Back to Journals » Journal of Pain Research » Volume 16
Methylnaltrexone Treatment for Opioid-Induced Constipation in Patients with and without Cancer: Effect of Initial Dose
Authors Chamberlain BH, Rhiner M, Slatkin NE, Stambler N , Israel RJ
Received 8 February 2023
Accepted for publication 9 July 2023
Published 27 July 2023 Volume 2023:16 Pages 2595—2607
DOI https://doi.org/10.2147/JPR.S405825
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amitabh Gulati
Bruce H Chamberlain,1 Michelle Rhiner,2 Neal E Slatkin,3,4 Nancy Stambler,5 Robert J Israel6
1Genesis Healthcare, Davenport, IA, USA; 2Department of Family Medicine, Loma Linda University Health, Loma Linda, CA, USA; 3University of California Riverside, School of Medicine, Riverside, CA, USA; 4Salix Pharmaceuticals, Medical Affairs, Bridgewater, NJ, USA; 5Progenics Pharmaceuticals, Inc, a subsidiary of Lantheus Holdings, Inc, Clinical Research, North Billerica, MA, USA; 6Bausch Health US, LLC, Clinical and Medical Affairs, Bridgewater, NJ, USA
Correspondence: Robert J Israel, Bausch Health US, LLC, Clinical and Medical Affairs, 400 Somerset Corporate Boulevard, Room 6-1001, Bridgewater, NJ, 08807, USA, Tel +1 908 541-2288, Fax +1 585 338-0668, Email [email protected]
Purpose: Opioid-induced constipation (OIC) is a common side effect of opioid therapy. Methylnaltrexone (MNTX) is a selective, peripherally acting μ-opioid receptor antagonist, with demonstrated efficacy in treating OIC. We pooled results from MNTX clinical trials to compare responses to an initial dose in patients with chronic cancer and noncancer pain.
Patients and Methods: This post hoc analysis used pooled data from 3 randomized, placebo-controlled studies of MNTX in patients with advanced illness with OIC. Assessments included the proportions of patients achieving rescue-free laxation (RFL) within 4 and 24 hours of the first study drug dose, time to RFL, current and worst pain intensity, and adverse events, stratified by the presence/absence of cancer.
Results: A total of 355 patients with cancer (MNTX n = 198, placebo n = 157) and 163 without active cancer (MNTX n = 83; placebo n = 80) were included. More patients treated with MNTX compared with those who received placebo achieved an RFL within 4 (cancer: MNTX, 61.1% vs placebo,15.3%, p< 0.0001; noncancer: MNTX, 62.2% vs placebo, 17.5%, p< 0.0001) and 24 hours (cancer: MNTX, 71.2% vs placebo, 41.4%, p< 0.0001; noncancer: MNTX, 74.4% vs placebo, 37.5%, p< 0.0001) of the initial dose. Cumulative RFL response rates within 4 hours of the first, second, or third dose of study drug were also higher in MNTX-treated patients. The estimated time to RFL was shorter among those who received MNTX and similar in cancer and noncancer patients. Mean pain scores declined similarly in all groups. The most common adverse events in both cancer and noncancer patients were abdominal pain, flatulence, and nausea.
Conclusion: After the first dose, MNTX rapidly induced a laxation response in the majority of both cancer and noncancer patients with advanced illness. Opioid-induced analgesia was not compromised, and adverse events were primarily gastrointestinal in nature. Methylnaltrexone is a well-tolerated and effective treatment for OIC in both cancer and noncancer patients.
Keywords: peripheral mu-opioid receptor antagonist, PAMORA, chronic pain, opioid
Introduction
Opioid-induced constipation (OIC) is a common side effect of opioid therapy for cancer or noncancer pain, particularly in patients with advanced illness. For many patients, OIC is one of the most common and bothersome side effects arising from opioid treatment.1–4 Although many side effects of opioid therapy improve or disappear with long-term use, OIC typically persists throughout opioid treatment, despite laxative use.5,6 Traditional laxatives and/or stool softeners provide limited effectiveness for OIC, because they do not counteract the underlying mechanism of OIC, the attachment of therapeutic opioids to peripheral µ-opioid receptors in the gastrointestinal (GI) tract.6,7 Consequently, patients may discontinue opioids or reduce dosing, compromising the effectiveness of pain management.1,5
There are several potential impacts of opioids in patients with advanced illness and chronic pain. Adverse events such as OIC occur when therapeutic opioid agonists bind to peripheral μ-opioid receptors in the GI tract, which leads to reduced GI motility, inhibited peristalsis, and prolonged transit time.6,8 However, constipation in patients with cancer or noncancer pain may have root causes other than opioid use alone (eg, physiologic dysfunction, concomitant medications, dehydration, immobility, diet, or metabolic causes, among several other factors9). In addition, activation of the µ-opioid receptor may promote cancer progression, opioid use is associated with shorter overall survival in cancer patients,10–12 and constipation itself has been identified as an adverse factor for survival in cancer patients.13,14 These additional lines of evidence suggest that responses to μ-receptor antagonists, such as methylnaltrexone, may differ based on cancer status and support the importance of determining if OIC treatments that target the µ-opioid receptor are equally effective in patients with or without cancer.
