Back to Journals » Infection and Drug Resistance » Volume 15
Mortality Predictors Among COVID-19 Elderly in Taif, Saudi Arabia
Authors Bakhshwin D, Alotaibi M, Ali AS, Althomali A, Alsuwat A, Alhamyani A, Alwathnani A, Alsaggaf S, Alrafiah A
Received 21 March 2022
Accepted for publication 9 June 2022
Published 20 June 2022 Volume 2022:15 Pages 3213—3223
DOI https://doi.org/10.2147/IDR.S364279
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Duaa Bakhshwin,1 Musim Alotaibi,2 Ahmed S Ali,1,3 Abdullah Althomali,2 Abdullah Alsuwat,2 Abdulrahman Alhamyani,2 Abdulqader Alwathnani,2 Samar Alsaggaf,4 Aziza Alrafiah5
1Department of Pharmacology Faculty of Medicine, King Abdulaziz University, Jeddah, Kingdom of Saudi Arabia; 2King Faisal Medical Complex, Taif, Kingdom of Saudi Arabia; 3Department of Pharmaceutics, Faculty of Pharmacy, Assiut University, Assiut, Egypt; 4Department of Anatomy, Faculty of Medicine, King Abdulaziz University, Jeddah, Kingdom of Saudi Arabia; 5Medical Laboratory Sciences, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Kingdom of Saudi Arabia
Correspondence: Aziza Alrafiah, Medical Laboratory Sciences, Faculty of Applied Medical Sciences, King Abdulaziz University, Jeddah, Kingdom of Saudi Arabia, Email [email protected]
Background: By December 2021, the COVID-19 pandemic had caused more than 266 million cases and 5 million deaths, especially among geriatric patients.
Objective: To identify determinants of COVID-19-related death in geriatric patients.
Methods: This is a comparative retrospective study involving 145 COVID-19 hospitalized patients who are more than 60 years old, conducted at King Faisal Medical Complex in Taif, Saudi Arabia, from June 2020 to August 2020. The main outcome studied was COVID-19-related death.
Results: Out of 145 elderly COVID-19 patients, 11% have died. There was a significant difference between those who died and the surviving group regarding hospital stay duration, with a higher duration median among those who died (22 days vs 12 day respectively, p=0.002). Transfer to ICU, mechanical ventilation, low oxygen saturation, shortness of breath, respiratory support, x-ray trend, and prolonged QT interval showed significant statistical differences between them (p< 0.001, < 0.001, 0.017, 0.045, < 0.001, < 0.001, 0.004, respectively). After doing logistic regression of predictors for progression to death, putting patients on oxygen only vs mechanical ventilation was statistically significant, with an adjusted odds ratio (AOR) of 0.038 (p=0.012). Worse x-rays vs constant also were statistically significant and had AOR of 23.459 (p=0.001). There was a significant moderate positive correlation between duration of hospital stay and duration from admission to medication start (SP=0.336 and p< 0.001).
Conclusion: We recommend accurately monitoring patients using x-rays to determine which patients have worse x-rays. However, the cost–benefit of using radiation must be well assessed and needs further research to determine if its benefit outweighs its risks, especially in high-risk patients. Furthermore, mechanically ventilated patients must be carefully monitored. Finally, the duration of hospital stay was highly correlated with the duration from admission to medication start. Therefore, proper treatment must be started as early as possible.
