Back to Journals » International Journal of General Medicine » Volume 16
Multimorbidity Patterns and Associations with Gait, Balance and Lower Extremity Muscle Function in the Elderly: A Cross-Sectional Study in Northwest China
Authors Yang K, Yang S, Chen Y, Cao G, Xu R, Jia X, Hou L, Li J, Bi C, Wang X
Received 20 April 2023
Accepted for publication 13 July 2023
Published 28 July 2023 Volume 2023:16 Pages 3179—3192
DOI https://doi.org/10.2147/IJGM.S418015
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Kaikai Yang, Shanru Yang, Yang Chen, Guihua Cao, Rong Xu, Xin Jia, Liming Hou, Jinke Li, Chenting Bi, Xiaoming Wang
Department of Geriatrics, Xijing Hospital, Air Force Medical University, Xi’an, 710032, People’s Republic of China
Correspondence: Xiaoming Wang, Department of Geriatrics, Xijing Hospital, Air Force Medical University, 127 Changle West Road, Xi’an, 710032, People’s Republic of China, Tel +86-29-84775543, Email [email protected]
Purpose: Fall is a common geriatric syndrome leading to various adverse outcomes in the elderly. Gait and balance disorders and decreased lower extremity muscle function are the major intrinsic risk factors of falls, and studies suggested that they were closely related to the underlying chronic conditions. This study aimed to explore the patterns of multimorbidity and determine the associations of these multimorbidity patterns with gait, balance and lower extremity muscle function.
Patients and Methods: A cross-sectional survey of 4803 participants aged ≥ 60 years in Shaanxi Province, China was conducted and the self-reported chronic conditions were investigated. The 6-m walk test, timed-up-and-go test (TUG) and 5-sit-to-stand test (5-STS) were conducted to evaluate gait, balance, and lower extremity muscle function respectively. Latent class analysis was used to explore patterns of multimorbidity, and multivariate regression analysis was used to determine the associations of multimorbidity patterns with gait, balance, and lower extremity muscle function.
Results: Five multimorbidity patterns were identified: Degenerative Disease Class, Cardio-metabolic Class, Stroke-Respiratory-Depression Class, Gastrointestinal Class, and Very sick Class, and they were differently associated with gait and balance disorders and decreased lower extremity muscle function. In particular, the multimorbidity patterns of Degenerative Disease Class and Stroke-Respiratory-Depression Class were closely associated with all the three risk factors of falls.
Conclusion: There are significant differences in the impact of different multimorbidity patterns on the major intrinsic risk factors of falls in the elderly population, and appropriate multimorbidity patterns are closely related to the prediction of falls and can help to develop fall prevention strategies in the elderly.
Keywords: elderly, multimorbidity, gait, balance, falls
Introduction
With the advancements in medical technology and the growth of the social economy, there has been a significant increase in the average life expectancy of human beings over the past two centuries.1 However, the improvement in healthy life expectancy has been comparatively slower in relation to overall life expectancy. According to World Health Statistics, between 2000 and 2019, the average life expectancy worldwide increased by 6.5 years. In contrast, the average healthy life expectancy only saw an increase of 5.4 years.2 As a result, a considerable number of older adults are now experiencing the onset of chronic diseases later in life. Among these, the coexistence of two or more conditions, referred to as multimorbidity,3,4 has become a prevalent issue within the elderly population and a growing public health concern.5 A European survey revealed that over 50% of older adults experience the coexistence of two or more diseases simultaneously.6 Moreover, two recent nationally representative surveys conducted in China reported the prevalence of multimorbidity among the elderly as 31.8% and 42.4% respectively.7,8 Multimorbidity has been linked to various adverse outcomes, including a decline in functional status and quality of life, increased rates of hospitalization, and elevated all-cause mortality.9–12 However, it is worth highlighting that the majority of current clinical guidelines primarily concentrate on individual diseases, and the few guidelines that exist for multimorbidity merely define it in terms of quantifying the number of chronic diseases.13,14 This quantitative approach to assessing multimorbidity has limitations in providing information to clinical guidelines because it is difficult to differentiate individuals with the same number but different types of chronic diseases (for example, two individuals with the same number of chronic diseases may have completely different disease combinations, treatment approaches, and prognoses). Consequently, numerous studies that employ a counts-based definition of multimorbidity have failed to produce consistent evidence supporting effective health management strategies.15–17 Due to the lack of integrated approaches, clinicians still primarily focus on individual diseases in the daily clinical practice of elderly patients with multiple conditions,18 which often fails to meet the complex needs of multimorbidity patients and can become duplicative, inefficient or even problematic.19 Therefore, it is crucial to look at multimorbidity as a whole, and there is also an urgent need for a more precise qualitative classification of multimorbidity combinations.20 Existing evidence indicates that the combination of chronic conditions in the same individuals is non-random, as they may share common risk factors, pathophysiological mechanisms, and mutually influence each other.21 Building upon this rationale, it is justifiable to identify distinct patterns of multimorbidity and approach them holistically in the study of risk factors, treatment outcomes, and prognostic management, which will help provide clues for the prevention and treatment of multimorbidity as well as improving prognosis.
