Back to Journals » Nature and Science of Sleep » Volume 14
Melatonin Treatment for Pediatric Patients with Insomnia: Is There a Place for It?
Authors Rolling J, Rabot J, Schroder CM
Received 16 June 2022
Accepted for publication 18 September 2022
Published 27 October 2022 Volume 2022:14 Pages 1927—1944
DOI https://doi.org/10.2147/NSS.S340944
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ahmed BaHammam
Julie Rolling1– 4*, Juliette Rabot1– 3,5,6*, Carmen M Schroder1– 6
1Department of Child and Adolescent Psychiatry, Strasbourg University Hospitals, Strasbourg, France; 2CNRS UPR3212- Research Team “Light, Circadian Rhythms, Sleep Homeostasis and Neuropsychiatry”, Institute of Cellular and Integrative Neurosciences, Strasbourg, France; 3Excellence Centre for Autism and Neurodevelopmental Disorders STRAS&ND, Strasbourg, France; 4Sleep Disorders Centre & International Research Centre for ChronoSomnology (Circsom), University Hospitals Strasbourg, Strasbourg, France; 5Expert Centre for High-Functioning Autism, Fondation FondaMental, Strasbourg, France; 6Autism Resources Centre 67 for Children and Adolescents, Strasbourg, France
*These authors contributed equally to this work
Correspondence: Carmen M Schroder, Email [email protected]
Abstract: Sleep is a vital physiological function that is impaired in ranges from 10% in the typically developing pediatric population to over 80% in populations of children with neurodevelopmental disorders and/or psychiatric comorbidities. Pediatric insomnia disorder is an increasing public health concern given its negative impact on synaptic plasticity involved in learning and memory consolidation but also on mood regulation, hormonal development and growth, and its significant impact on quality of life of the child, the adolescent and the family. While first-line treatment of pediatric insomnia should include parental education on sleep as well as sleep hygiene measures and behavioural treatment approaches, pharmacological interventions may be necessary if these strategies fail. Melatonin treatment has been increasingly used off-label in pediatric insomnia, given its benign safety profile. This article aims to identify the possible role of melatonin treatment for pediatric insomnia, considering its physiological role in sleep regulation and the differential effects of immediate release (IR) versus prolonged release (PR) melatonin. For the physician dealing with pediatric insomnia, it is particularly important to be able to distinguish treatment rationales implying different dosages and times of treatment intake. Finally, we discuss the benefit–risk ratio for melatonin treatment in different pediatric populations, ranging from the general pediatric population to children with different types of neurodevelopmental disorders, such as autism spectrum disorder or ADHD.
Keywords: melatonin, prolonged release, immediate release, pediatric insomnia, sleep, circadian, autism spectrum disorder, ADHD, delayed sleep phase syndrome
Introduction
Sleep is fundamental for the optimal development and overall health of children and adolescents, with both sufficient sleep duration and sleep quality being essential.1 Recent consensus statements have highlighted recommended sleep durations during childhood,2 as sleep needs vary by age. Additionally, uninterrupted night sleep is important for brain plasticity underlying learning and memory consolidation, and healthy sleep has shown many daytime benefits across development.1
However, sleep problems are common in children, and pediatric insomnia in children and adolescents ranges from 10% in typically developing children to over 80% in children with neurodevelopmental disorders (NDD) or psychiatric comorbidities,3 depending on age and definitions of insomnia used across studies. The Diagnostic and Statistical Manual of Mental Disorders (DSM-54) defines insomnia as a persistent disorder and the International Classification of Sleep Disorders, third Edition (ICSD-35) as chronic, with criteria of symptom frequency, duration since the start of the symptoms and associated daytime repercussions in the child, the parents or the family; if symptoms are mild or transient, ie if they appear only occasionally (thus they do not meet frequency criteria) or if they have no significant daytime repercussions, they should not be considered an insomnia disorder.
Pediatric sleep disturbances overall and insomnia in particular are increasingly considered a public health concern, as inadequate or disrupted sleep has been shown to have detrimental effects on daytime behavior, cognition (memory, attention and even language acquisition in the developing child)6–9 as well as on overall physical (eg obesity)10 and mental health, with higher risks of depression and suicide or self-harm behaviours in children and adolescents.11,12 Furthermore, pediatric insomnia and sleep disturbances have a high impact on quality of life of the entire family,13 and once insomnia is diagnosed, it tends to persist throughout childhood and adolescence if not treated.14,15
It is thus essential for the overall development of the child as well as for the well-being of the entire family to identify pediatric insomnia early on, and to design efficient treatment interventions. First-line treatment of pediatric insomnia should include parental education on sleep, taking into account the child’s individual development, as well as sleep hygiene measures and/or behavioural treatment approaches, which have been extensively described elsewhere in the literature.15 These non-pharmacological approaches have shown high efficiency (over 80%) in typically developing children but are often insufficient in children with NDD or psychiatric comorbidities.
When first-line treatment is insufficient, pharmacological alternatives exist but until recently, there was no approved drug for the treatment of insomnia in children. Because of its benign safety profile, melatonin has been increasingly used off-label in pediatric insomnia all over the globe,16–23 despite being approved only in specific indications and populations and not in all countries. This article aims to identify the possible role of melatonin treatment for pediatric insomnia, considering its physiological role in sleep regulation and the differential effects of immediate release (IR) versus prolonged release (PR) melatonin. For the physician dealing with pediatric insomnia, it is important to be able to distinguish treatment rationales, especially to differentiate melatonin treatment as an etiological treatment approach in some conditions where underlying melatonin or circadian rhythm abnormalities have been described, versus as a symptomatic treatment of pediatric insomnia, which implies different dosages and times of treatment intake.
For studies cited in this paper, a literature search was conducted using Medline (PubMed) in February 2022, using the terms “melatonin”, “sleep”, “circadian” and “children” or “adolescents”. In addition to the electronic search, we also used “pearling”, ie the examination of reference lists of identified articles for additional articles that may have been missed in our searches. Search criteria were inclusive of primary research studies, systematic reviews and meta-analyses related to melatonin use for sleep complaints in pediatric populations. For evaluating melatonin efficacy, the review included studies in children without underlying chronic conditions and children with NDD. To assess safety of melatonin treatment, we reviewed all available studies, including those patients with neurodevelopmental comorbidities and sleep disorders.
The first part of our paper will thus focus on the physiology of endogenous melatonin and on the differential effects of immediate release versus prolonged release melatonin in healthy subjects and different patient populations, as well as on safety of melatonin treatment. The second part reviews the conditions under which melatonin can be considered an etiological treatment, ie directly addressing a well described pathophysiology for insomnia in subgroups of pediatric patients; for these disorders, this paper will review the evidence for differential treatment with immediate versus prolonged release melatonin, as well as optimal dosages and times of treatment intake. Finally, the third part of the paper discusses the possible role of melatonin as a symptomatic treatment in pediatric insomnia, beyond indications described in the second part.
Part I. Melatonin
Melatonin Physiology
Melatonin (or 5-methoxy-N-acetyl-tryptamine) is a neuro-hormone mainly synthesized by the pineal gland from tryptophan. Both melatonin synthesis and secretion are controlled by the master biological clock located in the suprachiasmatic nuclei (SCN) of the hypothalamus which generates the internal circadian rhythm for each individual and regulates major physiological functions (sleep/wake, temperature, secretion of hormones, etc) with a rhythmicity of approximately 24 hours. Physiologically, the main external synchronizer (Zeitgeber) of the biological clock is the alternation of light and darkness. At the onset of darkness, the reduction of the retinal light supply leads in several steps to the disinhibition of enzymes responsible for melatonin synthesis within the pineal gland, whereas during light exposure melatonin synthesis and secretion is naturally blocked. Melatonin is therefore not the “sleep hormone” but the hormone that gives the signal to “switch to night mode” and reinforces the day/night contrast via the circadian clock. Melatonin thus plays a role as an endogenous synchronizer capable of reinforcing the circadian rhythms, stabilizing them and maintaining their phase relationship (internal synchronization), thus contributing to physiological coherence and to the adaptation of the whole organism to the photoperiod (see Figure 1). In addition, the concordance between the core body temperature nadir (around 4 a.m.) and the melatonin peak (around 3 to 4 a.m.) contributes to sleep maintenance.
 |
Figure 1 Melatonin, an endogenous synchronizer of the circadian system. Adapted from Claustrat B. Mélatonine et troubles du rythme veille-sommeil. Médecine Sommeil. 2009;6(1):12–24. Copyright©2009. Elsevier Masson SAS. All rights reserved.31 and Schröder CM, Broquère MA, Claustrat B, et al. Approches thérapeutiques des troubles du sommeil et des rythmes chez l’enfant avec TSA. L’Encéphale. 2022:S0013700621002177.Open Access.138 Abbreviation: SCN, suprachiasmatic nuclei. |
This physiological role of melatonin explains its effect in the treatment of sleep problems, its effect on hypertension and diabetes (reduction of insulin levels), its oncostatic effect and the reduction of cancer side effects, as well as its effect on certain gastrointestinal pathologies (see Figure 1).24–26 Melatonin acts through two main pathways: a receptor-mediated pathway (specifically MT1 and MT2 receptors) and a receptor-independent pathway.27,28 The receptor-mediated pathway acts on sleep promotion and circadian modulation, with three main effects of melatonin on sleep and circadian rhythms being identified: 1) a chronobiotic; 2) a chronohypnotic; and 3) a soporific effect.
