Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 16
Navigating the New EU Medical Devices Regulation: Retrospective Post-Market Follow-Up of Hyaluronic Acid Injections for Knee Osteoarthritis
Authors Alcina Navarro A, Gómez Valero S, Gimeno del Sol M , Coronel Granado MP
Received 14 November 2023
Accepted for publication 29 February 2024
Published 21 March 2024 Volume 2024:16 Pages 67—73
DOI https://doi.org/10.2147/OARRR.S446572
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Chuan-Ju Liu
Alejandro Alcina Navarro,1 Sara Gómez Valero,1 Mercedes Gimeno del Sol,2 María Pilar Coronel Granado2
1Rehabilitation Department, Hospital Universitario del Henares, Coslada, Madrid, Spain; 2Scientific Department, Meiji Pharma Spain, Alcalá de Henares, Madrid, Spain
Correspondence: María Pilar Coronel Granado, Scientific Department, Meiji Pharma Spain, Avda de Madrid, 94, Alcalá de Henares, Madrid, 28802, Spain, Tel +34 91 8870980, Email [email protected]
Purpose: The entry into force of the new Medical Device Regulation (EU) 2017/745 highlights the need for post-market clinical follow-up to ensure the safety and efficacy throughout the life cycle of medical devices. This study evaluates the efficacy and safety of a single intra-articular hyaluronic acid injection in knee osteoarthritis in real-world conditions, over a six-month period, aligning with the summary of safety and clinical performance (SSCP) required by the new regulation.
Patients and Methods: Patients over 18 years of age with knee osteoarthritis, treated with a single injection of HA (Adant® One, Meiji Pharma Spain, Spain) at a 3rd level hospital. Patients were treated and followed between January 1, 2020 and June 30, 2022. Demographic, clinical, and treatment-related data were collected, and efficacy regarding pain relief and/or function improvement was assessed using a Likert-type scale. Data were pseudo-anonymized and the comparison was performed using Fisher’ or Mann Whitney’ test. The study was approved by the Ethics Review Board of the Hospital Puerta de Hierro (Madrid, Spain).
Results: We followed 20 patients with knee osteoarthritis, with a mean age of 61 years, 80% women, and with a high burden of comorbidities (90%). A total of 60% of patients presented Kellgren-Lawrence grade III–IV. Four patients (20%) returned before 6 months due to lack of efficacy. Of the other patients, 65% showed a clinical response that lasted more than 12 months in 38.5% of cases. Time until medical appointment and taking concomitant medication for knee osteoarthritis were associated with better clinical response (p < 0.05).
Conclusion: The administration of a Adant® One single intra-articular hyaluronic acid injection in knee osteoarthritis is effective, safe, and maintains the improvement over a six-month period. Our findings also emphasize the need of using standardized tools for accurate efficacy assessment and optimal patient care.
Keywords: rehabilitation, real clinical practice, rheumatology, traumatology
Introduction
Osteoarthritis (OA) is a degenerative joint disorder characterized by the progressive deterioration of all joint structures (cartilage, meniscus, subchondral bone, infrapatellar fat pad and synovial membrane) leading to incapacitating pain and functional impairment. This pathology is also characterized by synovial membrane inflammation, subchondral sclerosis, and osteophyte formation.1–3 Furthermore, OA can lead to neurological changes that leads to neuropathic pain and enhanced pain sense.4 Several risk factors have been identified as central to the development and progression of knee OA, including aging, female sex, genetic alterations, comorbidities, previous knee injuries and excessive mechanical stress on the joint.5,6 Symptomatically, OA is characterized by chronic pain, joint stiffness and decreased functionality, affecting the quality of life and being one of the main causes of mobility dependency and disability worldwide.7,8
The prevalence of OA is a growing concern, given the aging population. Recent studies have shown an upward trend in the global prevalence of OA, increasing to 113.25% from 1990 to 2019,9 and being the knee the most affected joint.10 In addition to the deterioration in the quality of life of patients,11 knee OA also places a growing burden on the health system and involves a major economic expense, both for the medical resources, and for other expenses derived from the pathology (due to loss of work capacity, dependence).12,13
Currently, treatments for OA are focused on symptomatic alleviation or slowing the progression of the disease, and can be both non-pharmacological (ie, education, exercise, weight loss, assistive devices, physical therapy and dry-needling)14–16 and pharmacological (such as paracetamol, oral and topical non-steroidal anti-inflammatory drugs (NSAIDs), intra-articular (IA) corticosteroids, or IA hyaluronic acid).17,18 Viscosupplementation with hyaluronic acid (HA), is a widely extended therapeutic approach for the treatment of knee OA.19–22 Hyaluronic acid is a physiological component of synovial fluid with mechanical properties such as lubrication and shock absorption, that also favor joint environment homeostasis.23,24 Multiple studies have demonstrated the effectivity and safety of the use of IA AH in knee OA, reducing pain and improving joint functionality.25–29 Furthermore, from 2003 the recommendations for the use of IA AH in the Clinical Practice Guidelines (CPGs) have significantly increased, and currently more than 70% of the CPGs favorably recommend the use of IA AH in the treatment of OA.30 Single injection HA viscosupplementation therapy offers several advantages to patients and health system compared to multiple injection schemes, requiring fewer visits to the physician, reducing treatment-related costs, improving adherence to therapy, and having less risk of adverse events.