In recent few years increasing interest has been turned to the patterns of associative multimorbidity in older adults. A recent study conducted a systematic review incorporating 97 articles on the patterns of multimorbidity and their associated social and behavioral determinants.22 The study found that the most commonly reported patterns of multimorbidity were cardiometabolic, musculoskeletal, mental, and respiratory patterns, and that different multimorbidity patterns have different influencing factors in terms of sociodemographic characteristics, socioeconomic status, and lifestyle. Furthermore, a prospective cohort study showed that subjects belonging to the cardiovascular/anemia/dementia disease pattern had the highest risk of disability in basic activities of daily living (ADL) than other multimorbidity patterns they identified.23 In a prospective study from Italy, Fan Junning et al found that mortality among older residents of nursing homes differed between multimorbidity patterns. These two studies indicate that the prognosis of multimorbidity is strictly dependent on the patterns of underlying disease combination.24 Similarly, existing evidence suggests that different multimorbidity patterns have varying effects on disability, frailty, hospitalization rates, and quality of life.23,25–28 However, the current literature on multimorbidity patterns primarily comes from Europe and South America, and there is still limited information available on Asian populations, which need more research data to provide further support.22,29
Falls are one of the most common geriatric syndromes, which are the leading cause of unintentional injury and the third cause of chronic disability in older adults.30 Approximately 28.7% of the elderly over 65 years old reported at least one fall accident,31 seriously affecting the functional status and quality of life of the elderly. Although the causes of falls are multifactorial, many high-quality randomized clinical trials, systematic reviews and meta-analyses have shown that gait and balance disorders and decreased lower extremity muscle function are the major intrinsic risk factors for falls in older adults.32–34 Gait is a unique rhythmic leg activity characteristic of walking. The formation and maintenance of normal gait depend on the synergistic effect of multiple systems such as the nervous system, motor system, respiratory system, and circulatory system.35 Balance function is the ability to maintain the normal posture of the human body and automatically adjust the posture state when the posture changes, which is also important for the maintenance of normal gait. The elderly have a high prevalence of gait and balance disorders, because the postural reflex to transfer body weight and regulate balance in time when stability is disturbed is weaker due to the degeneration of the nervous system and the decline of muscle strength.36 Approximately 35% of adults aged more than 70 years and 61% aged more than 80 years have gait and balance disorders,37,38 the main manifestations of which are stiff and uncoordinated gait and impaired postural control ability. In addition, studies have shown that ankle, knee, and hip strength decreases by more than 30% per year after age 50,39,40 resulting in a 2–3 times increased risk of falls.41 Simultaneously, the decrease in lower extremity muscle function is also one of the main causes of abnormal balance in older adults,42 However, researches have demonstrated that gait and balance disorders and decreased lower extremity muscle function in older adults were not inevitable consequences of aging, but related to the underlying chronic conditions of the individual.43–45 In particular, the elderly are more likely to have multimorbidity, which further exacerbates the negative impact of chronic diseases and increases the risk of falls. Numerous studies have established a link between multimorbidity and an increased risk of falls. A multicenter trial involving 7 European centers demonstrated a significant correlation between baseline multimorbidity and elevated rates of both falls and injurious falls during a 3-year follow-up period.46 Similarly, a study in Ireland observed a prospective relationship between multimorbidity and falls, indicating that older adults with two chronic conditions had a 1.32-fold higher risk of falls, while those with more than four chronic conditions had a 1.92-fold higher risk of experiencing falls.47 Furthermore, consistent results have also been observed in two studies conducted in Asian countries, aligning with findings from Europe.48,49 To date, however, few studies have explored the relationship between different patterns of condition combinations and fall risk. A recent cross-sectional study discovered that specific multimorbidity patterns were associated with a 2-year history of falls among Chinese over 45 years old.50 Nevertheless, there is a lack of relevant research focused specifically on the elderly population. In particular, the impact of distinct multimorbidity patterns on gait, balance, and lower extremity muscle function, which are the three main intrinsic determinants of falls in the elderly, remains unclear. Previous studies have demonstrated that regular exercise targeting gait, balance, and muscle strength is an important preventive measure against falls and fall-related injuries.51,52 Therefore, understanding the association between multimorbidity patterns and gait and balance disorders, as well as decreased lower extremity muscle function, will not only help identify specific high-risk populations for falls but also facilitate the selection of more targeted preventive measures.
Accordingly, the purpose of the present study is to identify the patterns of multimorbidity among older adults in community and hospitals in northwest China, and examine the association of these multimorbidity patterns with gait, balance and lower extremity muscle function through a cross-sectional study design. We expect that our findings will provide more effective suggestions for screening high-risk population and formulating prevention strategies of falls.
Methods
Study Population
The study participants were inpatients and community elderly over 60 years old in 10 hospitals, 6 community healthcare centers and 1 nursing home in northwest China. A convenient sampling method was used and a face-to-face survey was conducted during September-December 2021. Participants were excluded if they were unable to complete the physical performance tests, or if they were in an unstable state of illness or an active phase of psychiatric illness. Finally, a total of 4803 elderly people were eligible participants in the study.
Data Collection
We conducted a field survey using the Elder Health Management Platform established by Beijing Hospital to collect and manage data. All investigators underwent uniform training and strictly followed standardized protocols for conducting the survey, measuring indices, and entering data. The survey process was supervised online by designated managers to ensure quality control and adherence to established guidelines. This study was conducted in compliance with the Declaration of Helsinki, and was reviewed and approved by the Ethics Committee of the First Affiliated Hospital of the Air Force Medical University (No.KY20212113). All subjects were informed of the purpose and significance of the study and signed informed consent prior to the survey.
From September to December 2021, we ascertained self-reported chronic conditions by asking “Have you been diagnosed with the following chronic conditions by a doctor” including hypertension, diabetes, heart disease, stroke, cancer, osteoarthropathy, anemia, cataract, Parkinson’s disease, respiratory disease, gastrointestinal disease, depression, kidney disease, hepatobiliary disease, and thyroid disease. Visual impairment and hearing impairment were defined by self-reported poor vision and poor hearing, respectively. Multimorbidity was defined as the simultaneous occurrence of two or more chronic conditions mentioned above. Meanwhile, we conducted the 6-m walk test, timed up and go test(TUG), and 5-Times Sit-to-Stand test (5-TST) in subjects, which are common assessment tools for gait performance, balance, and lower extremity muscle function, respectively.53–56 They are widely used in primary care settings due to their advantages of being easy to measure and no reliance on special equipment, and there is evidence of their validity in screening the risk of falls.57–59 In the 6-m walk test, participants were asked to walk a distance of 6 meters on a flat, unobstructed ground at their habitual pace (the use of walking aids was allowed) and the time it took was recorded by a stopwatch. Each subject was tested twice and the shortest time was used. Gait speed (meter per second) was calculated as the walking distance divided by the time. The timed up and go test (TUG) measured the duration of standing up from a 46cm high chair with 65cm high armrests, walking 3 m, returning, and sitting down. Participants were asked to start with their hands on the armrests and back against the back of the chair. Walking with a cane was allowed, but assistance was not. The 5-times sit to stand test measured the fastest time to get up and sit down 5 times in a chair without armrests, requiring that each rise must be upright. According to previous studies,60,61 the TUG duration and 5-STS duration were further categorized as abnormal and normal groups with the cut-off value of 13.5s and 5s, respectively. Furthermore, information of participants’ age, sex, height, nutritional status (BMI) (underweight, BMI<18.5 kg/m2; normal weight, BMI=18.5–23.9 kg/m2; overweight, BMI=24–27.9 kg/m2; and obesity, BMI≥28 kg/m2), residential region, family type, physical activity, vocational type, smoking status, drinking status, and medication use were collected as covariates.
