Back to Journals » International Journal of General Medicine » Volume 16
Navigating Thyroid Dysfunction and Comorbidities Among University Students in Abbottabad, Pakistan – A Cross-Sectional Evaluation of Screening Tool for Thyroid Dysfunction
Authors Iqbal A , Azhar S, Murtaza G, Bibi R, Samreen S , Iqbal MM, Syed W , Al-Rawi MBA
Received 15 May 2023
Accepted for publication 7 September 2023
Published 15 September 2023 Volume 2023:16 Pages 4193—4205
DOI https://doi.org/10.2147/IJGM.S415311
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ayesha Iqbal,1,2 Saira Azhar,3 Ghulam Murtaza,4 Rashida Bibi,5 Sana Samreen,6 Muhammad Mamoon Iqbal,7,8 Wajid Syed,9 Mahmood Basil A Al-Rawi10
1Division of Pharmacy Practice and Policy, School of Pharmacy, University of Nottingham, Nottingham, UK; 2Office of Lifelong Learning and the Physician Learning Program, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, AB T6G1C9, Canada; 3College of Pharmacy, University of Sargodha, Sargodha, 40100, Pakistan; 4Department of Pharmacy, COMSATS University Islamabad (CUI), Lahore Campus, Khyber Pakhtunkhwa, 54000, Pakistan; 5Department of Pharmacy, Abbottabad University of Science and Technology, Khyber Pakhtunkhwa, Pakistan; 6Aurobindo College of Pharmacy, Warangal, Telangana, India; 7Ayub Medical College, Abbottabad, Khyber Pakhtunkhwa, 22040, Pakistan; 8University Hospitals of Leicester NHS Trust, Balmoral Building Leicester Royal Infirmary, Infirmary Square Leicester Leicestershire, Leicester, LE1 5WW, UK; 9Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia; 10Department of Optometry, College of Applied Medical Sciences, King Saud University, Riyadh, 11451, Saudi Arabia
Correspondence: Wajid Syed, Email [email protected]
Background: Thyroid dysfunction has a direct role in diagnosing, and assessment and indicates the development of thyroid carcinoma. This study aimed to assess thyroid dysfunction through medical camps in different age and sex groups in students of Comsats University Abbottabad Pakistan.
Methods: In this study, a cross-sectional survey design was used. For data collection, a two-day medical camp was set in the Comsats University Abbottabad campus. The students were examined physically for symptoms of thyroid dysfunction using the survey questionnaire specifically designed for this study.
Results: The current research revealed that 78 out of 1032 students, or 7.6% of the population, had thyroid disease. Although 39.3% (=406) were found to have low risk, followed by 36.7% (n=379) had moderate risk and 23.9% (n=247) had high risk of thyroid dysfunction. Altogether, 6.1% (n=63) of the students had high blood pressure (BP), 3.2% (n=33) had high cholesterolemia, 3.4% (n=33) had angina, and 0.9% (n=9) had diabetes mellitus (DM). In relation, students who exhibit signs and symptoms that last longer than five weeks include 42.2% (n=435) who felt the need for excessive sleep, 35.3% (n=364) who felt tired, 36.8% (n=380) who had trouble concentrating and 30.1% (n=311) who had palpitations. The high risk of thyroid being seen predominantly in students between the ages of 15– 20 years (31.2%, n=148), as opposed to other age groups (p=0.001). Similar to this, women having a higher risk of thyroid disease (26.5%) than men (22.8%) (p =0.001).
Conclusion: In conclusion, few students suffer with thyroid found to have high risk of thyroid disease. This method of questionnaire-based screening for thyroid dysfunction is cost-effective, with no additive risk of adverse effects from excessive screening, and could help in the early detection of thyroid and help avoid excess costs related to thyroid dysfunction and cancer screening.