Methylnaltrexone (MNTX; Relistor®, Salix Pharmaceuticals, a division of Bausch Health US, LLC, Bridgewater, NJ, USA), a selective, peripherally acting μ-opioid receptor antagonist (PAMORA) restricted from crossing the blood–brain barrier (BBB), decreases OIC without attenuating opioid analgesia.15–18 MNTX tablets and subcutaneous (SC) injections are approved for the treatment of OIC in adults with chronic noncancer pain, including patients with chronic pain related to prior cancer or its treatment who do not require frequent (eg, weekly) opioid dosage escalation.15 In addition, MNTX injection is the only PAMORA19 indicated for the treatment of OIC in adults with advanced illness or pain caused by active cancer who require opioid dosage escalation for palliative care.15
We present a post hoc analysis of pooled results from 3 randomized, placebo-controlled trials of MNTX treatment for patients with advanced illness and OIC. The primary objective of the analysis was to investigate potential differences in MNTX efficacy following initial dosing in patients with or without active cancer who were receiving opioid therapy for pain, most of whom had not responded adequately to conventional laxatives. This analysis also aimed to assess the safety of MNTX as measured by adverse events, changes in pain scores, and opioid withdrawal symptoms.
Methods
Study Design
This was a post hoc analysis of pooled data from 3 multicenter, double-blind, randomized, placebo-controlled clinical trials conducted in adult patients with advanced illness and OIC. Detailed descriptions of the methods used in studies 301 (ClinicalTrials.gov identifier NCT00401362), 302 (NCT00402038), and 4000 (NCT00672477) have been published previously.16,17,20 In all 3 studies, patients who completed the double-blind phase were eligible to enroll in an open-label extension phase in which all patients received MNTX. All studies included in this pooled analysis were conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and principles of Good Clinical Practice. All patients provided written informed consent.
Study Population
Eligible patients included men and women aged ≥18 years with a diagnosis of advanced illness (ie, terminal diseases such as incurable cancer and end-stage organ/system disorders) with a life expectancy of ≥1 month (studies 302 and 4000) or 1 to 6 months (study 301). Patients were receiving opioids routinely for discomfort or pain management for ≥3 days (study 301) or ≥2 weeks (studies 302 and 4000), excluding as needed or rescue doses, and taking a stable opioid regimen for ≥3 days before receiving the first dose of study medication. A stable regimen was defined as one with no reduction of opioid dose ≥50% within 3 days prior to study drug initiation. Enrolled patients had OIC, defined as <3 bowel movements (BM) during the previous week,21 and no clinically significant laxation during the 24 hours preceding the first dose of study drug (studies 302 and 4000) or as no clinically significant laxation during the 48 hours preceding the first dose of study drug (study 301). For patients taking laxatives (eg, stool softener and senna or equivalent), the regimen was stable for ≥3 days prior to study drug initiation.
Potential patients were excluded if they had a history of MNTX treatment (for study 4000 only, patients were excluded if they had MNTX treatment at any time during the 7 days before the first dose of the study drug), any disease process suggesting the presence of a GI obstruction, evidence of fecal impaction, a history of fecal ostomy, or any potential nonopioid cause of bowel dysfunction, which in the opinion of the investigator, might have been primarily responsible for constipation.
Treatments
In study 301, patients were randomized in a 1:1:1 ratio to receive a single SC injection of MNTX 0.15 mg/kg, MNTX 0.30 mg/kg, or placebo. In study 302, patients were randomized to receive SC injections of MNTX 0.15 mg/kg or placebo every other day for 2 weeks; dose escalation to 0.30 mg/kg was allowed after study day 9 for patients who had <3 BM not associated with rescue medication or intervention. In study 4000, MNTX dosage was determined by weight. Patients were randomized to receive SC injections of 8 mg (subjects weighing ≥38 to <62 kg; ~0.13 to 0.21 mg/kg) or 12 mg (subjects weighing ≥62 kg; ≤0.19 mg/kg) MNTX or matching placebo every other day for a maximum of 7 doses.
Study Assessments
Efficacy assessments included the percentage of patients who achieved a rescue-free laxation (RFL, defined as laxation without use of other laxative, enema, or suppository) within 4 and 24 hours of the first dose (studies 301, 302, and 4000), the cumulative percentages of patients who achieved RFL within 4 hours of the first, second, and third doses (studies 302 and 4000), and time to RFL. Cumulative RFL rates were reported among pooled patients from studies 302 and 4000 only because patients in study 301 only received one dose of double-blind study treatment.
