Back to Journals » ClinicoEconomics and Outcomes Research » Volume 14
Medication Adherence and Healthcare Utilization in Relapsing-Remitting Multiple Sclerosis Patients Using Teriflunomide
Authors Greene N, Higuchi K, Bognar K , Chang E , Broder MS
Received 30 July 2022
Accepted for publication 15 December 2022
Published 22 December 2022 Volume 2022:14 Pages 755—761
DOI https://doi.org/10.2147/CEOR.S383934
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Nupur Greene,1 Keiko Higuchi,1 Katalin Bognar,2 Eunice Chang,2 Michael S Broder2
1Neurology & Immunology (N&I), Sanofi, Cambridge, MA, USA; 2Real World Evidence, PHAR (Partnership for Health Analytic Research), Beverly Hills, CA, USA
Correspondence: Nupur Greene, Global HEVA Business Partner, N&I, Sanofi, 450 Water Street, Cambridge, MA, USA, Tel +1 857 259 0037, Email [email protected]
Purpose: Multiple sclerosis (MS) is a costly, immune-mediated disease of the central nervous system. Most patients have relapsing-remitting MS (RRMS) for which disease-modifying therapies (DMTs) provide an effective treatment option by reducing relapse rates. However, adherence to DMTs is suboptimal. This study examines the association between adherence to teriflunomide and clinical and healthcare utilization outcomes.
Patients and Methods: Patients with RRMS who started treatment with teriflunomide between 1/1/2018 and 12/31/2019 were analyzed using IQVIA PharMetrics® Plus data. RRMS patients were identified via diagnosis codes and treatment types; the first prescription date for teriflunomide was the index date. Highly and poorly adherent patients were identified based on the proportion of days covered (PDC) post-index (PDC ≥ 0.8 and PDC ≤ 0.5, respectively). Patient demographics, clinical characteristics, healthcare utilization during the year pre- and post-index, and relapse rate post-index were reported descriptively. Outcomes were compared between highly and poorly adherent patients through logistic regression. Models were adjusted for demographics, comorbidities, and utilization measures during the baseline period.
Results: Among the 922 RRMS patients identified, 534 (57.9%) were highly adherent to teriflunomide, while 249 (27.0%) had PDC ≤ 0.5. The two groups were not statistically different in terms of demographic characteristics and comorbidities; however, poorly adherent patients were more likely to have emergency department (ED) or inpatient visits during baseline (36.9% versus 26.8%, P=0.004; 17.3% versus 10.9%, P=0.013, respectively). Unadjusted results suggested lower likelihood of both relapses and utilization during follow-up among highly adherent patients compared to poorly adherent patients. Adjusted results confirmed that high adherence was associated with decreased likelihood of post-index relapses, ED utilization, and inpatient utilization (OR [95% CI]: 0.55 [0.39– 0.76], 0.49 [0.34– 0.71], and 0.51 [0.27– 0.97], respectively) even after controlling for baseline utilization.
Conclusion: High adherence to teriflunomide was found to be associated with fewer relapses and lower healthcare utilization among patients with RRMS.
Keywords: administrative claims analysis, disease modifying therapies, medication compliance, percent of days covered
Introduction
Multiple sclerosis (MS) is a costly, immune-mediated disease of the central nervous system, with the mean total healthcare costs ranging from $8528 to $54,244 annually per patient.1 Of the estimated one million people affected by MS in the US, approximately 85% have the relapsing-remitting (RR) MS subtype, characterized by relapse events followed by partial or complete remission without disease progression during remission.2–4
Disease modifying therapies (DMTs) are the cornerstone of treatment for RRMS and various oral (fingolimod, teriflunomide, dimethyl fumarate, siponimod, cladribine), injectable (interferon and glatiramer acetate), and intravenous (natalizumab, ocrelizumab, alemtuzumab, and rituximab) options are available for patients in the US.5
There is existing evidence of suboptimal adherence to oral DMTs in MS – indicated by mean proportion of days covered (PDC) and medical possession rates (MPR), as well as by binary measures. Particularly, recent systematic reviews by Mardan et al and Nicholas et al found a wide range (61–90%) of patients taking oral DMTs with PDC ≥0.8.6,7
Several studies document that increased adherence to DMTs as a class is associated with reduced relapse rates, slower RRMS disease progression, and lower healthcare costs,8–10 possibly allowing patients to optimally benefit from DMTs’ efficacy. These studies, however, are several years old, and as new therapies are introduced, clinicians may modify their prescribing practices to accommodate new agents or new knowledge about older ones.