The chronobiotic effect is the main effect described for melatonin. It consists of the ability of a substance to modify the position of the sleep/wake rhythm by advancing or delaying it within the day–night cycle. The administration of exogenous melatonin in its IR formula allows to modify the position of the physiological secretion of melatonin according to time of administration.29–31 When melatonin is administered in the afternoon (beginning or end), an advance in melatonin secretion is observed subsequently, with a maximum phase shifting effect obtained with melatonin intake 4 to 5 hours before the beginning of endogenous secretion (see Figure 2). This “phase advance” effect can be reinforced by the morning administration of light (natural or light therapy). On the contrary, with morning administration of exogenous melatonin, the physiological secretion is delayed (“phase delay”). The chronobiotic effect therefore consists of the induction of a phase shift (advance or delay) of the internal biological clock. This chronobiotic action is the physiological basis for the treatment of circadian rhythm disturbances (jet lag syndrome, delayed sleep phase syndrome (DSPS), free-run in the visually impaired, etc). Some authors distinguish a chronohypnotic effect which is characterized by the inhibition of the arousal signal emanating from the circadian clock after melatonin administration, mostly through MT1 receptors on the SCN, facilitating the switch into “night mode”.28
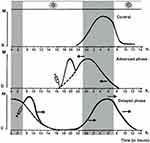 |
Figure 2 The chronobiotic action of melatonin: modification of endogenous melatonin secretion after administration of immediate release melatonin according to the phase response curve. Depending on the time of administration of immediate release melatonin, the central clock responds with a phase advance or delay. The melatonin rhythm constitutes a faithful marker of the activity of the clock allowing to objectify the phenomenon. (A) Control. (B) The plasma profile shows a phase advance after administration in the afternoon or evening, and (C), a phase delay after administration in the morning. The critical time (or turning point) which corresponds to the change in the direction of the phase change is around 15:00. Adapted from Claustrat B. Mélatonine: aspects biochimiques, physiologiques et pharmacologiques en relation avec les phénomènes rythmiques et le sommeil. Médecine Sommeil. 2020;17(3):177–194 and Claustrat B. Mélatonine et troubles du rythme veille-sommeil. Médecine Sommeil. 2009;6(1):12–24. Elsevier Masson SAS. All rights reserved.28,31 |
The soporific effect of melatonin is characterized by the induction of sleep when the homeostatic sleep pressure is insufficient, ie usually during the day and outside of the natural endogenous melatonin secretion phase.32 This effect has been explored through thermoregulation research: melatonin administration during the day mimics the endogenous thermophysiological processes that occur in the evening and which induce sleepiness (see Figure 3).32 Through an increase of distal heat loss, melatonin thus enhances the decrease in core body temperature in the late evening which promotes sleep propensity at the beginning of the night.33
 |
Figure 3 Effect of immediate release melatonin on distal vasodilatation. Illustration of the analysis of the topographic temperature with infrared thermometry in an individual (dorsal and palmar side of the hand) 1 h after taking a placebo and 1 h after taking 5 mg of immediate release melatonin (oral intake), the latter indicating a greater increase in skin blood flow by melatonin in the fingertip than in the proximal finger, most likely by opening arteriovenous anastomoses. Immediate release melatonin administration during the day (absence of endogenous melatonin secretion) mimics the endogenous thermophysiological processes that occur in the evening and induces sleepiness. Adapted from Kräuchi K, Cajochen C, Pache M, Flammer J, Wirz‐Justice A. Thermoregulatory effects of melatonin in relation to sleepiness. Chronobiol Int. 2006;23(1–2):475–484, Taylor & Francis Ltd, http://www.tandfonline.com by permission of the publisher.32 |
There is a great individual variability in physiological melatonin levels and the rate of endogenous melatonin secretion.26 The effects of exogenous melatonin as a treatment for insomnia do thus also vary on an individual level, and depend on the time of administration, dosage, the type of formulation (IR or PR) and on the association with other substances such as tobacco or contraceptive pills.26 Currently there are two treatment formulas of melatonin available, IR and PR melatonin, with differential effects on sleep and circadian rhythms.
Effects of Immediate Release Melatonin
There are many studies evaluating the effects of IR melatonin coming from the field of basic and applied research in chronobiology. Conversely, there are fewer clinical studies conducted,34–40 notably by the pharmaceutical industry, due to the wide availability of melatonin which is sold as a dietary supplement over the counter in many countries. Clinical studies are even rarer in the pediatric population than in the adult population. In addition, meta-analyses evaluating the efficacy of melatonin often include both IR and PR formulas, even though their mode of action and dosages differ. Thus, studies evaluating the efficacy of IR melatonin in primary or secondary insomnia have sometimes been realized, especially in the beginning, with high doses of several milligrams of melatonin to counteract the elimination related to the hepatic first-pass effect (plasma half-life is of the order of 20 to 30 minutes after oral intake).41 Peak plasma concentrations are reached between 20 and 240 minutes after oral administration for 2 mg IR melatonin, with a shorter peak duration than that of an endogenous profile (1–2 hours versus 8–10 hours) and with a shorter peak duration than those of PR formulation (see Figure 4).
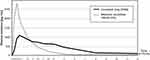 |
Figure 4 Comparison of plasma pharmacokinetics after administration of immediate release and prolonged release melatonin preparations. Plasma kinetics after administration of administration of immediate release melatonin (2 mg dose, light grey curve) versus prolonged release melatonin (2 mg dose, dark curve). Adapted from Zisapel N. Melatonin and sleep. Open Neuroendocrinol J. 2010;3:85–95.139 |
The effects of IR melatonin are explained through the combination of chronobiotic, chronohypnotic and soporific actions (see above and Figures 2 and 3). The soporific effect induces sleepiness, especially when given before the onset of the endogenous melatonin secretion, and the chronobiotic and chronohypnotic effects inhibit the wake signal emanating from the biological clock and induce a sleep phase advance. The combined effect is a decrease in sleep latency, consistently observed throughout studies,34–40 but which can also induce an earlier morning awakening, an effect few physicians are aware of. As such, Gringras et al demonstrated in a large RCT in 146 children aged 3 years to 15 years 8 months with NDD significantly earlier waking times compared to placebo (on average 29.9 minutes earlier, range: 13.6 to 46.3 minutes).106 The efficacy of IR melatonin in pediatric insomnia may thus partly be related to the treatment of an undiagnosed underlying circadian rhythm disorder through its chronobiotic effect, in particular delayed sleep phase syndrome (see below).
Effects of Prolonged Release Melatonin
The pharmacokinetic characteristics of IR melatonin which differ significantly from endogenous melatonin profiles have led to the development of PR formulations which mimic more closely the endogenous profile of the molecule (see Figure 4).42 PR melatonin can thus be prescribed to substitute melatonin over the entire night in case of insufficient endogenous melatonin secretion (for indications: see Part II). The PR form has been less studied in basic and applied chronobiology research compared to the IR form, and only few studies have been conducted in typically developing children; in contrast, scientific evidence is high in in children and adolescents with autism spectrum disorder (ASD) or neurogenetic disorders. PR melatonin produces a gradual increase in blood concentration, with a peak reached about 3 hours after administration, a plateau phase lasting about 3–4 hours at a maximum concentration of about 1000 pg/mL for a 2 mg dose, and a return to baseline within 10 hours after dosing (see Figure 4). No undesired effect on sleep phase advance has been reported. The aim of PR melatonin treatment is to improve sleep latency (like IR melatonin), but also to ensure that sleep continuity and total nighttime sleep duration are maintained. Historically, the marketing authorization for PR melatonin (Circadin®) was limited to older adults (age 55 years or older) with insomnia. Then, its efficacy and good tolerance in adults as well as empiric success in treatment of severe sleep disorders in children with ASD led to consider its use for this population. In 2015, Circadin® was first granted a temporary recommendation for use in some countries for the treatment of sleep disorders in children with ASD or neurogenetic disorders (Rett disease, Smith–Magenis syndrome, tuberous sclerosis of Bourneville and Angelman syndrome). In September 2018, pediatric PR melatonin received European marketing authorization in children with ASD.43 The recommended initial dose is 2 mg of pediatric PR melatonin that can be increased to 10 mg (increase to a 5 mg dosage over 2–4 weeks, then to 10 mg on the same schedule). The effectiveness of the treatment is evaluated clinically. In case of chronic prescription, an at least annual re-evaluation is recommended.44
Safety of Melatonin Treatment
Across studies, melatonin (IR as well as PR) has overall displayed a very benign safety profile (for studies and reviews in children and adolescents, see references.45–61 In terms of toxicology, melatonin has a good safety profile event at extremely high doses (up to 1600 mg) in adults, as shown by a recent meta-analysis,62 even though some authors suggest possible effects on the hypothalamic pituitary gonadal axis and the cardiovascular system in healthy adults.63 No suicide has ever been reported with melatonin even with very high doses (Texas Poison Centers, 779 cases between 1998 and 2003).26,64 The most common short-term side effects are, as expected, daytime somnolence, especially in the morning for PR melatonin, as well as headaches, probably linked to its vasodilatory effects (see Figure 3).65 As some children and adolescents with NDD are prescribed melatonin for more than two years,16,66,67 long-term side effects have also been studied in this population.48 In a RCT with PR melatonin for pediatric insomnia in children with ASD over a two-year study period, fatigue, agitation, cough and dyspnea were slightly more frequently reported in the PR melatonin-treated group, with no evidence, however, of impact on height, BMI or pubertal development.49 There were no withdrawal effects following long-term use and no safety concerns on concomitant therapy with stimulants.49 Another prospective 3.8-year follow-up study of 44 children with NDD who had participated in a RCT with PR melatonin for circadian rhythm sleep/wake disorders (CRSD) reported a similar mild adverse effects profile with no evidence of impact on development and puberty, no cardiovascular effect and no interactions with other medications.57
However, reports on isolated cases have raised awareness of rare side effects in adults,68,69 some of which may be linked to interactions with other medications metabolized by the same liver enzyme, cytochrome CYP1A2, among which several antidepressants and antiepileptics. On the other hand, some authors have suggested melatonin may have an inhibitory effect on CYP1A2, thus the serum concentration of substrates such as caffeine may be increased when taken together with melatonin.142 Data are unfortunately scarce regarding the prevalence of slow metabolizers of melatonin within the pediatric population, which may cause increased side effects especially with PR melatonin; future research should address this important topic.
