Back to Journals » Psychology Research and Behavior Management » Volume 16
Mediating Role of Depression Between Diabetes Management Self-Efficacy and Diabetes Self-Care Behavior Among Elderly Type 2 Diabetes Mellitus Patients in China
Authors Jiang R, Ta X, Xu M, Luo Z, Du Y, Zhong X, Pan T, Cao X
Received 9 November 2022
Accepted for publication 5 April 2023
Published 28 April 2023 Volume 2023:16 Pages 1545—1555
DOI https://doi.org/10.2147/PRBM.S396916
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mei-Chun Cheung
Ruobing Jiang,1,* Xin Ta,1,* Min Xu,2 Zhihua Luo,3 Yijun Du,4 Xing Zhong,4 Tianrong Pan,4 Xiujing Cao1
1Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, Anhui, People’s Republic of China; 2Department of Endocrinology, First Affiliated Hospital, Anhui Medical University, Hefei, Anhui, People’s Republic of China; 3Department of Pediatrics, First Affiliated Hospital, Anhui Medical University, Hefei, Anhui, People’s Republic of China; 4Department of Endocrinology, Second Affiliated Hospital, Anhui Medical University, Hefei, Anhui, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiujing Cao, Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, Anhui, People’s Republic of China, Email [email protected] Tianrong Pan, Department of Endocrinology, Second Affiliated Hospital, Anhui Medical University, Hefei, Anhui, People’s Republic of China, Email [email protected]
Objective: To investigate the current status of diabetes self-care behavior and the association between depression, self-efficacy and self-care in a sample of Chinese elderly type 2 diabetes mellitus (T2DM) patients.
Methods: A cross-sectional study with a convenient sample including 240 elderly T2DM patients collected the data of demographic characteristics, diabetes self-care behavior, self-efficacy and depression status. The difference of self-care behavior in different sample characteristics was compared by independent t-test. The Personal correlation analysis was employed to examine the correlation of study variables. The method of bootstrap was used to analyze mediating role of depression.
Results: Only 22.5% of patients reported better diabetes self-care behavior and depression partly mediated the association between self-efficacy and self-care behavior. The significant coefficient of path a (B = − 0.052, p < 0.001) and path b (B = − 0.423, p < 0.05) indicated negative associations of self-efficacy on depression, and depression on self-care behavior. The indirect effect (Path a × b) between self-efficacy and self-care behavior through depression was significant (B = 0.022, p < 0.05), the 95% bias-corrected bootstrap confidence interval was 0.004 to 0.006. Meanwhile, the mediating role of depression was not found significant among the participants reported 60– 74 years old (B = 0.104, p < 0.001). But depression completely mediated this association among the participants reported 75– 89 years old (B = 0.034, p > 0.05).
Conclusion: The level of diabetes self-care behavior among the elderly T2DM patients in Dahu community of Anqing city was hardly optimistic. The self-efficacy focused intervention could be encouraged for community and clinicians to improve diabetes self-care behavior. Moreover, the prevalence of depression and T2DM is increasing in younger population. More work is needed to confirm these findings, especially conducting cohort studies on different populations.
Keywords: diabetes self-care behavior, the elderly, type 2 diabetes mellitus, diabetes management self-efficacy, depression
Introduction
International Diabetes Federation (IDF) Diabetes Atlas (Ninth edition) revealed a fact that 463 million people are suffering diabetes worldwide, of which, 116.4 million in China on the top of the ranking.1 With the acceleration of ageing of the population processing in China and the changes in people’s lifestyle and diet, the incidence of diabetes in the elderly shows a trend of rapid growth.2 A nationally representative cross-sectional survey has been used in China. From Chinese Geriatrics Society demonstrated the prevalence of diabetes in the elderly was more than 20% (90–95% elderly diabetes is T2DM), and this data will continue increase in the future, and the older patients have the higher incidence of diabetes complications and mortality.3 It not only has impact on physical and mental health of people but also incurs more serious public health problems, increasing the burden on people’s families and decreasing socioeconomic level.4,5
For T2DM patients, diabetes self-care is the cornerstone of diabetes management, and is identified as daily behaviors that patients perform to care their T2DM such as self-testing blood glucose, diet and exercise.6 Importantly, a large number of researches demonstrated that good diabetes self-care behavior independently predicted a better glycemic control, reducing or postponing complication and improving the quality of life.7–9 Although more and more studies focused on self-care behavior, in Chinese diabetes population especially in aged diabetes patients in community, there are limited studies concentrating on this issue and its influencing factors.6
An important factor accounting for poor diabetes self-care behavior is probably poor diabetes management self-efficacy.6 The concept of self-efficacy originated from the social cognitive theory which considered individual’s behaviors can be determined and influenced by their belief.10 Employed in the field of diabetes, self-efficacy, as a strong predictor of diabetes self-care behavior,11,12 is the belief of diabetics in the ability to achieve self-care activities. This relationship between them has been shown stable across racial/ethnic groups and across varying levels of health literacy.13 In addition, some of experimental studies documented that self-efficacy focused intervention programs are beneficial to improve diabetes self-care behavior.14,15 However, not all patients with good self-efficacy have good diabetes self-care behavior,16,17 which indicated some adverse factors may hinder the process from the belief of self-efficacy to achievement of self-care behavior.