Keywords: COVID-19, mortality, elderly, ICU
Introduction
SARS-CoV-2, which is a highly infectious respiratory virus, caused a widespread pandemic of corona virus disease 2019 (COVID-19). This pandemic caused enormous human and economic losses. By December 2021, it had caused more than 266 million cases and 5 million deaths.1 In Saudi Arabia, there were more than 500,000 cases, with about 8800 deaths.2 High budget was assigned by Saudi Arabia to face the pandemic. Intensive care units were increased, hundreds of clinics were opened to make sure that anyone having COVID-19 symptoms received the needed care.3
COVID-19 symptoms range from mild to severe that require ICU transfer.4 Different symptoms such as diarrhea and vomiting are frequently caused by the virus.5 Many risk factors were identified as causing severe COVID-19 with bad prognosis, such as substance abuse, diabetes mellitus, heart diseases, renal diseases, liver diseases, cerebrovascular diseases, cancer, organ transplantation, immunosuppressive drugs, old age, pregnancy, and obesity.6
Infection with SARS-COV 2 was associated with cytokine storm development,7–10 which is an important cause for acute respiratory distress syndrome, multiple organ failure and death.11,12 In addition, viral droplet infections increase the probability of developing bacterial co-infection, causing more severe disease.13 Another risk factor for respiratory co-infections is old age and chronic diseases such as COPD.14 Co-infection with Influenza A was reported among severely ill COVID-19 cases.15
Stages of COVID-19 and the importance of starting different medication at the proper time must be well known for management to be effective. Three stages were identified: “early infection, pulmonary phase, and hyper inflammation phase”.16 The early use of some medications such as hydroxychloroquine, favipiravir and ivermectin was suggested to be effective for management of COVID-19. However, the late administration of antiviral drugs is usually ineffective.17
A previous study conducted in Saudi Arabia by Malik et al discussed the impact of COVID-19 on co-morbidities. It observed that 75% of COVID 19 patients hospitalized had at least one associated co-morbidity. The commonest co-morbidities reported were hypertension, diabetes, cancer, and cardiovascular diseases. It also reported that pre-existing polypharmacy and geriatric patients have worse complications of COVID-19.18
Currently, there are several vaccines developed showing favorable efficacy under clinical trials. Some of them were approved for use in many countries, such as Pfizer-BioNTech, Moderna, Oxford/AstraZeneca and Johnson & Johnson’s Janssen.19–21
Management plans are challenging due to limited access to intensive care units and shortage of oxygen supplies, particularly in low- or middle-income countries.22,23 Thus, we need to well understand the usual risk factors that predict mortality in COVID-19 patients to be able to early decide which patients are prioritized to have an intensive care unit.
The current study aims to find out the different predictors for mortality associated with COVID-19 among the elderly.
Methods and Patients
This study was a comparative retrospective cohort study involving 145 COVID-19 hospitalized patients whose age was more than 60 years old. It was conducted at King Faisal Medical Complex in Taif, Saudi Arabia, from June 2020 to August 2020.
Sample Size Calculation
Sample size was calculated using the website: https://www.surveysystem.com/sscalc.htm.24 The estimated sample size is 111 patients, at a confidence level of 95% and a power of 80%. To guard against drop out, the research team increased it by 20%, so the sample size is 145 patients. The estimated confidence interval is 10, the decided on minimum and maximum mortality among elderly patients.5–10
Inclusion Criteria
All elderly patients hospitalized with RT-PCR with a confirmed diagnosis of COVID-19 whose age was more than 60 years.
Exclusion Criteria
Pregnant women and patients whose age was less than 60 years old.
Study Tools
Data of patients was obtained from patients’ files and electronic information systems. Data included demographic characteristics, medical history, including symptoms and comorbidities, vital signs, laboratory investigations, and medications. The main outcome studied was COVID-19-related death.
Ethical Approval
Ethical approval was obtained from the Directorate of Health Affairs, Taif, research and studies department, and Medical Complex in Taif Research and Ethics Committee (Approval no. HAP-02-T-67).
Statistical Analysis
Data entry and analysis were done using SPSS software version 25 (IBM SPSS Statistics for Windows, version 25, IBM Corp., Armonk, N.Y., USA). Quantitative variables were summarized as mean ± standard deviation or median and 25th and 75th percentiles. Qualitative data were expressed using numbers and percentages. The test of significance used for qualitative data was Chi-square test; however, for quantitative data, it was student t-test for normally distributed data and Mann–Whitney U-test for non-normally distributed data. Spearman correlation was used to find correlation between quantitative variables. Logistic regression was used for finding out the predictors for morbidity associated with COVID-19. P-value <0.05 was considered statistically significant.