Teriflunomide, an oral pyrimidine synthesis inhibitor indicated for the treatment of adults with relapsing forms of MS, was approved by the FDA in 2012 as a once-a-day oral treatment. At this point in the history of its use, practices for teriflunomide use may have stabilized beyond what was observed in earlier studies. Insurance claims are well suited to studying the link between prescription fill behavior and outcomes as these data allow observations over relatively long periods with complete data on healthcare utilization.
The objective of this study was to examine association of high adherence and clinical outcome and healthcare utilization for patients initiating teriflunomide in a contemporary insurance claims data set. Specifically, we compared outcomes across RRMS patients initiating teriflunomide who are adherent to treatment to patients who are non-adherent.
Materials and Methods
This was a retrospective, longitudinal cohort study using the administrative claims data from IQVIA PharMetrics® Plus for years 2017–2020. IQVIA databases are administrative claims databases that comprise de-identified adjudicated pharmacy claims (eg, outpatient prescriptions) and medical claims (eg, inpatient and outpatient services) submitted for payment by providers, healthcare facilities, and pharmacies, as well as member enrollment and benefit, patient, provider, and hospital demographic information. IQVIA databases are Health Insurance Portability and Accountability Act compliant and thus consistent with 45 CFR 46.101(b)(4) and exempt from Institutional Review Board oversight.
The overall study population included adult patients (≥18 years) with RRMS who were newly treated with teriflunomide, during the identification (ID) period from January 01, 2018 to December 31, 2019. As no specific ICD-10 diagnosis code exists for RRMS, a validated claims-based algorithm was used to identify patients with the condition (positive predictive value of 95%).11 Patients with MS without evidence of disease progression were defined as RRMS patients. Disease progression was identified by observing use of specific medications.11 Specifically, patients were considered to have RRMS if they had (i) ≥1 claim for teriflunomide at any time during the ID period with a 1-year washout period with no teriflunomide use (the first fill of index treatment was defined as the index date), and (ii) ≥1 medical claim for MS (International Classification of Disease, 10th Revision, Clinical Modification [ICD-10-CM] codes: G35.xx) prior to or on the index date, and (iii) no use of medications commonly used for progressive disease (mitoxantrone, cyclophosphamide, or methotrexate) at any time during the study period. Additionally, patients were required to have continuous medical and pharmacy enrollment during the 1 year prior to (pre-index period) and 1 year after (post-index period) the index date and were at least 18 years old at the index date. Study schema is presented in Figure 1.
 |
Figure 1 Study design diagram. |
Among patients who met inclusion criteria, adherence to teriflunomide during the follow-up period was measured as PDC. PDC is a preferred method of measuring medication adherence and was calculated by the number of days that a patient had medication available divided by days of post-index period.12–15 Patients were grouped into high adherence (PDC ≥0.8) and low adherence cohorts (PDC ≤0.5). Patients not in the high or low adherence groups (0.5<0.8) were excluded.
Demographic characteristics were measured in the baseline period. To assess disease severity at baseline, we calculated Expanded Disability Status Scale (EDSS) using a claims-based algorithm.16 Kurtzke Functional System Scores (KFSS) were generated based on ICD-10-CM codes, then mapped to an EDSS score. We measured comorbidities in several ways, including the Charlson Comorbidity Index (CCI) and examining specific MS-related and autoimmune disease-related comorbidities of interest. Additionally, we summarized healthcare utilization in the baseline period. Given that the follow-up period intersected with the COVID-19 pandemic, we tracked the number of pandemic months during the patient’s follow-up period, using April 01, 2020 as the start of the pandemic.
