. The Institutional Ethical Committee of Integral University, Lucknow, India provided the ethical authorization for this study (reference number: IEC/IIMSR/2022/70). The study was conducted in accordance with the 1964 Helsinki Declaration,13 and all participants provided written consent before taking part in the study.
To determine the appropriate sample size for our study, we conducted a power analysis using G*Power software (version 3.15). This analysis was grounded on the criteria of achieving a minimum acceptable intraclass correlation coefficient (ICC) of 0.60, with a power (1-β) set at 0.80 and an alpha level (α) of 0.05, considering a 95% confidence interval. The outcome of the power analysis suggested that a minimum of 90 participants was necessary to detect a statistically significant difference within our study parameters.
To enhance the robustness of our study and to mitigate the potential for type II errors, we elected to include 100 participants, and they were split evenly into two groups (group A and group B).
Group A consisted of 50 bike riders who had experienced non-specific neck pain for a minimum of three months, while Group B was made up of 50 generally healthy bike riders without neck pain in the previous 12 months.14 Both male and female riders were represented in each group. Participants had to be aged between 20 and 50 and ride bikes for a minimum of two hours daily to qualify for either group. Inclusion in Group A was possible regardless of prior professional treatment for neck pain, provided that the individual’s self-reported neck pain intensity, as rated on a 0–10 spinal numerical pain scale (0: no pain; 10: worst pain imaginable), did not increase by more than two points during data gathering.15
Measurement of Cervical Range of Motion
The range of motion (ROM) in the cervical region was evaluated using a smartphone that had a clinometer and compass application installed, following the technique suggested by Khan et al.16 This method offered an inventive and dependable way to quantify cervical ROM, guaranteeing the collection of precise data.
The smartphone app used to measure the cervical range of motion in the frontal and sagittal planes are Clinometer (Peter Breitling, Version 3.3, http://www.plaincode.com/products), an app designed using the three inbuilt accelerometers (LIS302DL accelerometer). This app uses the internal three-axis linear accelerometers to measure the direction of gravity’s pull. For this, the gyroscope stays in one position, regardless of orientation. When placed against a solid surface, the inclinometer compares the object’s angle to the gyroscope and displays the results using the software interface. The app used to measure the cervical range of motion in the horizontal plane was the compass, software that was already integrated with the smartphone. In order to locate the orientation of the smartphone, the app uses the built-in magnetometer, which senses its orientation relative to the Earth’s magnetic field using the Hall effect. The chip (AKM AK8975) senses the field in three directions and locates the magnetic field pointing north. It also uses the accelerometer that tracks the movement of the device to measure orientation changes. The magnetic north was chosen to obtain the results for this study.
Participants were instructed to execute a set of movements such as flexion, extension, and rotation of the neck. The angle of the neck during each motion was recorded by the smartphone application, providing an accurate assessment of cervical ROM. Each movement was trialed three times, and the mean value was used for analysis.16
Assessment of Neck Proprioception
The proprioception of the neck, essentially the awareness of joint positioning, was assessed using a head repositioning examination. For this assessment, participants were blindfolded and instructed to return their heads to a neutral stance following active cervical flexion, extension, and rotation. The disparity from the neutral stance was noted, giving a quantifiable measure of the participant’s neck proprioception.4 The CROM device was then set to zero. During the testing procedure, participants were directed to close their eyes while their heads were moved by the examiner to a target position, representing 50% of their maximum range of motion. They were asked to hold this position for five seconds and to memorize it. Afterwards, the examiner directed the participant to return their head to the position they remembered. The CJPE was assessed based on the degree of precision in head repositioning. Each cervical movement tested three times, and the mean of these movements was calculated for analysis.