Changes from baseline in pain scores (including both current pain and worst pain) were assessed using an 11-point rating scale of 0 (no pain) to 10 (worst pain imaginable) to evaluate possible effects of treatment on opioid analgesia. Pain scores were assessed 4 hours after initial study drug administration.
Safety assessments included tabulation of treatment-emergent adverse events (TEAEs).
Statistical Analysis
Efficacy analyses were performed on the intent-to-treat (ITT) population, defined as all subjects who received at least 1 dose of study medication. For comparison purposes in the current post hoc analysis, pooled patient and outcome data from the 3 studies were stratified by patient cancer status (active cancer or noncancer). Safety analyses were performed on the pooled safety outcome data from the 3 studies involving the safety population, defined as all patients who received at least 1 dose of study medication. As with efficacy analyses, safety outcome data were stratified by patient cancer status.
Pooled patient demographics and baseline characteristics were analyzed by patient cancer status (cancer vs noncancer) and treatment group, and reported using summary statistics (N, mean, median, SD, minimum and maximum values). Response rates for patients achieving RFL within 4 and 24 hours and cumulative response rates 4 hours after the first, second, and third doses were compared by treatment group in cancer and noncancer patients using chi-square tests, and p-values were generated. Time to RFL was analyzed and plotted using Kaplan–Meier methods. Change from baseline in pain scores 4 hours after the first study medication dose was calculated; the MNTX group was compared with the placebo group using unpaired t-tests. Summary statistics were used to describe TEAEs by treatment group and disease state. The nominal level of significance was set at p<0.05, with no adjustments for multiplicity. All analyses were conducted using SAS® Version 9.4.
Results
Study Population
The pooled ITT population from the 3 studies included 518 randomized patients, 355 with cancer (MNTX n = 198, placebo n = 157) and 163 without active cancer (MNTX n = 83; placebo n = 80). A summary of patient demographics and baseline characteristics, stratified by the presence/absence of cancer and by treatment group, is shown in Table 1. Although the cancer and noncancer groups were similar with respect to current and worst pain scores and use of laxatives, the median morphine equivalent opioid dose at baseline was substantially lower for patients without cancer versus patients with cancer both for those who received MNTX (noncancer: 120 mg/d; cancer: 190 mg/d; p=0.3041) and those who received placebo (noncancer: 80 mg/d; cancer: 200 mg/d; p=0.0067).
 |
Table 1 Study Population Demographics and Baseline Characteristics, Stratified by Presence or Absence of Cancer (ITT Population) |
Rescue-Free Laxation at 4 and 24 Hours
As shown in Figure 1, significantly greater proportions of cancer and noncancer patients treated with MNTX had RFL within 4 and 24 hours compared with placebo after the initial drug dose (p<0.0001 for all MNTX-to-placebo comparisons). Overall, RFL was achieved in 61.1% and 62.2% of cancer and noncancer patients, respectively, within 4 hours after the first dose of MNTX compared with 15.3% and 17.5% of cancer and noncancer patients, respectively, who received placebo. This effect was sustained at 24 hours after the first dose with 71.2% and 74.4% of cancer and noncancer patients, respectively, who received MNTX reporting RFL compared with 41.4% and 37.5% of cancer and noncancer patients, respectively, who received placebo.
Cumulative Rescue-Free Laxation Response Rate
When cumulative response rates were considered, significantly greater proportions of MNTX-treated patients achieved RFL within 4 hours after the first dose (Figure 2A), after the first or second doses (Figure 2B), and within 4 hours after the first, second, or third doses (Figure 2C) compared with patients who received placebo.
Time to First Rescue-Free Laxation
The temporal patterns of estimated time to RFL response were similar between cancer and noncancer patients treated with MNTX, as most patients had responded by the 2-hour time point (Figure 3). The estimated time to RFL was much longer in both cancer and noncancer patients who received placebo.
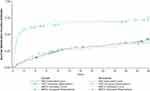 |
Figure 3 Kaplan–Meier analysis of time to rescue-free laxation among cancer and noncancer patients within 24 hours of initial dose of study drug. Abbreviations: MNTX, methylnaltrexone; PBO, placebo. |
Change from Baseline in Pain Scores
There were no significant differences between treatment groups in change from baseline in mean current and worst pain scores at the initial pain assessment 4 hours after the first study medication dose (Figure 4). Mean pain scores decreased slightly in all patient groups regardless of cancer status or treatment.