The primary outcomes were relapse rate and healthcare utilization (inpatient and emergency department [ED] visits) during follow-up. Relapses were determined from administrative claims data according to an algorithm used and validated in the literature17–19 requiring either (i) an inpatient visit with a primary diagnosis of MS or (ii) an outpatient visit with a diagnosis of MS and oral or intravenous corticosteroid use within 7 days of the outpatient visit. This algorithm was found to have a positive predictive value of 67.3%.19
Descriptive statistics including means, standard deviations (SD), and relative frequencies and percentages were reported for continuous and categorical data. In addition to descriptive analyses, modeling was performed to control for differences in observed characteristics between adherent and non-adherent patients that may confound the findings. Logistic regression models were conducted to estimate the likelihood of post-index relapses, ED visits, and inpatient visits. All models were adjusted for the following: age group, gender, region, baseline EDSS, baseline comorbidities, and baseline healthcare utilization. Odds ratio (OR) and 95% confidence intervals (CI), as well as adjusted rates and 95% CI, were reported for the logistic regression model.
All data transformations and statistical analyses were performed using SAS© version 9.4.
Results
Among the 922 patients with RRMS initiating teriflunomide who were identified and met the study criteria, 534 (57.9%) were highly adherent to the medication (PDC ≥0.8) and 249 (27.0%) were poorly adherent to the medication (PDC ≤0.5). The remaining 139 patients with intermediate adherence were removed from the analysis. Table 1 provides baseline characteristics for the study cohort. The mean age of highly adherent patients was 48.8 years versus 47.5 years for poorly adherent patients (P=0.085). The rate of females (78.5% versus 80.7%, P=0.469), as well as the geographic distribution of patients (P=0.175) were similar among highly and poorly adherent patients. Baseline disability and comorbidities were not statistically different between the two groups. The mean baseline EDSS score among highly adherent patients was 2.5, while the same measure among poorly adherent patients was 2.8 (P=0.254). The mean CCI was 0.7 in both groups (P=0.856), while the mean number of chronic conditions was 4.2 and 4.4 in the high and low adherence groups, respectively (P=0.151). Moreover, the prevalence of a wide range of MS and autoimmune related comorbidities were not statistically different between the two groups. Poorly adherent patients were more likely to have ED and inpatient visits at baseline than highly adherent patients (36.9% versus 26.8%, P=0.004 and 17.3% versus 10.9%, P=0.013, respectively).
 |
Table 1 Baseline Patient Characteristics and Utilization |
During the 1-year follow-up period, highly adherent patients were less likely to have relapses than patients with low adherence (28.5% versus 42.6%, P<0.001), while there was no statistical difference between the two groups in terms of likelihood of severe infection and EDSS scores. In terms of healthcare utilization, highly adherent patients were less likely to have either ED or inpatient visits during follow-up (17.2% versus 31.3%, P<0.001, and 4.5% versus 8.4%, P=0.027, respectively) (Table 2). The association between adherence and outcomes remained after adjusting for potential confounders, particularly baseline utilization. The logistic model showed that high adherence was associated with decreased likelihood of post-index relapses, ED visits, and inpatient hospitalization (OR [95% CI]: 0.55 [0.39–0.76], 0.49 [0.34–0.71], and 0.51 [0.27–0.97], respectively) even after controlling for baseline utilization (Table 3). The adjusted probability of relapse was 27.5% for highly adherent and 40.9% for poorly adherent patients. The adjusted likelihood of ED and inpatient visits was about twice as much for poorly adherent RRMS patients than for highly adherent patients (28.1% versus 16.0% and 6.7% versus 3.6%, respectively) (Figure 2).
 |
Table 2 Post-Index Measures (Unadjusted) |
 |
Table 3 Results of Logistic Regression Models |
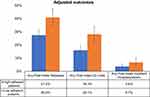 |
Figure 2 Adjusted outcomes. |
Discussion
In this study of commercially insured patients with RRMS initiating teriflunomide, we found that high adherence to teriflunomide (PDC ≥0.8) was associated with significantly better patient outcomes and lower healthcare utilization, with a decreased likelihood of relapses and ED or inpatient visits. Highly adherent patients were about 45% less likely to have a relapse, and about 50% less likely to have inpatient hospitalization or ED visits than patients in the low adherence cohort.
