Back to Journals » Open Access Journal of Sports Medicine » Volume 12
MRI-Detected Knee Ligament Sprains and Associated Internal Derangement in Athletes Competing at the Rio de Janeiro 2016 Summer Olympics
Authors Kompel A , Haran PH, Murakami AM , Engebretsen L , Jarraya M, Roemer F, Guermazi A
Received 24 November 2020
Accepted for publication 16 February 2021
Published 8 March 2021 Volume 2021:12 Pages 23—32
DOI https://doi.org/10.2147/OAJSM.S292763
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Andreas Imhoff
Andrew Kompel,1 Prashanth H Haran,1 Akira M Murakami,1 Lars Engebretsen,2– 4 Mohamed Jarraya,1,5 Frank Roemer,1,6,* Ali Guermazi1,7,*
1Department of Radiology, Boston University School of Medicine, Boston, MA, USA; 2Medical and Scientific Department, International Olympic Committee, Lausanne, Switzerland; 3Oslo Sports Trauma Research Center, Department of Sports Medicine, Norwegian School of Sport Sciences, Oslo, Norway; 4Department of Orthopedic Surgery, Oslo University Hospital, University of Oslo, Oslo, Norway; 5Department of Radiology, Brigham and Women’s Hospital, Boston, MA, USA; 6Department of Radiology, Friedrich-Alexander University Erlangen-Nürnberg, & Universitätsklinikum Erlangen, Erlangen, Germany; 7Department of Radiology, VA Boston Health System, Boston, MA, USA
*These authors contributed equally to this work
Correspondence: Andrew Kompel
Department of Radiology, Boston University School of Medicine, 820 Harrison Avenue, FGH Building 3rd Floor, Boston, MA, 02118, USA
Tel +1 617 638-6610
Fax +1 617 638-6616
Email [email protected]
Purpose: Describe the frequency and severity of knee ligament sprains diagnosed by MRI in athletes participating at the 2016 Summer Olympic Games, their association with certain sports and assess correlations with additional knee structural injury.
Patients and Methods: All knee MRIs performed in the Olympic Village and polyclinics during the 2016 Olympics were retrospectively, blindly reviewed for ligament sprains and associated knee injuries. In addition to the absence or presence of these abnormalities, athletes were stratified by age, gender and sport.
Results: 11,274 athletes participated in the 2016 Olympic Games: 113 athletes received at least one knee MRI with some having bilateral or repeat MRI on the same knee. Anterior cruciate and medial collateral ligament (ACL/MCL) sprains were most common, accounting for 32 of the 43 sprains (74.4%). Wrestling (10), hockey (7), athletics (7), and judo (5) accounted for over half of ligament sprains. ACL sprains showed a significant positive correlation with medial, lateral meniscal tears and bone contusions. The positive correlation between posterior cruciate ligament (PCL) sprains with MCL/lateral collateral ligament sprain, and popliteus tendon tear was statistically significant with 50% of total PCL sprains occurring in hockey. When athletes were stratified by gender, ligament sprains had a similar occurrence and distribution between men and women.
Conclusion: Knee ligament sprains, at the Rio 2016 Games, were most common in wrestling, hockey, athletics and judo with ACL and MCL sprains most frequent. Meniscal tears and bone contusions occurred often with ACL sprains. PCL sprains tended to be multi-ligamentous injuries. Sustained ligament sprains had similar occurrence between genders, while men had a peak incidence of sprains at a younger age and women at an older age.