Keywords: thyroid dysfunction, screening, medical camp, thyroid cancer
Introduction
Screening of certain medical diseases through risk factors is a scientifically accepted method of finding diseases in their early stages and identifying high-risk populations.1,2 One of the most effective methods of diagnosis in the early stages of disease is preliminary screening.1,2 Screening can be performed by pharmacists as they have acknowledged their role in interdisciplinary clinical practice settings and are an integral and vital part of health care teams.1,2 Thyroid is one of the endocrine diseases whose prevalence is increasing day by day.1 According to a recent epidemiological study, the prevalence of hypothyroidism is between 1% and 2%, and it is more common in older women and ten times more common in women than in men.3 In addition, it was believed that females are more prone to have alternation in thyroid function than males.3,4
The overall prevalence of hypothyroidism and hyperthyroidism in Pakistan is 4.1% and 5.1%, respectively. According to another recent study, 1.6% had a newly diagnosed subclinical hypothyroidism. While 1.2% of women had hyperthyroidism, 6% had known hypothyroidism, and 1% had overt hypothyroidism.5 A recent systematic review and meta-analysis on the global prevalence of thyroid revealed that the prevalence of Hashimoto’s thyroiditis was 7.5%, while in the low-middle-income group, the prevalence was 11.4%. Similarly, the prevalence was 5.6 in the upper-middle-income group, and in the high-income group, the prevalence was 8.4. The prevalence of thyroid was 14.2% in Africa, while in Oceania it was 11.0% in South America and Europe it was 8.0, and 7.8%. On the other hand, in North America, and Asia it was 5.8%.6 The American Thyroid Association revealed that approximately 20 million Americans have some form of thyroid disease; interestingly, the majority of the thyroids were unaware of their disease status.7,8
The most common early signs of thyroid diseases were a lump in the neck or swelling, followed by pain in the neck or difficulty in swallowing.7,8 The risk factors identified were gender, more particularly being a female, elderly aged above 60 years, recent pregnancy, posing autoimmune disease, presence of hypertension, and obesity are positively related to thyroid disease development.9,10 Other studies revealed that radiation is one of the most common predisposing factors especially irradiation of the head and neck in early childhood, which is found to link to thyroid carcinomas.9,10 Some earlier research showed a link that a high level of thyroid-stimulating hormone (TSH) is linked with thyroid various carcinoma.11,12
Thyroid diseases mainly constitute abnormal levels of TSH, triiodothyronine (T3), or thyroxine (T4).13,14 TSH is the major chemical marker to identify thyroid function.6 When the level of TSH is low, it results in hyperthyroidism while if the value increases it indicates hypothyroidism. Overall people who are suffering from thyroid dysfunction have 2% hyperthyroidism people, while 98% of people suffer from hypothyroidism.13,14 The most common cause of hyperthyroidism in Pakistan in the majority of cases is Grave’s disease, or multinodular goiter or adenoma5,15,16 and is characterized by multi-nodular goiter in the middle age and elderly population.5,15,16 Hypothyroidism is more common and involves increased TSH, slow metabolic rate, growth retardation, and impaired physical and mental development. The most common cause of hypothyroidism is iodine deficiency.16,17 Hypothyroidism can also be drug-induced, drugs like interferon alpha, thalidomide, and lithium can also precipitate or cause hypothyroidism.18
The lack of knowledge about this illness, as well as the ignorance of key risk factors like food, genetic predisposition, and environmental risk factors, is one of the causes for this increased frequency of thyroid disease among people. Due to a lack of data generated in various regional and geographical strategic points, it is currently impossible to determine the area-wise distribution of thyroid dysfunction and thyroid carcinoma in Pakistan; however, if this data is obtained, it will be useful for comparisons with the rest of Asia and the rest of the world. Screening camps are typically useful in identifying secondary or asymptomatic diseases that go unnoticed by the general populace. The goal of this medical camp is to test university students for thyroid dysfunctional symptoms and risk factors to diagnose thyroid issues early, treat them, and lower their risk of developing thyroid cancer. As a result, a questionnaire was created to assess thyroid dysfunction in various age and sex categories among Comsats University Abbottabad, Pakistan, students through medical camps.