Recently, the studies of psychological factors among T2DM patients are emerging.18,19 Depression, as a negative psychological factor, often co-occurs with diabetes. A meta-analysis identifying 42 studies revealed individuals with diabetes to be more than twice as likely to develop comorbid depression.20 In China, the prevalence of depression among T2DM patients was close to 50%, influencing their and family’s life severely.21 Some of studies suggested that depression has a direct impact on the index of diabetes self-care behavior,22,23 especially diet, exercise and glucose self-testing. A cross-sectional indicated that increased daily intake of vitamin B3 can reduce the risk of depression.24 Another study found that a high intake of other vegetables and fruits was a significant contributor to the reduced prevalence of T2DM.25 Diet has been shown to improve depressive symptoms and T2DM.26 Moreover, diabetes self-efficacy was demonstrated negatively associated with depression and the improvement of self-efficacy may reduce the depressive symptoms of patients.27 Nonetheless, there are no researches determining if depression mediated the relationship between self-efficacy and self-care behavior.
Taken together, this study will investigate the current status of diabetes self-care behavior and the mediating role of depression on the association between self-efficacy and self-care in a community sample of Chinese elderly T2DM patients. The following hypotheses are made.1. Self-efficacy was negatively correlated to depression. 2. Self-efficacy was positively correlated to self-care behavior. 3. The mediation effect of depression existed between self-efficacy and self-care behavior. It will be helpful to guide old patients to acquire perfect self-care behavior to achieve the goal of glycemic control and provide a valuable road for general practitioners to improve management and intervention efficiency.
Participants and Methods
Research Design
A cross-sectional study using face-to-face questionnaire was conducted in a community service center in Anqing City of Anhui province, China. Anqing is located in southeast China, Longitude: 117.054, Latitude: 30.5248. After preliminary investigation, the community has a sufficient sample population that meets the criteria and the community has good cooperation with this research group, which can ensure that the research is rigorous and smooth.
Participants
This study complies with the Declaration of Helsinki. Ethical approval was obtained from the institutional Ethics Committee at Anhui Medical University (ID:20190289) prior to the collection of data. All participants provided their written informed consent prior to responding to the survey. Two hundred and forty elderly T2DM patients managed by Dahu community service center in Anqing city of Anhui province were recruited into this study. The criteria of all participants includes: (1) age ≥60 years; (2) diabetes duration ≥1 years; (3) able to reading and writing Chinese and communicating effectively in Chinese; (4) meets WHO 1999 diagnostic criteria for diabetes. Participants were excluded when investigators found patients had severe psychotic illness, cognitive impairment and major complications that might influence their confidence and performance of diabetes self-care activities.
Data Collection
Data were collected from May to November, 2019 in Dahu community service center of Anqing city. The investigators are graduate students with some specialized knowledge. Before the survey, all investigators received training to ensure they absolutely understand the ideal of this survey and acquired investigation skill. After getting informed consent from participants, investigators released the questionnaire to participants who met the inclusion and exclusion criteria. Each person fills out the questionnaire in a separate room to ensure that they are not influenced by others. Any questions during the filling process will be explained by the researchers. Finally, 240 valid questionnaires were obtained.