Keywords: Olympics, knee, ligament, sprain, MRI
Introduction
The 2016 Rio de Janeiro Summer Olympic Games brought together worldwide, elite athletes at the height of their careers. Epidemiology and clinical-based information on sports injuries from the Olympic Games has been published, demonstrating the common nature of knee injuries among Olympic athletes.1–6 The high intensity and volume of training undertaken by these athletes make them susceptible to overuse and traumatic (contact and noncontact) injuries. Acute injuries have been shown as more common during competition, though overuse injuries are not infrequent.4 The most common sports-related knee injuries associated with acute trauma are medial meniscal and anterior cruciate ligament tears.7 However, low grade injuries including tendinitis and mild sprains were the most commonly described abnormalities at an Olympic training center.5 Additionally, certain sporting activities are associated with higher occurrence of all types and number of injuries.7
In Olympic and other high-level athletes, knee pain from acute injury or repetitive microtrauma is not uncommon, and magnetic resonance imaging (MRI) is a highly specific tool for characterizing internal derangement and determining the severity with high sensitivity.8,9 In addition to being a heavily utilized modality for diagnosing injuries, MRI serves a vital role in determining treatment and potentially impacting return to play.1,10 During the Rio 2016 Olympic Games, new or recurring injury led to at least one day of missed sporting activity in 40% of athletes, and that 20% of injuries resulted in at least 7 days of missed time. Of all possible anatomical locations, the knee was the most common site of injury (n=130).6
Kompel et al previously demonstrated that ligament sprains were not infrequent in this same Olympic population, being the third most common abnormality on MRI after cartilage damage and meniscal tears. Additionally, wrestling, athletics (track and field), judo, and hockey were the sports with the highest number of ligament sprains.11 However, the specific ligaments that were sprained and correlation with additional knee abnormalities were not analyzed. Given the relative high prevalence of ligament sprains in this population further detailed analysis is warranted to identify which athletes may be at highest risk.
The aim of our study is to describe the frequency of specific knee ligament sprains, diagnosed by MRI, in participating athletes at the Rio de Janeiro 2016 Summer Olympic Games. These injuries were then correlated with sport, other internal derangements of the knee and the age/gender of the athlete.
Methods
Subjects’ MRIs
The methods, including the data collection and image analysis, are similar to those performed by Kompel et al.11 We reviewed all knee MRI studies (GE Medical Systems) performed on athletes at the Rio 2016 Olympic Games while the Olympic Village was open (32 days), and were obtained from the Radiological Information System (RIS) and Picture Archiving and Communication System (PACS). The MRIs were performed for either chronic/recurrent knee pain without trauma or an acute injury while at the Games. In order to prevent duplicate results, as some athletes were treated by both the Rio 2016 medical staff and the National Olympic Committee (NOC) for the same condition, the athlete accreditation number was used. For duplicate results, the NOC data was utilized. Our study and intent to publish the data was approved by the International Olympic Committee (IOC).
Confidentiality and Ethical Approval
Athlete accreditation numbers were used to search the IOC database for athletes who had a knee MRI and to record their nationality, gender, and age. The information remained confidential and was de-identified in the database following the query. The medical research ethics division committee of the Southeastern Norway Regional Health Authority approved our study (#S-07196C) and a second IRB was obtained from Boston University (#H-36593). The requirement for informed consent was waived, as the data in this study was de-identified and anonymized. The athletes’ information was gathered, retained, and examined in strict adherence with data protection and confidentiality. The IOC consented to the review of the anonymized demographic data and imaging for publication.
Data Collection
In the Olympic Village, MRI’s were performed at the official IOC clinics, using 3T Discovery MR750w and 1.5T Optima 450 MRw MR scanners (GE Healthcare, Brazil). As previously detailed, the MRI images were retrospectively gathered through RIS. Athletes’ demographic data was anonymized and the information was stratified according to age, gender, country, sport-type, and specific internal knee derangement. MRI sequences performed included fat-suppressed proton density (intermediate-weighting) in multiple planes (axial, sagittal, and coronal), sagittal T2-weighted, and T1-weighted images in 1–3 planes (sagittal plane most commonly performed).
Imaging Analysis
A musculoskeletal (MSK) radiologist with board certification and 7-years MSK sub-specialization (AJK) blindly and independently analyzed every knee MRI without knowledge of the initial report or clinical history. The MRIs were evaluated for abnormalities of all ligaments, menisci, cartilage, tendons and osseous structures, as well as the presence of an ACL graft.