Methodology
Study Design
A cross-sectional study design was used for the assessment of thyroid-related signs and symptoms in university students. This camp was organized in collaboration with Agha Khan University Hospital Karachi (AKUH), Al-Rasheed Cancer Cure Trust Abbottabad and was organized from 29 to 30th August 2016 in Comsats Abbottabad campus during the Thyroid Cancer Awareness Month, which is listed in the American Hospital Association’s Calendar of Health Observances & Recognition Days. The students who participated in this study were enrolled in different undergraduate and graduate academic programs at the university. The ethical committee of Comsats University Abbottabad campus, Islamabad, reviewed and approved the study protocol before data collection (Approval No. 6734-CUIATD). Furthermore, written informed consent was obtained from students before data collection, and the study followed the guidelines outlined in the Helsinki Declaration. Students were informed that the data would be used solely for research purposes, that the submitted information would be kept confidential, and that they had the opportunity to withdraw from the study at any time throughout the study period.
Sample Size
Out of the total departments who participated in this medical camp, 1396 students visited the medical camp out of which 1032 were willing for the Thyroid problem assessment program, which corresponds to a response rate to 73.92%.
Study Tool
The questionnaire was designed using guidelines from the Thyroid Foundation of Canada, hyperthyroidism from Wayne’s Index 10, and the Billewicz score for hypothyroidism.19 The overall score was calculated as a sign and symptom score less than 3 was graded as low risk of thyroid dysfunction, a score between 3 and 8 was interpreted as a moderate risk of thyroid dysfunction and a score of 9 or above showed a high risk of thyroid dysfunction.
Implementation and Data Analysis
Before data collection, the data collection instrument was pilot-tested on a group of 30 university students who were randomly selected on campus to determine the validity and reliability of the tool. The value of Cronbach’s α was found to be 0.85 which indicates good reliability of the tool. A total of 1032 students visited the medical camp and were assessed by a direct interview as well as physical assessment and the data was recorded in the questionnaire (paper format). The questionnaire provided information about the assessment of thyroid-related signs and symptoms and screening of pre-disposing risk factors for thyroid dysfunction in all Comsats University Abbottabad campus students. The medical camp included a team of 08 volunteer members including doctors and pharmacists and examined each person individually for approximately 15 minutes. Volunteers collected demographic data including the age of the student, gender, area of residence, number of household members, and monthly income. The second portion of the assessment consisted of direct close-ended questions focusing on persistent symptoms for more than 05 weeks to detect any signs and symptoms linked to thyroid dysfunction. The students explained all conditions in a non-medical language (Urdu – A common language) so that they could understand properly. The third portion of data entry was focused on the assessment of thyroid personal and family history; the medical history of the student (presence of thyroid or not), and their family members including any diagnosed thyroid disorders current or past, current or past medication thyroid medicine use history, and any herbal dietary supplement for thyroid-related signs and symptoms. The last portion of the assessment included any co-morbid conditions like hypertension, diabetes ellitus, heart disease or angina, high cholesterolemia, and any form of malignancy.
Data Analysis
The data were analyzed using Statistical Package for Social Sciences version 26.0 (SPSS Inc., Chicago, IL, USA). A descriptive statistic was used to assess students’ responses, frequencies(n) and percentages (%) were used to describe categorical data, and the Chi-square/Fisher exact test was used to perform comparisons between variables. The dependent variables (means core of risk levels of thyroid) were considered numeric variables, and independent variables (age, gender residential status) were categorical, so we used multiple linear regression analysis to compute the association. A P-value of <0.05 was considered a statistically significant difference.
Results
Out of a total of 1396 students who participated in the medical assessment camp, there was a diverse age group which included 474 (45.3%) in 15–20 years of age, 523 (50.7%) in 21–25 years, 32 (3.1%) in 26–30 years and 03 (0.3%) in 31–35 years. Out of a total of 1032 students, 707 (68.5%) were males and 323 (31.5%) were females. In this study, 670 (64.9%) were from urban areas and 362 (35.1%) belonged to rural areas. Students come from different families and have different economic backgrounds. Those students whose family income was less than 25,000 Pakistani rupees (PKR) (average) were 156 (15.1%), whose income was 25,000–50,000 (high) PKR were 521 (50.5%) and those whose family income exceeded 50,000 (low income) PKR were 355 (34.4%) as shown in Table 1.