Results
Out of 145 COVID-19 patients, 11% died while about 89% survived (Figure 1).
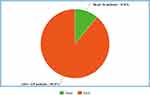 |
Figure 1 Outcome of COVID-19 patients (n=145). |
The mean age of the surviving patients was 69.3±7.5, while the mean age of the patients who died was 69.2±8.2; 12.3% of females died while 10% of males died. There was no significant difference between those who died and those who survived regarding age and gender (p=0.962 and 0.659, respectively). The mean duration of hospital stay was 23±35 days, while the median duration of hospital stay was 13 days. There was significant difference between those who died and the surviving group regarding the duration of hospital stay, with higher median duration among those who died (22 days vs 12 days, respectively, p=0.002). The median duration from admission to medication start was 3 days for those who died vs 1 day for the surviving group, with no significant difference between them (Table 1).
 |
Table 1 Demographic and Hospital Characteristics of Covid-19 Patients Who Died vs Those Alive (n=145) |
When comparing patients who died and and the surviving group regarding medical history, all diseases (such as diabetes, hypertension, ischemic heart diseases, asthma, and obesity) showed no significant differences except mental retardation, where the only COVID-19 patient who had mental retardation died (p=0.004). This mentally retarded patient was a 66-year-old male, who was transferred to ICU. He did not have any co-morbidity except for hepatitis. In addition, after stratification of patients according to the number of chronic diseases they had, no statistically significant difference was found when comparing those who died and and the surviving group using chi-square with linear trends test. However, we can notice that 30% (n=3) of patients having more than 2 chronic disease died as compared to 7% (n=2) of patients having no chronic diseases (Table 2).
 |
Table 2 Medical History of Covid-19 Patients Who Died vs Those Alive (n=145) |
Of patients transferred to ICU, 61.5% died. Moreover, 90% of patients who had mechanical ventilation also died. Only 14.5% of patients with low oxygen saturation died. In addition, only 15.5% of patients who had shortness of breath died. Of patients who did not require oxygen, 100% survived, while 6% of patients who needed oxygen-only died. About 70% of patients whose x-rays became worse died. No patient with improved x-ray died. The only patient with prolonged QT interval died. Transfer to ICU, mechanical ventilation, low oxygen saturation, shortness of breath, respiratory support, x-ray trend and prolonged QT interval showed significant statistical differences between patients who died and those who did not (p<0.001, <0.001, 0.017, 0.045, <0.001, <0.001, 0.004, respectively) (Table 3).
 |
Table 3 Symptoms, Signs and Investigations of Covid-19 Patients Who Died vs Those Alive (n=145) |
Regarding medications (such as favipiravir, hydroxychloroquine, standard of care, dexamethasone, aspirin, bronchodilators, clopidogrel, proton pump inhibitors, calcium channel blockers, statins, oseltamivir, beta-blockers, vitamin C, zinc, enoxaparin, ARPs, and diabetes medications) given to patients, all medications showed no statistically significant differences between patients who died and those who did not. Moreover, there was no significant difference between them regarding the number of medications for COVID-19, medications for chronic diseases, or medications for both COVID-19 and chronic diseases, although 13.7% of patients with polypharmacy (more than 4 drugs) died versus 6% of patients not taking any medications for either COVID-19 or chronic diseases. Furthermore, when patients stopped treatment due to adverse effects, this was not associated with death or not dying (Table 4).
 |
Table 4 Medications Given to Covid-19 Patients Who Died vs Those Alive |
Antibiotics given to patients showed no statistically significant difference between patients who died and those who did not (Table 5).
 |
Table 5 Antibiotics Given to Covid-19 Patients Who Died vs Those Alive |
After doing logistic regression of predictors for progression to death among COVID-19 patients, putting patients on oxygen only vs mechanical ventilation was statistically significant and had an adjusted odds ratio of 0.038 (p=0.012). Worse x-rays vs constant also were statistically significant and had an adjusted odds ratio of 23.459 (p=0.001) (Table 6).