Medial and lateral collateral ligament (MCL/LCL) sprains were graded based on their MRI characteristics including hyperintense signal superficial and deep to the ligament without discontinuity of the fibers (Grade 1), partial tearing of the fibers (Grade 2) or complete rupture of the ligament (Grade 3). All grades of ligament sprains were added together for analysis. Anterior and posterior cruciate ligament sprains (ACL/PCL) included partial and complete tears.12 Diagnosis of a meniscal tear included a flap or displaced tear (abnormal meniscal morphology) or hyperintense linear signal extending to the articular surface on two consecutive MRI images.13 Cartilage analysis followed the modified Outerbridge grading system with any cartilage loss (fraying/blistering to full thickness loss) included as cartilage abnormalities.14 For this study, cartilage heterogeneity without thinning was not considered an abnormality (Grade1). Tendon injuries included both partial or complete tears.15,16 Tendinosis was not included as an injury. Bone contusion was based on marrow edema on the fat-suppressed proton-density without circumscribed borders or fracture line.17
Statistical Analysis
Ligament sprains were grouped according to ligament involved (ACL, PCL, MCL, LCL). In addition, associated internal derangement (including other ligament sprains, meniscal tears, cartilage damage, tendon tears, and bone contusions) within the same knee was identified. To evaluate any significant correlation between the presence of a specific ligament sprain and associated internal derangement, a Pearson correlation coefficient (Pearson’s r) was performed.
A second reader (AG) assessed 30 random cases for image interpretation reliability using prevalence-adjusted and bias-adjusted kappa (PABAK) and overall percent agreement (Appendix). A few of the MRI findings were not common/low prevalence, therefore, PABAK was used for assessment as kappa was described previously as being highly dependent on prevalence.
Results
11274 athletes participated in the 2016 Olympic Games: 113 of these athletes received at least one knee MRI in the Olympic village, while 9 had bilateral knee MRIs or a repeat MRI on the same side. There was a total of 43 ligament sprains identified, with the highest number being complete ACL, Grade 1 MCL, and Grade 2 MCL sprains – 15, 9, and 6 respectively. When grouped, the total number of ACL and MCL sprains accounted for roughly 75% of all ligament sprains – 32 of 43 total. Wrestling, hockey, athletics, and judo together accounted for over half the total number of ligament sprains identified. A detailed overview of these results is presented in Table 1.
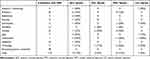 |
Table 1 Distribution of Ligament Sprain by Sport |
The positive correlation between grouped ACL sprains (partial and complete combined) was statistically significant with medial (r= 0.34) and lateral (r=0.32) meniscal tears, lateral femoral condyle (r=0.51), medial (r=0.38) and lateral tibial plateau (r=0.52) bone contusions. The positive correlation between grouped MCL sprains was statistically significant with PCL sprain (r=0.49), popliteus tendon tear (r=0.34), and lateral tibial plateau bone contusions (r=0.28). The positive correlation between grouped LCL sprains was statistically significant with ACL (r=0.31) and MCL sprains (r=0.33), tendon tears [semimembranosus (r=0.35) and popliteus (r=0.37)] and lateral femoral condyle bone contusion (r=0.31). Positive correlation between grouped PCL sprains was statistically significant with MCL (r=0.49) and LCL (r=0.28) sprains, semimembranosus (r=0.34), medial gastrocnemius (r=0.27), and popliteus tendon tears (r=0.49). There was no statistically significant correlation between grouped ligament sprains and cartilage damage (results summarized in Table 2).
 |
Table 2 Correlation Between Specific Knee Ligament Sprains and Other Internal Derangement |
When ligament sprains were stratified by age and sex, the overall prevalence of sprains between men and women are similar. In male athletes, ligament sprains occurred most frequently in ages 20–29 years old, with MCL and ACL injuries being the most common (17 of 23 ligament sprains, 11 of which were MCL or ACL injuries). Female athletes aged 20–29 also had the most identified ligament sprains (13 of 20 ligament injuries, 10 of which were MCL or ACL injuries). In both men and women, there were more sprains in the 30–39 age group than seen in the 15–19 age group (results summarized in Table 3).