Statistical Analysis
To explore the multimorbidity patterns in the study population, latent class analysis (LCA) was conducted based on the 17 chronic conditions described above. LCA is a type of structural equation modeling to identify the latent variables behind a set of observed variables that are statistically associated. Among the three commonly used unsupervised clustering methods, it is more advantageous when dealing with categorical data in comparison to exploratory factor analysis,62 and is more objective in the method of determining the optimal number of clusters than cluster analysis,63 Specifically, latent class analysis (LCA) can objectively select the best models with optimal number of clusters through some information criteria, such as Akaike Information Criterion (AIC), adjusted Bayesian Information Criterion (aBIC) and log-likelihood (LL). A series of LCA models ranging from two to eight classes were evaluated and compared to determine the optimal number of latent classes to fit the data. The model fit, classification accuracy, LMR likelihood ratio tests, parsimony, and clinical interpretability of the results were the final criteria to determine the best model. Model fit statistics used in comparing models include Akaike Information Criterion (AIC), sample size adjusted Bayesian Information Criterion (aBIC), and log-likelihood (LL), smaller values of which indicate better model fit to the data. The classification accuracy was evaluated by Entropy, and the larger the index, the higher the classification accuracy of the model. The LMR likelihood ratio tests were used to test whether the model was better as the number of classes increased. Once the optimal model is determined, A posterior probability (ie, the probability that an individual belongs to a specific latent class) can be calculated for each participant through the constructed model, and then each participant was assigned to a latent class with the highest computed posterior probability. Furthermore, the model should have substantive clinical meaning and a good classification effect on diseases.
In order to examine the association of multimorbidity and multimorbidity patterns with gait, balance, and lower extremity muscle function, multivariable linear regression analysis and multivariable binary logistic regression analysis were performed with gait speed, TUG duration, and 5-STS duration as dependent variables and multimorbidity or multimorbidity patterns as independent variable. These models were adjusted for the covariates mentioned above.
The LCA was performed using Mplus 8.3, and other analyses were conducted using SPSS 26.0. Descriptive analysis of the study population was performed by calculating the means with standard deviation (SD) for continuous variables and the frequencies with percentages for discrete variables. The t-test and ANOVA were used for comparison of continuous variables, and the comparisons of discrete variables were performed by chi-square test. All statistical tests were two-tailed, and the significance level was set at P = 0.05 or less.
Results
Characteristics of Study Participants
A total of 4803 participants aged 60 years or older were included, with a mean age of 69.94±6.68 years. Among them, 2527 were women (52.6%). It was found that 428 participants (8.9%) lived alone, 4057 (84.5%) lived in urban areas, and 1929 (40.2%) had a high school education or above (Table 1). The prevalence of multimorbidity was 39.2%, with 18.1% of participants having two chronic conditions, 11.2% having three chronic conditions, and 9.9% having four or more chronic conditions. The number of chronic conditions increased with age (Figure 1). The average gait speed was measured at 0.89±0.26 m per second. Additionally, 9.9% of participants had an abnormal Timed Up and Go (TUG) test duration, and 19.3% had an abnormal 5-Time Sit-to-Stand (5-STS) test duration. Participants with multimorbidity exhibited slower gait speed and a higher prevalence of abnormal TUG and 5-STS test durations compared to those with fewer than two chronic conditions.
 |
Table 1 Descriptive Characteristics of the Study Population (N=4803) |
 |
Figure 1 Proportion of respondents with different numbers of chronic conditions by age stratification. |
Identification of Multimorbidity Patterns
Determination of the Best Model with Optimal Number of Clusters
Seven LCA models ranging from 2–8 classes were constructed. The evaluation indices of the models can be found in Supplementary Table 1 and Figure 2. With an increase in the number of potential classes, the aBIC value reached its lowest point at six potential classes. Although the AIC value was lowest with eight latent classes, LMR likelihood ratio tests indicated that the improvement in model fit was not significant beyond six classes. Furthermore, the model with six latent classes was clinically interpretable for the potential classification of the 17 chronic diseases, and the classification accuracy was also acceptable. Hence, we consider the LCA model with six latent classes to be the optimal model.
 |
Figure 2 Scree plot of ACI and aBIC for LCA models with different numbers of clusters. |
Characteristics of the Five Multimorbidity Patterns
Figure 3 displays the conditional probabilities of the 17 chronic diseases across the six identified potential classes. Based on the patterns of chronic condition combinations, five multimorbidity patterns were identified and labeled as follows: Degenerative Disease Class (higher prevalence in cancer, anemia, Parkinson’s disease, visual impairment, hearing impairment, osteoarthrosis), Cardio-metabolic Class (higher prevalence in hypertension, diabetes, heart disease), Stroke-Respiratory-Depression Class (higher prevalence in stroke, respiratory disease and depression), Gastrointestinal Class (higher prevalence in gastrointestinal disease), and Very Sick Class (prevalence of all 17 conditions is above cohort average). Additionally, there was a class labeled as the “Relatively Healthy Class” where the prevalence of all investigated chronic diseases was significantly lower than that in the total sample.