The new Regulation (EU) 2017/745 on Medical Devices31 highlights, among the outstanding novelties, the need of conducting clinical investigations, not only for product registration but also once the product is in the market, as a part of a post-marketing clinical follow-up plan. In order to comply with this regulation, we designed a post-market study to further assess the clinical performance and safety of a hyaluronic acid-based product (a single injection of 4.9 mL of non-crosslinked HA at 1%, with molecular weight of 1000 kDa, obtained by biofermentation) in patients with knee OA. The study focused on assessing the product’s effectiveness in alleviating pain and/or improving function under real-world clinical conditions. We hypothesized that the administration of intraarticular HA would lead to a significant reduction in pain levels and/or an improvement in knee function compared to baseline. Furthermore, we aimed to further assess the safety profile of the product in this patient population. By elucidating these objectives and hypotheses, our study seeks to contribute valuable insights into the real-world clinical performance of the HA-based product, thereby fulfilling the regulatory requirements outlined in Regulation (EU) 2017/745.
Materials and Methods
Ethics
To conduct the study, approval was requested from the Ethics Review Board of the Hospital Puerta de Hierro (Madrid, Spain) (date of approval 20/06/2022). The Ethics Review Board granted an exemption from obtaining informed consent from patients due to the characteristics of the study and the anonymous treatment of the data. The study complies with the Declaration of Helsinki.
Study Design
Observational, cross-sectional, retrospective, post-marketing clinical study in a cohort of patients treated with IA HA for knee OA. The treatment consisted of a single injection of HA (Adant® One). IA HA injections were administered through lateral midpatellar (LMP) approach under aseptic conditions. The injection site was covered with a sterile patch and passive flex extension movements of the treated knee were performed. All patients were advised relative rest and intermittent local cold after injection and, if necessary, routine analgesia. Inclusion criteria included men and women aged ≥ 18 years, with clinical and radiological diagnosis of knee OA according to Kellgren-Lawrence, treated in the hospital between January 1st 2020 and June 30th 2022. Exclusion criteria were age under 18 years, and patients treated outside the established dates. Patients were followed according to the usual protocol.
Outcome Measures
For each patient, the following clinical history information was obtained: age, sex, employment status, diagnosis, laterality of the OA, Kellgren-Lawrence grade32 in treated knee, pain, date of injection, other diseases besides OA, concomitant medication (both for OA and for other diseases), adverse events detected after infiltration (pathologies, accidents, falls, surgeries), information regarding patient follow-up (time of appointment request).
The above information was included in a database for further statistical analysis. The data were pseudo anonymized and identified by a code, so there is not information that can identify patients.
Efficacy of single injection of hyaluronic acid and duration of effects were defined as primary outcomes. Improvement was assessed using a Likert-type scale by which patients assessed the improvement in their pain and/or function. This scale was divided into four levels: no improvement, partial improvement, improvement and great improvement. Due to the small sample size, for statistical analysis the data were grouped into improvement (partial improvement, improvement and great improvement) and no improvement. For the duration of effects, the time elapsed from the administration of the injection until the patient asked for a new appointment was considered.