 |
Table 3 Age and Gender Stratification of Ligament Sprains |
Discussion
Our data showed that of the total number of knee MRIs performed at the 2016 Olympic village and polyclinics, over one third demonstrated some form of ligament sprain. The most common of these injuries were ACL and MCL sprains of various severity – more commonly complete disruption of the ACL and lower grade sprains (Grade 1 and 2) involving the MCL (Figure 1A and B). The sports in which these ligament sprains were detected the most – wrestling, hockey, athletics, and judo - have been shown to carry a greater than 10% risk of injury to participating athletes.6,7,18,19
Knee injuries in wrestling are common, with collateral ligament sprains occurring much more frequently than ACL sprains.20,21 Our results support this literature by demonstrating that wrestling did not only have the most ligament sprains compared to other sports but also collateral ligament sprains outnumbered cruciate ligament tears. The mechanism of ligament injury is most often due to rotation on a planted foot with the leg in extension, usually during a takedown.20,21 In hockey, lower extremity injuries are the most common with ACL and collateral ligament sprains, caused by non-contact maneuvers including “cutting” and deceleration.22–24 Athletics encompasses many different types of running, jumping and throwing events in various combinations and distances. Injuries almost always are caused by overuse or non-contact trauma, and the lower extremity is the most commonly involved anatomical region with knee injuries representing a relatively high percentage of these lower extremity injuries.25–27 While tendinosis, tibial stress, and patellofemoral syndrome are more common injuries and related to overuse, acute ligament sprains can result from non-contact, especially in events requiring quick bouts of acceleration including sprinting, hurdles, jumping, and multi-event athletes.27,28 Judo had the 4th most ligament sprains composed mostly of ACL sprains. ACL rupture has been shown to not only be a frequent injury in Judo but also the most common severe type injury leading to months of recovery and decreased performance.7,19,29 The risk of ACL and MCL sprains in judo has been shown to significantly increase to the athlete being attacked rather than attempting to attack, certain leg techniques (such as osoto-gari), and with opponents having different grip styles.19,30
Our data also highlights associations within ligamentous sprains, and between ligament injury and other internal derangement diagnosed by MRI. The most pronounced correlation was between ACL sprains, meniscal tears, and bone contusions to the lateral femoral condyle, medial tibial plateau, and lateral tibial plateau (Figure 2A–C). Bone contusions associated with ACL sprain have been documented to have prevalence of up to 70% and more commonly occur than the traditional “unhappy triad” confluence of ACL, MCL, and medial meniscal tear.31 The significant correlation between ACL sprains with medial and lateral meniscal tears is in agreement with prior reports of meniscal tears (medial/lateral or both) occurring with an ACL sprain in 59–79% of cases, with the meniscal tears being nearly split evenly between medial and lateral.32,33 Additionally, while not a statistically significant correlation (p = 0.13), about a quarter of athletes with ACL sprains did have a concomitant MCL sprain indicating a trend for these injuries to occur together and percentage-wise comparable to previous literature.34
Multi-ligamentous knee injury is defined as involving at least 2 of the 4 major knee ligaments usually with at least one of these ligamentous being completely ruptured.35 Multi-ligamentous knee injuries have been shown to involve up to 11% of knee ligament sprains presenting for treatment with combined ACL/MCL sprains most frequent.35,36 While ACL/MCL combined injury was observed in this Olympic population, there was a significant correlation with PCL sprains occurring with MCL and/or LCL sprains and popliteus tendon tears, indicating injury to the posterolateral corner (Figure 3A–C). Although PCL sprains are much less common than ACL injuries, PCL sprains are known to commonly occur with other ligament (up to 95% of cases) and posterolateral corner knee injuries potentially related to the mechanism of injury or higher energy trauma required to injure the PCL.37–39 Therefore, if there is suspicion for PCL injury, the likelihood of concomitant internal derangement should be highly suspected, and MRI is highly accurate in diagnosing all related injuries.39,40 While isolated PCL injuries, especially low-to-moderate grade sprain, can be treated non-operatively, complete rupture or avulsion of the PCL and associated ligamentous/posterolateral corner injuries commonly require surgical intervention. Correct diagnosis of these injuries is critically important to the surgical planning, to ensure post-operative stability to the knee.38,41,42
The highest number of ligament sprains was observed in both male and female athletes aged 20–29, which can be expected given this age group has the largest number of competitors. Additionally, ligament sprains were nearly equally distributed between men and woman in terms of number and location of the sprain. Previous research demonstrates that woman have a higher rate of non-contact ACL tears which is thought to be related to underlying bone geometry, more specifically a shortened and rounded tibial plateau and increased tibial slope.43,44 However, when evaluating ACL sprains resulting from contact and non-contact causes and the sport involved, there are similar rates of ACL tears between genders.45,46 In terms of age, the sport and gender of the athlete have potential impact on spraining a knee ligament.47 For men, the rate of ligament sprain decreased with increasing age, which could represent younger athletes competing in sports with a higher risk of knee sprain compared to the older athletes.48 Additionally, previous research supports that the incidence of isolated ACL tears in men significantly decreases as age increases.49 For women, the rate increased with increasing age which could be related to sport. However, previous studies have shown that males have a peak incidence of ACL rupture in their early twenties and women have a second peak occurrence in their forties with an overall advanced age compared to men for when the sprain occurs.50 This increased risk for ligament sprain in older athletes is thought to be related age-dependent changes in connective tissue possible related to impaired healing capacity and vascular supply.51 Independent of the cause, this data should guide sports medicine personnel to the potential increased risk in older athletes, especially woman, and implement injury prevention mechanisms.