 |
Table 1 Students’ Demographics (n=1032) |
Of those students who had no co-morbid disease were 810 (78.5%). Among all 63 (6.1%) students were suffering from high BP, 33 (3.2%) students had high cholesterolemia levels, 35 (3.4%) students had angina, 9 (0.9%) students had diabetes mellitus (DM), 5 (0.5%) students had cancer (Table 2). Comorbidities with regard to gender, high BP was reported higher among females 20 (6.2%) than male 43 (6.1%), while cholesterol, angina, and diabetes were reported higher among male 24 (3.4%), 25 (3.5%),8 (1.1%) students than female 9 (2.8%), 10 (3.1%),1 (0.3%). Figure 1.
 |
Table 2 Comorbidities of Students (n=1032) |
 |
Figure 1 Comorbidities among respondents according to gender. |
Furthermore, out of all, 42 students were suffering from a combination of diseases, such as BP and cholesterol, 17 (1.6%), followed by BP and angina, 6 (0.6%), diabetes and high cholesterolemia, 4 (0.4%) BP, cholesterol and cancer, 2 (0.2%) has BP, cholesterol and cancer, 1 (0.1) student had BP and DM, 1 (0.1) student had high cholesterolemia and DM, 1 (0.1) student had DM and heart disease and 1 (0.1) student had DM, angina and cancer as indicated in Table 2. Similarly, the combination of the comorbidities was significantly different among genders, where a combination of BP and cholesterol, was higher among male students 37 (5.2%) than female 5 (1. 5%). Similarly, the BP and angina were higher in males 14 (2%) than females 3 (0.9%) as shown in Figure 2, indicating a statistically significant difference.
 |
Figure 2 Combination of comorbidities according to gender. |
Out of total 1032 students 435 (42.2%) felt the need for excessive sleep, 364 (35.3%) felt fatigued, 311 (30.1%) were experiencing palpitations, 380 (36.8%) had poor concentration, 335 (32.5%) experienced memory loss, 334 (32.4%) had difficulty sleeping, 318 (30.8%) had weak muscles, 248 (24%) had sore muscles, 337 (32.7%) were experiencing anxiety, 347 (33.6%) felt depressed, 323 (31.3%) students experienced dry skin, while 235 (22.8%) were experiencing itchy skin, 442 (42.8%) had cracked, 143 (13.9%) were experiencing infrequent bowel movements, 157 (15.2%) had frequent bowel movements, 199 (19.3%) experienced weight gain, while 157 (15.2%) lost weight, 134 (13%) experienced persistent pain at the front of the neck, 120 (11.6%) had hoarseness of voice, lump in throat was by 171 (16.6%), 171 (16.6%) reported diplopia, swelling or protrusion of eyes was felt by 167 (16.2%), 220 (21.3%) reported facial changes, sweating was experienced by 351 (34%), 265 (25.7%) reported difficulty tolerating cold, while 208 (20.2%) reported difficulty tolerating heat, hand tremors were felt by 157 (15.2%) as indicated in Table 3.
 |
Table 3 Signs and Symptoms Persist for More Than 05 Weeks in Students (n=1032) |
Students who had family members suffering from diagnosed thyroid disease were 91 (8.8%), and students who themselves were suffering from a thyroid disease were 78 (7.6%) out of 1032 students. Among those majority of them found to have under active thyroid (Figure 3). Those who were currently on treatment for any thyroid disease were 28 (2.7%), while those students who had taken treatment in the past medical history for thyroid disease were 39 (3.8%). All those students who themselves or their family members were diagnosed with a thyroid problem and who were taking/had taken any herbal remedy or any dietary supplement to benefit their thyroid disease constituted 3.2% (33) of all students as indicated in Table 4.
 |
Table 4 Thyroid Personal and Family History (n=1032) |
 |
Figure 3 Types of thyroid disease among students. |
Those students who had no or low risk of thyroid dysfunction were 406 (39.3%), those students who were at moderate risk were 379 (36.7%), while 247 (23.9%) had a high score and were at high risk of thyroid dysfunction (Table 5). All high-risk students were advised to visit a primary or secondary clinic with a physician to undergo further investigations for assessment of any underlying thyroid disease.