Finally, it must be considered that not all countries have the same safety regulation rules, creating discrepancies between countries in terms of safety profiles of melatonin products. Especially in the United States where melatonin treatment production is less regulated compared to Europe, US over-the-counter melatonin formulations should be considered with caution concerning their efficacy and safety.70
Part II. Melatonin as an Etiological Treatment in Pediatric Insomnia
In several pediatric populations at high risk for insomnia, melatonin treatment can be considered an etiological treatment approach: 1) either to supplement a deficient endogenous melatonin synthesis, eg in children with ASD; 2) to correct abnormal melatonin profiles, eg in children with neurogenetic disorders (eg Smith–Magenis syndrome, Rett’s disorder, tuberous sclerosis, Angelman syndrome); or 3) to correct a circadian phase disorder, eg in children or adolescents with delayed sleep phase disorder (DSPD), in particular if associated with attention-deficit hyperactivity disorder (ADHD) or other psychiatric conditions (eg anxiety, depression). Melatonin treatment has thus already been codified with several consensus guidelines as a treatment for pediatric and/or non-neurotypical patients for these indications, by the American Academy of Neurology, the British Association for Psychopharmacology, and the French Medical and Research Sleep Society, among others.108,132,143
Insomnia in Children with ASD
Prevalence and Symptomatology
ASD is a neurodevelopmental condition that affects 1% of children.71 ASD is defined by alterations in social interactions and communication, repetitive and stereotypic behaviors, and sensory integration and processing deficits. In 70% of cases ASD is associated with comorbidities, such as ADHD and other neurodevelopmental, psychiatric, and physical conditions.72,73 Sleep problems concern 50 to 80% of children with ASD,72,74 whereas in comparison, short-term insomnia appears during development in 27% of typically developing children and becomes a chronic disorder in only 4% of them.75 While any sleep disturbances are present in 50–80% of children with ASD, a recent meta-analysis reports a prevalence of diagnosed sleep–wake disorders of 13% in the ASD population compared to 3.7% in the general population.73 The relative risk of ASD children to have a sleep disorder diagnosis compared to their TD peers is thus at least two-fold.74
Insomnia is the most common sleep complaint in ASD children, with parents reporting mainly difficulties initiating sleep (51%) and long night awakenings (10%) that affect both the child’s and family’s daily functioning (20% and 23% respectively).76 The objective sleep data from actimetry and polysomnography shows that children with ASD have a longer sleep onset latency, a shorter total sleep time, a longer wake after sleep onset (WASO), a lighter sleep (more sleep time spent in N1) and less REM sleep.77 The subjective data gathered through parent-report questionnaires and sleep diaries in that same meta-analysis reported that parental complaints of children with ASD concerned mainly the difficulties to fall asleep: bedtime anxiety, bedtime resistance, prolonged sleep latency; more parasomnias are also reported in ASD children than in TD children.77
Insomnia being frequently related to circadian rhythm disorders, these have also been assessed in the ASD population.78,79 Studies report that circadian rhythm disorders such as phase delay of sleep periods and irregular sleep–wake patterns are more frequent in children with ASD and tend to persist during adulthood.74,80
Impact of Sleep Deprivation on ASD Symptomatology
Chronic sleep deprivation in children with ASD is associated with impaired memory consolidation,81 cognitive performance alterations,82 daytime behavioral problems,82–84 lower adaptive functioning,85,86 increased severity of ASD core symptoms,82,87,88 more internalizing problems and emotion dysregulation.84,87,89,90 Sleep problems can mimic or worsen associated ADHD symptoms such as attention difficulties, and motor hyperactivity may appear as a way of fighting perceived sleepiness.83,84,87 Poor sleep continuity is also reported in the ASD population with negative effects on mood and behavior.91 Sleep disturbances in children with ASD have been associated with a lower quality of life for the families and significantly higher parental distress.92–95
Etiology of Sleep Disorders in ASD
The etiology of sleep problems in ASD is thought to be multifactorial with genetic, hormonal, neurological and environmental compounds. To date, alterations in the core melatonin production pathway seem to be the most fitting hypothesis to explain sleep and circadian rhythm disorders in ASD. Indeed, elevated serotonin plasmatic levels associated with low melatonin plasmatic levels and elevated platelet N-acetyl-serotonin (NAS) have been found in children and adults with ASD compared to controls.96 63% of children and adolescents with ASD have nocturnal urinary 6-sulfatoxymelatonin (melatonin metabolite) excretion values which were less than half of the mean excretion rate observed in the control group.97 Diurnal and nocturnal melatonin excretion levels of adolescents and adults with ASD are lower than those of TD controls, and the circadian rhythmicity is flattened in this population instead of presenting a nocturnal peak (dim light onset of melatonin, DLMO).98
Genetic and neurobiological findings showed that sleep is a necessary component of synaptic homeostasis and that synaptic and clock genes could interact and be associated in the susceptibility to ASD.99,100 Polymorphisms in clock genes may be involved in the abnormalities of the melatonin pathway in the ASD population.101,102 A study from Pagan et al in 2017 reported reduced activities of two enzymes involved in melatonin synthesis, aralkylamine N-acetyltransferase (AANAT) and acetylserotonin-O-methyltransferase (ASMT) in the pineal gland, gut and platelets of ASD subjects compared to controls.103 In this study, a correlation has been found between the reduction of ASMT activity, an elevated NAS level in the platelets and a lower plasma melatonin level. A previous study from Melke et al in 2008 similarly showed a significant decrease in ASMT activity and melatonin level in individuals with ASD compared to controls, indicating that a low melatonin level caused by a primary deficit in ASMT activity could be a risk factor for ASD.104
Prolonged Release Melatonin: An Etiological Treatment for Insomnia in Children with ASD
Clinical guidelines recommend sleep hygiene and behavioral interventions as first-line treatment for insomnia in children with ASD,105 but only 25% respond to combined sleep hygiene and behavioural treatment approaches alone.106 As around two thirds of ASD children and adolescents present an altered core melatonin production,97 a substitutive treatment with synthesized melatonin administered orally has been recommended in the most recent practical guidelines105,107,108 for sleep and circadian rhythm disorders in this population and has been increasingly prescribed in this indication.109 Previous systematic reviews and meta-analysis evaluated the efficacy and safety of melatonin, but often without discriminating IR and PR formulations and limited by the variability in dosage across studies, and sometimes pooling ASD and other NDD (ADHD, neurogenetic disorders motor disorders, intellectual disabilities, etc).44,110–113 Whereas previous studies had shown a significant effect of IR melatonin mostly on sleep onset,106 results of a randomized controlled trial (RCT) with PR melatonin with doses ranging from 2 to 10 mg per day showed not only improved sleep onset latency, but also longer sleep duration and better sleep continuity,65 as well as improvement of externalizing problem behaviours and familial quality of life.114–116 76% of children with ASD with symptoms of insomnia responded to PR melatonin treatment.117 The recommended initiation dose is 2 mg per day 30 minutes to 1 hour before bedtime, with efficacity assessment after 2–4 weeks of treatment. In case of a partial effect obtained at 2 mg, the dose can be increased to 5–10 mg per day. A very good safety profile of melatonin has been shown in this specific pediatric population, as detailed previously (see Part I. above). Melatonin is to date the first and only pharmacological treatment to be approved by the European regulatory agencies (European Medicines Agency, EMA) for insomnia in children and adolescents from 2 to 18 years old with ASD or Smith–Magenis syndrome.43
Insomnia Associated with Delayed Sleep–Wake Phase Disorder (DSPD) in Children and Adolescents
Insomnia Associated with DSPD in Adolescents
Prevalence and Developmental Characteristics
The ICSD-35 defines DSPD as a CRSD which corresponds to CRSD common criteria: persistent or recurrent sleep–wake pattern disturbances due to alterations of the endogenous circadian system or to misalignment between the endogenous circadian rhythm and exogenous factors; leading to insomnia, excessive daytime sleepiness or both; and associated with impairment of social, occupational and/or other areas of functioning. Specific DSPD criteria include a significant and chronic delay in the phase of the major sleep period (minimum 2 hours of sleep-onset delay for at least three months, confirmed by actigraphy or sleep diaries), with inability to fall asleep and awaken at a desired and socially acceptable clock time. In DSPD the endogenous melatonin rhythm is delayed (measured through dim-light melatonin onset (DLMO) in the evening) and endogenous circadian rhythms are not synchronized with social constraints and desired times for sleep: this phenomenon is known as “social jet lag”.118 DSPD is often misinterpreted as sleep-onset insomnia. Around 10% of outpatients assessed in specialized sleep centers for insomnia complaints actually suffer from DSPD.119