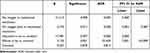 |
Table 6 Logistic Regression of Predictors for Progression to Death Among COVID-19 Patients |
There was a significant moderate positive correlation between duration of hospital stay and duration from admission to medication start (Spearman coefficient=0.336 and p<0.001). Furthermore, there was a significant strong positive correlation between duration of hospital stay and duration from medication start to discharge (Spearman coefficient=0.901 and p<0.001) (Table 7, Figures 2 and 3).
 |
Table 7 Spearman Correlation Between Duration of Hospital Stay and Other Variables Among Covid-19 Patients |
 |
Figure 2 Correlation between duration of hospital stay and duration from admission to medication start among Covid-19 patients. |
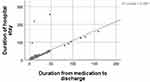 |
Figure 3 Correlation between duration of hospital stay and duration from medication to discharge among Covid-19 patients. |
Discussion
Understanding mortality predictors among COVID-19 patients (especially those who are older than 60 years) is a critical matter that should be thoroughly investigated. This is because if we predict which patients would die, we can direct them to the optimal care to prevent their death either by initiating the proper medications at the proper time or even transferring them to ICU if needed. In addition, this can save the limited number of ICU units for only those with severe disease.
In the current study, there was an association between mortality and mental retardation, transfer to ICU, mechanical ventilation, low oxygen support, shortness of breath, respiratory support, x-ray trend and prolonged QT interval. On doing logistic regression to find out mortality predictors among COVID-19 elderly patients, the need of mechanical ventilation and X-ray that is getting worse were significant predictors. There was a significant moderate positive correlation between duration of hospital stay and duration from admission to medication start.
The mortality rate in the current study was 11%. A previous meta-analysis study conducted in Saudi Arabia found a similar mortality rate of 11.5% among hospitalized COVID-19 patients after excluding critical cases. However, the total mortality rate was 17% and among critical cases was up to 40%.25
Age and gender showed no significant differences between those who died and the surviving group; however, the mean age was slightly higher among those who died. Male patients were higher than female patients; however, mortality was unexpectedly higher among females than males with no significant difference, which contradicts most literature. This is contrary to a previous study that found that males had higher mortality, higher risk of respiratory intubation and longer length of hospital stay than females.26 Another previous study conducted in Saudi Arabia reported that males outnumbered females in admission to hospitals by 2:1, with worse metabolic profile than females, although no clinical outcome differences.27 Other studies reported worse morbidity and mortality among men, establishing that male gender is a predictor for COVID-19.28–30 This can be rationalized by the fact that females have a higher immune response mostly due to estrogen, which is immune boosting, as opposed to testosterone, which is immune suppressing.31 Higher hospital admissions among Saudi males can be attributed to the higher number of Saudi male population and to being more socially mobile making them at higher risk for being infected with COVID-19.27
The mean duration of hospital stay was 23 days. This is close to the mean duration of hospital stay in a previous study in China, which was 20 days.32 However, this 3-day difference is an important matter which may be due to higher proportion of patients in our study having co-morbidities than in this previous study (81% vs 48%). The median duration from admission to medication start was 3 days for those who died vs 1 day for those in the surviving group; however, there was no significant difference between them. This could be due to the small difference between the two groups, which is just 2 days. However, we recommend starting treatment as early as possible.
Regarding co-morbidities, diabetes mellitus (DM) was the commonest disease followed by hypertension. A previous study conducted in Saudi Arabia found the same result.33 Although mortality was higher among diabetics than non-diabetics, the difference was non-significant. The American Diabetes Association mentioned that there is not enough data to suggest that DM increases the likelihood of infection with COVID-19; however, it increases the complications resulting after the infection.34 Interestingly, mortality was higher among non-hypertensive patients than hypertensive patients, which is contrary to what is found in the literature.35 However, the difference also was non-significant. The previous study conducted by Al-Ansari et al also found no significant difference between patients having DM or hypertension and those free from them.33 Also, the polypharmacy did not show any significant difference in mortality and this goes with the non-significant results we see with co-morbid conditions.