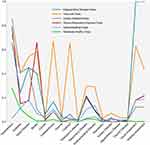 |
Figure 3 Probabilities of chronic conditions for each latent class. |
In the developed LCA model, the posterior probability, representing the probability of belonging to each of the six latent classes, was calculated for each participant. Subsequently, participants were assigned to the latent class with the highest posterior probability. The characteristics of individuals in the six latent classes are presented in Supplementary Table 2. The most prevalent multimorbidity pattern identified was the Cardio-Metabolic Class, with a prevalence of 17.7%. The prevalence of this pattern was significantly higher in urban areas compared to rural areas. However, no significant gender differences were observed among the five multimorbidity patterns. Participants in the Degenerative Disease Class were generally the oldest, with an average age of 76.79 years, followed by the Very Sick Class (73.9±8.1). Those in the Very sick Class presented the highest number of chronic conditions with an average of 5.95, followed by the Degenerative Disease Class (4.38 conditions on average). The Relatively Healthy Class had the youngest average age (68.9±6.1) and the lowest number of chronic conditions (0.5±0.5). Furthermore, participants in the Degenerative Disease Class displayed the slowest gait speed and the highest prevalence of abnormal Timed Up and Go (TUG) test duration and abnormal 5-Time Sit-to-Stand (5-STS) test duration.
Associations Between Multimorbidity Patterns and Gait Speed
After adjustment for covariates in the multiple linear regression analysis, the average gait speed of participants belonging to Very Sick Class, Degenerative Disease Class, and Stroke-Respiration-Depress Class decreased by 0.10m/s (95%CL: −0.15, −0.05), 0.08m/s (95%CL: −0.12, −0.05), and 0.03m/s (95%CL: −0.06, −0.01) respectively when compared with those in Relatively Healthy Class, while participants in Cardio-metabolic Class and Gastrointestinal Class had no significant difference in average gait speed with that of Relatively Healthy Class (Table 2).
 |
Table 2 Cross-Sectional Associations Between Multimorbidity Patterns and Gait Speed Among the Participants (N=4803) |
Associations Between Multimorbidity Patterns and TUG Test Duration
Table 3 shows the results of the binary logistic regression analysis exploring the cross-sectional association between multimorbidity patterns and abnormal TUG test duration. After adjusting for age, sex, height, nutritional status (BMI), residential region, family type, physical activity, vocational type, smoking status, drinking status and polypharmacy in Logistic regression analysis, we found that participants in stroke-respiration-depress Class (OR=2.23, 95%CL: 1.62, 3.07) and in Degenerative Disease Class (OR=1.61, 95%CL: 1.05, 2.48) were more likely to be abnormal in TUG test when compared with those in Relatively Healthy Class, while other multimorbidity patterns presented no statistically significant associations with abnormal TUG test duration.
 |
Table 3 Cross-Sectional Associations Between Multimorbidity Patterns and Abnormal TUG Test Duration Among the Participants (N=4803) |
Associations Between Multimorbidity Patterns and 5-STS Test Duration
The results of the binary logistic regression analysis investigating the associations between multimorbidity patterns and abnormal 5-STS test duration are displayed in Table 4. After adjusting for multiple covariates, we found that participants in all five latent classes had statistically significant increased odds of abnormal 5-STS test duration when compared with those in Relatively Healthy Class, with participants in Degenerative Disease Class had the highest odds ratio of 2.41 (95%CL: 1.69, 3.43), followed by those in Very Sick Class (OR=2.77, 95%CL: 1.70, 4.52) and Stroke-Respiratory-Depression Class (OR=2.03, 95%CL: 1.55, 2.65).
 |
Table 4 Cross-Sectional Associations Between Multimorbidity Patterns and Abnormal 5-STS Test Duration Among the Participants (N=4803) |
Discussion
Multimorbidity has attracted increasing interest worldwide due to its clinical complexity, high prevalence, and substantial impact on individual, household and society in recent decades.9,64,65 It has been noted that the impact of multiple conditions on one individual is not a simple linear accumulation of single conditions, but there would be synergistical or antagonistical effect among concurrent conditions.66,67 For example, a large collaborative study found that any combination of co-occurring cardio-metabolic conditions was associated with multiplicative mortality risk.68 Additionally, there are interlinks in pathophysiological trajectories among some chronic conditions that coexist so that they are not just random combination but have some certain relatively common and fixed combination patterns.69 As a result, the conventional management approaches that focus on single conditions may be impractical, irrelevant, or even harmful for patients with multimorbidity.18,70 Therefore, there is an urgent need to develop an integrated management strategy that regards multiple related conditions as a whole and aims to improve the overall status and reduce adverse outcomes of multimorbidity patients. However, the mechanisms and pathophysiology underlying the prevalence and adverse outcomes of multimorbidity are complicated and steal uncertain. This is partly due to the fact that the population with multimorbidity defined using chronic condition count as the only metric is highly heterogeneous, because it neglects the nature and interactions of chronic conditions.64 Thus, distinguishing different multimorbidity patterns to manage older adults with multiple chronic conditions may be a desirable way. Based on this, in the present study we explored multimorbidity patterns in the sample population through the method of Latent Class Analysis (LCA), a probabilistic modeling algorithm that can explore the latent variables behind observed categorical variables which are statistically associated. The LCA is more objective in the method of determining the optimal number of latent classes than cluster analysis,63 so it is widely used in studies concerning multimorbidity patterns.71–73 Then, for the first time, we explored the cross-sectional associations of the distinct multimorbidity patterns with gait, balance and lower extremity muscle function, which are three major intrinsic risk factors of falls, for the purpose of providing evidence for the development of prevention strategy of falls in older adults with multimorbidity.