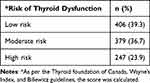 |
Table 5 Estimation of Thyroid Dysfunction Risk Based on Physical Assessment |
Table 6 details the association between thyroid risk levels and students’ gender and age. As shown in the table, there was a significant association between the age of the student and thyroid risk levels, where high risk was observed mostly among students aged between 15 and 20 years (31.2% n=148), compared to other age groups (p<0.001). Similarly, the thyroid risk levels were significantly associated with gender, where 26.5% of the females were associated with a high risk of thyroid, compared to males (22.8%) indicating significant association (p <0.001).
 |
Table 6 Association Between Students ‘Age and Gender in Relation to Thyroid Risk Levels |
The risk levels of the thyroid among students were significantly associated with the presence of comorbidities, high BP was higher among low-risk students, compared to moderate and high-risk students (p<0.001). The comorbidity of high BP was found to be higher among all the three risk levels of the students as shown in Figure 4. Similarly, the cholesterol levels were found to be high among moderate risk levels of the students compared to low-risk and high-risk students, indicating significant association (p<0.001) (Figure 4). As shown in Figure 5 herbal medicine consumption was significantly associated with risk levels of thyroid, indicating a significant association (p<0.001).
 |
Figure 4 Association between comorbidities and thyroid risk levels. |
 |
Figure 5 Association between consumption of herbal medicine versus risk levels of thyroid. |
To find out the relationship between the mean risk levels of thyroid, and student demographics, a multiple linear regression model was utilized in which gender, age, area of residence, monthly income, presence of comorbidities, family member diagnosed with thyroid, currently and ever treatment status for thyroid and consumption status of herbal medicine status were considered as explanatory variables and mean score of risk levels of thyroid the dependent variable. There was a significant association between age, gender, residential status, and the presence of family members diagnosed with thyroid with risk levels mean score of thyroid risk. The results of the regression model demonstrated that there was a significant relationship between the mean score of risk levels of thyroid and gender (p<0.001), age (p<0.001), and residential status (p<0.001) as shown in Table 7.
 |
Table 7 Regression Results of Thyroid Risk with Some Demographic Features of Students |
Discussion
The thyroid gland performs important functions like regulation of metabolism, growth of organs and body tissues as well as hemostatic functions. Although the risk of thyroid and its cancer is not fully understood20 certain predisposing risk factors have a major contribution like genetics, being female gender and living with chronic diseases, such as diabetes and graves diseases, and another factor.21 In this cross-sectional study of 1032, students were medically assessed for thyroid dysfunction. Many studies have shown the association of thyroid dysfunction with thyroid carcinoma as well as other cancer risks.22–24 Although previous studies like a cohort study showed a link between subclinical hypothyroidism with an increased risk of thyroid cancer incidence.25 On the other hand, previous results also revealed that untreated subclinical hypothyroidism may be associated with an increased risk of colorectal cancer.25 Similarly, another study showed a high incidence of thyroid cancer after being treated with radioactive iodine therapy.26 In addition, hyperthyroid patients receiving radioactive iodine treatment may have a little higher chance of developing cancer in the future. However, results regarding cancer mortality are more erratic, showing either no increased risk or a very slight absolute increase in risk.27
Thyroid dysfunction serious risk and was seen in about 7.6% of students, this finding is consistent with other studies where thyroid dysfunction was found in college students.28–30 For instance, Mohammed et al reported that 8.1% (n=395) of the students treated for hypothyroidism.28 Similarly, another previous study revealed that 41 (24.7%) subjects had positive results on thyroid disease screening, 24 (70.6%) students had solitary nodules, and 10 (29.4%) had multiple nodules.29 Likewise, another study among college students reported that 12.5% (n=1292) of the students had abnormal TSH. The overall prevalence of elevated TSH was 11% out of which 9.7% had mild TSH elevation. A low TSH was seen in 1.3% of the study population. These findings suggested that thyroid dysfunction is common among university students, and more particularly in females, since thyroid dysfunction is associated with difficulty in concentration, memory loss, fatigue, and other complications, which may raise the challenge for students in their education. Therefore, the findings suggest early detection and appropriate treatment can prevent the complications associated with it.