Circadian sleep–wake rhythms can be objectively measured through DLMO assessment or indirectly derived through chronotype. A study by Paine et al in New Zealand identified a prevalence of 8.90% of moderate to extreme evening chronotypes in a sample of 9100 adults (assessed using the Munich Chronotype Questionnaire).120 The chronotype has intraindividual variations through life with a physiological developmental delay in sleep–wake rhythms during adolescence and a progressive advance with age during adulthood (see Figure 5).118 DSPD is by far the most frequent CRSD and compared to a prevalence of only about 0.17–1.51% in the adult population,121 its prevalence is highest during adolescence with 3.3–17% of teenagers suffering from it;122,123 furthermore, in teenagers, DSPD has been linked to higher rates of depression, anxiety, and ADHD symptoms.124
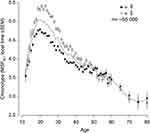 |
Figure 5 Chronotype variation across lifetime, depending on gender. Chronotype was assessed through the Munich Chronotype Questionnaire, with lower values indication morning chronotypes and higher values evening chronotypes (Adapted from Sleep Med Rev. 11(6). Roenneberg T, Kuehnle T, Juda M, et al. Epidemiology of the human circadian clock. 429–438, Copyright 2007, with permission from Elsevier).118 During adolescence, studies have shown a significant phase shift towards evening types. This phase delay is more important and lasts longer in boys compared to girls. |
Insomnia Associated with DSPD in Children with ADHD
Prevalence and Symptomatology
ADHD is a neurodevelopmental disorder characterized by inattentive symptoms, impulsivity and hyperactivity, that affects 5–7% of children.125,126 25–55% of parents of children with ADHD report that their children have sleep problems.127 The results of a meta-analysis from Cortese et al in 2009 on subjective sleep-related measures showed a higher bedtime resistance, more sleep onset difficulties, more night awakenings, more difficulties with morning awakenings and significantly more daytime sleepiness in children with ADHD compared to the general pediatric population.127 The same meta-analysis results on objective sleep data reported a longer sleep latency, a higher number of stage shift per hour of sleep and a lower sleep efficiency in children with ADHD compared to controls. Additionally, a significantly higher apnea–hypopnea index (AHI) was shown in children with ADHD compared to controls.127
Bi-Directional Effects of Insomnia and ADHD Symptomatology
Excessive sleepiness during the day may not only cause attention difficulties, but also induce hyperkinetic behavior to fight against perceived somnolence, therefore mimicking or aggravating ADHD symptoms.128 Symptoms of ADHD in the evening, such as hyperactivity, restlessness and poor planification skills, may contribute to difficult behavior around bedtime, increase bedtime resistance and thus delay sleep. A rebound effect at the end of the medication effectiveness in the late afternoon or evening may also contribute to sleep initiation difficulties. On the contrary, persistent effects of prolonged release psychostimulant in the evening may have a direct negative effect on sleep initiation. Restless leg syndrome (RLS) is also more frequent in ADHD and can mimic evening hyperactivity and explain an increased nocturnal motor activity and agitation during sleep in children with ADHD, possible related to higher rates of periodic limb movement disorder which is commonly associated with RLS.128 As iron is a cofactor in dopamine synthesis whose pathway is involved in ADHD, iron deficiency has been pointed as a possible common underlying etiopathophysiological factor to RLS and ADHD.128 Iron supplementation is proven to be effective on both RLS and ADHD symptoms in children with iron deficiency.129 Finally, given the prevalence of sleep-onset insomnia, studies have assessed the presence of DSPD in children and adolescents with ADHD through measure of DLMO,128 and have been able to show a delayed sleep phase and delayed DLMO in this population.130
Immediate Release Melatonin: An Etiological Treatment for Insomnia Symptoms Related to DSPD in Children with ADHD and Adolescents
IR melatonin treatment is the gold standard pharmacological approach for DSPD in children, adolescents and adults.131,132 Chronobiological research had shown for a long time that the chronobiotic phase advance effect of IR melatonin exists already at dosages as low as 0.3 mg and does not benefit from dose increases.133 However, IR melatonin is available as a dietary food supplement in many countries and as such has not been evaluated or approved by any regulatory agency to treat sleep or circadian rhythm disorders. A review of 19 randomized controlled trials of IR melatonin daily treatment on a total of 841 children and adolescents with DSPD showed a consistent improvement of sleep latency by 22 to 60 min without serious adverse effects.47 A meta-analysis of seven RCTs assessing efficacy and safety of melatonin in 387 children and adolescents with sleep-onset insomnia associated with DSPD from 6 to 19 years old concluded that melatonin advanced mean sleep-onset time by 37 min and DLMO by 49 min,46 including two RCTS on children and adolescents with ADHD (see Table 1).134,135 Another study from Mohammadi et al in 2012 evaluated the effect of combined treatment of melatonin (3–6 mg) and methylphenidate (1 mg/kg) in a group of 26 children with ADHD whose sleep symptoms were assessed using the Sleep Disturbance Scale for Children (SDSC) parent-questionnaire, with a placebo group of 24 children treated with placebo+methylphenidate (1 mg/kg).136 The results showed a partial improvement of total sleep score at SDSC in the melatonin group versus placebo group but failed to reach significance, possibly due to the fact that they did not restrict the inclusion criteria to children with insomnia symptoms or diagnosed DSPD. This sum of scientific evidence points out that IR melatonin is an efficacious and safe chronobiotic treatment for DSPD in children and adolescents with or without ADHD when administered at 0.5 mg, 3 to 5 h before DLMO (corresponding to 4–6 h before usual sleep initiation time) for an optimal chronobiotic phase advance effect. Alternatively, for a combination of the chronobiotic, chronohypnotic and soporific effect of IR melatonin (see Part I, above), a prescription of 1 to 3 mg at bedtime is equally interesting (though the degree of the induced phase shift will be less than if given several hours earlier, see Figure 2).47,132 Even though the benign safety profile of melatonin is established (see above), as chronotype varies across lifespan and endogenous circadian rhythm may change during long-term treatment, it is recommended to stop and reassess the indication of melatonin treatment regularly (at least once a year, for example during the summer holidays).
 |
Table 1 IR or PR Melatonin as an Etiological Treatment: Summary of Indications, Evidence and Approvals |
Part III. Is There a Role for Melatonin in Pediatric Insomnia?
We have hereabove reviewed in detail scientific evidence from clinical as well as from basic chronobiology research, in order to clarify the differential roles of IR versus PR melatonin treatment as an etiological treatment in several pediatric populations, with recommendations on differential dosing and timing of melatonin administration. Based on these data, the question arises of whether melatonin (IR or PR) could also be used as a symptomatic treatment in pediatric insomnia disorder outside of the indications described in Part II (above), if sleep hygiene measures and behavioural treatment approaches have not been successful. Some have argued, for occasional sleeplessness in the pediatric population which is different from pediatric insomnia described here, that the benefit–risk ratio may be in favor of occasional melatonin treatment, in particular when taking into account its benign safety profile (see above) compared to other pharmacological agents available for children.44,137
Overall scientific evidence for the efficacity of melatonin treatment in pediatric insomnia remains limited,34–40 and only few randomized controlled trials have been conducted to date.34,38–40 Furthermore, many studies have not clearly distinguished insomnia complaints from pediatric insomnia disorder and from DSPD, adding a significant bias to some of the study results.
Taking into account these different evidences, and in line with the expert consensus of the French Medical and Research Sleep Society (SFRMS),132 we suggest that IR melatonin in particular may have a relevant role in treating pediatric insomnia if a first line of sleep hygiene measures and behavioral treatment approaches have not been successful, and after ruling out other underlying sleep disorders such as sleep apnea syndrome, restless leg syndrome or central hypersomnolence disorders. Additional arguments in favor of IR melatonin treatment in an individual child with pediatric insomnia disorder are: 1) if the problem is mainly sleep-onset insomnia; 2) if the pediatric insomnia disorder is associated with a sleep phase delay (even if DSPD criteria are not completely met); 3) if there is a positive family history of DSPD or late chronotype; and finally 4) when daytime repercussions are major and/or repercussions on the life of the family, eg very high stress levels and/or appearance of depressive or anxious symptomatology in parents related to the lack of sleep due to their child’s insomnia disorder. Under these conditions, IR melatonin treatment has a highly positive benefit–risk ratio, given the severe repercussions of pediatric insomnia disorder in the long run and its persistence into adulthood if not treated (see above), on one hand, and the benign safety profile of melatonin on the other. The dosages and times of administrations are similar to the ones described above for IR melatonin.