The five multimorbidity patterns identified in our study are not only statistically significant but also clinically explicable. The combination of gastrointestinal diseases, labeled as Gastrointestinal Class, are mainly due to their common pathophysiological basis as the diseases belong to the same system. This multimorbidity pattern was not rare in related studies. In a large sample cross-sectional study from China, a pattern of “gastrointestinal and hepatorenal multimorbidity” was reported as one of the four multimorbidity patterns prevalent in the study population.7 The same is true in European population, as a similar pattern labeled “gastrointestinal diseases and cancer pattern” was also demonstrated in a study on Germans.74 Cardio-Metabolic Class, which was the highest prevalent multimorbidity pattern in our sample population, was also the most common patterns reported in similar studies on both western and Asian population.62,75 Indeed, hypertension and diabetes are frequently coexist because they have more than one interlinks in their pathophysiological trajectories,76,77 and heart disease is a common adverse outcome of both hypertension and diabetes. Thus, this is likely the intrinsic mechanism for the prevalence of this multimorbidity pattern. The Degenerative Disease Class comprised a combination of diseases that are related to advancing age, such as Parkinson’s disease, cancer, osteoarthrosis, visual impairment and hearing impairment. Consistently, several studies have demonstrated similar multimorbidity patterns which mainly consist of arthritis or joint disease, musculoskeletal system diseases, cancer, eye problems and hearing disorders.78–80 Of note, few studies have reported multimorbidity patterns similar to “Stroke-Respiratory-Depression Class”, but there are some evidences to explain the nonrandom combination of the three conditions. A meta-analysis has reported that approximately one-third of stroke survivors experience depression at any time-point in the first year after stroke, although the mechanism is still unclear.81 According to a prospective cohort study, the risk of depression in the elderly with slow gait speed was 1.82 times higher than that of the normal elderly during a two-year follow-up.82 Hence we speculate that the fear of falling and activity limitation caused by abnormal gait function after stroke may increase the risk of depression in the elderly. Moreover, stroke often causes decreased respiratory muscle function and changes in respiratory rhythm, thereby affecting lung function and increasing the risk of chronic pulmonary infection.83 In the end, there were some older adults with multimorbidity unlike any of the above patterns, because they present the worst health status and have low capacity for disease prevention, so that they are vulnerable to all chronic conditions. They were assigned to the “Very Sick Class” as another multimorbidity pattern. Not surprisingly, we found that the elderly with this multimorbidity pattern suffered the most chronic conditions.
Our study found that distinct multimorbidity patterns were differently associated with gait and balance disorders and decreased lower extremity muscle function. Specifically speaking, the Degenerative Disease Class and Stroke-Respiratory-Depression Class were strongly associated with slower gait speed, poorer TUG test performance and poorer 5-STS test performance compared with Relatively Healthy Class. This may be resulted from comprehensive impact of chronic conditions in these patterns, such as Parkinson’s disease, osteoarthrosis, visual impairment, as well as stroke. By contrast, the Cardio-Metabolic Class and Gastrointestinal Class had no significant associations with either slower gait speed or poorer 5-STS test performance. This indicates that there are significant differences in the impact of different multimorbidity patterns on the major intrinsic risk factors of falls in the elderly population. Likewise, there has been a large body of evidence demonstrating that certain specific multimorbidity patterns are associated with more severe adverse health outcomes, such as increased health care utilization,84 disability,85 and mortality.86 It will be beneficial to uncover these multimorbidity patterns and conduct targeted prevention and intervention. The results of our study emphasized the necessity for distinguishing multimorbidity patterns to predict risk for falls in the elderly and, in particular, called for a greater focus on the prevention of falls in those with multimorbidity patterns of Degenerative Disease Class and Stroke-Respiratory-Depression Class in the population. In addition, a previous study showed that older adults frequently paid attention to environmental and behavioral risk factors of falls but always overlooked the intrinsic ones.87 However, numerous studies have highlighted the importance of intervening the intrinsic factors to prevent falls, such as balance, gait and muscle strength exercise.51,52,88 The findings of our study can help distinguish the specific risk population of falls with intrinsic risk factors and contribute to its targeted prevention and management.
We noted that the elderly with multimorbidity pattern of Very sick Class in this study had the highest average number of diseases, and all 17 chronic diseases had high prevalence in this population. However, binary Logistic regression analysis showed that this multimorbidity pattern was not significantly associated with abnormal TUG test duration after adjusting for multiple covariates. One possible explanation for this is that the subjects included in the present study were elderly people who were able to complete the three tests, while those with poor physical conditions who were unable to complete the gait, balance, and sit-to-stand tests were not included, thus introducing a selection bias. In addition, the regression results were less stable due to the small number of elderly people classified as Very sick Class. We suggest that future studies make up for the shortcomings of this study by using possible alternative outcome variables so that they are able to include the older adults who have difficulty completing the gait, balance, and sit-to-stand tests in research.
The present study has several strengths. To the best of our knowledge, this is the first study to examine the association of multimorbidity patterns with the three major intrinsic risk factors of falls (gait and balance disorders and decreased lower extremity muscle function) based on a large sample of Chinese older adults, which is helpful for developing healthcare and management strategies for specific populations in the elderly with multimorbidity. Second, our study used validated performance-based indicators to assess three major intrinsic risk factors for falls, which are much more objective. Third, we used Latent Class Analysis (LCA) to identify multimorbidity patterns, which is more objective in the method of determining the optimal number of latent classes compared to cluster analysis.63 However, our study also has several limitations. First, the study population was selected by convenient sampling, which may lead to selection bias. Second, self-reported disease history is subject to recall bias, which leads to a underestimation of the prevalence of chronic conditions, and the stage and severity of diseases cannot be evaluated. Finally, this study is cross-sectional and therefore cannot determine causality.
Conclusion
We found that the five multimorbidity patterns identified in the study population were differently associated with gait and balance disorders and decreased lower extremity muscle function. In particular, the multimorbidity patterns of Degenerative Disease Class and Stroke-Respiratory-Depression Class were closely associated with all the three risk factors of falls. Thus, early interventions, especially regular strength, balance, and gait training, might be beneficial for the elderly with multimorbidity of Degenerative Disease Class or Stroke-Respiratory-Depression Class to prevent falls. Further longitudinal research and interventional trial are needed to elucidate the causality and evaluate the effectiveness on prevention of falls by targeted functional training for elderly people with specific multimorbidity patterns.
Abbreviations
TUG, Timed-up-and-go test; 5-STS, 5-times sit to stand test; LCA, Latent class analysis; AIC, Akaike Information Criterion; aBIC, adjusted Bayesian Information Criterion; BMI, Body mass index; OR, Odds ratio; CL, Confidence interval; SD, Standard deviation.
Data Sharing Statement
The data of this study are available from the corresponding author, upon reasonable request.
Ethics Approval and Consent to Participate
This study was reviewed and approved by the Ethics Committee of the First Affiliated Hospital, the Air Force Medical University (No.KY20212113). All subjects were informed of the purpose and significance of the study and signed informed consent prior to the survey. Consent for publication.
Acknowledgments
Thanks to Professor Lei Shang for his guidance in statistical methods.