Safety
Among cancer patients in the safety population pooled from the 3 studies who received MNTX or placebo, TEAEs reported by more than 10% of patients were primarily GI in nature, including abdominal pain, flatulence, and nausea (Table 2). A similar pattern of TEAEs was observed among noncancer patients in the safety population. Abdominal pain, a common symptom associated with laxation, was the most frequently reported TEAE in the MNTX group and was more frequently reported in patients who received MNTX (36.4% and 25.3% in the cancer and noncancer cohorts, respectively) compared with the placebo group (14.0% and 16.3% in the noncancer cohorts, respectively).
 |
Table 2 Proportion of Patients Reporting a TEAE Occurring in >10% in Any of the Study Groups (Safety Populationa) |
Discussion
In this analysis of pooled results from 3 randomized, placebo-controlled clinical trials, MNTX produced RFL in more than 60% of patients with advanced illness with OIC within 4 hours of a single SC administration while less than 20% of patients who received placebo achieved RFL in the same timeframe. The difference in first-dose effects between treatment groups was sustained at 24 hours with >70% of patients who received MNTX reporting RFL compared with approximately 40% of patients who received placebo. These differences were also maintained over the first few doses, with significantly greater cumulative proportions of MNTX-treated patients achieving RFL within 24 hours of the first, second, and third doses compared with patients who received placebo. Response rates were similar between cancer and noncancer patients, despite substantially greater mean daily opioid use among cancer patients. It is still unclear how variables such as opioid dose, cancer status, or presence of advanced illness affect response to MNTX, and further analyses evaluating this are ongoing. Mean pain scores did not show any clinically relevant changes and were similar between treatment groups, indicating that central opioid analgesia was not compromised with MNTX treatment. This effect did not differ between cancer and noncancer patients.
Time-to-event analyses showed that the estimated temporal pattern of RFL response following single-dose administration of MNTX was nearly identical in cancer and noncancer patients with most responding patients experiencing an RFL within 2 hours, regardless of the presence or absence of cancer. This finding complements previous analyses22 of MNTX in the treatment of OIC and highlights the speed of response in a severely ill patient population.
Analyses investigating the time to onset of OIC relief after treatment with the PAMORA naldemedine (Symproic, Shionogi, Inc., Florham Park, NJ, USA) have also been conducted in patients with and without cancer in the Phase 3 COMPOSE-1, −2, and −4 trials.23,24 Treatment with naldemedine resulted in significantly shorter times to first spontaneous bowel movement (SBM) versus placebo in all 3 trials; the median times to first SBM were 16.1 hours and 18.3 hours in COMPOSE-1 and COMPOSE-2, respectively, and 4.7 hours in COMPOSE-4.23,24 Naloxegol (Movantik, RedHill Biopharma Inc., Raleigh, NC, USA) is another orally administered PAMORA approved for the treatment of OIC in adult patients with chronic noncancer pain.25 Time to first postdose SBM in patients with noncancer pain and OIC was assessed in 2 placebo-controlled, double-blind, 12-week studies, KODIAC-4 and KODIAC-5. In KODIAC-4, the median time to first postdose SBM was 5.9 and 20.4 hours with naloxegol 25 mg and 12.5 mg, respectively; in KODIAC-5, the median time to first SBM was 12.0 and 19.3 hours with naloxegol 25 mg and 12.5 mg, respectively.26 In contrast, the estimated time to RFL in the current analysis of MNTX in patients with and without cancer was <2 hours. The SC administration of MNTX in the current analysis likely explains the faster response observed with MNTX.27 SC formulations may be particularly useful in patients with advanced disease, who may not be able to take orally administered medicines and who require management of complex symptoms with frequent administration of medications.28 As such, the rapid response we observed with MNTX would seem very useful clinically.29 There do not appear to be additional safety risks associated with SC administration either; the most common TEAEs in this study were abdominal pain, nausea, and flatulence, consistent with studies on naldemedine and naloxegol.23,26 It is also worth noting that the baseline mean daily dose of oral opioid morphine equivalents in naldemedine-treated cancer patients in COMPOSE-4 was substantially lower than the baseline median daily dose of opioid morphine equivalents received by MNTX-treated cancer patients in the current study (57.3 mg vs 190 mg);24 mean baseline daily doses of opioid morphine equivalents in noncancer patients receiving active treatment in COMPOSE-1 and COMPOSE-2 were comparable to median baseline doses in the current study (125.2 mg, 118.0 mg, and 120 mg, respectively).23 Additionally, patients in the current analysis had advanced illness, whereas patients in the COMPOSE and KODIAC trials did not.24,26,30 While differences in study designs, patient characteristics, and assessment methods need to be taken into account when comparing the results of these trials, the data suggest that treatment with SC MNTX may result in a shorter time to relief of OIC in both patients with and without cancer.