Determination of Craniovertebral Angle
The craniovertebral angle (CVA) was gauged using Surgimap, specialized software for evaluating spinal alignment and posture. Participants were side-photographed in their natural stance, with Surgimap analyzing the cervical spine’s horizontal alignment, quantifying the craniovertebral angle (CVA). A smaller CVA implies a more pronounced forward head posture (FHP). An image of the sagittal plane for each subject was captured with objective access to the CVA, the digital camera was positioned at 1.5 m and fixed with a camera stand without any rotation or tilt. In order to standardize the subject’s head and neck position, the level of the camera was set to the height of the subject’s shoulder and the image obtained was analyzed using the Surgimap system software. If an individual’s CVA is less than 48◦, they are classified as having FHP, whereas a CVA greater than 48◦ indicates a normal craniovertebral posture. It has been stated that this procedure is very reliable (ICC = 0.88).17
Evaluation of Quality of Life
The Short Form-36 (SF-36) questionnaire was utilized to evaluate Quality of Life (QOL). The SF-36 is a commonly employed health survey that assesses how health influences a person’s daily activities. It has two important summary measures, namely, the Physical Component Score (PCS) and the Mental Component Score (MCS). The raw scores for each of the eight SF-36 dimensions, namely vitality (VT), physical functioning (PF), bodily pain (BP), general health perceptions (GH), role physical (RP), role emotional (RE), social functioning (SF), and mental health (MH), were obtained by totalling the item scores and transforming them into a range of 0 to 100.18
The Neck Disability Index (NDI) comprises 10 items, each with a maximum score of 5, resulting in a total score of 100 (50 × 2). A higher score indicates more significant neck disability as reported by the patients. Unless patients indicated that one or two items were not relevant to their situation, we calculated the instrument’s maximum potential score as 45, which we then converted to 100% and divided by 2. The minimum clinically meaningful difference ranged from 5% to 10% for each patient.19
Data Analysis
IBM SPSS Statistics software (version 26.0) was utilized for the statistical analysis. Descriptive statistics offered a summary of the data. Independent t-tests were employed to analyse the discrepancies between the two groups. The correlation between Neck Disability Index (NDI) and the evaluated variables (cervical ROM, neck proprioception, CVA, and QOL) was determined using Pearson’s correlation coefficient. To assess the relationship between the SF-36 questionnaire and NDI scores, correlation analysis (scatter diagram) was performed. Internal consistency reliability for multi-items sub-scales (taking at least three items) was evaluated using the coefficient of Cronbach’s alpha. Alpha coefficient ≥ 0.7 was considered acceptable. The significance threshold was established at a p-value ≤ 0.05.
Results
Table 1 provides an overview of the demographics for two separate groups: those experiencing neck pains (n=50) and those not experiencing neck pains (n=50). The information presented includes the average age, gender distribution, and the average length of time spent daily on bike riding for both groups.
 |
Table 1 Descriptive Statistics for Subjects Characteristics |
Table 2 details the statistical description of the cervical range of motion (ROM) for two distinct groups: those with neck pain and those without. The ROM metrics examined include flexion, extension, and both left and right rotations. These values are denoted as mean ± standard deviation (SD).
 |
Table 2 Descriptive Statistics for Cervical Range of Motion, Craniovertebral Angle, Neck Proprioception, Physical Functioning and General Health |
It was observed that the group with neck pain exhibited a significantly diminished cervical ROM across all metrics when compared to the group without neck pain. Particularly, the average flexion was lesser in the neck pain group (32.3° ± 5.6) than in the group without neck pain (45.2° ± 5.1). The t-test result (T-value = 12.04, p-value = < 0.001) confirms that this difference holds statistical significance.
Likewise, the neck pain group had less extension (35.2° ± 6.1) compared to the group without neck pain (48.5° ± 6.2). The t-test result further supports the statistical significance of this difference (T-value = 10.22, p-value =< 0.001).
In terms of rotation, the neck pain group exhibited significantly lesser left and right rotations than the group without neck pain. Specifically, for left rotation, the average ROM was 39.6° ± 7.8 in the neck pain group and 52.1° ± 7.6 in the group without neck pain (T-value = 8.09, p-value= < 0.001). For right rotation, the average ROM was 40.2° ± 7.3 in the neck pain group and 52.9° ± 7.1 in the group without neck pain (T-value = 8.42, p-value= < 0.001).
These findings demonstrate that individuals suffering from neck pain have a notably reduced cervical range of motion in flexion, extension, and both left and right rotations compared to individuals without neck pain.
Moreover, in observing the craniovertebral angle, the group with neck pain exhibited a notably smaller angle (48.5° ± 5.3) than the group without neck pain (54.6° ± 4.2, t=6.89, p-value=<0.001), suggesting a more compromised neck posture in the group suffering from neck pain.
