Back to Journals » Journal of Inflammation Research » Volume 16
Myeloid/Lymphoid Neoplasms with ETV6::PDGFRB Fusion Gene: A Rare Case of Poor Response to Imatinib and Possible Transformation Mechanisms from Myeloid Neoplasms of Bone Marrow to T-Cell Lymphoblastic Lymphoma Invasion in Lymph Nodes
Authors Gou Y, Tang Y, Liu S, Cheng S, Deng X, Wen Q, Feng Y, Peng X, Wang P, Zhang X
Received 24 July 2023
Accepted for publication 20 September 2023
Published 11 November 2023 Volume 2023:16 Pages 5163—5170
DOI https://doi.org/10.2147/JIR.S427995
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Yang Gou,* Yongjie Tang,* Shuiqing Liu, Siyu Cheng, Xiaojuan Deng, Qin Wen, Yimei Feng, Xiangui Peng, Ping Wang, Xi Zhang
Medical Center of Hematology, Xinqiao Hospital of Army Medical University, Chongqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ping Wang, Medical Center of Hematology, The Xinqiao Hospital of Army Medical University, Chongqing, People’s Republic of China, Email [email protected]
Abstract: The ETV6::PDGFRB fusion gene is commonly reported in chronic myelomonocytic leukemia with eosinophilia, yet patients with ETV6::PDGFRB presenting myeloid and lymphoid neoplasms successively have not been reported. Here, we report the first case of a 35-year-old man with myeloid and lymphoid neoplasms harboring an ETV6::PDGFRB fusion gene who demonstrated poor response to imatinib. The patient was diagnosed with an ETV6::PDGFRB fusion gene myeloid neoplasm on initial diagnosis at our hospital. After 5 months of treatment with imatinib, he was diagnosed with T-cell lymphoblastic lymphoma. ETV6::PDGFRB turned negative after increasing the dose of imatinib, but enlarged superficial lymph nodes reappeared the following year. Notably, the patient exhibited a worse response to imatinib treatment. This study describes this rare case and speculates on a possible mechanism.
Keywords: ETV6, PDGFRB, fusion, myeloid/lymphoid neoplasms, imatinib
Introduction
The ETV6::PDGFRB fusion gene is commonly associated with myeloid neoplasms with monocytosis (such as CMML), and with eosinophilia.1 The PDGFRB gene, located on 5q33, encodes PDGFRβ, a type III tyrosine kinase comprising an extracellular domain consisting of five immunoglobulin (Ig)-like domains, a single-transmembrane helix domain, a juxtamembrance domain, and an intracellular tyrosine kinase domain.2 PDGFRB can fuse with >30 partner genes (ETV6 being the most commonly seen) and result in a constitutive activation of the tyrosine kinase domain, despite extracellular signals, and give rise to an uncontrolled proliferation of blood cells, mostly later-stage myeloid cells, and less frequently immature B- or T-lymphoid cells.2 The ETV6::PDGFRB fusion gene with lymphoid blasts is rarely seen and less frequently reported in the literature.1,2
In the past, the aim of treatment was to limit organ damage by controlling the eosinophil count using drugs like prednisone, hydroxyurea, and IFNα. Since imatinib, a TKI first approved for the treatment of chronic myeloid leukemia by inhibiting ABL kinase activity, was discovered to block PDGF receptors at even lower concentrations in 2002, the prognosis of PDGFRB-rearrangement neoplasms was revolutionized.3 Patients with ETV6::PDGFRB exhibit an excellent response to imatinib, with much less frequent transform to blastic crisis phase.3,4 It is challenging for clinicians to treat patients with poor response to target therapy, and even disease transformation can occurr.
Here, we report a rare case of ETV6::PDGFRB that manifested initially as a myeloid neoplasm and was treated with imatinib, but then an invasion of lymphoblastic T cells was found on lymph node (LN) biopsy. The patient got better after a course of chemotherapy and an increasing dose of imatinib, but enlarged superficial LNs reappeared the following year. Notably, the patient exhibited a worse response to imatinib treatment. This study describes this rare case and speculates on a possible mechanism, displays the complexity of targeting fusion genes, and highlights the need for a comprehensive understanding of the molecular basis of neoplasms and personalized therapeutic strategies.