Author Contributions
All author made a significant contribution to the article. They all have agreed on the journal to which the article will be submitted, reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage, and agree to take responsibility and be accountable for the contents of the article.
Funding
The research was supported by the National Key R&D Program of China (No. 2020YFC2008000) and Military Health Care Project of China (No. 23BJZ13).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vaupel JW. Biodemography of human ageing. Nature. 2010;464(7288):536–542. doi:10.1038/nature08984
2. Life expectancy and healthy life expectancy data by country; 2023. Available from: https://apps.who.int/gho/data/node.main.SDG2016LEX?lang=en.
3. Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev. 2017;37:53–68. doi:10.1016/j.arr.2017.05.003
4. van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity. Eur J Gen Pract. 1996;2(2):65–70. doi:10.3109/13814789609162146
5. Partridge L, Deelen J, Slagboom PE. Facing up to the global challenges of ageing. Nature. 2018;561(7721):45–56. doi:10.1038/s41586-018-0457-8
6. Sheridan PE, Mair CA, Quiñones AR. Associations between prevalent multimorbidity combinations and prospective disability and self-rated health among older adults in Europe. BMC Geriatr. 2019;19(1):198. doi:10.1186/s12877-019-1214-z
7. Fan J, Sun Z, Yu C, et al. Multimorbidity patterns and association with mortality in 0.5 million Chinese adults. Chin Med J. 2022;135(6):648–657. doi:10.1097/cm9.0000000000001985
8. Yao SS, Cao GY, Han L, et al. Prevalence and patterns of multimorbidity in a nationally representative sample of older Chinese: results from the China health and retirement longitudinal study. J Gerontol A Biol Sci Med Sci. 2020;75(10):1974–1980. doi:10.1093/gerona/glz185
9. Makovski TT, Schmitz S, Zeegers MP, Stranges S, van den Akker M. Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res Rev. 2019;53:100903. doi:10.1016/j.arr.2019.04.005
10. Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. doi:10.1093/epirev/mxs009
11. Rodrigues LP, Vissoci JRN, França DG, et al. Multimorbidity patterns and hospitalisation occurrence in adults and older adults aged 50 years or over. Sci Rep. 2022;12(1):11643. doi:10.1038/s41598-022-15723-4
12. Fisher K, Griffith LE, Gruneir A, Kanters D, Markle-Reid M, Ploeg J. Functional limitations in people with multimorbidity and the association with mental health conditions: baseline data from the Canadian Longitudinal Study on Aging (CLSA). PLoS One. 2021;16(8):e0255907. doi:10.1371/journal.pone.0255907
13. Kernick D, Chew-Graham CA, O’Flynn N. Clinical assessment and management of multimorbidity: NICE guideline. Br J Gen Pract. 2017;67(658):235–236. doi:10.3399/bjgp17X690857
14. Palmer K, Marengoni A, Forjaz MJ, et al. Multimorbidity care model: recommendations from the consensus meeting of the Joint Action on Chronic Diseases and Promoting Healthy Ageing across the Life Cycle (JA-CHRODIS). Health Policy. 2018;122(1):4–11. doi:10.1016/j.healthpol.2017.09.006
15. Salisbury C, Man MS, Bower P, et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet. 2018;392(10141):41–50. doi:10.1016/s0140-6736(18)31308-4
16. Hopman P, de Bruin SR, Forjaz MJ, et al. Effectiveness of comprehensive care programs for patients with multiple chronic conditions or frailty: a systematic literature review. Health Policy. 2016;120(7):818–832. doi:10.1016/j.healthpol.2016.04.002
17. Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2021;1(1):Cd006560. doi:10.1002/14651858.CD006560.pub4
18. Guthrie B, Payne K, Alderson P, McMurdo ME, Mercer SW. Adapting clinical guidelines to take account of multimorbidity. BMJ. 2012;345:e6341. doi:10.1136/bmj.e6341
19. Muth C, Glasziou PP. Guideline recommended treatments in complex patients with multimorbidity. BMJ. 2015;351:h5145. doi:10.1136/bmj.h5145
20. Vetrano DL, Calderón-Larrañaga A, Marengoni A, et al. An international perspective on chronic multimorbidity: approaching the elephant in the room. J Gerontol A Biol Sci Med Sci. 2018;73(10):1350–1356. doi:10.1093/gerona/glx178
21. Juul-Larsen HG, Andersen O, Bandholm T, et al. Differences in function and recovery profiles between patterns of multimorbidity among older medical patients the first year after an acute admission-An exploratory latent class analysis. Arch Gerontol Geriatr. 2020;86:103956. doi:10.1016/j.archger.2019.103956
22. Álvarez-Gálvez J, Ortega-Martín E, Carretero-Bravo J, Pérez-Muñoz C, Suárez-Lledó V, Ramos-Fiol B. Social determinants of multimorbidity patterns: a systematic review. Front Public Health. 2023;11:1081518. doi:10.3389/fpubh.2023.1081518
23. Marengoni A, Akugizibwe R, Vetrano DL, et al. Patterns of multimorbidity and risk of disability in community-dwelling older persons. Aging Clin Exp Res. 2021;33(2):457–462. doi:10.1007/s40520-020-01773-z
24. Vetrano DL, Damiano C, Tazzeo C, et al. Multimorbidity patterns and 5-year mortality in institutionalized older adults. J Am Med Dir Assoc. 2022;23(8):1389–1395.e4. doi:10.1016/j.jamda.2022.01.067
25. Tazzeo C, Rizzuto D, Calderón-Larrañaga A, et al. Multimorbidity patterns and risk of frailty in older community-dwelling adults: a population-based cohort study. Age Ageing. 2021;50(6):2183–2191. doi:10.1093/ageing/afab138
26. Wang Z, Peng W, Li M, et al. Association between multimorbidity patterns and disability among older people covered by long-term care insurance in Shanghai, China. BMC Public Health. 2021;21(1):418. doi:10.1186/s12889-021-10463-y