This study included all MRIs performed at the Olympic village and polyclinics however, if an athlete was transferred to an outside hospital for treatment, likely for more serious injuries, any MRIs at that hospital and the athlete’s knee injuries were not included in this analysis. The clinical context for obtaining an MRI was not known in this retrospective review. This includes the indication for the MRI (acute injury during the games, recurrent injury or pain present while at the Games without a trauma), physical exam findings, mechanism of injury (if a trauma occurred), treatment, and any return to play timeline. Also, the overall sample size is small, including 130 athletes who were clinically diagnosed with a knee injury and 113 athletes had an MRI performed in the Olympic village/polyclinics.
These results show that ligament sprains in Olympians align with other high-performing athletic populations and associated internal knee derangement is consistent with previously described patterns. Given the volume and intensity levels these athletes train, knowing which athletes and sports may be more susceptible can lead to increased surveillance and potential injury mitigation training techniques. Additionally, performing this analysis over multiple Olympic Games will further delineate significant associations between knee ligament sprains, concomitant internal derangement and the association with certain sports and athletes’ demographics.
Conclusion
Ligament sprains are the third most common knee lesion in this Olympic population after cartilage damage and meniscal tears. Certain sports are more commonly associated with knee ligament sprains including wrestling, hockey, athletes and judo. ACL and MCL sprains were detected most frequently and could result from contact and non-contact mechanisms depending on the sport. In support of the literature, ACL sprains commonly have associated injuries including medial and/or lateral meniscal tears and bone contusion. PCL sprains, though much less common, are usually multi-ligamentous injuries, including the posterolateral corner, and frequently require surgical intervention. When evaluating ligament sprains based on gender and age, the overall rate of occurrence is similar between gender when including contact and noncontact sports.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Ali Guermazi is the president of Boston Imaging Core Lab (BICL), LLC, and a consultant to Merck Serono, AstraZeneca, Pfizer, Galapagos, Roche and TissueGene. Frank Roemer is a shareholder of BICL, LLC. Lars Engebretsen is a consultant to Arthrex, Smith and Nephew, and head of Scientific Activities in the IOC. Akira Murakami, Andrew J. Kompel, and Mohamed Jarraya are consultants for BICL. Prashanth Haran has nothing to disclose.
References
1. Bethapudi S, Budgett R, Engebretsen L, O’Connor P. Imaging at London 2012 summer Olympic Games: analysis of demand and distribution of workload. Br J Sports Med. 2013;47(13):850–856. doi:10.1136/bjsports-2013-092345
2. Calhoon G, Fry AC. Injury rates and profiles of elite competitive weightlifters. J Athl Train. 1999;34(3):232–238.
3. Engebretsen L, Soligard T, Steffen K, et al. Sports injuries and illnesses during the London Summer Olympic Games 2012. Br J Sports Med. 2013;47(7):407–414. doi:10.1136/bjsports-2013-092380
4. Junge A, Engebretsen L, Mountjoy ML, et al. Sports injuries during the Summer Olympic Games 2008. Am J Sports Med. 2009;37(11):2165–2172. doi:10.1177/0363546509339357
5. Micheo WF, Figueroa C. Comparison of the pattern of injuries in children and adult athletes. The first 10 years experience at the Olympic Training Center. Bol Asoc Med P R. 2006;98(1):7–14.