Measurements
As a measuring tool, the questionnaire initially included general demographic questions such as age, gender (males and females), social economical status and so on. Age was divided into 60–74 years (young-old) and 75–89 years (old-old) groups.28 Otherwise, diabetes-related questions such as diabetes duration (continuous variable), personal monthly expenditure on diabetes and three major scales which measured diabetes self-care behaviors, diabetes management self-efficacy and depression were followed.
Diabetes Self-Care Behavior
The Summary of Diabetes of Self-care Activities (SDSCA) was developed by Toobert et al29 for diabetics over 60 years old. It was widely employed to assess diabetes self-care behavior in community-based old diabetics both in China and in the other countries.30–32 In this study, the Chinese version of scale consists of 11 items, measuring, respectively, 6 subdomains such as general diet (2 items), special diet (2 items), exercise (2 items), blood sugar testing (2 items), foot care (2 item), and medication taking (1 item). The score of every item ranging from 0 to 7 represents the number or average of days in a week for completing these activities. The possible total score was 0–77, with higher total score showing better level of self-care behaviors. According to scoring index = (actual score/highest possible score) × 100%, scoring index ≥60% is defined as better self-care behavior. Wan et al33 tested the reliability and validity of the scale, the overall Cronbach’s α was 0.84, the Cronbach’s α of 5 subscales was 0.71~0.93.
Diabetes Management Self-Efficacy
To evaluate diabetes management self-efficacy, this study used Chinese version of the Diabetes Management Self-efficacy Scale (C-DMSES) which translated from the 20-items Australia/English version DMSES by Shu-Fang Vivienne Wu (Cronbach’s alpha = 0.77 to 0.93).34 This measurement asks participants to recall their confidence in managing their blood glucose level, foot care, medication, diet, and level of physical activities. The possible total score is around 0–200 and a high score represents a high level of self-efficacy. According to scoring index = (actual score/highest possible score) × 100%, scoring index ≤40% is defined as low level of self-care behaviors, 40–80% is medium level, and ≥80% is high level. In this study, this scale exhibited high reliability (Cronbach’s alpha = 0.936).
Depression
The Patient Health Questionnaire-9 (PHQ-9) was widely employed to determine depression status by evaluating the frequency of occurrence of 8 symptoms in emotion and 1 symptom in suicide ideation among diabetics in China and in the other countries.35,36 It is a 9-items scale and the score of each item is 0–3. Therefore, the total score ranges from 0 to 27. The total score among 0–4 indicates no depression. The total score over 4 indicates having depressive symptoms. The Cronbach’s alpha is 0.783 in the present study.
Statistical Analysis
SPSS 23.0 (Statistical Product and Service Solutions, SPSS) was used to manage and analyze data. Firstly, each variable was described by mean (standard deviation) or number of cases (percentage). Secondly, the differences of self-care behavior in different demographic characteristics, diabetes-related information, diabetes management self-efficacy, depression were, respectively, compared by independent t-test. Then, the Pearson correlations analysis was employed to analyze the correlation among diabetes management self-efficacy, depression and diabetes self-care behavior. Finally, the method of Bootstrap using PROCESS macro in SPSS 23.0 recommended by Hayes37 was applied to test the mediation effect of depression between diabetes management self-efficacy and self-care behavior by using Model 4 in the way that the bias-corrected 95% confidence interval (CI) was calculated with 5000 bootstrapping re-samples. The Bootstrap 95% CI of indirect effect (Path a×b) without “0” indicted a significant mediation effect. Moreover, the mediating effect of depression also was tested respectively in different age groups. The study considered statistical significance at p-value <0.05 (two-tailed).