Demographic information, comorbidities, concomitant treatments, and adverse events following IA injection (pathologies, accidents, falls, or surgeries) were also analyzed.
Statistics
Qualitative variables have been described using absolute frequencies and percentages. Quantitative variables that conform to a normal distribution have been described by mean, standard deviation (SD), minimum (Min) and maximum (Max). For those variables that do not conform to a normal distribution according to the Kolmogorov’s test, it has been decided to maintain the use of means and SD to simplify the presentation of the results.
Univariate comparisons between categorical variables have been made using Fisher’s exact test. For continuous variables, the shape of the distributions has been analyzed using Kolmogorov’s test, and comparisons have been made using Mann–Whitney U-test.
Statistical significance was set at p < 0.05. For statistical analysis, SPSS software, version 14, was used.
Results
A total of 20 patients treated and followed-up from January 2020 to June 2022 were included in the study. Sociodemographic and clinical characteristics of the patients are shown in Table 1. The patients’ mean age was 61.05 years (± 16.11 years) with a minimum of 27 years and a maximum of 85 years, 80% were female, and 55% were non-active.
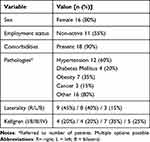 |
Table 1 Sociodemographic and Clinical Variables. |
The Kellgren-Lawrence OA grades32 presented by patients were mainly III–IV (60%), with mostly unilateral involvement (45% in the right knee, and 40% in the left knee), but with 3 cases of bilateral involvement (15%), resulting in the inclusion of a total of 23 knees. Moreover, 60% of patients had previously received treatment with IA AH injections: 10 on one occasion (50%), 1 on two occasions (5%), and 1 on three occasions (5%). There was is a high rate of comorbidities (90%) with the associated pharmacological treatments (the predominant ones being antihypertensives, psychotropic drugs, hypocholesterolemic agents and oral antidiabetics) (Table 2).
 |
Table 2 Pharmacological Treatments |
All patients were taking concomitant medication for OA pain (Table 2), consuming 1, 2 or 3 medications (30%, 50% and 20%, respectively), with the most frequent treatments being paracetamol (65%) and other analgesics (50%). Also, the consumption of opioids (40%) outstands over NSAIDs (30%).
Throughout the follow-up period, 80% of patients attended their medical appointment after 6 months. Further analysis showed that the improvement exceeded 12 months in almost 40% of these patients. When performing the bivariate comparative analysis between improvement and no improvement patients, only significant differences were found in the use of concomitant treatments for OA and the time a new appointment request (Table 3). Patients who improved took a mean of 2.15 concomitant treatments (SD = 0.69) while those who did not improve took a mean of 1.43 (SD = 0.53) (p = 0.031). In the case of patients who improved, the mean time to request a new appointment was 316 days (SD = 160), while in the case of patients who have not shown improvement it was 160 days (SD = 70) (p = 0.032).
 |
Table 3 Bivariate Comparative Analysis Results |
Regarding safety, patients did not report adverse events related to the administration of IA HA. There were two cases in which patients required knee surgery (a prosthesis implantation 19 months after injection, and a meniscectomy 10 months after injection).
Discussion
Intra-articular administration of HA is a widely employed treatment for knee OA. This approach has garnered substantial attention due to its reported ability to mitigate pain and enhance join function, offering a non-surgical alternative to conventional interventions.20,25,30 Several clinical studies have endeavored to assess the efficacy and safety profile of IA HA, concluding that its efficacy is superior to placebo and has an exceptional safety profile.25,26,28,29 In addition, IA HA injections, due to their long-term effectivity and scarce adverse events, have advantages over other intra-articular treatments and it is recommended by more than 70% of the CPGs.30 On the other hand, there are clinical studies that point out the lack of efficacy of intra-articular injections of HA,33 and the efficacy and duration of the effects following intra-articular HA injections is a topic of debate, with published studies often reaching conflicting conclusions. However, it is pivotal to consider that there are many HA-based products with varying molecular weights, concentrations, cross-linking, injection volume, and sources, which have been shown to potentially impact their efficacy and safety,34 and therefore cannot be considered equivalent and should be assessed independently.
