Back to Journals » Substance Abuse and Rehabilitation » Volume 14
Nearly One-Fourth of Eastern Ethiopian Adolescents are Current Psychoactive Substance Users: A School-Based Cross-Sectional Study
Authors Birhanu A , Bete T, Eyeberu A , Getachew T , Yadeta E , Negash A , Lami M , Balcha T, Sertsu A , Deballa A
Received 30 December 2022
Accepted for publication 22 April 2023
Published 26 April 2023 Volume 2023:14 Pages 25—34
DOI https://doi.org/10.2147/SAR.S401843
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rajendra Badgaiyan
Abdi Birhanu,1 Tilahun Bete,2 Addis Eyeberu,3 Tamirat Getachew,3 Elias Yadeta,3 Abraham Negash,3 Magarsa Lami,3 Tegenu Balcha,3 Addisu Sertsu,4 Adera Deballa3
1School of Medicine, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 2Department of Psychiatry, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 3Department of Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 4Department of Nursing, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Correspondence: Abdi Birhanu, Haramaya University, P.O. Box: 235, Harar, Ethiopia, Email [email protected]
Introduction: Psychoactive substance use is a growing health problem in both developing and developed countries. Despite adolescents being at high risk of practicing risky behaviors including substance use, there is no adequate information on the problem in the Harari Region, in the Eastern part of Ethiopia. Hence, the present study aimed to identify the burden of current substance use in high school adolescent students of Harari Region, Ethiopia, from 10th April to 10th May 2022.
Methods: A school-based cross-sectional study was employed on a total of 1498 randomly selected adolescent students. Poisson regression was used for the assessment of substance use over the last three months among adolescent students. The substance use burden was reported by IRR (incidence rate ratio) at a 95% Confidence interval. The final model fitness was checked using Akaike information criterion (AIC) and Bayesian information criterion (BIC) reports. The variables that had less than 0.05 P-value were declared to be statistically significant.
Results: The overall psychoactive substance use was 373 (24.9%, 95% Confidence Interval (CI); 22.8– 27.1%). The substances included khat (21.6%, 95% CI; 18.6– 23.6%), alcohol drinking (1.8%; 95% CI; 1.3– 2.6%), and smoking (1.2%, 95% CI; 0.75– 1.9%). Being male (IRR (Incidence Rate ratio) = 1.21, 95% CI; 1.11– 1.38), availability of the substance (IRR (Incidence Rate ratio) = 2.02, 95%; 1.53– 2.66), having substance user friends (IRR=1.60: 95% CI: 1.30– 2.01), and being at a younger age (IRR = 1.21; 95% CI: 1.02– 1.44) increased the psychoactive substance use rate in the adolescents.
Conclusion and Recommendation: One out of four adolescents was a current psychoactive substance user. Being male, substance availability, having substance-user friends, and being at younger age increased the psychoactive substance use rate in school adolescents in Eastern Ethiopia. The intervention that involves the schools’ community, students’ families, and executive bodies should be strengthened to overcome the substance use-related burdens among high school adolescent students.