There was no evidence that the efficacy of opioid analgesia was compromised by MNTX treatment as mean pain scores declined slightly among all cohorts, including MNTX-treated cancer and noncancer patients. The absence of any negative effects of MNTX treatment on opioid analgesia in cancer patients is particularly important. Opioid and opioid antagonist effects on the central nervous system (CNS) may be dependent upon an intact BBB, which is responsible for reducing brain permeability and solidifying connections between vascular endothelial cells.31–33 Because of its large structure and low lipid solubility, MNTX is restricted from crossing the BBB and is unable to interfere with opioid-mediated CNS analgesic effects in patients with intact BBBs. As opioid medications have been a cornerstone of cancer pain treatment for several decades34 and one of the most common side effects of opioid treatment is constipation,35 it is reassuring that this analysis provides no evidence that MNTX penetrates the BBB in such patients. Additional analyses of MNTX in cancer patients with brain metastases showed no differences from placebo in posttreatment changes in pain score or adverse events after the first does of MNTX, further supporting the safety and efficacy of MNTX in cancer patients with OIC.36
Considering this is a post hoc analysis of previously published studies, there are several limitations that deserve discussion. The data for this analysis were pooled from 3 distinct, although similarly designed studies. Subtle differences in dosing regimen, patient populations, and study durations, for example, may confound the results of the pooled data. It should also be noted that this population included patients with advanced illnesses who may have had comorbidities and several concomitant medications that may have contributed to the complexity of their diseases and safety outcomes. Although the majority of the TEAEs reported were GI-related, it is unclear if they are directly related to MNTX. In particular, one study of MNTX showed that abdominal pain is commonly reported among patients with OIC who are RFL responders, indicating that abdominal pain may be a consequence of efficacy (ie, laxation) rather than a side effect.37
Conclusions
When administered to severely ill OIC patients receiving chronic opioid therapy with an inadequate response to conventional laxatives, a single dose of MNTX produced RFL responses in significantly greater proportions of cancer and noncancer patients than placebo. Additionally, treatment with MNTX produced RFL response in more than 60% of patients within 4 hours and more than 70% within 24 hours. Response rates and the timing of laxation responses were similar in patients with and without cancer, and there was no evidence, based on predose and postdose pain evaluations, that MNTX treatment interfered with the efficacy of opioid analgesia. These results demonstrate that MNTX provides effective, safe, and rapid relief of OIC symptoms without compromising opioid analgesia in both cancer and noncancer patients.
Abbreviations
BBB, blood–brain barrier; BM, bowel movements; CNS, central nervous system; GI, gastrointestinal; ITT, intent to treat; MNTX, methylnaltrexone; N/A, not available; OIC, opioid-induced constipation; PAMORA, peripherally acting μ-opioid receptor antagonist; PBO, placebo; RFL, rescue-free laxation; SBM, spontaneous bowel movement; SC, subcutaneous; SD, standard deviation; TEAE, treatment-emergent adverse event.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available at this time due to the proprietary nature of this information. Requests for additional information should be made to the corresponding author.
Ethics Approval and Informed Consent
Patients or their legally acceptable representative provided written informed consent to participate before any study-specific procedures were conducted. The specific ethical review boards that provided approval and oversight are listed below for each study.
Study 301
Human Investigative Committee, University of Virginia Health System, Charlottesville, Virginia, USA
University of Wisconsin Health Sciences IRB, VA Medical Center, Madison, Wisconsin, USA
Stanford University Institutional Review Board, Stanford University, Palo Alto, California, USA
University of Utah IRB, University of Utah Health Sciences Center, Salt Lake City, Utah, USA
Schulman Associates Institutional Review Board, Cincinnati, Ohio, USA
Beth Israel Medical Center Institutional Review Board, Beth Israel Medical Center, New York, New York, USA
University of Alabama at Birmingham IRB, University of Alabama at Birmingham, Alabama, USA
City of Hope IRB, City of Hope, Duarte, California, USA
San Diego Hospice IRB, San Diego Hospice, San Diego, California, USA
The University of Texas IRB, M.D. Anderson Cancer Center, Houston, Texas, USA
Hospice of North Central Florida IRB, Hospice of North Central Florida, Gainesville, Florida, USA