Case Presentation
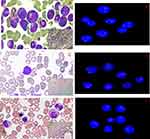
A 35-year-old man with a history of IgA nephropathy was followed up in our hospital. A bone marrow (BM) aspiration biopsy was done when a significant leukocytosis (WBCs 26×109/L) and eosinophilia (nucleated cells [eosinophils] 12.5%) was observed on complete blood count. A marked myeloid hyperplasia with 5% myeloblasts and 3% eosinophils was found in the BM aspirate smear, while lymphoid was hypoplasia with only 1.5% of mature lymphocytes counted (Figure 1A). A positive ETV6::PDGFRB fusion gene and negative BCR/ABL was found on RTq-PCR, PDGFRB gene breakage of 90% of cells was detected by FISH (Figure 1B), and karyotype analysis showed 46, XY, del(12) (p13p11.2), indicative of a diagnosis of myeloid neoplasms with ETV6::PDGFRB fusion gene. After hydroxyurea (Qilu Pharma, China; 1.5 g/day) for 4 days, followed by imatinib (Hansoh Pharma, China) 200 mg/day, his WBCs and eosinophils had normalized within a month, then imatinib was decreased to 100 mg/day. Five months after initial diagnosis, an enlargement of LNs was found after a cold in his bilateral neck, axilla and groin. Ultrasound examination showed the max LN was 3.7×1.5 cm in zone II of the right neck with a regular shape and clear border. Biopsy of the max LN revealed intermediate blastoid infiltration by neoplastic lymphocytes. Immunohistochemical analysis of lymphoma cells showed CD34+, CD10+, CD3+, CD7+, and Tdt+ scattered, leading to a diagnosis of T-LBL. At the same time, the BM aspirate showed a hypocellularity with 11.5% blasts (Figure 1C), and 24% PDGFRB breakage cells on FISH (Figure 1D). The karyotype was normal at this time.
Imatinib was increased to 400 mg/d, and induction chemotherapy with PCIOD (asparaginase, cyclophosphamide, idarubicin, vindesine, dexamethasone) was begun. Shrunken LNs after chemotherapy, but a severe pulmonary fungal infection occurred in the process, and an impaired renal function arose, then imatinib was decreased to 200 mg/day (after 1 month of 400 mg/day). WBC and eosinophil counts reached normality gradually. The BM aspirate was normal, and hypocellularity and PDGFRB breakage detection in BM was negative on FISH 1 year after initial diagnosis and remained negative on follow-up (Figure 1E and F). However, 14 months after initial diagnosis, an enlargement of his LNs was detected in his bilateral neck, axilla, and groin again. Maximum sizes were 1.4–1.8×0.6–0.9 cm on ultrasound. Impacted by the COVID-19 situation in our city, 200 mg/day imatinib was continued. Enlarged LNs kept stable relative to 1 month before manuscript submission (20 months after initial diagnosis). For further treatment decisions and understanding the pathogenesis of this disease, more experiments were done.
Methods
Serial BM and LN samples were collected for FCM, FISH, and DNA and RNA sequencing at three time points: (A) first diagnosis of myeloid/lymphoid neoplasm, abbreviated as diagnosis; (B) lymphoblastic T-cell invasion in LNs, abbreviated as invasion; and (C) 1 year after diagnosis, when PDGFRB breakage cells in BM had turned negative on FISH, abbreviated as CR. FCM immunophenotyping analyses were performed using 10-color flow cytometry (Navios, Beckman Coulter, USA). FISH analyses were performed on unstimulated interphase cells using dual-color break-apart probes (D-FISH, Jinpujia, China; CSF1R signal red, PDGFRB signal green, two yellow signals represent PDGFRB without breakage, one red, one green, and yellow signals represent one PDGFRB breakage detected) according to the manufacturer’s instructions. Targeted DNA sequencing and RNA sequencing were performed with the NovaSeq 6000 sequencing platform (Illumina, USA) and high-throughput Sanger sequencing using an ABI 3730 automated DNA sequencer (Applied Biosystems, USA). Total genomic DNA and RNA was extracted from BM and LN samples for target sequencing, and 38 genes commonly mutated in myeloid neoplasms were investigated with a custom-designed next-generation sequencing approach for library construction (Yuanqi, China). RNA-sequencing libraries were prepared using the TruSeq Stranded Total RNA Library Prep Kit (Illumina, USA) following the manufacturer’s instructions. P< 0.05 and log2-fold change >2 were considered to be significantly differentially expressed. GO and KEGG pathway enrichment analysis was performed using KOBAS (http://kobas.cbi.pku.edu.cn) and DAVID (https://david.ncifcrf.gov).