Conclusion
Solid scientific evidence from clinical as well as from basic chronobiology research underlines the differential roles of IR versus PR melatonin treatment as an etiological treatment in several pediatric populations, in particular in children with NDD, or if the insomnia complaint is associated with delayed sleep phase disorder. For these indications, treatment recommendations regarding differential dosing and timing of IR versus PR melatonin administration are provided. Additionally, IR melatonin may have a role in pediatric insomnia disorder, when first-line therapy with sleep hygiene measures and behavioural treatment approaches have failed, and when other underlying sleep disorders have been ruled out. Taking into account the many negative repercussions of pediatric insomnia disorder on the child’s daytime functioning and long-term development on the one hand, the benign safety profile of IR melatonin and its beneficial effect on sleep (in particular sleep onset) and quality of life of the child and the family on the other, the benefit–risk ratio weighs largely in favor of a role for melatonin treatment in pediatric insomnia, under conditions detailed above. Future research should address efficacy of PR melatonin in pediatric insomnia beyond the autism spectrum and neurogenetic disorders, eg in children with ADHD and other neurodevelopmental or child psychiatric disorders, as well as conduct head-to-head studies on IR versus PR melatonin for different types of pediatric insomnia, in order to further refine treatment melatonin treatment indications and modalities in children and adolescents.
Acknowledgment
Julie Rolling and Juliette Rabot are co-first authors for this study. We would like to thank Bruno Claustrat and Kurt Kräuchi for their valuable contribution during discussions regarding the present manuscript and for their consent to use illustrative figures for this article.
Disclosure
Prof. Dr. Carmen M Schroder reports grants and/or personal fees from Neurim and Biocodex, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Meltzer LJ, Williamson AA, Mindell JA. Pediatric sleep health: it matters, and so does how we define it. Sleep Med Rev. 2021;57:101425. doi:10.1016/j.smrv.2021.101425
2. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1(4):233–243. doi:10.1016/j.sleh.2015.10.004
3. Meltzer LJ, Plaufcan MR, Thomas JH, Mindell JA. Sleep problems and sleep disorders in pediatric primary care: treatment recommendations, persistence, and health care utilization. J Clin Sleep Med JCSM off Publ Am Acad Sleep Med. 2014;10(4):421–426. doi:10.5664/jcsm.3620
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
5. American Academy of Sleep Medicine. International Classification of Sleep Disorders; 2014.
6. Dionne G, Touchette E, Forget-Dubois N, et al. Associations between sleep-wake consolidation and language development in early childhood: a longitudinal twin study. Sleep. 2011;34(8):987–995. doi:10.5665/SLEEP.1148
7. Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin. 2011;58(3):649–665.
8. Owens J. Adolescent Sleep Working Group, Committee on Adolescence. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–932. doi:10.1542/peds.2014-1696
9. Ai L, et al. The Developmental Course of Sleep Disturbances Across Childhood Relates to Brain Morphology at Age 7: the Generation R Study. Sleep. 2017;40:1. doi:10.1093/sleep/zsw022
10. Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: a systematic review. Sleep Med Rev. 2012;16(3):231–241. doi:10.1016/j.smrv.2011.05.005
11. Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe M. Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use. J Youth Adolesc. 2015;44(2):362–378. doi:10.1007/s10964-014-0170-3
12. Wong MM, Brower KJ, Zucker RA. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res. 2011;45(4):505–511. doi:10.1016/j.jpsychires.2010.09.005
13. Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. J Fam Psychol JFP J Div Fam Psychol Am Psychol Assoc Div. 2007;21(1):67–73. doi:10.1037/0893-3200.21.1.67
14. Cook F, Conway LJ, Giallo R, Gartland D, Sciberras E, Brown S. Infant sleep and child mental health: a longitudinal investigation. Arch Dis Child. 2020;105(7):655–660. doi:10.1136/archdischild-2019-318014
15. Meltzer LJ, Wainer A, Engstrom E, Pepa L, Mindell JA. Seeing the Whole Elephant: a scoping review of behavioral treatments for pediatric insomnia. Sleep Med Rev. 2021;56:101410. doi:10.1016/j.smrv.2020.101410
16. Hartz I, Handal M, Tverdal A, Skurtveit S. Paediatric Off-Label Use of Melatonin – a Register Linkage Study between the Norwegian Prescription Database and Patient Register. Basic Clin Pharmacol Toxicol. 2015;117(4):267–273. doi:10.1111/bcpt.12411
17. Hartz I, Furu K, Bratlid T, Handal M, Skurtveit S. Hypnotic drug use among 0–17 year olds during 2004–2011: a nationwide prescription database study. Scand J Public Health. 2012;40(8):704–711. doi:10.1177/1403494812464446
18. Braüner JV, Johansen LM, Roesbjerg T, Pagsberg AK. Off-Label Prescription of Psychopharmacological Drugs in Child and Adolescent Psychiatry. J Clin Psychopharmacol. 2016;36(5):500–507. doi:10.1097/JCP.0000000000000559
19. Bock DE, Roach-Fox E, Seabrook JA, Rieder MJ, Matsui D. Sleep-promoting medications in children: physician prescribing habits in Southwestern Ontario, Canada. Sleep Med. 2016;17:52–56. doi:10.1016/j.sleep.2015.10.003
20. Nielsen ES, Rasmussen L, Hellfritzsch M, Thomsen PH, Nørgaard M, Laursen T. Trends in Off-Label Prescribing of Sedatives, Hypnotics and Antidepressants among Children and Adolescents – a Danish, Nationwide Register-Based Study. Basic Clin Pharmacol Toxicol. 2017;120(4):360–367. doi:10.1111/bcpt.12706
21. Efron D, Danchin MH, Cranswick NE, Gulenc A, Hearps S, Hiscock H. Medication prescribed by Australian paediatricians: psychotropics predominate. J Paediatr Child Health. 2017;53(10):957–962. doi:10.1111/jpc.13615
22. Procaccini DE, Kudchadkar SR. Melatonin Administration Patterns for Pediatric Inpatients in a Tertiary Children’s Hospital. Hosp Pediatr. 2021;11(11):e308–e312. doi:10.1542/hpeds.2021-006117
23. Kimland EE, Bardage C, Collin J, Järleborg A, Ljung R, Iliadou AN. Pediatric use of prescribed melatonin in Sweden 2006–2017: a register based study. Eur Child Adolesc Psychiatry. 2021;30(9):1339–1350. doi:10.1007/s00787-020-01598-1
24. Rivara S, Pala D, Bedini A, Spadoni G. Therapeutic uses of melatonin and melatonin derivatives: a patent review (2012 – 2014). Expert Opin Ther Pat. 2015;25(4):425–441. doi:10.1517/13543776.2014.1001739
25. Tordjman S, Chokron S, Delorme R, et al. Melatonin: pharmacology, Functions and Therapeutic Benefits. Curr Neuropharmacol. 2017;15(3):434–443. doi:10.2174/1570159X14666161228122115
26. Lalanne S, Fougerou-Leurent C, Anderson GM, et al. Melatonin: from pharmacokinetics to clinical use in autism spectrum disorder. Int J Mol Sci. 2021;22(3):1490. doi:10.3390/ijms22031490
27. Reiter RJ, Tan DX, Galano A. Melatonin: exceeding Expectations. Physiology. 2014;29(5):325–333. doi:10.1152/physiol.00011.2014
28. Claustrat B. Mélatonine: aspects biochimiques, physiologiques et pharmacologiques en relation avec les phénomènes rythmiques et le sommeil. Médecine Sommeil. 2020;17(3):177–194. doi:10.1016/j.msom.2019.12.187
29. Lewy AJ, Ahmed S, Jackson JML, Sack RL. Melatonin Shifts Human Circadian Rhythms According to a Phase-Response Curve. Chronobiol Int. 1992;9(5):380–392. doi:10.3109/07420529209064550
30. Zaidan R, Geoffriau M, Brun J, et al. Melatonin Is Able to Influence Its Secretion in Humans: description of a Phase-Response Curve. Neuroendocrinology. 1994;60(1):105–112. doi:10.1159/000126726
31. Claustrat B. Mélatonine et troubles du rythme veille-sommeil. Médecine Sommeil. 2009;6(1):12–24. doi:10.1016/j.msom.2009.02.001
32. Kräuchi K, Cajochen C, Pache M, Flammer J, Wirz‐Justice A. Thermoregulatory effects of melatonin in relation to sleepiness. Chronobiol Int. 2006;23(1–2):475–484. doi:10.1080/07420520500545854
33. Strassman RJ, Qualls CR, Lisansky EJ, Peake GT. Elevated rectal temperature produced by all-night bright light is reversed by melatonin infusion in men. J Appl Physiol. 1991;71(6):2178–2182. doi:10.1152/jappl.1991.71.6.2178
34. Smits MG, Nagtegaal EE, van der Heijden J, Coenen AM, Kerkhof GA. Melatonin for chronic sleep onset insomnia in children: a randomized placebo-controlled trial. J Child Neurol. 2001;16(2):86–92. doi:10.1177/088307380101600204
35. Ivanenko A, Crabtree VM, Tauman R, Gozal D. Melatonin in children and adolescents with insomnia: a retrospective study. Clin Pediatr (Phila). 2003;42(1):51–58. doi:10.1177/000992280304200108
36. van der Heijden KB, Smits MG, van Someren EJW, Boudewijn Gunning W. Prediction of melatonin efficacy by pretreatment dim light melatonin onset in children with idiopathic chronic sleep onset insomnia. J Sleep Res. 2005;14(2):187–194. doi:10.1111/j.1365-2869.2005.00451.x
37. van Geijlswijk IM, van der Heijden KB, Egberts ACG, Korzilius HPLM, Smits MG. Dose finding of melatonin for chronic idiopathic childhood sleep onset insomnia: an RCT. Psychopharmacology. 2010;212(3):379–391. doi:10.1007/s00213-010-1962-0
38. Eckerberg B, Lowden A, Nagai R, Åkerstedt T. Melatonin treatment effects on adolescent students’ sleep timing and sleepiness in a placebo-controlled crossover study. Chronobiol Int. 2012;29(9):1239–1248. doi:10.3109/07420528.2012.719962
39. van Maanen A, Meijer AM, Smits MG, van der Heijden KB, Oort FJ. Effects of Melatonin and Bright Light Treatment in Childhood Chronic Sleep Onset Insomnia With Late Melatonin Onset: a Randomized Controlled Study. Sleep. 2017;40:2. doi:10.1093/sleep/zsw038
40. Smits MG, van Stel HF, van der Heijden K, Meijer AM, Coenen AML, Kerkhof GA. Melatonin improves health status and sleep in children with idiopathic chronic sleep-onset insomnia: a randomized placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2003;42(11):1286–1293. doi:10.1097/01.chi.0000085756.71002.86
41. Di WL, Kadva A, Johnston A, Silman R. Variable Bioavailability of Oral Melatonin. N Engl J Med. 1997;336(14):1028–1029. doi:10.1056/NEJM199704033361418
42. Garfinkel D, Laudon M, Nof D, Zisapel N. Improvement of sleep quality in elderly people by controlled-release melatonin. Lancet Lond Engl. 1995;346(8974):541–544. doi:10.1016/s0140-6736(95)91382-3