Results
The Characteristics of Participant
The demographic characteristics, diabetes-related characteristics, self-care behavior, self-efficacy, and depression of 240 older adults with T2DM are shown in Table 1. The mean age of participants was 73.76 years, ranged from 60 to 88 years old, with 108 (45.0%) male. Most participants were married (76.7%) and with having junior high school or above educational level (65.4%). There are 36 (15.0%) patients had a household monthly income <2000 yuan and 87 (36.3%) spend more than 400 yuan on diabetes monthly. The mean diabetes duration of the participants was 12.47 years and the mean BMI was 23.73. There are 54 (22.5%) patients had better self-care behavior and 89 (37.1%) had high level of self-efficacy. Nearly half of participants suffered from depression (46.7%).
 |
Table 1 Participants’ Demographic Characteristics, Diabetes-Related Characteristics, Self-Care Behavior, Self-Efficacy, and Depression (n = 240) |
Comparison of Participants’ Characteristics with Self-Care Behavior
As shown in Table 2, the significant differences were found among SDSCA total score such as marriage (p<0.05), education (p<0.01), personal monthly expenditure on diabetes (p<0.05), BMI (p<0.05), self-efficacy (p<0.001) and depression (p<0.001). Individuals who were married, had junior high school education or above, the BMI <24 and spend more than 200 yuan on diabetes monthly were more likely to have higher score of SDSCA total. In terms of the subscales of SDSCA, the participants among 75–89 years old presented higher score of general diet compared with the age of 60~74 (p<0.01). The male elderly participants reported higher score of exercise (p<0.05). The married participants reported higher score of exercise (p<0.01) and foot care (p<0.05). The household monthly income of participants >400 yuan was significantly relating to higher score of specific diet (p<0.05) and foot care (p<0.05). The participants who had a junior high school education or above were more likely to have higher score of exercise (p<0.001) and foot care (p<0.01). The participants who spend more than 200 yuan on diabetes monthly reported higher blood sugar testing score (p<0.05). The diabetes duration of participants >10 years was significantly relating to higher score of general diet (p<0.01) and medication taking (p<0.05). The participants who had a BMI <24 were more likely to have higher score of general diet (p<0.001). Moreover, the participants who reported high level of self-efficacy were more likely to have higher score of SDSCA total (p<0.001), general diet (p<0.001), exercise (p<0.001), foot care (p<0.001) and medication taking (p<0.001). The participants without depressive symptoms reported higher score of SDSCA total (p<0.001), general diet (p<0.01), exercise (p<0.001), and foot care (p<0.01).
 |
Table 2 Comparison of Participants’ Demographic and Diabetes-Related Characteristics with Self-Care Behavior |
Correlation Between Self-Efficacy, Depression and Self-Care Behavior
Table 3 provides the correlation between self-efficacy, depression and self-care behavior. Self-efficacy was negatively correlated to depression (p < 0.01), and correlation coefficient is −0.486. Self-efficacy was positively correlated to self-care behavior (r = 0.311, p < 0.01). Depression had a significantly negative relation to self-care behavior (r = −0.264, p < 0.01).
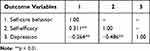 |
Table 3 Correlation Between Self-Efficacy, Depression and Self-Care Behavior |
The Mediation Effect of Depression Between Self-Efficacy and Self-Care Behavior
Table 4 shows the results of the mediation analysis. In the total participants, the total effect (path c) of self-efficacy on self-care behavior was significant (B = 0.095, p<0.001). The significant coefficient of path a (B = −0.052, p < 0.001) and path b (B = −0.423, p < 0.05) indicated negative associations of self-efficacy on depression, and depression on self-care behavior. The indirect effect (Path a×b) between self-efficacy and self-care behavior through depression was significant (B = 0.022, p < 0.05), and the 95% bias-corrected bootstrap confidence interval was 0.004 to 0.006. The path c’ was significant (B = 0.073, p < 0.001), which indicated that depression partly mediate the relationship between self-efficacy and self-care behavior. The significant coefficients are shown in Figure 1. However, the indirect effect was not significant among the participants reported 60–74 years old, the 95% bias-corrected bootstrap confidence interval was −0.036 to 0.015. Among the participants reported 75–89 years old, the path c’ was significant (B = 0.034, p > 0.05), which indicated that depression completely mediate the relationship between self-efficacy and self-care behavior.
 |
Table 4 The Mediation Effect of Depression Between Self-Efficacy and Self-Care Behaviors |
 |
Figure 1 Schematic model of depression as the mediator between self-efficacy and self-care behaviors. |
Discussion
This study evaluated the current status of diabetes self-care behavior and examined the mediating role of depression between diabetes management self-efficacy and self-care behavior among the elderly community T2DM patients in China.