The risk of hypothyroidism poses a threat of infertility, loss of reproductive functions, and abnormalities in developing fetuses in the young population, especially females, and screening for thyroid disorders should be made a routine as a medical checkup. In this study, there are many female students, who are also listed as high-risk students for thyroid dysfunction. Thyroid function is an important parameter in pregnant women where it causes premature births and miscarriages. If this is left untreated, it causes mental and behavioral impairment in 60% of babies and congenital malformations in 20% of babies. It is also responsible for perinatal death.31 Our study shows that 23.9% of students were at high risk of thyroid dysfunction, which can lead to hypothyroidism or hyperthyroidism. In one of the studies conducted hypothyroidism can help in reducing the overall risk of breast cancer as well as improving the prognosis of breast cancer,22 but in another study, the results were inconsistent with the aforementioned study, and thyroid antibodies were found indicating autoimmune hypothyroidism contributed towards breast cancer risk.22 Thus, students having a high risk of thyroid dysfunction, especially the female population are at not only a risk for thyroid carcinoma but also other common malignancies.
In this study, the majority of students who participated in the medical camp were young, healthy, and active but still, some of the students reported having high cholesterolemia, hypertension, and angina. Some of them even had a combination of two or more of these serious medical problems. Thyroid dysfunction is found to raise the levels of total cholesterol, low-density lipoproteins (LDL), and triglycerides, hence leading to heart disease and increasing the risk of hypertension and cardiovascular events. Students presented with heart disease (angina), high cholesterolemia, and hypertension along with a high score of thyroid dysfunction may eventually lead to diagnosing thyroid-related signs and symptoms, which may lead them to develop serious medical conditions and mortality. The thyroid gland helps regulate the metabolism of the body and the disorder of the thyroid gland is a crucial health issue. Thyroid dysfunction leads to an increased level of lipids in the body.32 The direct link of hypothyroidism with hypertension is controversial, but the majority of them reported an increased prevalence of high BP in patients with diagnosed hypothyroidism33 but hypothyroidism is directly linked with hyperlipidemia.33,34 In this study, some of the students were suffering from DM which has an established link with thyroid disorder.35 Furthermore, obesity, hypertension, diabetes, and dyslipidemia have been associated with cancer incidence or mortality.35,36 In this study, the co-morbidities were recorded and included in the analysis, which is not found in other similar studies.30 Additionally, in the current findings, many students reported memory loss and depression which is consistent with other studies where thyroid dysfunction is linked with depression and dementia.37
The sample size was as large as possible, however, 30% of the sample did not finish the survey and was thus eliminated from the study, which is one of the study’s drawbacks. Second, because just one university in Abbottabad, Pakistan, participated in the study, the findings might not truly represent the risks that other undergraduates in Pakistan or other nations face. Third, due to a lack of funding for lab testing, blood TSH, T3, and T4 levels were not measured when individuals were physically evaluated in the medical camp. Lipid profile testing was also excluded. Even after adjusting for demographic, clinical symptom manifestation, socioeconomic, and lifestyle characteristics as in our analysis, there may still be residual confounding factors because this is an observational cross-sectional study. Despite these limitations, current findings have several benefits to get started, this study examines the value of individual’s health status in early thyroid illness screening to avoid issues related to thyroid. Additionally, there is a dearth of such research in the sector, particularly among students. However, utilizing the results of this kind of assessment, policymakers may be able to quickly examine societal issues and offer recommendations.
Conclusion
In conclusion, 7.6% of the students, had thyroid disease, and 23.9% of the students were found to have had a high risk of thyroid dysfunction. This study serves as a baseline for motivating people to get a medical checkup if their score is high without putting a cost burden on individuals. This study is specifically important for low-income populations and people from developing countries where thyroid blood testing, a costly process can be done secondary to this questionnaire medical assessment if the candidate’s score is high and is at potential risk of thyroid dysfunction. People from developing countries are not medically insured. It will eventually result in more people getting checked earlier, early diagnosis of thyroid dysfunction, early detection of thyroid gland malignancies, and overall decreased morbidity and mortality associated with thyroid carcinoma.
Data Sharing Statement
The data used to support the findings of this study is available from the corresponding author upon request.
Acknowledgments
The authors of this study extend their appreciation to Researchers Supporting Project (Project number RSP-2023/378), King Saud University, Riyadh, Saudi Arabia.