Keywords: psychoactive substance use, adolescents, students, Ethiopia
Introduction
Psychoactive substances are the compounds/chemicals that cause health and social problems, including addiction.1 These substances affect brain functions and cause disturbance in thought, feeling, mood, awareness, or any other behavior. For instance, drinking alcohol, and taking marijuana, nicotine, caffeine, and some pain medicines can change an individual’s behaviors.2 These substances can be grouped into legal (eg, tobacco and alcohol), illegal (eg, cocaine and heroin), and controlled for use by authorized bodies for treatment purposes that could be organized into 7 categories based on their behavioral and pharmacological effects such as Nicotine containing substances (chewing tobacco and smoking cigarettes), drinking alcohol, taking Cannabinoids (marijuana, hashish), Opioids (Heroin), Depressants (Benzodiazepines and Barbiturates), Stimulants (Cocaine and amphetamine), and Hallucinogens.1,2
Substance use is a growing problem in both developed and developing nations.3 Drug prescription abuse and psychoactive substances like heroin, cannabis, smack, and crack have increased considerably in the youth people, along with the already high burden of alcohol and tobacco consumption.4 Again, an increasing number of novel psychoactive substances are emerging worldwide.5 Among many children and adolescents, tobacco use, alcohol consumption, and using other substances are growing tremendously throughout the world.6 In addition, licit and illicit substances consumption is also growing more than ever globally, and surprisingly, these groups of the population are starting the consumption at their early life stage.7 In 2016, 10.3 million cancer-related disability-adjusted life years lost were attributable to substance use.8 In 2015, the attributable disability-adjusted life-years were the peak for tobacco consumption (170.9 million DALYs), followed by the consumption of alcohol. The overall substance-attributable death rates were primarily contributed by tobacco consumption (110.7 deaths per 100,000 population), followed by alcohol drinking (33.0 deaths per 100,000 population), respectively.9 Particularly, of these substances, smoking shares about five million deaths per year and is responsible for the largest burden of global diseases.10 Moreover, studies demonstrated that chronic khat chewing causes severe neurological disorders, cardiovascular problems, dental carries gastrointestinal disturbance, psychiatric conditions, and reproductive dysfunctions.11–14
In Ethiopia, the most frequently used substances by adolescents are cigarettes, khat, and alcohol.15 A study conducted in the central part of Ethiopia revealed that about 16.3% of individuals were substance users. Of these, 8.3%, 6.4%, and 5.9% of them were alcohol drinkers, cigarette smokers, and khat chewers, respectively.15 The burden of smoking in high school students was 11% of which 9.4% were current smokers.16 A substantial number of the students were exposed to common substances and those who used the khat, alcohol, and cigarette smoking as a lifetime in Ethiopia was 22.5%, 41.4%, and 21.5%, respectively.17 The current use was 47.9%, while the lifetime was found to be 65.4% in northern Ethiopia.18 Ethiopia was one of the countries that has signed the World Health Organization FRAMEWORK convention on substance use particularly, on the tobacco controls that ban the consumption of any type of tobacco products including cigarettes across the country in both indoor and outdoor spaces. However, the problems continue to rise at an alarming rate.19
Factors that drive substance use include age, having substance-user friends,16 community norms, substance-using family history, offspring’s substance use,18 close to smoking people (parents, teachers, and friends), substance availability, socioeconomic status, academic performance, level of self-esteem, perceived risk of using the substance,16 gender, having alcohol drinking family member, having khat chewing family member, poor school substance use controlling rule, substance retailing shops in the living areas, strong relationship with parents, and being a member of school mini-media.15 Even though pieces of evidence are indicating that the age of substance users is falling by,7 the number of substance-using adolescents is increasing by.18 In Ethiopia, existing kinds of reports focused mainly the substance use in higher institutions like universities and college students.20–24 Moreover, to the level of our knowledge, no studies done to determine the current substance use in the high school attending students in the study area where the availability and accessibility of such substances specifically cigarette smoking, khat chewing, and alcohol consumption are usually practiced.25,26 Therefore, this investigation is intended to determine the burden of the current substance use among high school adolescent students in the eastern part of Ethiopia.
Methods and Material
Study Area, Design, and Period
An institution-based cross-sectional study design was conducted in the Harari region state of Ethiopia, between 10th April and 10th May 2022. The region is situated 525 km away from the capital city of the eastern part of Ethiopia. The region is encircled by the Oromia region. There are two public and four private secondary schools in the region. More than 4000 students are attending class currently of which 50.1% are females.
Population and Eligibility Criteria
High school students who were attending their education from 9th to 12th grade in Harari Region were the target group of this study. Students who were in the randomly selected schools were considered the study population. The students were on the roster and actively attending their education during the semester in which this study was conducted. Students who were severely ill during the data collection time and were unable to respond to the questions due to their ill health condition were excluded from the study.
Sample Size Calculation and Sampling Technique
The sample size was calculated using a single population proportion formula as follows:
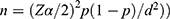 ; whereas n: the required sample size for this study, Zα/2(1.96): is significance level at α = 0.05 with 95% confidence interval, p: is the prevalence of substance use in school students in Kolfe Keranyo sub-city of Addis Ababa, Ethiopia (26.3%)15 and d: is the margin of error (3%). By considering the design effect of 1.5, the sample was determined to be 1323 with a non-response rate of 10%. Finally, a total of 1498 adolescents were randomly selected. Ninth to twelfth grade students were proportionally identified and randomly included using their registration numbers from the registrar’s office.