6. Soligard T, Steffen K, Palmer D, et al. Sports injury and illness incidence in the Rio de Janeiro 2016 Olympic Summer Games: a prospective study of 11274 athletes from 207 countries. Br J Sports Med. 2017;51(17):1265–1271. doi:10.1136/bjsports-2017-097956
7. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. doi:10.1016/j.knee.2006.01.005
8. Boeve BF, Davidson RA, Staab EV
9. Guermazi A, Hayashi D, Jarraya M, et al. Sports injuries at the Rio de Janeiro 2016 Summer Olympics: use of diagnostic imaging services. Radiology. 2018;287(3):922–932. doi:10.1148/radiol.2018171510
10. Bethapudi S, Ritchie D, Bongale S, Gordon J, MacLean J, Mendl L. Data analysis and review of radiology services at glasgow 2014 Commonwealth Games. Skeletal Radiol. 2015;44(10):1477–1483. doi:10.1007/s00256-015-2194-5
11. Kompel AJ, Murakami AM, Engebretsen L, et al. MRI-detected sports-related knee injuries and abnormalities at the Rio de Janeiro 2016 Summer Olympic Games. AJR Am J Roentgenol. 2018;211(4):880–886. doi:10.2214/AJR.17.19334
12. Nissman D, Hobbs R, Pope T, Geier D, Conway W. Imaging the knee: ligaments. Appl Radiol. 2008;37(12):25–32.
13. Lefevre N, Naouri JF, Herman S, et al. Review of the meniscus imaging: proposition of a useful tool for its radiologic analysis. Radiol Res Pract. 2016;2016:8329296. doi:10.1155/2016/8329296
14. Jungius KP, Schmid MR, Zanetti M, Hodler J, Koch P, Pfirrmann CW. Cartilaginous defects of the femorotibial joint: accuracy of coronal short inversion time inversion-recovery MR sequence. Radiology. 2006;240(2):482–488. doi:10.1148/radiol.2401050077
15. Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics. 2010;30(4):961–981. doi:10.1148/rg.304095755
16. Sonin AH, Fitzgerald SW, Bresler ME, Kirsch MD, Hoff FL, Friedman H. MR imaging appearance of the extensor mechanism of the knee: functional anatomy and injury patterns. Radiographics. 1995;15(2):367–382. doi:10.1148/radiographics.15.2.7761641
17. Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000;20 Spec No:S135–S151. doi:10.1148/radiographics.20.suppl_1.g00oc19s135
18. Jarret GJ, Orwin JF, Dick RW. Injuries in collegiate wrestling. Am J Sports Med. 1998;26(5):674–680. doi:10.1177/03635465980260051301
19. Pocecco E, Ruedl G, Stankovic N, et al. Injuries in judo: a systematic literature review including suggestions for prevention. Br J Sports Med. 2013;47(18):1139–1143. doi:10.1136/bjsports-2013-092886
20. Lightfoot AJ, McKinley T, Doyle M, Amendola A. ACL tears in collegiate wrestlers: report of six cases in one season. Iowa Orthop J. 2005;25:145–148.
21. Wroble RR, Mysnyk MC, Foster DT, Albright JP. Patterns of knee injuries in wrestling: a six year study. Am J Sports Med. 1986;14(1):55–66. doi:10.1177/036354658601400110
22. Barboza SD, Joseph C, Nauta J, van Mechelen W, Verhagen E. Injuries in field hockey players: a systematic review. Sports Med. 2018;48(4):849–866. doi:10.1007/s40279-017-0839-3
23. Junge A, Langevoort G, Pipe A, et al. Injuries in team sport tournaments during the 2004 Olympic Games. Am J Sports Med. 2006;34(4):565–576. doi:10.1177/0363546505281807
24. Rishiraj N, Taunton JE, Niven B. Injury profile of elite under-21 age female field hockey players. J Sports Med Phys Fitness. 2009;49(1):71–77.
25. D’Souza D. Track and field athletics injuries–a one-year survey. Br J Sports Med. 1994;28(3):197–202. doi:10.1136/bjsm.28.3.197
26. Edouard P, Morin J-B, Pruvost J, Kerspern A. Injuries in high-level heptathlon and decathlon. Br J Sports Med. 2011;45(4):346. doi:10.1136/bjsm.2011.084038.102
27. Bennell KL, Crossley K. Musculoskeletal injuries in track and field: incidence, distribution and risk factors. Aust J Sci Med Sport. 1996;28(3):69–75.