27. Akugizibwe R, Calderón-Larrañaga A, Roso-Llorach A, et al. Multimorbidity patterns and unplanned hospitalisation in a cohort of older adults. J Clin Med. 2020;9(12):4001. doi:10.3390/jcm9124001
28. Munyombwe T, Dondo TB, Aktaa S, et al. Association of multimorbidity and changes in health-related quality of life following myocardial infarction: a UK multicentre longitudinal patient-reported outcomes study. BMC Med. 2021;19(1):227. doi:10.1186/s12916-021-02098-y
29. Busija L, Lim K, Szoeke C, Sanders KM, McCabe MP. Do replicable profiles of multimorbidity exist? Systematic review and synthesis. Eur J Epidemiol. 2019;34(11):1025–1053. doi:10.1007/s10654-019-00568-5
30. Liu-Ambrose T, Davis JC, Best JR, et al. Effect of a home-based exercise program on subsequent falls among community-dwelling high-risk older adults after a fall: a randomized clinical trial. JAMA. 2019;321(21):2092–2100. doi:10.1001/jama.2019.5795
31. Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged ≥65 years - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(37):993–998. doi:10.15585/mmwr.mm6537a2
32. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61. doi:10.1016/j.maturitas.2013.02.009
33. Cuevas-Trisan R. Balance problems and fall risks in the elderly. Clin Geriatr Med. 2019;35(2):173–183. doi:10.1016/j.cger.2019.01.008
34. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi:10.1056/nejm198812293192604
35. Huimin C, Yilong W. Review on gait analysis. Chin J Stroke. 2020;15(1):102–107. doi:10.3969/j.issn.1673-5765.2020.01.017
36. McIlroy WE, Maki BE. Age-related changes in compensatory stepping in response to unpredictable perturbations. J Gerontol A Biol Sci Med Sci. 1996;51(6):M289–M296. doi:10.1093/gerona/51a.6.m289
37. Mahlknecht P, Kiechl S, Bloem BR, et al. Prevalence and burden of gait disorders in elderly men and women aged 60–97 years: a population-based study. PLoS One. 2013;8(7):e69627. doi:10.1371/journal.pone.0069627
38. Auvinet B, Touzard C, Montestruc F, Delafond A, Goeb V. Gait disorders in the elderly and dual task gait analysis: a new approach for identifying motor phenotypes. J Neuroeng Rehabil. 2017;14(1):7. doi:10.1186/s12984-017-0218-1
39. Cahalan TD, Johnson ME, Liu S, Chao EY. Quantitative measurements of Hip strength in different age groups. Clin Orthop Relat Res. 1989;246:136–145. doi:10.1097/00003086-198909000-00022
40. Winegard KJ, Hicks AL, Sale DG, Vandervoort AA. A 12-year follow-up study of ankle muscle function in older adults. J Gerontol a Biol Sci Med Sci. 1996;51(3):B202–7. doi:10.1093/gerona/51a.3.b202
41. Scott D, Stuart AL, Kay D, Ebeling PR, Nicholson G, Sanders KM. Investigating the predictive ability of gait speed and quadriceps strength for incident falls in community-dwelling older women at high risk of fracture. Arch Gerontol Geriatr. 2014;58(3):308–313. doi:10.1016/j.archger.2013.11.004
42. Song Q, Zhang X, Mao M, et al. Relationship of proprioception, cutaneous sensitivity, and muscle strength with the balance control among older adults. J Sport Health Sci. 2021;10(5):585–593. doi:10.1016/j.jshs.2021.07.005
43. Alexander NB. Differential diagnosis of gait disorders in older adults. Clin Geriatr Med. 1996;12(4):689–703. doi:10.1016/S0749-0690(18)30196-4
44. Salzman B. Gait and balance disorders in older adults. Am Fam Physician. 2010;82(1):61–68.
45. Kuo HK, Yu YH. The relation of peripheral arterial disease to leg force, gait speed, and functional dependence among older adults. J Gerontol A Biol Sci Med Sci. 2008;63(4):384–390. doi:10.1093/gerona/63.4.384
46. Huberty S, Freystätter G, Wieczorek M, et al. Association between multimorbidity and rate of falls: a 3-year 5-country prospective study in generally healthy and active community-dwelling adults aged ≥70 years. J Am Med Dir Assoc. 2023;24(6):804–810.e4. doi:10.1016/j.jamda.2022.12.011
47. Jacob L, Shin JI, Kostev K, et al. Prospective association between multimorbidity and falls and its mediators: findings from the Irish longitudinal study on ageing. J Clin Med. 2022;11(15):4470. doi:10.3390/jcm11154470
48. Barik M, Panda SN, Tripathy SS, et al. Is multimorbidity associated with higher risk of falls among older adults in India? BMC Geriatr. 2022;22(1):486. doi:10.1186/s12877-022-03158-5
49. You L, Guo L, Li N, Zhong J, Er Y, Zhao M. Association between multimorbidity and falls and fear of falling among older adults in eastern China: a cross-sectional study. Front Public Health. 2023;11:1146899. doi:10.3389/fpubh.2023.1146899
50. Yan J, Wang M, Cao Y. Patterns of multimorbidity in association with falls among the middle-aged and older adults: results from the China Health and Retirement Longitudinal Study. BMC Public Health. 2022;22(1):1814. doi:10.1186/s12889-022-14124-6
51. Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1(1):Cd012424. doi:10.1002/14651858.CD012424.pub2
52. Kannus P, Sievänen H, Palvanen M, Järvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366(9500):1885–1893. doi:10.1016/s0140-6736(05)67604-0
53. Nightingale CJ, Mitchell SN, Butterfield SA. Validation of the timed up and go test for assessing balance variables in adults aged 65 and older. J Aging Phys Act. 2019;27(2):230–233. doi:10.1123/japa.2018-0049
54. Bohannon RW. Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills. 1995;80(1):163–166. doi:10.2466/pms.1995.80.1.163
55. Butler AA, Menant JC, Tiedemann AC, Lord SR. Age and gender differences in seven tests of functional mobility. J Neuroeng Rehabil. 2009;6:31. doi:10.1186/1743-0003-6-31
56. Peel NM, Kuys SS, Klein K. Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci. 2013;68(1):39–46. doi:10.1093/gerona/gls174