Regarding neck proprioception, the group with neck pain showed significantly inferior proprioception (4.8° ± 1.2) compared to the group without neck pain (2.6° ± 0.9, t=10.47, p-value=<0.001).
When assessing physical functionality and overall health, the group with neck pain registered significantly lower scores than the group without neck pain. Specifically, the mean score for physical functionality was 64.8 ± 10.4 in the neck pain group, compared to 83.6 ± 9.1 in the group without neck pain (t=9.62, p-value=<0.001). Similarly, the average overall health score was lower in the neck pain group (62.1 ± 11.3) compared to the group without neck pain (78.3 ± 10.2, t=7.99, p-value=<0.01).
In summary, these findings suggest that neck pain is linked to decreased cervical range of motion, compromised neck posture, poor neck proprioception, and diminished physical functionality and overall health.
Table 3 depicts the correlation coefficients between neck pain and several variables under study. These coefficients quantify the strength and directionality of the relationship between neck pain and each study variable.
The inverse correlations between neck pain and the cervical range of motion (ROM) in flexion (−0.47), extension (−0.46), left rotation (−0.44), and right rotation (−0.45) suggest that an increase in neck pain corresponds to a decrease in cervical ROM across all these motions. The moderate magnitudes of these correlations imply that while the relationship between neck pain and cervical ROM holds statistical significance, it is not overwhelmingly strong.
The direct correlation between neck pain and neck proprioception (0.41) suggests that an increase in neck pain corresponds to an increase in neck proprioception. However, since proprioception is typically associated with the body’s capacity to sense movement and position, an increase in neck proprioception might signify deteriorated proprioception (ie, a higher value indicating a greater degree of impairment).
The inverse correlation between neck pain and the craniovertebral angle (−0.40) implies that an increase in neck pain corresponds to a decrease in the craniovertebral angle, which suggests a more forward-leaning neck position.
In the context of quality of life, both Physical Component Score (−0.65) and Mental Component Score (−0.60) demonstrate inverse correlations with neck pain, suggesting that as neck pain increases, scores in these domains of quality-of-life decrease, indicating a decline in quality of life.
In conclusion, all variables examined exhibit a significant correlation with neck pain. Specifically, an increase in neck pain is linked with decreased cervical ROM, compromised neck proprioception, a reduced craniovertebral angle, and a decline in quality of life in terms of both physical functioning and general health.
SF-36 physical and mental status of the patient was significantly correlated with NDI, and found that a significant indirect correlation between both the PCS and the MCS scores and the NDI (Figures 1-3).
 |
Figure 1 Measurement of Craniovertebral Angle (CVA) with Surgimap Software. |
 |
Figure 2 Correlation between NDI and SF-36 (PCS). |
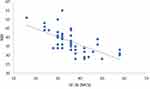 |
Figure 3 Correlation between NDI and SF-36 (MCS). |
Table 4 illustrates that the comparison of mean difference eight SF-36 dimensions among with pain and without neck pain groups. All SF-36 domain scores were statistically significantly lower than the without neck pain groups values.
 |
Table 4 Comparison of Mean Difference Eight SF-36 Dimensions Among with Pain and Without Neck Pain Groups |
Discussion
The present study revealed several significant relationships among neck pain, cervical range of motion (ROM), neck proprioception, craniovertebral angle (CVA), and quality of life (QOL) in bike drivers. These findings are consistent with previous research that identified a decrease in cervical ROM and neck proprioception and an alteration in CVA among individuals with neck pain.20 The significant reduction in cervical ROM observed in the neck pain group aligns with prior studies that found similar results among patients with chronic neck pain.3 This reduction can be explained by muscle spasm or fear of pain, leading to limitation of neck movements.21 Further research is needed to clarify the direct mechanism behind this observed limitation. Neck proprioception was also found to be impaired in the neck pain group. This is in line with research by Revel et al, who suggested that neck pain could lead to a deficit in proprioceptive feedback, which might be due to changes in muscle spindle sensitivity.22 However, it should be noted that an increase in neck proprioception score in our study corresponds to an increase in proprioceptive error, indicating poorer proprioception.