Geisinger IRB, Geisinger, Danville, Pennsylvania, USA
Humility of Mary Health Partners IRB, Humility of Mary Health Partners, Youngstown, Ohio, USA
Study 302
Schulman Associates Institutional Review Board, Cincinnati, Ohio, USA
Research Ethics Board, McGill University Health Centre, Montreal, Quebec, Canada
University of British Columbia, British Columbia Cancer Agency Research Ethics Board, Vancouver, British Columbia, Canada
San Diego Hospice IRB, San Diego Hospice, San Diego, California, USA
University of Utah Institutional Review Board, University of Utah Health Sciences Center, Salt Lake City, Utah, USA
Henry Ford Health System Institutional Review Board, Henry Ford Health System, Detroit, Michigan, USA
Human Subjects Protection Office, The Penn State University/Milton S Hershey Medical Center, Hershey, Pennsylvania
City of Hope IRB, City of Hope, Duarte, California, USA
Study 4000
Schulman Associates Institutional Review Board, Cincinnati, Ohio, USA
The University of Texas IRB, M.D. Anderson Cancer Center, Houston, Texas, USA
Division of Research Integrity & Compliance, Moffitt Cancer Center, Tampa, Florida, USA
Fox Chase Cancer Centre Institutional Review Board, Fox Chase Cancer Centre, Rockledge, Pennsylvania, USA
Regonala Etikprövningsnämnden i Linköping, Palliative Unit Vrinnevi Hospital, Linköping, Sweden
Ethics Committee CEIC. CSUB Ciutat Sanitaria Universitaria Bellvitge, Spain
Bellberry Limited, Dulwich, South Australia, Australia
Azienda Sanitaria Locale di Asti - ASL AT Sede, Asti, Italy
Comitato Etico Dell`Azienda Ospedaliera Guido Salvini di Garbagnate Milanese, Milan, Italy
Comitato Etico Indipendente Della Fondazione IRCCS Istituto Nazionale dei Tumori di Milano, Milan, Italy
St Vincent’s Hospital Human Research Ethics Committee (HREC), St Vincent’s Hospital, Darlinghurst, New South Wales, Australia
Ethik-Kommission an der Medizinischen Fakultät Technischen Hochschule Aachen, University of Aachen, Aachen, Germany
Ethik-Kommission bei der Medizinischen Fakultät der Ludwig-Maximilians Universität München, Munich, Germany
The Peter Mac Ethics Committee, Peter MacCallum Cancer Center, East Melbourne, Victoria, Australia
CIUSSS Research Ethics Board, The Jewish General Hospital, Montreal, Quebec, Canada
Bannatyne Campus Research Ethics Board, University of Manitoba, Winnipeg, Manitoba, Canada
Ethics Committee Research Leuven, UZ Leuven, Leuven, Belgium
Comité de Protection des Personnes – Sud Est V, Centre Hospitalier Universitaire de Grenoble, Grenoble, France
Hamilton Health Sciences, Hamilton, Ontario, Canada
London – Central MREC, London, United Kingdom
CHUQ Research Ethics Committee, Centre Hospitalier Universitaire de Quebec, Quebec City, Quebec, Canada
Western Institutional Review Board, Olympia, Washington, USA
Comitê de ética em Pesquisa em seres Humanos da Fundação Antônio Prudente, A.C. Camargo Cancer Center, São Paulo, Brazil
University of Utah Institutional Review Board, University of Utah Health Sciences Center, Salt Lake City, Utah, USA
Alberta Cancer Research Ethics Committee, University of Alberta, Edmonton, Alberta, Canada
Comité Bioético para la Investigación Clínica, Mexico City, Mexico
VA New Jersey Healthcare System Institutional Review Board, VA New Jersey Healthcare System, East Orange, New Jersey, USA
Previous Presentations
Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association; March 13–16, 2019; Orlando, Florida.
Society of Hospital Medicine 2019; March 24–27, 2019; National Harbor, Maryland.
PAINWeek 2019; September 3–7, 2019; Las Vegas, Nevada.
Annual National Conference of the American Society for Pain Management Nursing; September 18–21, 2019; Portland, Oregon.
Funding
This study was supported by Salix Pharmaceuticals, a division of Bausch Health US, LLC, Bridgewater, NJ, USA, which has licensed the rights to develop and commercialize Relistor® from Progenics Pharmaceuticals, Inc., a wholly owned subsidiary of Lantheus Holdings, Inc., North Billerica, MA. Progenics Pharmaceuticals had a role in the study design, implementation of the study, and data collection. Salix had a role in the data collection, data analysis, and the decision to publish. Technical editorial and medical writing assistance was provided under the direction of the authors by Drayton Hammond, PharmD, Echelon Brand Communications, LLC, an OPEN Health company, Parsippany, NJ, USA. Funding for this support was provided by Salix Pharmaceuticals.
Disclosure
Dr Chamberlain has nothing to disclose. Dr Rhiner received funding from Wyeth Pharmaceuticals for the methylnaltrexone studies 301 and 302 referenced in this paper and reports grants from City of Hope, during the conduct of the study. Dr Slatkin is an employee of Salix Pharmaceuticals, a division of Bausch Health, US, LLC. Dr Stambler is a full-time employee of Progenics Pharmaceuticals, Inc., a subsidiary of Lantheus Holdings, Inc., and a shareholder of Lantheus Holdings, Inc. Dr Israel is an employee of Bausch Health US, LLC.