The only COVID-19 patient who had mental retardation died. This patient was a 66-year-old male, who did not have any co-morbidity except for hepatitis. Although mental retardation was significantly associated with mortality, we cannot rely on this as it is only one patient. Thus, more patients are needed. In addition, respiratory infections were found to be the leading cause for death among people with intellectual disabilities.36
About 61% of patients transferred to ICU died and there was a significant difference between them and the surviving group. This mortality rate among ICU admitted patients was similar to what was found in a previous study conducted in Saudi Arabia, which was 58% among patients whose mean age was 55 years old.37
Furthermore, 90% of patients who had mechanical ventilation also died. This is a very high mortality rate, as a previous study conducted in Brazil found mechanically ventilated patients’ mortality to be 58%.38 However, the median age of patients participating in this previous study was less than the current study (54 years vs 66 years), which may be the cause for this lower rate. Another study conducted in developing countries found total mortality of 30–44% in their populations, while it was more than 70% in low-income countries.39 In addition, many studies found age to be a predictor for mortality.40 Therefore, the reason for this high mortality among mechanically ventilated patients in the current study can be the old age of the participating patients. However, in the current study, only 14% of patients with low oxygen saturation died. Similarly, 15% of patients who had shortness of breath died. Fortunately, all patients who did not require oxygen survived.
Unfortunately, 70% of patients whose x-rays became worse died. No patient with improved x-ray died. Similarly, a study found that Brixia score, which is a new chest X-ray scoring system developed for COVID-19 pneumonia, was a predictor for in-hospital mortality.41
The only patient with prolonged QT interval died. Transfer to ICU, mechanical ventilation, low oxygen saturation, shortness of breath, respiratory support, x-ray trend and prolonged QT interval showed significant statistical differences between patients who died and those who did not.
After doing logistic regression of predictors for progression to death among COVID-19 patients, the significant predictors were putting patients on oxygen-only and worse x-rays. Putting patients on oxygen-only vs mechanical ventilation had an adjusted odds ratio of 0.038. This means that putting patients on oxygen-only rather than mechanical ventilation decreases the likelihood of mortality by 96%. Worse x-rays had an adjusted odds ratio of 23.459, which means that worse x-rays increase the likelihood of mortality 23 times more than having constant x-ray.
There was a significant moderate positive correlation between duration of hospital stay and duration from admission to medication start. However, we could not find previous studies investigating this correlation. However, we recommend starting treatment as early as possible.
Limitations of the Study
One of the study limitations is the small sample size. Also, the generalizability of the study might be limited to the population in the study.
Conclusion and Recommendations
This study aimed to investigate predictors of mortality among COVID-19 geriatric patients. We found an association between mortality and mental retardation, transfer to ICU, mechanical ventilation, low oxygen support, shortness of breath, respiratory support, x-ray trend, and prolonged QT interval. However, logistic regression found only the need for mechanical ventilation and X-ray that is getting worse to be the significant predictors. Thus, we recommend accurately monitoring patients using x-rays to determine which patients had worse x-rays than their initial x-rays when they came to the hospital. However, the cost–benefit of using radiation must be well assessed and needs further research to determine if its benefit outweighs its risks, especially in high-risk patients.
Furthermore, mechanically ventilated patients must be carefully monitored as they are at very high mortality risk. In addition, the duration of hospital stay was found to be highly correlated with the duration from admission to medication start. Therefore, proper treatment must be started as early as possible.
Institutional Review Board Statement
The study was conducted according to the guidelines of the bioethics and research committee of the King Faisal Medical Complex, Taif, Saudi Arabia, and approved by Taif Research and Ethics Committee (Approval # HAP- 02-T-67) under the reference number of (Reference Approval # HAP-02-T-67). As there is a cooperation between the Saudi Arabia ministry of higher education and the ministry of health, the research proposal was submitted to the health affair in Taif. Since the research idea was about psychiatric disease, the health affair in Taif directed the research to Mental Health Hospital in Taif.