; whereas n: the required sample size for this study, Zα/2(1.96): is significance level at α = 0.05 with 95% confidence interval, p: is the prevalence of substance use in school students in Kolfe Keranyo sub-city of Addis Ababa, Ethiopia (26.3%)15 and d: is the margin of error (3%). By considering the design effect of 1.5, the sample was determined to be 1323 with a non-response rate of 10%. Finally, a total of 1498 adolescents were randomly selected. Ninth to twelfth grade students were proportionally identified and randomly included using their registration numbers from the registrar’s office.
Quality Control and Tools for Collecting Data
A designed self-administered tool was utilized for collecting all relevant information. The tool was developed from different literature using the English Language. Once prepared in English, the tool is retranslated into two local languages (Afaan Oromo and Amharic) to which the participants can read, write, listen, and speak. The substance use status was measured using Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST). This checklist was prepared by the World Health Organization international group of substance use investigators.27 The tool is primarily used to evaluate the substance use of both the lifetime and current use.27–29 A pretest was conducted on 5% of the sample before the actual data collection on non-selected high schools. The two-day training was provided for the data collectors and supervisors on the principles, procedures, and purpose of the study. Once the data were collected, the filled forms were manually assessed for consistency, accuracy, and validity checks. In the case of error, the data collectors were ordered to refill the incomplete information a day after the collection.
Operational Definition
Current psychoactive substance use was defined as when the student utilized a specific substance (for non-medical purposes) over the past three months.30,31
Every substance user was defined as a student who consumed a certain substance for non-medical purposes even only one time throughout their life.30
Statistical Analysis
The data were entered into Epi-data 3.1 and transferred to Stata 14.2 versions for analysis. The descriptive statistics including frequency, percent, and arithmetic mean with SD were computed. A Poisson regression extension of the binomial was run to determine the rate of using a psychoactive substance. A dichotomized outcome variable (current psychoactive substance user vs non-users) and independent variables association was assessed to identify the factors that affect substance use. The incidence rate ratio was used to assess the current psychoactive substance use in the last three months. Information criteria (AIC and BIC) were used for the model fitness test, and the model with the lowest score was used as the model fitted. The model with the lower value of AIC was selected to be the final analysis. Finally, the IRR with 95% CI was reported. Finally, the variables that had a P-value of <0.05 were declared as having a statistically significant association with the outcome variable of the study.
Ethical Statement
The Haramaya University College of Health and Medical Sciences (CHMS) Institutional Health Research Ethics Review Committee (IHRERC) reviewed and provided an ethical approval letter for this study. Then, data were collected after getting permission from the study schools based on the letter of cooperation sent from the college. The interview was held after taking informed, voluntary written and signed consent from all schools’ heads and students who aged 18 and above. In addition, the parental/legal guardian consent was obtained for the participants under 18 years of age. Taking part in the study was voluntary, and any information collected from the study participants was kept confidential. Participants were informed about the purpose of the study. Reports and other documents did not include the names of participants. The Helsinki Declaration was followed in each step of data obtaining and processing in this study.
Results
Sociodemographic Features of the Study Participants
The data of 1498 high school students are included in this study. More than half (n = 815, 54.41%) of the students were females, while the rest 45.59% were males. The average age of the students was 15 years with +3 Standard Deviation (SD). More than three-fourths, 1142 (76.23%) of the participants were single, while the rest were in a relationship (n = 299, 19.96%) and married (n = 57, 3.81%). Nearly three-fourths of the study respondents lived in an urban area with their parents. More than three-fourths of both fathers and mothers attended at least primary education. The majority of the high school students got money in their pockets whereas only 513 (34.25%) could not get it (Table 1).