References
1. Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European patient survey (PROBE 1). Pain Med. 2009;10(1):35–42. doi:10.1111/j.1526-4637.2008.00495.x
2. Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S. Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain. 2001;93(3):247–257. doi:10.1016/S0304-3959(01)00324-4
3. Panchal SJ, Muller-Schwefe P, Wurzelmann JI. Opioid-induced bowel dysfunction: prevalence, pathophysiology and burden. Int J Clin Pract. 2007;61(7):1181–1187. doi:10.1111/j.1742-1241.2007.01415.x
4. Weschules DJ, Bain KT, Reifsnyder J, et al. Toward evidence-based prescribing at end of life: a comparative analysis of sustained-release morphine, oxycodone, and transdermal fentanyl, with pain, constipation, and caregiver interaction outcomes in hospice patients. Pain Med. 2006;7(4):320–329. doi:10.1111/j.1526-4637.2006.00184.x
5. Coyne KS, Margolis MK, Yeomans K, et al. Opioid-induced constipation among patients with chronic noncancer pain in the United States, Canada, Germany, and the United Kingdom: laxative use, response, and symptom burden over time. Pain Med. 2015;16(8):1551–1565. doi:10.1111/pme.12724.
6. Kumar L, Barker C, Emmanuel A. Opioid-induced constipation: pathophysiology, clinical consequences, and management. Gastroenterol Res Pract. 2014. doi:10.1155/2014/141737
7. Nelson AD, Camilleri M. Chronic opioid induced constipation in patients with nonmalignant pain: challenges and opportunities. Therap Adv Gastroenterol. 2015;8(4):206–220. doi:10.1177/1756283X15578608.
8. Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working group consensus statement on opioid-induced constipation. Neurogastroenterol Motil. 2014;26(10):1386–1395. doi:10.1111/nmo.12417.
9. Wickham RJ. Managing constipation in adults with cancer. J Adv Pract Oncol. 2017;8(2):149–161.
10. Lennon FE, Mirzapoiazova T, Mambetsariev B, et al. The mu opioid receptor promotes opioid and growth factor-induced proliferation, migration and epithelial mesenchymal transition (EMT) in human lung cancer. PLoS One. 2014;9(3):e91577. doi:10.1371/journal.pone.0091577.
11. Singleton PA, Moss J, Karp DD, Atkins JT, Janku F. The mu opioid receptor: a new target for cancer therapy? Cancer. 2015;121(16):2681–2688. doi:10.1002/cncr.29460.
12. Zylla D, Steele G, Shapiro A, Richter S, Gupta P. Impact of opioid use on health care utilization and survival in patients with newly diagnosed stage IV malignancies. Support Care Cancer. 2018;26(7):2259–2266. doi:10.1007/s00520-018-4062-z.
13. Lee YJ, Suh SY, Choi YS, et al. EORTC QLQ-C15-PAL quality of life score as a prognostic indicator of survival in patients with far advanced cancer. Support Care Cancer. 2014;22(7):1941–1948. doi:10.1007/s00520-014-2173-8.
14. Brown J, Thorpe H, Napp V, et al. Assessment of quality of life in the supportive care setting of the big lung trial in non-small-cell lung cancer. J Clin Oncol. 2005;23(30):7417–7427. doi:10.1200/JCO.2005.09.158.
15. Salix Pharmaceuticals. Relistor [Package Insert]. Bridgewater, NJ: Salix Pharmaceuticals; 2020.
16. Slatkin N, Thomas J, Lipman AG, et al. Methylnaltrexone for treatment of opioid-induced constipation in advanced illness patients. J Support Oncol. 2009;7(1):39–46.
17. Thomas J, Karver S, Cooney GA, et al. Methylnaltrexone for opioid-induced constipation in advanced illness. N Engl J Med. 2008;358(22):2332–2343. doi:10.1056/NEJMoa0707377.
18. Yuan CS, Foss JF, O’Connor M, Toledano A, Roizen MF, Moss J. Methylnaltrexone prevents morphine-induced delay in oral-cecal transit time without affecting analgesia: a double-blind randomized placebo-controlled trial. Clin Pharmacol Ther. 1996;59(4):469–475. doi:10.1016/S0009-9236(96)90117-4.
19. Chamberlain BH, Rhiner M, Slatkin NE, Stambler N, Israel RJ. Subcutaneous methylnaltrexone for treatment of opioid-induced constipation in cancer versus noncancer patients: an analysis of efficacy and safety variables from two studies. J Pain Res. 2021;14:2687–2697. doi:10.2147/JPR.S312731.