57. Tiedemann A, Shimada H, Sherrington C, Murray S, Lord S. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing. 2008;37(4):430–435. doi:10.1093/ageing/afn100
58. Kang L, Han P, Wang J, et al. Timed Up and Go Test can predict recurrent falls: a longitudinal study of the community-dwelling elderly in China. Clin Interv Aging. 2017;12:2009–2016. doi:10.2147/cia.S138287
59. Alosaimi RM, Almegbas NR, Almutairi GR, et al. The Five Times Sit-to-Stand Test is associated with both history of falls and fear of falling among community adults aged 50 years and older. Ir J Med Sci. 2023. doi:10.1007/s11845-023-03287-9
60. Buatois S, Miljkovic D, Manckoundia P, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc. 2008;56(8):1575–1577. doi:10.1111/j.1532-5415.2008.01777.x
61. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. doi:10.1093/ptj/80.9.896
62. Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67(3):254–266. doi:10.1016/j.jclinepi.2013.09.021
63. Sinha P, Calfee CS, Delucchi KL. Practitioner’s guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. 2021;49(1):e63–e79. doi:10.1097/ccm.0000000000004710
64. Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–439. doi:10.1016/j.arr.2011.03.003
65. Skou ST, Mair FS, Fortin M, et al. Multimorbidity. Nat Rev Dis Primers. 2022;8(1):48. doi:10.1038/s41572-022-00376-4
66. Van Wilder L, Devleesschauwer B, Clays E, et al. The impact of multimorbidity patterns on health-related quality of life in the general population: results of the Belgian Health Interview Survey. Qual Life Res. 2022;31(2):551–565. doi:10.1007/s11136-021-02951-w
67. Galenkamp H, Braam AW, Huisman M, Deeg DJ. Somatic multimorbidity and self-rated health in the older population. J Gerontol B Psychol Sci Soc Sci. 2011;66(3):380–386. doi:10.1093/geronb/gbr032
68. Di Angelantonio E, Kaptoge S, Wormser D, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. 2015;314(1):52–60. doi:10.1001/jama.2015.7008
69. Olson JE, Takahashi PY, St Sauver JM. Understanding the patterns of multimorbidity. Mayo Clin Proc. 2018;93(7):824–825. doi:10.1016/j.mayocp.2018.05.016
70. Boyd CM, Kent DM. Evidence-based medicine and the hard problem of multimorbidity. J Gen Intern Med. 2014;29(4):552–553. doi:10.1007/s11606-013-2658-z
71. Puri P, Singh SK, Pati S. Identifying non-communicable disease multimorbidity patterns and associated factors: a latent class analysis approach. BMJ Open. 2022;12(7):e053981. doi:10.1136/bmjopen-2021-053981
72. Roomaney RA, van Wyk B, Cois A, Pillay van-Wyk V. Multimorbidity patterns in South Africa: a latent class analysis. Front Public Health. 2022;10:1082587. doi:10.3389/fpubh.2022.1082587
73. Whitson HE, Johnson KS, Sloane R, et al. Identifying patterns of multimorbidity in older Americans: application of latent class analysis. J Am Geriatr Soc. 2016;64(8):1668–1673. doi:10.1111/jgs.14201
74. Kirchberger I, Meisinger C, Heier M, et al. Patterns of multimorbidity in the aged population. Results from the KORA-Age study. PLoS One. 2012;7(1):e30556. doi:10.1371/journal.pone.0030556
75. Rajoo SS, Wee ZJ, Lee PSS, Wong FY, Lee ES. A systematic review of the patterns of associative multimorbidity in Asia. Biomed Res Int. 2021;2021:6621785. doi:10.1155/2021/6621785
76. Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380(9841):601–610. doi:10.1016/s0140-6736(12)60987-8
77. Hamilton BP. Diabetes mellitus and hypertension. Am J Kidney Dis. 1990;16(4 Suppl 1):20–29.
78. Gu J, Chao J, Chen W, et al. Multimorbidity and health-related quality of life among the community-dwelling elderly: a longitudinal study. Arch Gerontol Geriatr. 2018;74:133–140. doi:10.1016/j.archger.2017.10.019
79. Honda Y, Nakamura M, Aoki T, Ojima T. Multimorbidity patterns and the relation to self-rated health among older Japanese people: a nationwide cross-sectional study. BMJ Open. 2022;12(9):e063729. doi:10.1136/bmjopen-2022-063729
80. Wang R, Yan Z, Liang Y, et al. Prevalence and patterns of chronic disease pairs and multimorbidity among older Chinese adults living in a rural area. PLoS One. 2015;10(9):e0138521. doi:10.1371/journal.pone.0138521
81. Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke. 2005;36(6):1330–1340. doi:10.1161/01.Str.0000165928.19135.35
82. Veronese N, Solmi M, Maggi S, et al. Frailty and incident depression in community-dwelling older people: results from the ELSA study. Int J Geriatr Psychiatry. 2017;32(12):e141–e149. doi:10.1002/gps.4673
83. Menezes KK, Nascimento LR, Avelino PR, Alvarenga MTM, Teixeira-Salmela LF. Efficacy of interventions to improve respiratory function after stroke. Respir Care. 2018;63(7):920–933. doi:10.4187/respcare.06000
84. Soley-Bori M, Bisquera A, Ashworth M, et al. Identifying multimorbidity clusters with the highest primary care use: 15 years of evidence from a multi-ethnic metropolitan population. Br J Gen Pract. 2022;72(716):e190–e198. doi:10.3399/bjgp.2021.0325
85. Zhou J, Wei MY, Zhang J, Liu H, Wu C. Association of multimorbidity patterns with incident disability and recovery of Independence among middle-aged and older adults. Age Ageing. 2022;51(8). doi:10.1093/ageing/afac177
86. Zhu Y, Edwards D, Mant J, Payne RA, Kiddle S. Characteristics, service use and mortality of clusters of multimorbid patients in England: a population-based study. BMC Med. 2020;18(1):78. doi:10.1186/s12916-020-01543-8
87. Yardley L, Bishop FL, Beyer N, et al. Older people’s views of falls-prevention interventions in six European countries. Gerontologist. 2006;46(5):650–660. doi:10.1093/geront/46.5.650
88. Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–1758. doi:10.1136/bjsports-2016-096547
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