Informed Consent Statement
This study was a comparative retrospective cohort study. At hospital admission, patients’ consents were taken to use their data with complete confidentiality. This study was compliant with the Declaration of Helsinki. Confidentiality was respected and data was not used for any other purpose.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. University JH. COVID 19 map; 2021. Available from: https://coronavirus.jhu.edu/region/saudi-arabia.
2. University JH. COVID 19 in Saudi; 2021. Available from: https://coronavirus.jhu.edu/map.html.
3. Khan A, Alsofayan Y, Alahmari A, Alowais J, Algwizani A, Alserehi H. COVID-19 in Saudi Arabia: the national health response. East Mediterr Health J. 2021;27:1114–1124. doi:10.26719/emhj.21.048
4. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
5. Wong SH, Lui RN, Sung JJ. Covid‐19 and the digestive system. J Gastroenterol Hepatol. 2020;35(5):744–748. doi:10.1111/jgh.15047
6. Allotey J, Stallings E, Bonet M, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi:10.1136/bmj.m3320
7. Henderson LA, Canna SW, Schulert GS, et al. On the Alert for cytokine storm: immunopathology in COVID −19. Arthritis Rheumatol. 2020;72:1059–1063. doi:10.1002/art.41285
8. Mahmudpour M, Roozbeh J, Keshavarz M, Farrokhi S, Nabipour I. COVID-19 cytokine storm: the anger of inflammation. Cytokine. 2020;133:155151. doi:10.1016/j.cyto.2020.155151
9. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
10. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–539. doi:10.1007/s00281-017-0629-x
11. Richards M, DeBonis K. Psychiatric training during a global pandemic: how COVID-19 has affected clinical care, teaching, and trainee well-being. Psychiatr Serv. 2020;71(12):1300–1302. doi:10.1176/appi.ps.202000277
12. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi:10.1016/S2213-2600(20)30076-X
13. Morris DE, Cleary DW, Clarke SC. Secondary bacterial infections Associated with Influenza Pandemics. Front Microbiol. 2017;8:1041. doi:10.3389/fmicb.2017.01041
14. Cox MJ, Loman N, Bogaert D, O’grady J. Co-infections: potentially lethal and unexplored in COVID-19. Lancet Microbe. 2020;1(1):e11. doi:10.1016/S2666-5247(20)30009-4
15. Hashemi SA, Safamanesh S, Ghafouri M, Taghavi MR. Co-infection with COVID-19 and influenza A virus in two died patients with acute respiratory syndrome, Bojnurd, Iran. J Med Virol. 2020;92:2319–2321. doi:10.1002/jmv.26014
16. Griffin DO, Brennan-Rieder D, Ngo B, et al. The importance of understanding the stages of COVID-19 in treatment and trials. AIDS Rev. 2021;23. doi:10.24875/AIDSRev.200001261
17. Real-time-meta-analysis. COVID-19 early treatment: real-time analysis of 749 studies: unknown; 2021Available from: https://c19early.com/.
18. Ahmad Malik J, Ahmed S, Shinde M, et al. The impact of COVID-19 on comorbidities: a review of recent updates for combating it. Saudi J Biol Sci. 2022;29(5):3586–3599. PMID: 35165505; PMCID: PMC8828435. doi:10.1016/j.sjbs.2022.02.006
19. Yan Y, Pang Y, Lyu Z, et al. The COVID-19 vaccines: recent development, challenges and prospects. Vaccines. 2021;9(4):349. doi:10.3390/vaccines9040349
20. Montastruc J-L, Lafaurie M, de Canecaude C, et al. COVID-19 vaccines: a perspective from social pharmacology. Therapies. 2021;76:311–315. doi:10.1016/j.therap.2021.05.010
21. Food, Administration D. COVID-19 vaccines authorized for emergency use; 2021.
22. Salluh JI, Lisboa T, Bozza FA. Challenges for the care delivery for critically ill COVID-19 patients in developing countries: the Brazilian perspective. Crit Care. 2020;24(1):1–3. doi:10.1186/s13054-020-03278-7
23. Cénat JM. The vulnerability of low-and middle-income countries facing the COVID-19 pandemic: the case of Haiti. Travel Med Infect Dis. 2020;37:101684. doi:10.1016/j.tmaid.2020.101684