43. EMA. Slenyto. European Medicines Agency; 2018. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/slenyto.
44. Bruni O, Angriman M, Calisti F, et al. Practitioner Review: treatment of chronic insomnia in children and adolescents with neurodevelopmental disabilities. J Child Psychol Psychiatry. 2018;59(5):489–508. doi:10.1111/jcpp.12812
45. Salanitro M, Wrigley T, Ghabra H, et al. Efficacy on sleep parameters and tolerability of melatonin in individuals with sleep or mental disorders: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2022;139:104723. doi:10.1016/j.neubiorev.2022.104723
46. Wei S, Smits MG, Tang X, et al. Efficacy and safety of melatonin for sleep onset insomnia in children and adolescents: a meta-analysis of randomized controlled trials. Sleep Med. 2020;68:1–8. doi:10.1016/j.sleep.2019.02.017
47. Mantle D, Smits M, Boss M, Miedema I, van Geijlswijk I. Efficacy and safety of supplemental melatonin for delayed sleep-wake phase disorder in children: an overview. Sleep Med X. 2020;2:100022. doi:10.1016/j.sleepx.2020.100022
48. Zisapel N. Assessing the potential for drug interactions and long term safety of melatonin for the treatment of insomnia in children with autism spectrum disorder. Expert Rev Clin Pharmacol. 2022;15(2):175–185. doi:10.1080/17512433.2022.2053520
49. Malow BA, Findling RL, Schroder CM, et al. Sleep, Growth, and Puberty After 2 Years of Prolonged-Release Melatonin in Children With Autism Spectrum Disorder. J Am Acad Child Adolesc Psychiatry. 2021;60(2):252–261.e3. doi:10.1016/j.jaac.2019.12.007
50. Yuge K, Nagamitsu S, Ishikawa Y, et al. Long-term melatonin treatment for the sleep problems and aberrant behaviors of children with neurodevelopmental disorders. BMC Psychiatry. 2020;20(1):445. doi:10.1186/s12888-020-02847-y
51. Zwart TC, Smits MG, Egberts TCG, Rademaker CMA, van Geijlswijk IM. Long-Term Melatonin Therapy for Adolescents and Young Adults with Chronic Sleep Onset Insomnia and Late Melatonin Onset: evaluation of Sleep Quality, Chronotype, and Lifestyle Factors Compared to Age-Related Randomly Selected Population Cohorts. Healthc Basel Switz. 2018;6(1):E23. doi:10.3390/healthcare6010023
52. McDonagh MS, Holmes R, Hsu F. Pharmacologic Treatments for Sleep Disorders in Children: a Systematic Review. J Child Neurol. 2019;34(5):237–247. doi:10.1177/0883073818821030
53. Boafo A, Greenham S, Alenezi S, et al. Could long-term administration of melatonin to prepubertal children affect timing of puberty? A clinician’s perspective. Nat Sci Sleep. 2019;11:1–10. doi:10.2147/NSS.S181365
54. Erland LAE, Saxena PK. Melatonin Natural Health Products and Supplements: presence of Serotonin and Significant Variability of Melatonin Content. J Clin Sleep Med JCSM off Publ Am Acad Sleep Med. 2017;13(2):275–281. doi:10.5664/jcsm.6462
55. van Geijlswijk IM, Mol RH, Egberts TCG, Smits MG. Evaluation of sleep, puberty and mental health in children with long-term melatonin treatment for chronic idiopathic childhood sleep onset insomnia. Psychopharmacology. 2011;216(1):111–120. doi:10.1007/s00213-011-2202-y
56. Hoebert M, Van Der Heijden KB, Van Geijlswijk IM, Smits MG. Long-term follow-up of melatonin treatment in children with ADHD and chronic sleep onset insomnia. J Pineal Res. 2009;47(1):1–7. doi:10.1111/j.1600-079X.2009.00681.x
57. Carr R, Wasdell MB, Hamilton D, et al. Long-term effectiveness outcome of melatonin therapy in children with treatment-resistant circadian rhythm sleep disorders. J Pineal Res. 2007;43(4):351–359. doi:10.1111/j.1600-079X.2007.00485.x
58. Besag F, Vasey MJ, Lao KS, Wong IC. Adverse events associated with melatonin for the treatment of primary or secondary sleep disorders: a systematic review. CNS Drugs. 2019;33(12):1167–1186. doi:10.1007/s40263-019-00680-w
59. Foley HM, Steel AE. Adverse events associated with oral administration of melatonin: a critical systematic review of clinical evidence. Complement Ther Med. 2019;42:65–81. doi:10.1016/j.ctim.2018.11.003
60. Andersen LPH, Gögenur I, Rosenberg J, Reiter RJ. The safety of melatonin in humans. Clin Drug Investig. 2016;36(3):169–175. doi:10.1007/s40261-015-0368-5
61. Seabra MD, Bignotto M. Randomized, double-blind clinical trial, controlled with placebo, of the toxicology of chronic melatonin treatment. J Pineal Res. 2000;29(4):193–200. doi:10.1034/j.1600-0633.2002.290401.x
62. Menczel Schrire Z, Phillips CL, Chapman JL, et al. Safety of higher doses of melatonin in adults: a systematic review and meta-analysis. J Pineal Res. 2022;72(2):e12782. doi:10.1111/jpi.12782
63. Kennaway DJ. What do we really know about the safety and efficacy of melatonin for sleep disorders? Curr Med Res Opin. 2022;38(2):211–227. doi:10.1080/03007995.2021.2000714
64. Forrester MB. Melatonin exposures reported to Texas poison centers in 1998-2003. Vet Hum Toxicol. 2004;46(6):345–346.
65. Gringras P, Nir T, Breddy J, Frydman-Marom A, Findling RL. Efficacy and Safety of Pediatric Prolonged-Release Melatonin for Insomnia in Children With Autism Spectrum Disorder. J Am Acad Child Adolesc Psychiatry. 2017;56(11):948–957.e4. doi:10.1016/j.jaac.2017.09.414
66. Bliddal M, Kildegaard H, Rasmussen L, et al. Melatonin use among children, adolescents, and young adults: a Danish nationwide drug utilization study. Eur Child Adolesc Psychiatry. 2022;1:1–9.