The results revealed the level of diabetes self-care behavior was dissatisfied in this community. Only 22.5% of patients possessed better diabetes self-care behavior in this sample that included 240 elderly with T2DM. It is similar with the result of another recent study that 20.1% of diabetics reported having better diabetes self-care behavior in other communities in China.31 As bodily and social functions are increasingly decline, a lot of important factors have impact on diabetes self-care behavior.6 This study indicated individuals who are married, had junior high school education or above, had the BMI <24 and spend more than 200 yuan on diabetes monthly were more likely to have better diabetes self-care behavior. Moreover, this study found that the participants aged 75–89 had better general diet. The participants who have the diabetes duration >10 years was related to better general diet and medication taking. The reason may be related to the fact that the patients with the older age or longer diabetes duration had more knowledge and accumulated more experience about diabetes, which could promote self-care ability. Beyond that, we can see that the male elderly participants reported higher score of exercise and the higher household monthly income of participants was related to higher score of specific diet and foot care. Because the higher level of income indicated that greater capacity to obtain expensive food (such as milk and vegetables) and more time to manage daily life.
Social cognitive theory considered that individual’s belief of self-efficacy determines whether coping behavior will be initiated, how much effort will be expended, and how long it will be sustained in the face of obstacles and aversive experiences.11 Consistent with this assumption, the participants with higher self-efficacy also performed better self-care behavior, especially performing better general diet, exercise, foot care and medication taking in the present study, which was similar with the former research in China.38 Meanwhile, the Personal correlation analyses confirmed again that self-efficacy of the elderly T2DM patients is positively associated with diabetes self-care behavior.
Depression and diabetes are all serious chronic diseases and often co-occur, especially among the elderly. Diabetes-related depression is also a major complication of diabetes. However, the pathogenesis remains to be revealed. Recently, studies have revealed that hippocampal neuronal apoptosis, triggered by mitophagy via the abnormal Glu-GluR2-Parkin pathway, may be involved in the pathogenesis of diabetes-related depression.39 The elderly with DM experience always have greater risk for subsequent development or recurrence of depression, and conversely, the history of depression increases the risk for new onset DM.40 There is a two-way effect between diabetes and depression. Moreover, compared to T2DM patients without depression symptoms, the patients suffering depression indicated increasing risk of severe disease, more complications, treatment resistance and higher mortality.31 Meanwhile, those patients with depression performed poor self-care behavior.40 Consistent with previous articles,41,42 this study found that nearly half of participants suffered from depression and depression had negatively associated with diabetes management self-efficacy and self-care behavior.
In the context of diabetes self-care behavior, self-efficacy was mainly originated from positive emotion response.43 However, there are no researches to investigate the role of negative emotion symptoms on the relationship between diabetes management self-efficacy and diabetes self-care behavior. The result that mediation role of depression added evidence to demonstrate our hypothesis that depression may mediate the association between diabetes management self-efficacy and diabetes self-care behavior among the elderly T2DM patients. However, the mediating role of depression was not found significant among the participants reported 60–74 years old. Depression exclusively mediated this association among the participants aged 75–89.
This study, applying it to the elderly T2DM patients, is considering the role of depression on relationship between diabetes self-care behavior and self-efficacy. There are some limitations that should be emphasized in this study. Firstly, our sample came from one community which cannot represent the overall elderly population in China. The sample size is relatively small. An investigation with large sample size should be carrying out to better speculate the current situation of diabetes self-care behavior and understand the relationship among depression self-efficacy and self-care behavior. For example, communities in different areas are sampled for surveys. Study representativeness was increased on the basis of expanding sample sizes. Secondly, compared to longitudinal designs, this cross-sectional design cannot clearly draw the causal conclusions. We will continue to carry out longitudinal and intervention studies in the future. Finally, this study did not control all the confounding factors such as family history of diabetes, complications, family history of T2DM, or chemical exposure, age, gender, comorbidities, drug use and so on. In later studies, we should attach the importance of controlling of confounding factors and consider them as the covariates during investigation.