20. Bull J, Wellman CV, Israel RJ, Barrett AC, Paterson C, Forbes WP. Fixed-dose subcutaneous methylnaltrexone in patients with advanced illness and opioid-induced constipation: results of a randomized, placebo-controlled study and open-label extension. J Palliat Med. 2015;18(7):593–600. doi:10.1089/jpm.2014.0362.
21. Rome IV criteria; 2016. Available from: https://theromefoundation.org/rome-iv/rome-iv-criteria/.
22. Chamberlain BH, Rhiner M, Slatkin NE, Stambler N, Israel RJ. Subcutaneous methylnaltrexone for opioid-induced constipation in advanced-illness patients with or without active cancer. Pain Manag. 2020;10(2):73–84. doi:10.2217/pmt-2019-0045.
23. Wild J, Yamada T, Arjona Ferreira JC, Hale M. Onset of action of naldemedine in the treatment of opioid-induced constipation in patients with chronic noncancer pain: results from 2 randomized, placebo-controlled, phase 3 trials. Pain. 2019;160(10):2358–2364. doi:10.1097/j.pain.0000000000001629.
24. Katakami N, Harada T, Murata T, et al. Randomized phase III and extension studies: efficacy and impacts on quality of life of naldemedine in subjects with opioid-induced constipation and cancer. Ann Oncol. 2018;29(6):1461–1467. doi:10.1093/annonc/mdy118.
25. AstraZeneca Pharmaceuticals. Movantik [Package Insert]. Wilmington, DE: AstraZeneca Pharmaceuticals; 2020.
26. Chey WD, Webster L, Sostek M, Lappalainen J, Barker PN, Tack J. Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med. 2014;370(25):2387–2396. doi:10.1056/NEJMoa1310246.
27. Rauck R, Slatkin NE, Stambler N, Harper JR, Israel RJ. Randomized, double-blind trial of oral methylnaltrexone for the treatment of opioid-induced constipation in patients with chronic noncancer pain. Pain Pract. 2017;17(6):820–828. doi:10.1111/papr.12535.
28. Bartz L, Klein C, Seifert A, Herget I, Ostgathe C, Stiel S. Subcutaneous administration of drugs in palliative care: results of a systematic observational study. J Pain Symptom Manage. 2014;48(4):540–547. doi:10.1016/j.jpainsymman.2013.10.018.
29. Peacock WF, Slatkin NE, Israel RJ, Stambler N. First-dose efficacy of methylnaltrexone in patients with severe medical illness and opioid-induced constipation: a pooled analysis. J Emerg Med. 2022;62(2):231–239. doi:10.1016/j.jemermed.2021.10.012.
30. Hale M, Wild J, Reddy J, Yamada T, Arjona Ferreira JC. Naldemedine versus placebo for opioid-induced constipation (COMPOSE-1 and COMPOSE-2): two multicentre, phase 3, double-blind, randomised, parallel-group trials. Lancet Gastroenterol Hepatol. 2017;2(8):555–564. doi:10.1016/S2468-1253(17)30105-X.
31. Arshad F, Wang L, Sy C, Avraham S, Avraham HK. Blood-brain barrier integrity and breast cancer metastasis to the brain. Patholog Res Int. 2010. doi:10.4061/2011/920509.
32. Wardill HR, Mander KA, Van Sebille YZ, et al. Cytokine-mediated blood brain barrier disruption as a conduit for cancer/chemotherapy-associated neurotoxicity and cognitive dysfunction. Int J Cancer. 2016;139(12):2635–2645. doi:10.1002/ijc.30252.
33. Branca JJV, Maresca M, Morucci G, et al. Oxaliplatin-induced blood brain barrier loosening: a new point of view on chemotherapy-induced neurotoxicity. Oncotarget. 2018;9(34):23426–23438. doi:10.18632/oncotarget.25193.
34. World Health Organization. Cancer Pain Relief: With a Guide to Opioid Availability.
35. Glare P, Walsh D, Sheehan D. The adverse effects of morphine: a prospective survey of common symptoms during repeated dosing for chronic cancer pain. Am J Hosp Palliat Care. 2006;23(3):229–235. doi:10.1177/1049909106289068.
36. Brenner DM, Slatkin NE, Stambler N, Israel RJ, Coluzzi PH. The influence of brain metastases on the central nervous system effects of methylnaltrexone: a post hoc analysis of 3 randomized, double-blind studies. Support Care Cancer. 2021;29(9):5209–5218. doi:10.1007/s00520-021-06070-7.
37. Slatkin NE, Lynn R, Su C, Wang W, Israel RJ. Characterization of abdominal pain during methylnaltrexone treatment of opioid-induced constipation in advanced illness: a post hoc analysis of two clinical trials. J Pain Symptom Manage. 2011;42(5):754–760. doi:10.1016/j.jpainsymman.2011.02.015.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