 |
Table 1 Sociodemographic and Behavioral Characteristics of Students Attending Their High School Education in Harari Regional State, Eastern Ethiopia, 2022 |
Clinical History-Related Characteristics and Substance Use
Among a total of 1498 students, only 102 (6.8%) had a familial history of mental illness, while about 46 (3.1%) had a history of committing suicide in the family. About 83 (5.6%) of them had a history of suicidal attempts in their family. Many of the students (70.2%) slept for a maximum of 7 hours per day. About one-fourth of the students were users of any form of psychoactive products throughout their life. These ever-used substances were Khat (24.1%), smoking (1.8%), alcohol (3.3%), and others (1.4%). The reason why the students were using substances included availability (14.85%), peer influence (9.75%), academic purpose (8.2%), and his/her friends used (19.43%), and family used (39.49%). About 1043 (69.63%) of the students had a strong family control over using substances. Nearly one out of two students were challenged with poor social support. Depression and anxiety were identified in 668 (44.62%) and 589 (39.32%) of the students, respectively (Table 2).
 |
Table 2 Clinical Characteristics and Types of Substance Use Among High School Students in Harari Regional State, Eastern Ethiopia, 2022 |
Types and Patterns of Currently Used Psychoactive Substances
The overall psychoactive substance use was 373 (24.9%, 95% CI; 22.8–27.1%). The individual contribution of the substance was khat (325, 21.6%, 95% CI; 18.6–23.6%), alcohol consumption (28, 1.8%; 95% CI; 1.3–2.6%), smoking (18, 1.2%, 95% CI; 0.75–1.9%).
Factors Affecting Current Psychoactive Substance Using
The variables that had a p-value of <0.2 were transformed into the final analysis. In the final model, gender, age, substance-using friends, and easy availability of psychoactive substances had a significant relationship with the current psychoactive substance use among adolescent students.
The rate of substance use in male adolescents was 1.2 times more likely to occur than in female students (IRR = 1.2, 95% CI; 1.1–1.4). The psychoactive substance use rate was observed as 2 times more likely among adolescents who could easily get the substance around their living area (IRR = 2.02, 95%; 1.53–2.66). Among the students who had a friend of a psychoactive substance user, the substance use rate occurred 1.6 times than those whose friends were non-user of psychoactive substances (IRR = 1.60; 95% CI; 1.28–2.02). The probability of using the substance in younger adolescents was higher by 1.2-fold than among individuals in the late adolescence period (IRR=1.2: 95% CI: 1.1–1.4) (Table 3).
 |
Table 3 Factors Affecting Psychoactive Substance Use Among High School Adolescent Students in Harari Region, Eastern Ethiopia, 2022 |
Discussions
The current study is intended to evaluate the burden and features affecting current psychoactive substance use in adolescent students in East Ethiopia. Accordingly, the study publicized that the overall current any kind of substance use in the last three months was 24.9%, 95% CI; 22.8–27.1%. The individual contribution of these substances was khat (20.4%, 95% CI; 18.6–22.6%), alcohol consumption (1.8%; 95% CI; 1.3–2.6%), smoking (1.2%, 95% CI; 0.75–1.9%). Factors such as gender, age, having substance-using friends, and living with substance-using families had a significant relationship with substance use in East Ethiopian high school adolescents.
The overall use of any psychoactive substance rate in the last three months was 24.9% in students attending high school students. The report is lower compared to the study conducted in Southern Ethiopia disclosed that the current substance use was 35.5% among university students.32 As the majority of high school students are more attached to their families than University-level students, this lower finding indicates the paramount role of the family in shaping their siblings’ behaviors. Moreover, this could be evidence of the role of the family in coughing their children by counseling them not to be exposed to substance use.33
The studies conducted in Morocco (overall substance use, 6.3%),34 Nigeria (alcohol consumption, 13.6%).35 Another study from Morocco showed that 4.8% of young people were psychoactive substance users. The study clearly showed that cannabis was the most used substance and alcohol was used by 4.3% of students. However, the current study revealed that the most used substance was khat (21.6%), and 1.8% of alcohol consumption. This could be due to variations of psychoactive substance distribution across the countries and level of exposure differences due to geographical variation and sociodemographic differences. In addition, because of this study time, the COVID-19 pandemic might cause depression that enforces adolescents to use psychoactive substances.36,37
In the current study, substance use was high among male adolescents in school. The studies from Morocco,34 and South Africa38 supported that males are a high probability of using substances than females. Different findings reported that men are a risky group for having substance use disorder.39,40 This could be probably due to that males use substances to get acceptability, for enjoying, be courageous and bold enough, for engaging in sexual activities, and overcome stress in hard situations.41,42
Younger high school students used psychoactive substances higher than older adolescents. This result is consistent with the reports of studies from South Africa and Nepal.38,43 Age is one of the most important features responsible for the fast growth of substance use. The report showed that psychoactive substance-related mental and behavioral problems are rising among younger people.44 This could be due to the fact that younger age is the time when people start to practice something that they perceived to be new or told to do so by peers. As the young are encouraged to use the substance by the people around them or the environment, they can be easily immersed in the problem without knowing the health ill effect of using these substances.