24. Available from: https://www.surveysystem.com/sscalc.htm.
25. Macedo A, Gonçalves N, Febra C. COVID-19 fatality rates in hospitalized patients: systematic review and meta-analysis. Ann Epidemiol. 2021;57:14–21. doi:10.1016/j.annepidem.2021.02.012
26. Nguyen NT, Chinn J, De Ferrante M, Kirby KA, Hohmann SF, Amin A. Male gender is a predictor of higher mortality in hospitalized adults with COVID-19. PLoS One. 2021;16(7):e0254066. doi:10.1371/journal.pone.0254066
27. Alguwaihes AM, Al-Sofiani ME, Megdad M, et al. Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a single-centre retrospective study. Cardiovasc Diabetol. 2020;19:205. doi:10.1186/s12933-020-01184-4
28. Jin JM, Bai P, He W, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi:10.3389/fpubh.2020.00152
29. Galbadage T, Peterson BM, Awada J, et al. Systematic review and meta-analysis of sex-specific COVID-19 clinical outcomes. Front Med. 2020;7:348. doi:10.3389/fmed.2020.00348
30. Strope JD, Chau CH, Figg WD. Are sex discordant outcomes in COVID-19 related to sex hormones? Semin Oncol. 2020;S0093–7754(20):30062. doi:10.1053/j.seminoncol.2020.06.002
31. Ortona E, Pierdominici M, Rider V. Editorial: sex hormones and gender differences in immune responses. Front Immunol. 2019;10:1076. doi:10.3389/fimmu.2019.01076
32. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. PMID: 32171076; PMCID: PMC7270627. doi:10.1016/S0140-6736(20)30566-3
33. Al-Ansari RY, Alshaer A, Al-Anazi A, et al. ABO in correlation to the requirement of mechanical ventilation and mortality in critically Ill patients with COVID-19. J Hematol. 2021;10(2):64–70. doi:10.14740/jh821
34. American Dental Association. How coronavirus impacts people with diabetes; 2021. Available from: https://www.diabetes.org/coronavirus-covid-19/how-coronavirus-impacts-people-with-diabetes.
35. Mubarik S, Liu X, Eshak ES, et al. The Association of Hypertension With the Severity of and Mortality From the COVID-19 in the Early Stage of the Epidemic in Wuhan, China: a Multicenter Retrospective Cohort Study. Front Med. 2021;8:631.
36. O’Leary L, Hughes-McCormack L, Dunn K, Cooper SA. Early death and causes of death of people with down syndrome: a systematic review. J Appl Res Intellect Disabil. 2018;31(5):687–708. doi:10.1111/jar.12446
37. Al Mutair A, Al Mutairi A, Zaidi ARZ, et al. Clinical predictors of COVID-19 mortality among patients in intensive care units: a retrospective study. Int J Gen Med. 2021;14:3719–3728. doi:10.2147/IJGM.S313757
38. Kurtz P, Bastos LSL, Dantas LF, et al. Evolving changes in mortality of 13,301 critically ill adult patients with COVID-19 over 8 months. Intensive Care Med. 2021;47(5):538–548. doi:10.1007/s00134-021-06388-0
39. Borghesi A, Zigliani A, Golemi S, et al. Chest X-ray severity index as a predictor of in-hospital mortality in coronavirus disease 2019: a study of 302 patients from Italy. Int J Infect Dis. 2020;96:291–293. doi:10.1016/j.ijid.2020.05.021
40. Chiwhane A, Diwan S. Characteristics, outcome of patients on invasive mechanical ventilation: a single center experience from central India. J Crit Care Med. 2016;4(3):113–118. doi:10.1016/j.ejccm.2016.10.003
41. Schönhofer B, Euteneuer S, Nava S, Suchi S, Köhler D. Survival of mechanically ventilated patients admitted to a specialised weaning centre. Intensive Care Med. 2002;28(7):908–916. PMID: 12122529. doi:10.1007/s00134-002-1287-5
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