This study has assessed the efficacy and duration of effects of a single IA HA injection in knee OA during a clinical follow-up period over 12 months. The patients included in the study, mainly women with a high burden of comorbidities (90%), are an accurate representation of the overall population with knee OA.9 During the study, intra-articular administration of HA was carried out by lateral midpatellar (LMP) via, since this approach has previously been shown to have a high accuracy rate (93%), as long as it is conducted by a qualified professional.35 After the administration of IA-AH, a good clinical response was showed even in patients with Kellgren-Lawrence III–IV grades (61.5% of these patients showed improvement). Furthermore, despite possible adverse events described in the product information (such as skin rash or swelling and pain at the injection site) no complications were reported by patients, highlighting the excellent safety profile of IA AH injections. During the study two statistically significant variables related to improvement/non-improvement were identified: consumption of concomitant medication for knee OA, which was higher in patients who showed improvement, and the days until appointment request, which increased in case of good clinical response.
While it is indicated that the Adant® One single injection effect lasts for 6 months, this study has shown that the clinical improvement can last between 6 and 12 months, and even exceed 12 months. A single intra-articular injection of hyaluronic acid presents several advantages over multiple injections in the context of knee OA management. Firstly, the single-injection approach offers enhanced patient adherence, as it reduces the burden of frequent clinic visits. It also minimizes the risk of infection or complications related to repetitive injections, and the potential adverse effects such as pain or swelling at the administration site.
Regarding the clinical implications, the long-term efficacy of the product showed along the study suggests that a single HA injection can provide sustained symptom relief, reducing the need for frequent visits and increasing treatment adherence. Furthermore, the sustained effect of the product may reduce the use of concomitant medication, which is especially relevant in populations in which the use of NSAIDs or corticosteroids is contraindicated. These findings also underscore the importance of individualized assessment and the need to use objective measures to evaluate treatment efficacy in clinical practice.
The entry into force of Regulation (EU) 2017/745 on Medical Devices31 has meant a paradigm shift in the clinical investigations with medical devices and their follow-up after registration as this Regulation emphasizes proactive measures to ensure safety and efficacy throughout its life cycle. By imposing rigorous post-market surveillance requirements, the EU strives to strengthen patient safety, encourage continuous product improvements and provide a rapid response to emerging safety concerns. In this context, the study we have conducted, with its remarkable novelty and relevance, underscores the importance of adherence to the new regulation and highlights its usefulness as a fundamental resource to improve clinical decision-making for the benefit of patients and public health.
Strengths and Limitations
Our study reliably represents the daily clinical practice in the Hospital’s Rehabilitation Department for the treatment of patients with moderate-severe knee OA. Nevertheless, the low number of patients included is the main limitation. In addition, it should be noticed that the period of patients’ recruitment and follow-up periods includes the Covid-19 pandemic times. The study started in January 2020 and shortly after the Covid-19 pandemic was declared worldwide (March 13th in Spain). For the next few months, the frequency of medical appointments was reduced both by the hospital due to restrictions and overload, and by patients due to fear of possible contagion, and multiple appointments were delayed until months later. Total normality did not occur until early 2022, and thus a great disparity in the dates of post-infiltration review was generated. Another limitation of the study stems from the subjective way to measure treatment efficacy. However, this reflects routine clinical practice and underscores the need to implement an objective assessment of treatment efficacy in real-world practice.
Conclusion
The administration of HA in knee OA is effective, safe, and it is characterized by its straightforward and routine administration in a Rehabilitation Service whenever and when it is administered by a qualified professional. The findings of our study demonstrate than in 80% of cases the administration of a single injection of Adant® One maintains an improvement at least over six-month period on knee OA symptoms. Our findings also highlight the need to employ standardized assessment tools in routine clinical practice to accurately measure the effectiveness of interventions and ensure optimal individualized patient care.
Acknowledgments
The authors thank Dr. J.J. Granizo (Granadatos S.L.) for the statistical analysis of the results.
Funding
This study was funded by Meiji Pharma Spain (MPS).
Disclosure
MP. Coronel and M. Gimeno del Sol are employees of Meiji Pharma Spain. The other authors report no conflicts of interest in this work.