This study presented that having a friend who uses psychoactive substances is another important factor that increased the substance use rate among school students. This finding agreed with the reports presented from the Northern part of Ethiopia,45 the southern part of Ethiopia,32 and the southwest part of Ethiopia.46 Peer pressure could negatively or positively affect adolescents whether for using or not using psychoactive substances.47 Therefore, the substance-using student could easily push his/her friend to share what he/she is practicing for getting stimulated and enjoy together.48 Moreover, the social learning that can be shared with family, friends, classmates, and any form of interaction can share risky behaviors among adolescents.34,49,50 Hence, any enabling factors from family, friends, and other surroundings could lead adolescents to be psychoactive substance users.51,52
The psychoactive substance use rate was 2 times more likely among those adolescents who easily got the substance nearby their living area. This finding is supported by the reports from the USA,53 South Africa,54 and Abu Dhabi.55 It could be due to the fact that available substance can be used by other population segments in the area. If others use it, the age of adolescence is the time at which adolescents exercise something which is practiced by others. Therefore, the availability and common utilizing psychoactive substances by the community could increase the tendency of practicing what others are utilizing. In general, in this study, identifying the burden and driving factors of psychoactive substance use can contribute to strengthening interventions such as awareness creation through alarming the concerned bodies about the magnitude and negative consequences of using substances among adolescents. Even if this study has much strength, the study would not be free from limitations. The first limitation of the study could be the cross-sectional study nature would not enable the study to know the causal relationships between factors and substance use due to the snap-shooting approach of data capturing. Secondly, even if the study was conducted on the largest number of adolescents than probably some studies previously done; the findings cannot represent all Ethiopian adolescents.
Conclusion and Recommendation
One out of four adolescents was a current user of psychoactive substances in the Harari Region, Ethiopia. Being male, substance availability, having substance user friends, and being at younger age increased the rate of using psychoactive substances in-school adolescents in Eastern Ethiopia. The intervention that involves the schools’ community, students’ families, and executive bodies should be strengthened to overcome the substance use-related burdens among high school adolescent students. Awareness creation efforts should be made to prevent the health effect of using psychoactive substances among adolescents.
Data Sharing Statement
Data used in the current study are available from AB upon reasonable request.
Disclosure
All authors declared that they have no conflicts of interest in this work.
References
1. McLellan AT. Substance misuse and substance use disorders: why do they matter in healthcare? Trans Am Clin Climatol Assoc. 2017;128:112.
2. Stangor C, Walinga J, Sanders L. 7.4 altering consciousness with psychoactive drugs. In: Introduction to Psychology. University of Saskatchewan Open Press; 2019.
3. Kaur R, Singh T, Basu D, Kumar R. Prevalence and pattern of psychoactive substance use among female students aged 18–25 years in universities of North India. Int J Commun Med Public Health. 2019;6(2):602–609. doi:10.18203/2394-6040.ijcmph20190176
4. Aich TK, Saha I, Ram D, Ranjan S, Subedi S. A comparative study on 136 opioid abusers in India and Nepal. J Psychiatrists Assoc Nepal. 2015;2(2):11–17.
5. United Nations Office on Drugs and Crime. Global Synthetic Drugs Assessment: Amphetamine-Type Stimulants and New Psychoactive Substances. United Nations Office on Drugs and Crime; 2014.
6. Roy R. Psychosocial factors contributing towards substance abuse among adolescents–A qualitative study. J Psychosoc Res. 2018;13(2):425–433. doi:10.32381/JPR.2018.13.02.17
7. World Health Organization. Summary Results of the Global Youth Tobacco Survey in Selected Countries of the WHO European Region. World Health Organization; 2020.