Funding
This study was supported by the Research Supporting Project, King Saud University, Riyadh Saudi Arabia, (RSP-2023/378) which provided funding for this work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Standing Committee on Screening. Population-Based Screening Framework Updated August; 2018.
2. To Screen or Not to Screen? - The Benefits and Harms of Screening Tests’. NIH News in Health. National Institutes of Health; 2017. Available from: https://newsinhealth.nih.gov/2017/03/screen-or-not-screen.
3. Vanderpump MP. The thyroid and its diseases: a comprehensive guide for the clinician. In: Epidemiology of Thyroid Disorders. Cham: Springer International Publishing; 2019:75–85.
4. Alqahtani SAM. Prevalence and Characteristics of Thyroid Abnormalities and Its Association with Anemia in ASIR Region of Saudi Arabia: a Cross-Sectional Study. Clin Pract. 2021;11(3):494–504. doi:10.3390/clinpract11030065.
5. Sohail R, Yasmin H, Tasneem N, et al. The Prevalence of Subclinical Hypothyroidism During Early Pregnancy in Pakistan: a Cross-Sectional Study. Cureus. 2021;13(12):e20316. doi:10.7759/cureus.20316.
6. Hu X, Chen Y, Shen Y, Tian R, Sheng Y, Que H. Global prevalence and epidemiological trends of Hashimoto’s thyroiditis in adults: a systematic review and meta-analysis. Front Public Health. 2022;10:1020709. doi:10.3389/fpubh.2022.1020709
7. American Thyroid Association. General Information/Press Room; 2017.
8. Syed W, Samarkandi OA, Alsadoun A, Harbi MK, Al-Rawi MB. Evaluation of clinical knowledge and perceptions about the development of thyroid cancer—an observational study of healthcare undergraduates in Saudi Arabia. Front Public Health. 2022;15(10):912424. doi:10.3389/fpubh.2022.912424
9. Liu F, Zhang X. Hypertension and obesity: risk factors for thyroid disease. Front Endocrinol. 2022;13:939367. doi:10.3389/fendo.2022.939367
10. Are you at risk for thyroid disease? Available from: https://www.everydayhealth.com/thyroid-conditions/evaluating-your-thyroid-disease-risk.aspx..
11. Demircioglu ZG, Demircioglu MK, Aygun N, et al. Relationship between thyroid-stimulating hormone level and aggressive pathological features of papillary thyroid cancer. Sisli Etfal Hastan Tip Bul. 2022;56(1):126–131. doi:10.14744/SEMB.2022.14554.
12. Su A, Zhao W, Wu W, et al. The association of preoperative thyroid-stimulating hormone level and the risk of differentiated thyroid cancer in patients with thyroid nodules: a systematic review and meta-analysis. Am J Surg. 2020;220(3):634–641. doi:10.1016/j.amjsurg.2020.01.009
13. Yeza EN, Mir CN, Ares RM, Pedrozo WR, Bonneau GA. Prevalence of thyroid dysfunction and its relationship with the lipid profile in patients at the Hospital of Encarnación. Rev cienc tecnol. 2021;36(1):70–77.
14. Pirahanchi Y, Toro F, Jialal I. Physiology, Thyroid Stimulating Hormone. Treasure Island (FL): StatPearls Publishing: 2023.
15. Javed R. Incidence of thyroid diseases in local population. Pak J Med Health Sci. 2023;17(1):17. doi:10.53350/pjmhs202317117
16. De Leo S, Lee SY, Braverman LE. Hyperthyroidism. Lancet. 2016;388(10047):906–918. doi:10.1016/S0140-6736(16)00278-6.
17. Khan M, Jose A, Sharma S. Physiology Parathyroid Hormone. Treasure Island (FL): StatPearls Publishing.; 2023.
18. Rizzo LFL, Mana DL, Serra HA. Drug-induced hypothyroidism. Medicina. 2017;77(5):394–404.
19. Billewicz WZ, Chapman RS, Crooks J, et al. Statistical methods applied to the diagnosis of hypothyroidism. Q J Med. 1969;38(150):255–266.
20. InformedHealth.org [Internet]. Cologne, Germany: institute for Quality and Efficiency in Health Care (IQWiG); 2006-. How does the thyroid gland work?; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279388/.