67. Tedroff K, von Euler M, Dahlén E. Melatonin usage in children and young adults, a registry-based cohort study. Eur J Paediatr Neurol. 2022;39:30–34. doi:10.1016/j.ejpn.2022.05.007
68. Hong YG, Riegler JL. Is melatonin associated with the development of autoimmune hepatitis? J Clin Gastroenterol. 1997;25(1):376–378. doi:10.1097/00004836-199707000-00020
69. Bardazzi F, Placucci F, Neri I, D’Antuono A, Patrizi A. Fixed drug eruption due to melatonin. Acta Derm Venereol. 1998;78(1):69–70. doi:10.1080/00015559850135913
70. Skrzelowski M, Brookhaus A, Shea LA, Berlau DJ. Melatonin Use in Pediatrics: evaluating the Discrepancy in Evidence Based on Country and Regulations Regarding Production. J Pediatr Pharmacol Ther. 2021;26(1):4–20. doi:10.5863/1551-6776-26.1.4
71. Zeidan J, Fombonne E, Scorah J, et al. Global prevalence of autism: a systematic review update. Autism Res off J Int Soc Autism Res. 2022;15(5):778–790. doi:10.1002/aur.2696
72. Lai MC, Lombardo MV, Baron-Cohen S. Autism. Lancet Lond Engl. 2014;383(9920):896–910. doi:10.1016/S0140-6736(13)61539-1
73. Lai MC, Kassee C, Besney R, et al. Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(10):819–829. doi:10.1016/S2215-0366(19)30289-5
74. Elrod MG, Nylund CM, Susi AL, et al. Prevalence of diagnosed sleep disorders and related diagnostic and surgical procedures in children with autism spectrum disorders. J Dev Behav Pediatr. 2016;37(5):377–384. doi:10.1097/DBP.0000000000000248
75. Combs D, Goodwin JL, Quan SF, Morgan WJ, Shetty S, Parthasarathy S. Insomnia, health-related quality of life and health outcomes in children: a seven year longitudinal cohort. Sci Rep. 2016;6(1):1–10. doi:10.1038/srep27921
76. Krakowiak P, Goodlin-Jones B, Hertz-Picciotto I, Croen LA, Hansen RL. Sleep problems in children with autism spectrum disorders, developmental delays, and typical development: a population-based study. J Sleep Res. 2008;17(2):197–206. doi:10.1111/j.1365-2869.2008.00650.x
77. Díaz-Román A, Zhang J, Delorme R, Beggiato A, Cortese S. Sleep in youth with autism spectrum disorders: systematic review and meta-analysis of subjective and objective studies. Evid Based Ment Health. 2018;21(4):146–154. doi:10.1136/ebmental-2018-300037
78. Geoffray MM, Nicolas A, Speranza M, Georgieff N. Are circadian rhythms new pathways to understand Autism Spectrum Disorder? J Physiol-Paris. 2016;110(4):434–438. doi:10.1016/j.jphysparis.2017.06.002
79. Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: a systematic review and meta-analysis. Dev Med Child Neurol. 2011;53(9):783–792. doi:10.1111/j.1469-8749.2011.03980.x
80. Carmassi C, Palagini L, Caruso D, et al. Systematic Review of Sleep Disturbances and Circadian Sleep Desynchronization in Autism Spectrum Disorder: toward an Integrative Model of a Self-Reinforcing Loop. Front Psychiatry. 2019;10. doi:10.3389/fpsyt.2019.00366
81. Maski K, Holbrook H, Manoach D, Hanson E, Kapur K, Stickgold R. Sleep Dependent Memory Consolidation in Children with Autism Spectrum Disorder. Sleep. 2015;38(12):1955–1963. doi:10.5665/sleep.5248
82. Veatch OJ, Sutcliffe JS, Warren ZE, Keenan BT, Potter MH, Malow BA. Shorter sleep duration is associated with social impairment and comorbidities in ASD. Autism Res off J Int Soc Autism Res. 2017;10(7):1221–1238. doi:10.1002/aur.1765
83. Cohen S, Conduit R, Lockley SW, Rajaratnam SM, Cornish KM. The relationship between sleep and behavior in autism spectrum disorder (ASD): a review. J Neurodev Disord. 2014;6(1):1–10. doi:10.1186/1866-1955-6-44
84. Mazurek MO, Sohl K. Sleep and Behavioral Problems in Children with Autism Spectrum Disorder. J Autism Dev Disord. 2016;46(6):1906–1915. doi:10.1007/s10803-016-2723-7
85. Sikora DM, Johnson K, Clemons T, Katz T. The relationship between sleep problems and daytime behavior in children of different ages with autism spectrum disorders. Pediatrics. 2012;130(Supplement_2):S83–S90. doi:10.1542/peds.2012-0900F
86. Taylor MA, Schreck KA, Mulick JA. Sleep disruption as a correlate to cognitive and adaptive behavior problems in autism spectrum disorders. Res Dev Disabil. 2012;33(5):1408–1417. doi:10.1016/j.ridd.2012.03.013
87. Mayes SD, Calhoun SL. Variables related to sleep problems in children with autism. Res Autism Spectr Disord. 2009;3(4):931–941. doi:10.1016/j.rasd.2009.04.002
88. Nguyen AKD, Murphy LE, Kocak M, Tylavsky FA, Pagani LS. Prospective Associations Between Infant Sleep at 12 Months and Autism Spectrum Disorder Screening Scores at 24 Months in a Community-Based Birth Cohort. J Clin Psychiatry. 2018;79(1):16m11127. doi:10.4088/JCP.16m11127
89. Mindell JA, Leichman ES, DuMond C, Sadeh A. Sleep and Social-Emotional Development in Infants and Toddlers. J Clin Child Adolesc Psychol off J Soc Clin Child Adolesc Psychol Am Psychol Assoc Div. 2017;46(2):236–246. doi:10.1080/15374416.2016.1188701
90. May T, Cornish K, Conduit R, Rajaratnam SMW, Rinehart NJ. Sleep in high-functioning children with autism: longitudinal developmental change and associations with behavior problems. Behav Sleep Med. 2015;13(1):2–18. doi:10.1080/15402002.2013.829064
91. Yavuz-Kodat E, Reynaud E, Geoffray MM, et al. Disturbances of Continuous Sleep and Circadian Rhythms Account for Behavioral Difficulties in Children with Autism Spectrum Disorder. J Clin Med. 2020;9(6):1978. doi:10.3390/jcm9061978
92. Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep. 2009;32(5):599–606. doi:10.1093/sleep/32.5.599
93. Doo S, Wing YK. Sleep problems of children with pervasive developmental disorders: correlation with parental stress. Dev Med Child Neurol. 2006;48(8):650–655. doi:10.1017/S001216220600137X
94. Levin A, Scher A. Sleep Problems in Young Children with Autism Spectrum Disorders: a Study of Parenting Stress, Mothers’ Sleep-Related Cognitions, and Bedtime Behaviors. CNS Neurosci Ther. 2016;22(11):921–927. doi:10.1111/cns.12651
95. Polimeni M, Richdale A, Francis A. The impact of children’s sleep problems on the family and behavioural processes related to their development and maintenance. E-J Appl Psychol. 2007;3(1):):. doi:10.7790/ejap.v3i1.82
96. Pagan C, Delorme R, Callebert J, et al. The serotonin-N-acetylserotonin-melatonin pathway as a biomarker for autism spectrum disorders. Transl Psychiatry. 2014;4:e479. doi:10.1038/tp.2014.120
97. Tordjman S, Anderson GM, Pichard N, Charbuy H, Touitou Y. Nocturnal excretion of 6-sulphatoxymelatonin in children and adolescents with autistic disorder. Biol Psychiatry. 2005;57(2):134–138. doi:10.1016/j.biopsych.2004.11.003
98. Tordjman S, Anderson GM, Bellissant E, et al. Day and nighttime excretion of 6-sulphatoxymelatonin in adolescents and young adults with autistic disorder. Psychoneuroendocrinology. 2012;37(12):1990–1997. doi:10.1016/j.psyneuen.2012.04.013
99. Bourgeron T. From the genetic architecture to synaptic plasticity in autism spectrum disorder. Nat Rev Neurosci. 2015;16(9):551–563. doi:10.1038/nrn3992
100. Bourgeron T. The possible interplay of synaptic and clock genes in autism spectrum disorders. In: Cold Spring Harbor Symposia on Quantitative Biology. Vol. 72. Cold Spring Harbor Laboratory Press; 2007:645–654.
101. Yang Z, Matsumoto A, Nakayama K, et al. Circadian-relevant genes are highly polymorphic in autism spectrum disorder patients. Brain Dev. 2016;38(1):91–99. doi:10.1016/j.braindev.2015.04.006
102. Nicholas B, Rudrasingham V, Nash S, Kirov G, Owen MJ, Wimpory DC. Association of Per1 and Npas2 with autistic disorder: support for the clock genes/social timing hypothesis. Mol Psychiatry. 2007;12(6):581–592. doi:10.1038/sj.mp.4001953
103. Pagan C, Goubran-Botros H, Delorme R, et al. Disruption of melatonin synthesis is associated with impaired 14-3-3 and miR-451 levels in patients with autism spectrum disorders. Sci Rep. 2017;7(1):2096. doi:10.1038/s41598-017-02152-x
104. Melke J, Goubran Botros H, Chaste P, et al. Abnormal melatonin synthesis in autism spectrum disorders. Mol Psychiatry. 2008;13(1):90–98. doi:10.1038/sj.mp.4002016
105. Recommendations | autism spectrum disorder in under 19s: support and management | guidance | NICE. Available from: https://www.nice.org.uk/guidance/cg170/chapter/Recommendations.