8. Rehm J, Shield KD, Weiderpass E. Alcohol consumption. A leading risk factor for cancer. Chem Biol Interact. 2020;331:109280. doi:10.1016/j.cbi.2020.109280
9. Peacock A, Leung J, Larney S, et al. Global substance use: 2017 update; 2017.
10. Mathers C, Stevens G, d’Espaignet E, Wolfenden L. WHO Global Report: Mortality Attributable to Tobacco. World Health Organization; 2012.
11. Hassan NA, Gunaid AA, Abdo-Rabbo AA, et al. The effect of Qat chewing on blood pressure and heart rate in healthy volunteers. Trop Doct. 2000;30(2):107–108. doi:10.1177/004947550003000219
12. Al‐Hebshi N, Skaug N. Effect of khat chewing on 14 selected periodontal bacteria in sub‐and supragingival plaque of a young male population. Oral Microbiol Immunol. 2005;20(3):141–146. doi:10.1111/j.1399-302X.2004.00195.x
13. Ghani NA, Eriksson M, Kristiansson B, Qirbi A. The influence of khat-chewing on birth-weight in full-term infants. Soc Sci Med. 1987;24(7):625–627. doi:10.1016/0277-9536(87)90068-2
14. Al‐Motarreb A, Baker K, Broadley KJ. Khat: pharmacological and medical aspects and its social use in Yemen. Phytother Res. 2002;16(5):403–413. doi:10.1002/ptr.1106
15. Seid L, Gintamo B, Mekuria ZN, Hassen HS, Gizaw Z. Substance use and associated factors among preparatory school students in Kolfe-Keranyo sub-city of Addis Ababa, Ethiopia. Environ Health Prev Med. 2021;26(1):1–12. doi:10.1186/s12199-021-01032-1
16. Duko B, Melese Y, Ebrahim J. Determinants of cigarette smoking among adolescents in Ethiopia: a cross-sectional study. Tob Induc Dis. 2019;17. doi:10.18332/tid/110800
17. Roba HS, Beyene AS, Irenso AA, Gebremichael B. Prevalence of lifetime substances use among students in Ethiopia: a systematic review and meta-analysis. Syst Rev. 2019;8(1):1–16. doi:10.1186/s13643-019-1217-z
18. Birhanu AM, Bisetegn TA, Woldeyohannes SM. High prevalence of substance use and associated factors among high school adolescents in Woreta Town, Northwest Ethiopia: multi-domain factor analysis. BMC Public Health. 2014;14(1):1–11. doi:10.1186/1471-2458-14-1186
19. Geleta TA, Amdisa D, Gizaw AT, Tilahun D. Why are youth engaged in substance use? A qualitative study exploring substance use and risk factors among the youth of Jimma Town, Southwest Ethiopia. Subst Abuse Rehabil. 2021;12:59. doi:10.2147/SAR.S328079
20. Tesfaye G, Derese A, Hambisa MT. Substance use and associated factors among university students in Ethiopia: a cross-sectional study. Jo Addict. 2014;2014:1–8. doi:10.1155/2014/969837
21. Gebremariam TB, Mruts KB, Neway TK. Substance use and associated factors among Debre Berhan University students, Central Ethiopia. Subst Abuse Treat Prev Policy. 2018;13(1):1–8. doi:10.1186/s13011-018-0150-9
22. Deressa W, Azazh A. Substance use and its predictors among undergraduate medical students of Addis Ababa University in Ethiopia. BMC Public Health. 2011;11(1):1–11. doi:10.1186/1471-2458-11-660
23. Derese A, Seme A, Misganaw C. Assessment of substance use and risky sexual behaviour among Haramaya University Students, Ethiopia. Sci J Public Health. 2014;2(2):102–110.