Results
At diagnosis, FCM analysis showed one progenitor-cell population with CD34par+CD38+CD117+CD7-CD56par+cMPO+CD123dimHLA-DR+cCD3- in the BM sample (Figure 2A). Upon invasion, progenitor-cell populations were CD34+CD38+CD117par+CD7+CD56+cMPOpar+CD123+HLA-DR+cCD3- in the BM sample (Figure 2B) and CD34+CD38+CD117±CD7+CD56+cMPOfew+ CD123+ HLA-DR-cCD3+ in the LN sample (Figure 2C). Once it was that found blast cells coexpressed cMPO and cCD3 simultaneously in the LN sample upon invasion, a CD117 gate was used, and the results showed CD117-positive cells (red cells, accounting for 13.93% of nuclear cells) were positive for cMPO and cCD3 (a mixed T and myeloid phenotype), CD117 negative cells were cMPO-negative and cCD3-positive (blue cells, accounting for 69% of nuclear cells) (T-LBL phenotype) (Figure 2C). In LNs during invasion, the imprint cytology image showed intermediate blastoids with intermediate-to-condensed chromatin and scant cytoplasm (Figure 2D). FISH detected a break in 64% of the cells from the invaded LNs (Figure 2E).
NPM1 and TET2 mutations were positive at diagnosis and negative at invasion in the BM sample, while TET2 mutation was positive at invasion in LN samples. NOTCH3 p. R2031H mutation kept positive but changed the VAF at diagnosis, while VAFs of CHD8, MUC16 and PLCG2 remained close to 50% in samples at diagnosis and invasion. Additionally, MED12 mutation was detected at invasion in the LN sample (Table 1). RNA sequencing demonstrated the same break points in ETV6::PDGFRB fusion (12:12006495:+-5:149510225:-) between the BM sample and LN sample.
 |
Table 1 Major gene mutations detected in the disease course |
RNA sequencing revealed some important expression changes in BM samples between diagnosis and CR (Figure 3). GO functional enrichment analysis revealed that stem cell–related genes had higher expression at diagnosis, such as embryonic organ development and morphogenesis, cell-fate commitment, and signaling pathways regulating pluripotency of stem cells. Neutrophil-related genes in terms of neutrophil activation, neutrophil-mediated immunity, and neutrophil degranulation were more highly expressed during CR. Additionally, KEGG functional analysis revealed that some signaling pathway conduction had also changed, with more gene expression related to the NOTCH pathway, MAPK signaling, PI3K signaling, and less gene expressions related to NF-B signaling at diagnosis.