Our study demonstrated a smaller CVA in the neck pain group, suggesting a forward head posture. This finding is consistent with Szeto et al, who identified a significant association between neck pain and forward head posture in computer workers.2 A forward head posture might be a compensatory mechanism to reduce neck pain, but it could also contribute to the development of neck pain due to increased stress on the cervical spine.23
The negative correlations observed between neck pain and QOL domains (physical functioning and general health) are consistent with the findings of a study by Nolet et al that reported decreased QOL scores in individuals with neck pain.24 This could be due to the discomfort and limitation in activities associated with neck pain, which may negatively impact individuals’ overall health and functioning.
Our findings suggest that neck pain among bike drivers is associated with decreased cervical ROM, impaired neck proprioception, altered CVA, and decreased QOL. These findings highlight the need for interventions focusing on these aspects to improve the QOL of bike drivers experiencing neck pain.
Despite the valuable insights generated by this study into the connection between neck pain and various health metrics among bike drivers, certain limitations should be noted. The cross-sectional design of the study precludes the determination of causality between the examined variables. The small sample size and the inclusion of only bike drivers aged between 20 and 50 years may limit the generalizability of the results. Potential bias could have been introduced through the use of self-report measures like the SF-36 questionnaire, due to individual perceptions and interpretations. Additionally, the study did not consider potential confounding factors such as occupational history, physical activity level, or other health conditions.
Future research should take these limitations into account. Longitudinal studies could be designed to examine the causal relationships among neck pain, cervical ROM, neck proprioception, CVA, and QOL. The inclusion of a larger and more diverse age group of bike drivers could enhance the generalizability of the findings. Objective measurement tools for neck proprioception and CVA would further strengthen the reliability of results. Moreover, incorporating potential confounding factors in future analyses would contribute to a more comprehensive understanding of the relationship between neck pain and the examined variables.
The findings of this study, however, bear significant implications for the health and well-being of bike drivers. The association between neck pain and decreased cervical ROM, impaired neck proprioception, a forward head posture, and decreased QOL underscores the importance of comprehensive assessments and interventions in this population. Clinicians and health professionals may utilize these findings to develop targeted rehabilitation programs, focusing on improving cervical ROM, proprioception, and posture. The results also emphasize the need for preventive strategies against neck pain among bike drivers. These could potentially include ergonomics education, regular breaks, and exercises designed to maintain proper neck function and posture. Addressing these aspects could significantly enhance the quality of life of bike drivers.
Conclusion
In conclusion, this study has highlighted the significant associations between neck pain and decreased cervical range of motion, impaired neck proprioception, a forward head posture, and lower quality of life in bike drivers. These findings gain added significance considering our methodological rigor in participant selection, underscoring the study novelty in targeting non-professional bike Drivers, a largely understudied population. Despite the limitations of a cross-sectional design and a relatively small, narrow age range sample, the findings provide important preliminary insights that can be used to develop targeted interventions for this population. The results underscore the potential value of comprehensive assessments, rehabilitation programs, and preventive strategies in improving the health and well-being of bike drivers. Future research should aim to address the limitations of this study, expanding the sample size and age range, incorporating objective measurement tools, and considering potential confounding factors to provide a more comprehensive understanding of the relationship between neck pain and the examined variables. Longitudinal studies are particularly warranted to investigate the causal relationships among these variables. Ultimately, these research efforts could lead to enhanced quality of life and occupational health outcomes for bike drivers.
Registration
The study is registered under Clinical Trial Registry India (CTRI) with registration number CTRI/2022/11/047689.
Institutional Review Board Statement
The study was conducted after obtaining ethical clearance from the Institutional Ethical Committee of Integral University, Lucknow, India (IEC/IIMS&R/2022/70) and performed in accordance with the principles of the Declaration of Helsinki.
Data Sharing Statement
The datasets analysed in the current study are available from the corresponding author on reasonable request.
Informed Consent Statement
All participant’s written informed consent was signed and obtained publication of this study.
Acknowledgment
This work is acknowledged under Integral University manuscript number IU/R&D/2023-MCN0002254. The authors are also grateful to the Faculty of Health and Medical Sciences, Integral University, India, for the scientific support to this research. The authors are also very grateful to the Research Unit, Department of Physical Therapy, Jazan University.