24. Gebresilassie Tesema A, Hadush Kahsay Z, Gidey Lemma G, et al. Prevalence of, factors associated with and level of dependence of psychoactive substance use among Mekelle University students, Ethiopia. Int J Environ Res Public Health. 2020;17(3):847. doi:10.3390/ijerph17030847
25. Yitayih Y, van Os J. Prevalence and determinants of chewing khat among women in Ethiopia: data from Ethiopian demographic and health survey 2016. BMC Psychiatry. 2021;21(1):1–8. doi:10.1186/s12888-021-03136-y
26. Guliani H, Gamtessa S, Çule M. Factors affecting tobacco smoking in Ethiopia: evidence from the demographic and health surveys. BMC Public Health. 2019;19(1):1–17. doi:10.1186/s12889-019-7200-8
27. Heslop K, Ross C, Osmond B, Wynaden D. The Alcohol Smoking and Substance Involvement Screening Test (ASSIST) in an acute mental health setting. Int J Ment Health Addict. 2013;11(5):583–600. doi:10.1007/s11469-013-9428-3
28. Group WAW. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi:10.1046/j.1360-0443.2002.00185.x
29. Muhamad NA, Mihat O, Ramly R, et al. Translation, cross-cultural adaptation, reliability and validity of the Malay version of Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) V3. 1. Health. 2018;10(07):985. doi:10.4236/health.2018.107073
30. Sintayehu M, Mulat H, Yohannis Z, Adera T, Fekade M. Prevalence of mental distress and associated factors among caregivers of patients with severe mental illness in the outpatient unit of Amanuel Hospital, Addis Ababa, Ethiopia, 2013: cross-sectional study. J Mol Psychiatry. 2015;3(1):1–10. doi:10.1186/s40303-015-0014-4
31. Bete T, Lami M, Negash A, et al. Current alcohol, tobacco, and Khat use and Associated Factors among Adults Living in Harari Regional State, Eastern Ethiopia: a Community Based Cross-sectional Study. Front Psychiatry. 2022;13:2517.
32. Kassa A, Taddesse F, Yilma A. Prevalence and factors determining psychoactive substance (PAS) use among Hawassa University (HU) undergraduate students, Hawassa Ethiopia. BMC Public Health. 2014;14:1044. doi:10.1186/1471-2458-14-1044
33. Janicijevic KM, Kocic SS, Radevic SR, Jovanovic MR, Radovanovic SM. Socioeconomic factors associated with psychoactive substance abuse by adolescents in Serbia. Data report. Front Pharmacol. 2017;2017:8. doi:10.3389/fphar.2017.00366
34. Zarrouq B, Bendaou B, El Asri A, et al. Psychoactive substances use and associated factors among middle and high school students in the North Center of Morocco: a cross-sectional questionnaire survey. BMC Public Health. 2016;16(1):468. doi:10.1186/s12889-016-3143-5
35. Makanjuola AB, Daramola TO, Obembe AO. Psychoactive substance use among medical students in a Nigerian university. World Psychiatry. 2007;6(2):112–114.
36. Lima G, Muniz-Pardos B, Kolliari-Turner A, et al. Anti-doping and other sport integrity challenges during the COVID-19 pandemic. J Sports Med Phys Fitness. 2021;61(8):1173–1183. doi:10.23736/S0022-4707.21.12777-X
37. Negro F, Di Trana A, Marinelli S. The effects of the COVID-19 pandemic on the use of the performance-enhancing drugs. Acta Bio Medica. 2022;92(6). doi:10.23750/abm.v92i6.12377
38. Muchiri BW, Dos Santos MML. Family management risk and protective factors for adolescent substance use in South Africa. Subst Abuse Treat Prev Policy. 2018;13(1):24. doi:10.1186/s13011-018-0163-4
39. McHugh RK, Votaw VR, Sugarman DE, Greenfield SF. Sex and gender differences in substance use disorders. Clin Psychol Rev. 2018;66:12–23. doi:10.1016/j.cpr.2017.10.012
40. Woldeamanuel BT, Anteneh LM, Yohannes YB, Aga MA. Assessment of exposure to sexually explicit materials and substance abuse among high-school adolescents in North Shewa Zone: application of logistic regression analysis. J Addict. 2020;2020:8105087. doi:10.1155/2020/8105087