References
1. Martel-Pelletier J, Barr AJ, Cicuttini FM, et al. Osteoarthritis. Nat Rev Dis Primers. 2016;2(1):16072. doi:10.1038/nrdp.2016.72
2. Herrero-Beaumont G, Pérez-Baos S, Sánchez-Pernaute O, Roman-Blas JA, Lamuedra A, Largo R. Targeting chronic innate inflammatory pathways, the main road to prevention of osteoarthritis progression. Biochem Pharmacol. 2019;165:24–32. doi:10.1016/j.bcp.2019.02.030
3. Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–1759. doi:10.1016/S0140-6736(19)30417-9
4. Iuamoto LR, Ito FLK, Tomé TA, et al. Effects of neuroplasticity in people with knee osteoarthritis: a systematic review of the literature. Medicine. 2022;101(3):e28616. doi:10.1097/MD.0000000000028616
5. Abramoff B, Caldera FE. Osteoarthritis: pathology, diagnosis, and treatment options. Med Clin North Am. 2020;104(2):293–311. doi:10.1016/j.mcna.2019.10.007
6. Deveza LA, Melo L, Yamato TP, Mills K, Ravi V, Hunter DJ. Knee osteoarthritis phenotypes and their relevance for outcomes: a systematic review. Osteoarthritis Cartilage. 2017;25(12):1926–1941. doi:10.1016/j.joca.2017.08.009
7. Vongsirinavarat M, Nilmart P, Somprasong S, Apinonkul B. Identification of knee osteoarthritis disability phenotypes regarding activity limitation: a cluster analysis. BMC Musculoskelet Disord. 2020;21(1):237. doi:10.1186/s12891-020-03260-y
8. Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–656.
9. Long H, Liu Q, Yin H, et al. Prevalence trends of site-specific osteoarthritis from 1990 to 2019: findings from the global burden of disease study 2019. Arthritis Rheumatol. 2022;74(7):1172–1183. doi:10.1002/art.42089
10. Yang G, Wang J, Liu Y, et al. Burden of Knee Osteoarthritis in 204 Countries and Territories, 1990–2019: results from the global burden of disease study 2019. Arthritis Care Res. 2023:2. doi:10.1002/acr.25158
11. van Schoor NM, Zambon S, Castell MV, et al. Impact of clinical osteoarthritis of the Hip, knee and hand on self-rated health in six European countries: the European Project on OSteoArthritis. Qual Life Res. 2016;25(6):1423–1432. doi:10.1007/s11136-015-1171-8
12. Leifer VP, Katz JN, Losina E. The burden of OA-health services and economics. Osteoarthritis Cartilage. 2022;30(1):10–16. doi:10.1016/j.joca.2021.05.007
13. Puig-Junoy J, Ruiz Zamora A. Socio-economic costs of osteoarthritis: a systematic review of cost-of-illness studies. Semin Arthritis Rheum. 2015;44(5):531–541. doi:10.1016/j.semarthrit.2014.10.012
14. Sinatti P, Sánchez Romero EA, Martínez-Pozas O, Villafañe JH. Effects of patient education on pain and function and its impact on conservative treatment in elderly patients with pain related to hip and knee osteoarthritis: a systematic review. Int J Environ Res Public Health. 2022;19(10):6194. doi:10.3390/ijerph19106194
15. Sánchez-Romero EA, González-Zamorano Y, Arribas-Romano A, et al. Efficacy of manual therapy on facilitatory nociception and endogenous pain modulation in older adults with knee osteoarthritis: a case series. Appl Sci. 2021;11(4):1895. doi:10.3390/app11041895
16. Sánchez Romero EA, Fernández-Carnero J, Calvo-Lobo C, Ochoa Sáez V, Burgos Caballero V, Pecos-Martín D. Is a combination of exercise and dry needling effective for knee OA? Pain Med. 2019. doi:10.1093/pm/pnz036
17. Bruyère O, Honvo G, Veronese N, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Semin Arthritis Rheum. 2019;49(3):337–350. doi:10.1016/j.semarthrit.2019.04.008
18. Overton C, Nelson AE, Neogi T. Osteoarthritis Treatment Guidelines from Six Professional Societies: similarities and Differences. Rheum Dis Clin North Am. 2022;48(3):637–657. doi:10.1016/j.rdc.2022.03.009