Discussion
ETV6::PDGFRB was first reported in a CMML patient in 1994, and in the 2022 WHO and ICC classification, neoplasms associated with ETV6::PDGFRB were classified as myeloid/lymphoid neoplasm with eosinophilia and tyrosine kinase gene fusions (M/LN-eo-TK), a specific entity and an updated name.5–7 Although the category name includes myeloid and lymphoid neoplasms, ETV6::PDGFRB-associated neoplasms with both myeloid and lymphoid cells in one patient had never been reported in the literature. Fusions of PDGFRB with partners like DIAPH1, SART3, RABEP1, and CBORF204 were reported to be associated with chronic myeloid neoplasms in BM and T-cell lymphoid neoplasms in LNs.8,9 The ETV6 gene, located on 12p13, encodes a transcriptional repressor playing a crucial role in hematopoietic regulation and can also fuse with >30 partners in myeloid and lymphoid leukemia, among which ETV6::PDGFRB in CMML and ETV6::RUNX1 in acute lymphoblastic B-cell leukemia (ALL) are well known.10 ETV6::LYN and ETV6::NCOA2 have been reported to be related to T-cell lymphoid and myeloid-mixture leukemia.11,12
PDGFRB-rearranged patients demonstrated good response to imatinib at 100–400 mg/day: 96% response rate, 90% 10-year overall survival,13 and median duration of 6.6 years.14 In non-AML cases, a low imatinib dosage (100–200 mg) is sufficient to induce and maintain long-term hematological, cytogenetic, and molecular remissions.4 In blastic crisis patients, whether to proceed with HSCT can only be made on an individual basis.15 In one study, all three patients with allogeneic HSCT relapsed. Patients may only be offered TKI monotherapy, rather than intensive chemotherapy.8 Three patients with chronic myeloid neoplasms and lymphoblastic T-cell lymphoma neoplasms received chemotherapy: two had a poor outcome, and the other transplant patient survived >3 years with complete molecular remission.8,9 For this young male patient in this study, the neoplasm cells were controlled by 200 mg/day imatinib, but were partly controlled by 200 mg/day imatinib again. The dose of imatinib is very important, and may show better outcomes with 200–300 mg/day imatinib continuously. Overall, there was a poor response to imatinib, whether at diagnosis or used alone after chemotherapy.
The existence of ETV6::PDGFRB fusion within the cells with T-cell and myeloid-cell biomarkers in the LNs revealed the same origin as the tumor cells in BM. CD34+CD117+CD7+CD56+ cell populations appeared simultaneously in invasive BM, and lymphatic samples confirmed it. Once the N-terminal part of the transcription repressor ETV6 is joined to the kinase domain of PDGFRB, the kinase domain is constitutively activated despite PDGF, resulting in the increased activation of several signaling pathways, including PI3K, STAT, MAPK and NF-B.16 NF-KB is critical for the cell growth and differentiation of ETV6::PDGFRB.17 NF-B signaling was not activated in this case, revealing that further mechanisms may go beyond the known role of ETV6::PDGFRB. Deregulated NOTCH3 and pre-TCR signaling contribute to the development of leukemia and lymphoma.18 Mutated MED12 can increase NOTCH signaling in CLL patients and was mutated in 10% pediatric T-ALL.19,20 The mutated NOTCH3 and activated NOTCH signaling in this case may be associated with the T-cell phenotype, especially in LN cells that have passed the pre-TCR signaling process.
ETV6::PDGFRB is capable of transforming lymphocytes in mice expressing it, although it is usually displayed as a myeloproliferative disease in mouse models.21,22 The break point in intron 8 of PDGFRB was special in the ETV6::PDGFRB fusion gene in this case snd in intron 10 in most cases, resulting in the retention of the fifth Ig domain expressed by exon 9 and exon 10, which may also be associated with the special phenotype of this case, likely abnormal increased activating ability of PDGFRB2.2 Notably, the karyotype at diagnosis favored a cryptic variant translocation, which was consistent with the atypical break point of PDGFRB. Several mechanisms have been proposed for the transformation of leukemia lineage, including stem-cell plasticity in which common myeloid/lymphoid progenitor cells were present expression of myeloid and B/T-lymphoid antigen, and clonal selection in which subclones with different phenotypes exist such that major clones could change under selection of drugs.23,24 ETV6::NCOA2 fusion can cause lymphoid specification while sustaining myeloid potential, and then cooperate with mutated NOTCH1, resulting in a T/My MAL.12 This case manifested as a phenotype of T/My MAL in the disease process. Both stem-cell plasticity and clonal selection were assumed to function, and in the background of multiple gene mutations, drugs like imatinib play an important role in accelerating the manifestation of T-LBL.