41. Aguocha CM, Duru CB, Ndukuba AC, Nwefoh EC. Gender differences in psychoactive substance use among undergraduates in a developing country. J Subst Use. 2021;26(1):85–93. doi:10.1080/14659891.2020.1779363
42. Stella A, Marinelli S, Berretta P, Pacifici R, Del Rio A. Sex enhancers: challenges, threats and the need for targeted measures. Clin Ter. 2019;170(3):e181–e183. doi:10.7417/CT.2019.2130
43. Poudel A, Gautam S. Age of onset of substance use and psychosocial problems among individuals with substance use disorders. BMC Psychiatry. 2017;17(1):10. doi:10.1186/s12888-016-1191-0
44. Le Querrec F, Bounes V, Mestre ML, Azema O, Longeaux N, Gallart J-C. Sex and age differences in ED patients with mental and behavioral disorders due to psychoactive substance use. Am J Emerg Med. 2015;33(11):1612–1616. doi:10.1016/j.ajem.2015.06.068
45. Gebreslassie M, Feleke A, Melese T. Psychoactive substances use and associated factors among Axum University students, Axum Town, North Ethiopia. BMC Public Health. 2013;13:693. doi:10.1186/1471-2458-13-693
46. Ayenew M, Kabeta T, Woldemichael K. Prevalence and factors associated with substance use among street children in Jimma town, Oromiya national regional state, Ethiopia: a community based cross-sectional study. Subst Abuse Treat Prev Policy. 2020;15(1):61. doi:10.1186/s13011-020-00304-3
47. Keyzers A, Lee SK, Dworkin J. Peer pressure and substance use in emerging adulthood: a latent profile analysis. Subst Use Misuse. 2020;55(10):1716–1723. doi:10.1080/10826084.2020.1759642
48. Reed MD, Rountree PW. Peer pressure and adolescent substance use. J Quant Criminol. 1997;13(2):143–180. doi:10.1007/BF02221306
49. Adesina BO, Adebayo AM, Iken OF. Factors associated with psychoactive substance use among in-school adolescents in Zaria Local Government Area, Kaduna State, Nigeria: a cross-sectional study. Int J Schl Health. 2020;7(1):14–22. doi:10.30476/intjsh.2020.83659.1030
50. Shek DTL, Zhu X, Dou D, Chai W. Influence of family factors on substance use in early adolescents: a longitudinal study in Hong Kong. J Psychoactive Drugs. 2020;52(1):66–76. doi:10.1080/02791072.2019.1707333
51. Carver H, Elliott L, Kennedy C, Hanley J. Parent–child connectedness and communication in relation to alcohol, tobacco and drug use in adolescence: an integrative review of the literature. Drugs Educ Prevent Policy. 2017;24(2):119–133. doi:10.1080/09687637.2016.1221060
52. Khalil MM, Hamdan-Mansour AM. Factors associated with substance use disorder among adolescents age group: an integrative review. Open J Nurs. 2019;9(09):998. doi:10.4236/ojn.2019.99074
53. Broman CL. The availability of substances in adolescence: influences in emerging adulthood. J Child Adolesc Subst Abuse. 2016;25(5):487–495. doi:10.1080/1067828x.2015.1103346
54. Aram Khoza HNS. Substance use and associated factors among in school adolescents in South Africa. Open Public Health J. 2021. doi:10.2174/1874944502114010435
55. Alhyas L, Al Ozaibi N, Elarabi H, et al. Adolescents’ perception of substance use and factors influencing its use: a qualitative study in Abu Dhabi. JRSM Open. 2015;6(2):2054270414567167. doi:10.1177/2054270414567167
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Factors Influencing Undergraduate Students’ Preference of Health Sciences Specialties
Gameraddin M, Al-sultan K, Salih S, Gareeballah A, Hasaneen M, Alomaim W, Omer A
Advances in Medical Education and Practice 2022, 13:1351-1358
Published Date: 21 October 2022
Comprehensive Knowledge, Attitudes, Behaviors, and Associated Factors of HIV/AIDS in Gondar City Public Health Facilities Among HIV Testing and Counselling Service Users, Northwest Ethiopia, 2022; an Ordinal Logistic Regression Analysis
Terefe B, Techane MA, Assimamaw NT
HIV/AIDS - Research and Palliative Care 2023, 15:713-726
Published Date: 7 December 2023