Our findings suggest that improving adherence to teriflunomide in patients with RRMS may lead to better health outcomes as well as decreased utilization of healthcare resources. In particular, if 100 poorly adherent patients were instead highly adherent, roughly 13 relapses and 12 ED visits may be avoided in the first year after initiation. We recognize that inherent differences between the study’s non-randomized comparator groups may lead to differences in relapse rate and utilization. For example, highly adherent patients may be healthier or less likely to go to the emergency department than poorly adherent patients. To minimize the effect of such confounding factors, we performed multivariable analyses using various controls for disease severity and adjusting for baseline healthcare utilization. We also utilized a novel claims-based algorithm16 to create a proxy measurement for EDSS, a measure commonly used in clinical settings to assess disability in MS, thus allowing us to control for severity of disease in addition to the standard comorbidity measures.
Several studies have established links between adherence and patient outcomes and utilization. In contrast to our study, these studies are mostly based on older data, consider class-level associations, and may not have adequately controlled for disability.8–10 However, their results are similar to what was found in this study. Particularly, Burks et al10 found that patients with MS who are highly adherent to DMTs are about 42% less likely to have relapses during the year post-index and about 52% and 38% less likely to have hospital and ER visits, respectively, compared to poorly adherent patients. Yermakov et al8 found qualitatively similar results in that higher adherence is associated with fewer relapses and lower healthcare resource utilization; however, they report change in outcomes associated with a 10% increase in adherence so quantitative comparison of results is difficult. Finally, Tan et al9 used significantly older data and focused on earlier available treatments. They found that high adherence is associated with better outcomes, but the magnitude of the effects was smaller than ones reported in this study.
Limitations
In order to provide updated information on adherence and outcomes in RRMS, we used the most recent years of data available. This presented a potential challenge in that the COVID-19 pandemic may have impacted patient behavior and healthcare utilization. We searched for, but did not find, a statistically significant interaction between COVID-19 and risk of relapse, ED visits, or hospitalization in our data. Our results were limited by the short duration of the pandemic period in our data. Repeating our analysis with additional data as it becomes available would provide needed insight on the burden faced by patients with MS during the pandemic, as well as further characterizing treatment patterns. Additionally, this study was a retrospective, observational analysis using large administrative claims data. These data lack important clinical details, including disease severity and symptoms, which prevented us from using such details to determine if a patient has RRMS. However, we used a validated algorithm to identify these patients. Additionally, when analyzing administrative claims data, direct information on whether medications are taken as prescribed is not available, thus we relied instead on medication fills. Moreover, most medications administered in hospitals are not captured in claims.
Our data only allow us to report on the association between adherence and outcomes rather than on causality. It is conceivable that patients with progressive disease and worse health outcomes would stop taking medication. Finally, this study is limited to patients with commercial and Medicare supplemental insurance. Results may not be generalizable to other populations.
Conclusion
Our study further confirmed that adherence to DMTs among RRMS patients is suboptimal despite evidence showing that high adherence is associated with better outcomes and lower healthcare utilization. Increased adherence to DMT is necessary to improve patient outcomes. Our study may inform decisions on selecting interventions to improve adherence to treatment for RRMS patients.
Acknowledgments
Medical writing support was provided by Marian H. Tarbox of PHAR (Partnership for Health Analytic Research) and funded by Sanofi.
Funding
The study was funded by Sanofi.
Disclosure
NG and KH are full-time employees of Sanofi and may own stock or stock options. KB, EC, and MSB are employees of PHAR (Partnership for Health Analytic Research), a health services company paid by Sanofi to conduct the research reported in this manuscript and by Akcea, Amgen, BioMarin Pharmaceuticals, BMS, Dompe, Eisai, Genentech, Gilead, Mirum Pharmaceuticals, Novartis, Otsuka, Prothena, Regeneron, and Takeda Pharmaceuticals for work related to the work described in the manuscript.