21. Mayo clinic. Hypothyroidism (underactive thyroid). Available from: https://www.mayoclinic.org/diseasesconditions/hypothyroidism/symptoms-causes/syc-20350284.
22. Yuan S, Kar S, Vithayathil M, et al. Causal associations of thyroid function and dysfunction with overall, breast and thyroid cancer: a two-sample Mendelian randomization study. Int J Cancer. 2020;147(7):1895–1903. doi:10.1002/ijc.32988.
23. Wang Z, Lin Y, Jiang Y, Fu R, Wang Y, Zhang Q. The associations between thyroid-related hormones and the risk of thyroid cancer: an overall and dose-response meta-analysis. Front Endocrinol. 2022;13:992566. doi:10.3389/fendo.2022.992566.
24. Song YS, Kim KS, Kim SK, Cho YW, Choi HG. Screening leads to overestimated associations of thyroid dysfunction and thyroiditis with thyroid cancer risk. Cancers. 2021;13(21):5385. doi:10.3390/cancers13215385
25. Gómez-Izquierdo J, Filion KB, Boivin JF, Azoulay L, Pollak M, Yu OHY. Subclinical hypothyroidism and the risk of cancer incidence and cancer mortality: a systematic review. BMC Endocr Disord. 2020;20(1):83. doi:10.1186/s12902-020-00566-9.
26. Shim SR, Kitahara CM, Cha ES, Kim SJ, Bang YJ, Lee WJ. Cancer risk after radioactive iodine treatment for hyperthyroidism: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(9):e2125072. doi:10.1001/jamanetworkopen.2021.25072
27. Evron JM, Esfandiari NH, Papaleontiou M. Cancer incidence and mortality following treatment of hyperthyroidism with radioactive iodine. Curr Opin Endocrinol Diabetes Obes. 2020;27(5):323–328. doi:10.1097/MED.0000000000000561.
28. Mohammed RA, Baqais OA, Basalib SG, et al. Hypothyroidism among college students and its association with academic performance: a cross-sectional study. Cureus. 2023;15:7.
29. Bafaraj S, Awad I, Jastaniah S, Abbas H, Musa A. Screening for thyroid diseases among students of applied medical sciences at King Abdulaziz University, Saudi Arabia. Saudi Med J. 2018;39(3):311–314. doi:10.15537/smj.2018.3.22137.
30. Velayutham K, Selvan SS, Unnikrishnan AG. Prevalence of thyroid dysfunction among young females in a South Indian population. Indian J Endocrinol Metab. 2015;19(6):781–784. doi:10.4103/2230-8210.167546.
31. Alexander EK, Pearce EN, Brent GA, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017;27(3):315–389. doi:10.1089/thy.2016.0457
32. Alhazmi RA, Alobaid AM, Althunayyan SM, Syed W, Al-Rawi MBA. A cross-sectional assessment of knowledge, awareness of risk factors, and perceptions of thyroid disease (TD) among adults living in Saudi Arabia - A community based study. Front Public Health. 2022;10:1041745. doi:10.3389/fpubh.2022.1041745.
33. Berta E, Lengyel I, Halmi S, et al. Hypertension in thyroid disorders. Front Endocrinol. 2019;10:482. doi:10.3389/fendo.2019.00482.
34. Mavromati M, Jornayvaz FR. Hypothyroidism-Associated Dyslipidemia: potential Molecular Mechanisms Leading to NAFLD. Int J Mol Sci. 2021;22(23):12797. doi:10.3390/ijms222312797.
35. Biondi B, Kahaly GJ, Robertson RP. Thyroid dysfunction and diabetes mellitus: two closely associated disorders. Endocr Rev. 2019;40(3):789–824. doi:10.1210/er.2018-00163.
36. Scully T, Ettela A, LeRoith D, Gallagher EJ. Obesity, type 2 diabetes, and cancer risk. Front Oncol. 2021;10:615375. doi:10.3389/fonc.2020.615375.
37. Elbadawy AM, Mansour AE, Abdelrassoul IA, Abdelmoneim RO Relationship between thyroid dysfunction and dementia. Egypt J Intern Med 2020;32:1–9. doi:10.1186/s43162-020-00003-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