Fortunately, the LN size was still under control, but for this young patient, choosing whether to increase doses of imatinib, second/third generation of TKIs, or combine with chemotherapy while LNs enlarge again is challenging. TKI targets the kinase domain of ETV6::PDGFRB protein and blocks the constitutive activation of signaling pathways.25 Due to the atypical activated signaling pathway in this patient, single administration of TKIs may have had limited efficacy. Combined with target therapy on NOTCH signaling, chemotherapy and HSCT may be tried in the future.26 It is regretful that imatinib plasma levels were not measured in this patient, and the LN was not biopsied during the second enlargement. Meanwhile, there are some limitations of this study, such as the potential influence of individual genetic variability on treatment response and the limitations of using a single case to draw broad conclusions, which could be partly controlled by expanding case numbers in future studies.
Abbreviations
LN, lymph node; CMML, chronic myelomonocytic leukemia; TKI, tyrosine kinase inhibitor; BM, bone marrow; WBC, white blood cell; RTq-PCR, real-time quantitative polymerase chain reaction; FISH, fluorescence in situ hybridization; T-LBL, T-cell lymphoblastic lymphoma; FCM, flow cytometry; CR, complete response; GO, Gene Ontology; KEGG, Kyoto Encyclopedia of Genes and Genomes; VAF, variant allele frequency; WHO, World Health Organization; ICC, International Consensus Classification; HSCT, hematopoietic stem-cell transplantation; T/My MAL, T/myeloid mixed phenotype acute leukemia.
Ethics Approval
This study was approved by the Medical Ethics Committee of the Second Affiliated Hospital of Army Medical University.
Consent to Participate
The patient provided their written informed consent to participate in this study.
Consent for Publication
All authors have seen and approved the final version of the manuscript being submitted.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
Shuiqing Liu: Young Talent Project of Xinqiao Hospital (2022YQB076). Xiaojuan Deng: General Project of Chongqing Medical Scientific Research (2021MSXM140).
Disclosure
The authors declare no competing interests in this work.
References
1. Pozdnyakova O, Orazi A, Kelemen K, et al. Myeloid/lymphoid neoplasms associated with eosinophilia and rearrangements of PDGFRA, PDGFRB, or FGFR1 or with PCM1-JAK2. Am J Clin Pathol. 2021;155(2):160–178. doi:10.1093/ajcp/aqaa208
2. Appiah-Kubi K, Lan T, Wang Y, et al. Platelet-derived growth factor receptors (PDGFRs) fusion genes involvement in hematological malignancies. Crit Rev Oncol Hematol. 2017;109:20–34. doi:10.1016/j.critrevonc.2016.11.008
3. Havelange V, Demoulin JB. Review of current classification, molecular alterations, and tyrosine kinase inhibitor therapies in myeloproliferative disorders with hypereosinophilia. J Blood Med. 2013;4:111–121. doi:10.2147/JBM.S33142
4. Di Giacomo D, Quintini M, Pierini V, et al. Genomic and clinical findings in myeloid neoplasms with PDGFRB rearrangement. Ann Hematol. 2022;101(2):297–307. doi:10.1007/s00277-021-04712-8
5. Golub TR, Barker GF, Lovett M, Gilliland DG. Fusion of PDGF receptor beta to a novel ets-like gene, tel, in chronic myelomonocytic leukemia with t(5;12) chromosomal translocation. Cell. 1994;77(2):307–316. doi:10.1016/0092-8674(94)90322-0
6. Khoury JD, Solary E, Abla O, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36(7):1703–1719. doi:10.1038/s41375-022-01613-1
7. Arber DA, Orazi A, Hasserjian RP, et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: integrating morphologic, clinical, and genomic data. Blood. 2022;140(11):1200–1228. doi:10.1182/blood.2022015850