106. Gringras P, Gamble C, Jones AP, et al. Melatonin for sleep problems in children with neurodevelopmental disorders: randomised double masked placebo controlled trial. BMJ. 2012;345(nov05 1):e6664. doi:10.1136/bmj.e6664
107. Buckley AW, Hirtz D, Oskoui M, et al. Practice guideline: treatment for insomnia and disrupted sleep behavior in children and adolescents with autism spectrum disorder: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2020;94(9):392–404. doi:10.1212/WNL.0000000000009033
108. Howes OD, Rogdaki M, Findon JL, et al. Autism spectrum disorder: consensus guidelines on assessment, treatment and research from the British Association for Psychopharmacology. J Psychopharmacol. 2018;32(1):3–29. doi:10.1177/0269881117741766
109. Rasmussen L, Bilenberg N, Thomsen Ernst M, Abitz Boysen S, Pottegård A. Use of Psychotropic Drugs among Children and Adolescents with Autism Spectrum Disorders in Denmark: a Nationwide Drug Utilization Study. J Clin Med. 2018;7(10):339. doi:10.3390/jcm7100339
110. Parvataneni T, Srinivas S, Shah K, Patel RS. Perspective on Melatonin Use for Sleep Problems in Autism and Attention-Deficit Hyperactivity Disorder: a Systematic Review of Randomized Clinical Trials. Cureus. 2014;12(5):e8335. doi:10.7759/cureus.8335
111. Rzepka-Migut B, Paprocka J. Efficacy and Safety of Melatonin Treatment in Children with Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder—A Review of the Literature. Brain Sci. 2020;10(4):219. doi:10.3390/brainsci10040219
112. Abramova R, Campbell P, Baron J, Patel K, Parmar S. Review of Melatonin Supplementation for Sleep Disorders in Pediatric Special Populations. J Pharm Pract. 2020;33(4):533–539. doi:10.1177/0897190019845982
113. Abdelgadir IS, Gordon MA, Akobeng AK. Melatonin for the management of sleep problems in children with neurodevelopmental disorders: a systematic review and meta-analysis. Arch Dis Child. 2018;103(12):1155–1162. doi:10.1136/archdischild-2017-314181
114. Schroder CM, Malow BA, Maras A, et al. Pediatric Prolonged-Release Melatonin for Sleep in Children with Autism Spectrum Disorder: impact on Child Behavior and Caregiver’s Quality of Life. J Autism Dev Disord. 2019;49(8):3218–3230. doi:10.1007/s10803-019-04046-5
115. Waldron AY, Spark MJ, Dennis CM. The Use of Melatonin by Children: parents’ Perspectives. J Clin Sleep Med. 2014;12(10):1395–1401. doi:10.5664/jcsm.6198
116. Breik N, Kuo I, Bugden S, Moffat M, Alessi-Severini S. Treating Children with ASD: the Perspective of Caregivers. J Pharm Pharm Sci. 2018;21(1s):74s–87s. doi:10.18433/jpps29829
117. Maras A, Schroder CM, Malow BA, et al. Long-term efficacy and safety of pediatric prolonged-release melatonin for insomnia in children with autism spectrum disorder. J Child Adolesc Psychopharmacol. 2018;28(10):699–710. doi:10.1089/cap.2018.0020
118. Roenneberg T, Kuehnle T, Juda M, et al. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11(6):429–438. doi:10.1016/j.smrv.2007.07.005
119. Dement W, Guilleminault C, Zarcone V. The pathologies of sleep: a case series approach. Nerv Syst. 1975;2:501–518.
120. Paine SJ, Fink J, Gander PH, Warman GR. Identifying advanced and delayed sleep phase disorders in the general population: a national survey of New Zealand adults. Chronobiol Int. 2014;31(5):627–636. doi:10.3109/07420528.2014.885036
121. Nesbitt AD. Delayed sleep-wake phase disorder. J Thorac Dis. 2018;10(Suppl 1):S103–S111. doi:10.21037/jtd.2018.01.11
122. Sivertsen B, Pallesen S, Stormark KM, Bøe T, Lundervold AJ, Hysing M. Delayed sleep phase syndrome in adolescents: prevalence and correlates in a large population based study. BMC Public Health. 2013;13:1163. doi:10.1186/1471-2458-13-1163
123. LeBlanc JC, Morehouse R, Rajda M, et al. Prevalence of delayed sleep phase syndrome in adolescents: a school-based survey. Pediatr Res. 1999;45(7):5. doi:10.1203/00006450-199904020-00035
124. Sivertsen B, Harvey AG, Pallesen S, Hysing M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J Sleep Res. 2015;24(1):11–18. doi:10.1111/jsr.12254
125. Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135(4):e994–1001. doi:10.1542/peds.2014-3482
126. Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43(2):434–442. doi:10.1093/ije/dyt261
127. Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 2009;48(9):894–908. doi:10.1097/CHI.0b013e3181ac09c9
128. Konofal E, Lecendreux M, Cortese S. Sleep and ADHD. Sleep Med. 2010;11(7):652–658. doi:10.1016/j.sleep.2010.02.012
129. Konofal E, Lecendreux M, Deron J, et al. Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatr Neurol. 2008;38(1):20–26. doi:10.1016/j.pediatrneurol.2007.08.014
130. Van der Heijden KB, Smits MG, Van Someren EJW, Gunning WB. Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: a circadian rhythm sleep disorder. Chronobiol Int. 2005;22(3):559–570. doi:10.1081/CBI-200062410
131. Auger RR, Burgess HJ, Emens JS, Deriy LV, Thomas SM, Sharkey KM. Clinical Practice Guideline for the Treatment of Intrinsic Circadian Rhythm Sleep-Wake Disorders: advanced Sleep-Wake Phase Disorder (ASWPD), Delayed Sleep-Wake Phase Disorder (DSWPD), Non-24-Hour Sleep-Wake Rhythm Disorder (N24SWD), and Irregular Sleep-Wake Rhythm Disorder (ISWRD). An Update for 2015: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med JCSM off Publ Am Acad Sleep Med. 2015;11(10):1199–1236. doi:10.5664/jcsm.5100
132. Quera-Salva MA, Kilic-Huck U, Vecchierini MF. La mélatonine et son usage dans les troubles circadiens du rythme veille sommeil: recommandations de la société française de recherche et de médecine du sommeil (SFRMS). Médecine Sommeil. 2021;18(2):55–69. doi:10.1016/j.msom.2021.04.002
133. Mundey K, Benloucif S, Harsanyi K, Dubocovich ML, Zee PC. Phase-dependent treatment of delayed sleep phase syndrome with melatonin. Sleep. 2005;28(10):1271–1278. doi:10.1093/sleep/28.10.1271
134. Van der Heijden KB, Smits MG, Van Someren EJW, Ridderinkhof KR, Gunning WB. Effect of melatonin on sleep, behavior, and cognition in ADHD and chronic sleep-onset insomnia. J Am Acad Child Adolesc Psychiatry. 2007;46(2):233–241. doi:10.1097/01.chi.0000246055.76167.0d
135. Weiss MD, Wasdell MB, Bomben MM, Rea KJ, Freeman RD. Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. J Am Acad Child Adolesc Psychiatry. 2006;45(5):512–519. doi:10.1097/01chi.0000205706.78818.ef
136. Mohammadi MR, Mostafavi SA, Keshavarz SA, et al. Melatonin Effects in Methylphenidate Treated Children with Attention Deficit Hyperactivity Disorder: a Randomized Double Blind Clinical Trial. Iran J Psychiatry. 2012;7(2):87–92.
137. Goldman RD, Bongiorno PB, Olcese JM, Witt-Enderby PA, Shatkin JP. Myths and Evidence Regarding Melatonin Supplementation for Occasional Sleeplessness in the Pediatric Population. Pediatr Ann. 2021;50(9):e391–e395. doi:10.3928/19382359-20210823-01
138. Schröder CM, Broquère MA, Claustrat B, et al. Approches thérapeutiques des troubles du sommeil et des rythmes chez l’enfant avec TSA. L’Encéphale. 2022:S0013700621002177. doi:10.1016/j.encep.2021.08.005
139. Zisapel N. Melatonin and sleep. Open Neuroendocrinol J. 2010;3:85–95.
140. Wasdell MB, Jan JE, Bomben MM, et al. A randomized, placebo-controlled trial of controlled release melatonin treatment of delayed sleep phase syndrome and impaired sleep maintenance in children with neurodevelopmental disabilities. J Pineal Res. 2008;44(1):57–64. doi:10.1111/j.1600-079X.2007.00528.x
141. Appleton RE, Jones AP, Gamble C, et al. The use of MElatonin in children with neurodevelopmental disorders and impaired sleep: a randomised, double-blind, placebo-controlled, parallel study (MENDS). Health Technol Assess Winch Engl. 2012;16(40):i–239.
142. Chang TK, Chen J, Yang G, Yeung EY. Inhibition of procarcinogen‐bioactivating human CYP1A1, CYP1A2 and CYP1B1 enzymes by melatonin. J Pineal Res. 2010;48(1):55–64. doi:10.1111/j.1600-079X.2009.00724.x
143. Buckley AW, Hirtz D, Oskoui M, et al. Practice guideline: treatment for insomnia and disrupted sleep behavior in children and adolescents with autism spectrum disorder: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2020;94(9):392–404. doi:10.1212/WNL.0000000000009033
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