28. Zemper ED. Track and field injuries. Med Sport Sci. 2005;48:138–151. doi:10.1159/000084287
29. Akoto R, Lambert C, Balke M, Bouillon B, Frosch KH, Hoher J. Epidemiology of injuries in judo: a cross-sectional survey of severe injuries based on time loss and reduction in sporting level. Br J Sports Med. 2018;52(17):1109–1115. doi:10.1136/bjsports-2016-096849
30. Koshida S, Deguchi T, Miyashita K, Iwai K, Urabe Y. The common mechanisms of anterior cruciate ligament injuries in judo: a retrospective analysis. Br J Sports Med. 2010;44(12):856–861. doi:10.1136/bjsm.2008.051425
31. Papalia R, Torre G, Vasta S, et al. Bone bruises in anterior cruciate ligament injured knee and long-term outcomes. A review of the evidence. Open Access J Sports Med. 2015;6:37–48. doi:10.2147/OAJSM.S75345
32. Hagino T, Ochiai S, Senga S, et al. Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg. 2015;135(12):1701–1706. doi:10.1007/s00402-015-2309-4
33. Binfield PM, Maffulli N, King JB. Patterns of meniscal tears associated with anterior cruciate ligament lesions in athletes. Injury. 1993;24(8):557–561. doi:10.1016/0020-1383(93)90038-8
34. Remer EM, Fitzgerald SW, Friedman H, Rogers LF, Hendrix RW, Schafer MF. Anterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiographics. 1992;12(5):901–915. doi:10.1148/radiographics.12.5.1529133
35. Cox CL, Spindler KP. Multiligamentous knee injuries - surgical treatment algorithm. N Am J Sports Phys Ther. 2008;3(4):198–203.
36. Kaeding CC, Pedroza AD, Parker RD, Spindler KP, McCarty EC, Andrish JT. Intra-articular findings in the reconstructed multiligament-injured knee. Arthroscopy. 2005;21(4):424–430. doi:10.1016/j.arthro.2004.12.012
37. Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: part II. Arthroscopy. 1995;11(5):526–529. doi:10.1016/0749-8063(95)90127-2
38. Wind WM
39. Sonin AH, Fitzgerald SW, Friedman H, Hoff FL, Hendrix RW, Rogers LF. Posterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiology. 1994;190(2):455–458. doi:10.1148/radiology.190.2.8284399
40. Rodriguez W
41. Laprade RF, Wentorf FA, Olson EJ, Carlson CS. An in vivo injury model of posterolateral knee instability. Am J Sports Med. 2006;34(8):1313–1321. doi:10.1177/0363546506286785
42. Wiley WB, Askew MJ, Melby A
43. Wahl CJ, Westermann RW, Blaisdell GY, Cizik AM. An association of lateral knee sagittal anatomic factors with non-contact ACL injury: sex or geometry? J Bone Joint Surg Am. 2012;94(3):217–226. doi:10.2106/JBJS.K.00099
44. Senisik S, Ozgurbuz C, Ergun M, et al. Posterior tibial slope as a risk factor for anterior cruciate ligament rupture in soccer players. J Sports Sci Med. 2011;10(4):763–767.
45. Hurd WJ, Axe MJ, Snyder-Mackler L. Influence of age, gender, and injury mechanism on the development of dynamic knee stability after acute ACL rupture. J Orthop Sports Phys Ther. 2008;38(2):36–41. doi:10.2519/jospt.2008.2609
46. Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810–817. doi:10.4085/1062-6050-48.6.03
47. Gray AM, Buford WL. Incidence of patients with knee strain and sprain occurring at sports or recreation venues and presenting to United States Emergency Departments. J Athl Train. 2015;50(11):1190–1198. doi:10.4085/1062-6050-50.11.06
48. Watura C, Barton C, Webborn N, Maffulli N, Morrissey D. Sports injuries at the Olympics: a review of incidence related data from past games and the implications for FUTURE multi-sport events. Br J Sports Med. 2013;47(17):e4–e4. doi:10.1136/bjsports-2013-093073.1
49. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. doi:10.1177/0363546516629944
50. Nicholls M, Aspelund T, Ingvarsson T, Briem K. Nationwide study highlights a second peak in ACL tears for women in their early forties. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):648–654. doi:10.1007/s00167-017-4807-0
51. McCarthy MM, Hannafin JA. The mature athlete: aging tendon and ligament. Sports Health. 2014;6(1):41–48. doi:10.1177/1941738113485691
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