8. Jawhar M, Naumann N, Schwaab J, et al. Imatinib in myeloid/lymphoid neoplasms with eosinophilia and rearrangement of PDGFRB in chronic or blast phase. Ann Hematol. 2017;96(9):1463–1470. doi:10.1007/s00277-017-3067-x
9. Ondrejka SL, Jegalian AG, Kim AS, et al. PDGFRB-rearranged T-lymphoblastic leukemia/lymphoma occurring with myeloid neoplasms: the missing link supporting a stem cell origin. Haematologica. 2014;99(9):e148–e151. doi:10.3324/haematol.2014.105452
10. De Braekeleer E, Douet-Guilbert N, Morel F, et al. ETV6 fusion genes in hematological malignancies: a review. Leuk Res. 2012;36(8):945–961. doi:10.1016/j.leukres.2012.04.010
11. Telford N, Alexander S, McGinn OJ, et al. Myeloproliferative neoplasm with eosinophilia and T-lymphoblastic lymphoma with ETV6-LYN gene fusion. Blood Cancer J. 2016;6(4):e412. doi:10.1038/bcj.2016.11
12. McCormack MP. T/myeloid MPAL: origin and pathogenesis. Blood. 2022;139(3):313–315. doi:10.1182/blood.2021014129
13. Reiter A, Gotlib J. Myeloid neoplasms with eosinophilia. Blood. 2017;129(6):704–714. doi:10.1182/blood-2016-10-695973
14. Cheah CY, Burbury K, Apperley JF, et al. Patients with myeloid malignancies bearing PDGFRB fusion genes achieve durable long-term remissions with imatinib. Blood. 2014;123(23):3574–3577. doi:10.1182/blood-2014-02-555607
15. Metzgeroth G, Schwaab J, Gosenca D, et al. Long-term follow-up of treatment with imatinib in eosinophilia-associated myeloid/lymphoid neoplasms with PDGFR rearrangements in blast phase. Leukemia. 2013;27(11):2254–2256. doi:10.1038/leu.2013.129
16. Demoulin JB, Montano-Almendras CP. Platelet-derived growth factors and their receptors in normal and malignant hematopoiesis. Am J Blood Res. 2012;2(1):44–56.
17. Montano-Almendras CP, Essaghir A, Schoemans H, et al. ETV6-PDGFRB and FIP1L1-PDGFRA stimulate human hematopoietic progenitor cell proliferation and differentiation into eosinophils: the role of nuclear factor-kappaB. Haematologica. 2012;97(7):1064–1072. doi:10.3324/haematol.2011.047530
18. Bellavia D, Campese AF, Checquolo S, et al. Combined expression of pTalpha and Notch3 in T cell leukemia identifies the requirement of preTCR for leukemogenesis. Proc Natl Acad Sci U S A. 2002;99(6):3788–3793. doi:10.1073/pnas.062050599
19. Fernandez-Martinez JL, deAndres-Galiana EJ, Sonis ST. Genomic data integration in chronic lymphocytic leukemia. J Gene Med. 2017;19(1–2):e2936.
20. Spinella JF, Cassart P, Richer C, et al. Genomic characterization of pediatric T-cell acute lymphoblastic leukemia reveals novel recurrent driver mutations. Oncotarget. 2016;7(40):65485–65503. doi:10.18632/oncotarget.11796
21. Ritchie KA, Aprikyan AA, Bowen-Pope DF, et al. The Tel-PDGFRbeta fusion gene produces a chronic myeloproliferative syndrome in transgenic mice. Leukemia. 1999;13(11):1790–1803. doi:10.1038/sj.leu.2401494
22. Cain JA, Xiang Z, O’Neal J, et al. Myeloproliferative disease induced by TEL-PDGFRB displays dynamic range sensitivity to Stat5 gene dosage. Blood. 2007;109(9):3906–3914. doi:10.1182/blood-2006-07-036335
23. Schmidt CA, Przybylski GK. What can we learn from leukemia as for the process of lineage commitment in hematopoiesis? Int Rev Immunol. 2001;20(1):107–115. doi:10.3109/08830180109056725
24. Jamil SF, Sharma U, Singh C, et al. Lineage switch of acute myeloid leukemia to T-Cell acute lymphoblastic leukemia - A unique case report. Indian J Pathol Microbiol. 2023;66(1):191–195. doi:10.4103/ijpm.ijpm_441_21
25. Banerji L, Sattler M. Targeting mutated tyrosine kinases in the therapy of myeloid leukaemias. Expert Opin Ther Targets. 2004;8(3):221–239. doi:10.1517/14728222.8.3.221
26. Wang X, Huang R, Zhang X, Zhang X. Current status and prospects of hematopoietic stem cell transplantation in China. Chin Med J. 2022;135(12):1394–1403. doi:10.1097/CM9.0000000000002235
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.