References
1. Adelman G, Rane SG, Villa KF. The cost burden of multiple sclerosis in the United States: a systematic review of the literature. J Med Econ. 2013;16(5):639–647. doi:10.3111/13696998.2013.778268
2. Wallin MT, Culpepper WJ, Campbell JD, et al. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029–e1040. doi:10.1212/WNL.0000000000007035
3. Lublin FD, Reingold SC, Cohen JA, et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014;83(3):278–286. doi:10.1212/WNL.0000000000000560
4. Vukusic S, Confavreux C. Prognostic factors for progression of disability in the secondary progressive phase of multiple sclerosis. J Neurol Sci. 2003;206(2):135–137. doi:10.1016/s0022-510x(02)00426-4
5. Saleem S, Anwar A, Fayyaz M, Anwer F, Anwar F. An overview of therapeutic options in relapsing-remitting multiple sclerosis. Cureus. 2019. doi:10.7759/cureus.5246
6. Mardan J, Hussain MA, Allan M, Grech LB. Objective medication adherence and persistence in people with multiple sclerosis: a systematic review, meta-analysis, and meta-regression. JMCP. 2021;27(9):1273–1295. doi:10.18553/jmcp.2021.27.9.1273
7. Nicholas JA, Edwards NC, Edwards RA, Dellarole A, Grosso M, Phillips AL. Real-world adherence to, and persistence with, once- and twice-daily oral disease-modifying drugs in patients with multiple sclerosis: a systematic review and meta-analysis. BMC Neurol. 2020;20(1):281. doi:10.1186/s12883-020-01830-0
8. Yermakov S, Davis M, Calnan M, et al. Impact of increasing adherence to disease-modifying therapies on healthcare resource utilization and direct medical and indirect work loss costs for patients with multiple sclerosis. J Med Econ. 2015;18(9):711–720. doi:10.3111/13696998.2015.1044276
9. Tan H, Cai Q, Agarwal S, Stephenson JJ, Kamat S. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv Ther. 2011;28(1):51–61. doi:10.1007/s12325-010-0093-7
10. Burks J, Marshall T, Ye X. Adherence to disease-modifying therapies and its impact on relapse, health resource utilization, and costs among patients with multiple sclerosis. Clinicoecon Outcomes Res. 2017;9:251–260. doi:10.2147/CEOR.S130334
11. Van Le H, Le Truong CT, Kamauu AWC, et al. Identifying patients with relapsing-remitting multiple sclerosis using algorithms applied to US integrated delivery network healthcare data. Value Health. 2019;22(1):77–84. doi:10.1016/j.jval.2018.06.014
12. Peterson AM, Nau DP, Cramer JA, Benner J, Gwadry-Sridhar F, Nichol M. A checklist for medication compliance and persistence studies using retrospective databases. Value Health. 2007;10(1):3–12. doi:10.1111/j.1524-4733.2006.00139.x
13. Nau D. Proportion of Days Covered (PDC) as a preferred method of measuring medication adherence. Pharma Qual Allian. 2012;6:25.
14. Pharmacy Quality Alliance. Adherence. Pharmacy Quality Alliance; 2022. Avialable from: https://www.pqaalliance.org/adherence-measures.
15. Centers for Medicare & Medicaid Services. Health Insurance Exchange: 2020 Quality Rating System Measure Technical Specifications. Centers for Medicare & Medicaid Services; 2019:201–206. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/Downloads/2020-QRS-Measure-Tech-Specs_20190925_508.pdf.
16. Truong CTL, Le HV, Kamauu AW, et al. Creating a real-world data, United States healthcare claims-based adaptation of kurtzke functional systems scores for assessing multiple sclerosis severity and progression. Adv Ther. 2021;38(9):4786–4797. doi:10.1007/s12325-021-01858-9
17. Ollendorf DA, Jilinskaia E, Oleen-Burkey M. Clinical and economic impact of glatiramer acetate versus beta interferon therapy among patients with multiple sclerosis in a managed care population. J Manag Care Pharm. 2002;8(6):469–476. doi:10.18553/jmcp.2002.8.6.469
18. Capkun-Niggli G, Lahoz R, Verdun E, et al. Medical and pharmacy claims-based algorithms for identifying relapses in patients with multiple sclerosis. Value Health. 2013;16(7):A582. doi:10.1016/j.jval.2013.08.1596
19. Chastek BJ, Oleen-Burkey M, Lopez-Bresnahan MV. Medical chart validation of an algorithm for identifying multiple sclerosis relapse in healthcare claims. J Med Econ. 2010;13(4):618–625. doi:10.3111/13696998.2010.523670
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