19. Trojian TH, Concoff AL, Joy SM, Hatzenbuehler JR, Saulsberry WJ, Coleman CI. AMSSM scientific statement concerning viscosupplementation injections for knee osteoarthritis: importance for individual patient outcomes. Br J Sports Med. 2016;50(2):84. doi:10.1136/bjsports-2015-095683
20. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, Hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589. doi:10.1016/j.joca.2019.06.011
21. Conrozier T, Diraçoglù D, Monfort J, et al. EUROVISCO good practice recommendations for a first viscosupplementation in patients with knee osteoarthritis. Cartilage. 2023;14(2):125–135. doi:10.1177/19476035221138958
22. Conrozier T, Monfort J, Chevalier X, et al. EUROVISCO recommendations for optimizing the clinical results of viscosupplementation in osteoarthritis. Cartilage. 2018;11(1):47–59. doi:10.1177/1947603518783455
23. Costa FR, Costa Marques MR, Costa VC, et al. Intra-articular hyaluronic acid in osteoarthritis and tendinopathies: molecular and clinical approaches. Biomedicines. 2023;11(4):1061. doi:10.3390/biomedicines11041061
24. Altman RD, Manjoo A, Fierlinger A, Niazi F, Nicholls M. The mechanism of action for hyaluronic acid treatment in the osteoarthritic knee: a systematic review. BMC Musculoskelet Disord. 2015;16(1):321. doi:10.1186/s12891-015-0775-z
25. Maheu E, Rannou F, Reginster JY. Efficacy and safety of hyaluronic acid in the management of osteoarthritis: evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45(4, Supplement):S28–S33. doi:10.1016/j.semarthrit.2015.11.008
26. Navarro-Sarabia F, Coronel P, Collantes E, et al. A 40-month multicentre, randomised placebo-controlled study to assess the efficacy and carry-over effect of repeated intra-articular injections of hyaluronic acid in knee osteoarthritis: the AMELIA project. Ann Rheum Dis. 2011;70(11):1957. doi:10.1136/ard.2011.152017
27. Yaftali NA, Weber K. Corticosteroids and Hyaluronic Acid Injections. Clin Sports Med. 2019;38(1):1–15. doi:10.1016/j.csm.2018.08.006
28. Gavín C, Blanco FJ, Pablos JL, et al. One-year, efficacy and safety open label study, with a single injection of a new hyaluronan for knee OA: the SOYA trial. J Pain Res. 2021;14:2229–2237. doi:10.2147/JPR.S321841
29. Lee CL, Wang YC, Huang HT, Chen CH, Chang KL, Tien YC. Efficacy of Intra-articular injection of biofermentation-derived high-molecular hyaluronic acid in knee osteoarthritis: an ultrasonographic study. Cartilage. 2022;13(1):19476035221077404. doi:10.1177/19476035221077404
30. Phillips M, Bhandari M, Grant J, et al. A systematic review of current clinical practice guidelines on intra-articular hyaluronic acid, corticosteroid, and platelet-rich plasma injection for knee osteoarthritis: an international perspective. Orthop J Sports Med. 2021;9(8):23259671211030270. doi:10.1177/23259671211030272
31. Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices, Amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and Repealing Council Directives 90/385/EEC and 93/42/EEC; 2017:1–175. Available from: http://data.europa.eu/eli/reg/2017/745/oj.
32. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi:10.1136/ard.16.4.494
33. van der Weegen W, Wullems JA, Bos E, Noten H, van Drumpt RAM. No difference between intra-articular injection of hyaluronic acid and placebo for mild to moderate knee osteoarthritis: a randomized, controlled, double-blind trial. J Arthroplasty. 2015;30(5):754–757. doi:10.1016/j.arth.2014.12.012
34. Altman RD, Bedi A, Karlsson J, Sancheti P, Schemitsch E. Product differences in intra-articular hyaluronic acids for osteoarthritis of the knee. Am J Sports Med. 2015;44(8):2158–2165. doi:10.1177/0363546515609599
35. Jackson DW, Evans NA, Thomas BM. Accuracy of needle placement into the intra-articular space of the knee. JBJS. 2002;84(9). doi:10.2106/00004623-200209000-00003
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