Funding
There is no funding to report.
Disclosure
All the authors declare that they have no competing interest in this work.
References
1. Descatha A, Roquelaure Y. Neck and hand pain in office workers, “a piece of cake”. Scand J Work Environ Health. 2009;35(5):321–323. doi:10.5271/sjweh.1345
2. Szeto GP, Straker L, Raine S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl Ergon. 2002;33(1):75–84. doi:10.1016/S0003-6870(01)00043-6
3. Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther. 2004;9(2):89–94. doi:10.1016/S1356-689X(03)00086-9
4. Revel M, Andre-Deshays C, Minguet M. Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehabil. 1991;72(5):288–291.
5. Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 2008;13(1):2–11. doi:10.1016/j.math.2007.06.003
6. Johnston V, Jull G, Souvlis T, Jimmieson NL. Neck movement and muscle activity characteristics in female office workers with neck pain. Spine. 2008;33(5):555–563. doi:10.1097/BRS.0b013e3181657d0d
7. Yip CH, Chiu TT, Poon AT. The relationship between head posture and severity and disability of patients with neck pain. Man Ther. 2008;13(2):148–154. doi:10.1016/j.math.2006.11.002
8. Ferreira EA, Duarte M, Maldonado EP, Burke TN, Marques AP. Postural assessment software (PAS/SAPO): validation and Reliabiliy. Clinics. 2010;65(7):675–681. doi:10.1590/S1807-59322010000700005
9. Nejati P, Lotfian S, Moezy A, Moezy A, Nejati M. The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Med J Islam Repub Iran. 2015;29:26.
10. Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther. 2009;32(2 Suppl):S46–S60. doi:10.1016/j.jmpt.2008.11.010
11. Côté P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine. 1998;23(15):1689–1698. doi:10.1097/00007632-199808010-00015
12. Hush JM, Michaleff Z, Maher CG, Refshauge K. Individual, physical and psychological risk factors for neck pain in Australian office workers: a 1-year longitudinal study. Eur Spine J. 2009;18(10):1532–1540. doi:10.1007/s00586-009-1011-z
13. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
14. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. doi:10.1371/journal.pmed.0040296
15. Schaufele MK, Boden SD. Physical function measurements in neck pain. Phys Med Rehabil Clin N Am. 2003;14(3):569–588. doi:10.1016/S1047-9651(03)00030-5
16. Khan AR, Aafreen KA, Ahmed H, Shaphe MA, Qasheesh M, Qasheesh M. Test–retest reliability and validity of cervical range of motion measurement using a smartphone clinometer and compass application among individuals with and without neck pain. Int J Therapy Rehabilit. 2023;30(2):1–13. doi:10.12968/ijtr.2022.0004
17. Aafreen KA, Ahmed H, Khan AR, et al. Clinimetric properties of a smartphone application to measure the Craniovertebral Angle in different age groups and positions. Heliyon. 2023;9(2023):e19336. doi:10.1016/j.heliyon.2023.e19336
18. Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. doi:10.1097/00005650-199206000-00002
19. Howell ER. The association between neck pain, the Neck Disability Index and cervical ranges of motion: a narrative review. J Can Chiropr Assoc. 2011;55(3):211–221.
20. Sterling M, Jull G, Vicenzino B, Kenardy J. Characterization of acute whiplash-associated disorders. Spine. 2004;29(2):182–188. doi:10.1097/01.BRS.0000105535.12598.AE
21. Falla D, Bilenkij G, Jull G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine. 2004;29(13):1436–1440. doi:10.1097/01.BRS.0000128759.02487.BF
22. Revel M, Minguet M, Gregoy P, Vaillant J, Manuel JL. Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study. Arch Phys Med Rehabil. 1994;75(8):895–899. doi:10.1016/0003-9993(94)90115-5
23. Nejati P, Lotfian S, Moezy A, Moezy A, Nejati M. The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Med J Islam Repub Iran. 2014;28:26.
24. Nolet PS, Côté P, Kristman VL, Rezai M, Carroll LJ, Cassidy JD. Is neck pain associated with worse health-related quality of life 6 months later? A population-based cohort study. Spine J. 2015;15(4):675–684. doi:10.1016/j.spinee.2014.12.009
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