With the acceleration of ageing of the population process and the rapid development of primary health care in China, community is becoming a critical site that managing and intervening chronic disease for older adults.44 Therefore, it is of significant importance for the improvement of management and intervention focused on the elderly T2DM patients to investigate the current situation of diabetes self-care behavior and its influencing factors in community of China. Moreover, these findings can be helpful for community and clinicians to realize that strengthening diabetes management self-efficacy and controlling and relieving depressive symptom could improve self-care behavior among the elderly T2DM patients directly and indirectly, especially among adults aged 75–89. Community service center should both pay attention to the health outcome of the elderly T2DM patients and care their mental health.
Acknowledgments
The authors gave thanks to all participants in the study and the members of the survey teams. This study was supported by grants from Education Quality Engineering of Anhui Province (grant No.2020jyxm0614) and Basic and Clinical Cooperative Research Promotion Plan of Anhui Medical University (grant No. 2020xkjT035, 2021lcxk024). Ruobing Jiang and Xin Ta are co-first authors for this study. Xiujing Cao and Tianrong Pan are co-correspondence authors for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. International Diabetes Federation. IDF diabetes atlas, 9th ed. Int Diab Fed; 2019. Available from: http://www.diabetesatlas.org/.
2. Wang LM, Chen ZH, Zhang M, et al. Study of the prevalence and disease burden of chronic disease in the elderly in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:277–283. Chinese. doi:10.3760/cma.j.issn.0254-6450.2019.03.005
3. Geriatric Endocrinology and Metabolism Branch, Chinese Geriatrics Society. Expert consensus of the diagnosis and treatment measures for the Chinese elderly patients with type 2 diabetes (2018 edition). Chin J Intern. 2018;57(9):626–641. doi:10.3760/cma.j.issn.0578-1426.2018.09.004
4. Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–2523. doi:10.1001/jama.2017.7596
5. Jing Z, Chu J, Imam Syeda Z, et al. Catastrophic health expenditure among type 2 diabetes mellitus patients: a province-wide study in Shandong, China. J Diabetes Investig. 2019;10(2):283–289. doi:10.1111/jdi.12901
6. Luo X, Liu T, Yuan X, et al. Factors influencing self-management in Chinese adults with type 2 diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health. 2015;12(9):11304–11327. doi:10.3390/ijerph120911304
7. Al-Khawaldeh OA, Al-Hassan MA, Froelicher ES. Self-efficacy, self-management, and glycemic control in adults with type 2 diabetes mellitus. J Diabetes Complications. 2012;26(1):10–16. doi:10.1016/j.jdiacomp.2011.11.002
8. Walker RJ, Smalls BL, Egede LE. Social determinants of health in adults with type 2 diabetes-contribution of mutable and immutable factors. Diabetes Res Clin Pract. 2015;110:193–201. doi:10.1016/j.diabres.2015.09.007
9. Christensen NI, Drejer S, Burns K, Lundstrøm SL, Hempler NF, Qualitative A. Exploration of facilitators and barriers for diabetes self-management behaviors among persons with type 2 diabetes from a socially disadvantaged area. Patient Prefer Adherence. 2020;14:569–580. doi:10.2147/PPA.S237631
10. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi:10.1037//0033-295x.84.2.191
11. Saad AMJ, Younes ZMH, Ahmed H, Brown JA, Al Owesie RM, Hassoun AAK. Self-efficacy, self-care and glycemic control in Saudi Arabian patients with type 2 diabetes mellitus: a cross-sectional survey. Diabetes Res Clin Pract. 2018;137:28–36. doi:10.1016/j.diabres.2017.12.014
12. Noll AN, Glenn LL. Self-efficacy and management in type 2 diabetes mellitus. J Diabetes Complications. 2012;26:562;author reply 562–3. doi:10.1016/j.jdiacomp.2012.05.010
13. Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–829. doi:10.2337/diacare.29.04.06.dc05-1615
14. Jiang X, Wang J, Lu Y, Jiang H, Li M. Self-efficacy-focused education in persons with diabetes: a systematic review and meta-analysis. Psychol Res Behav Manag. 2019;12:67–79. doi:10.2147/PRBM.S192571
15. Sharoni SKA, Abdul Rahman H, Minhat HS, Shariff Ghazali S, Azman Ong MH. A self-efficacy education programme on foot self-care behaviour among older patients with diabetes in a public long-term care institution, Malaysia: a Quasi-experimental pilot study. BMJ Open. 2017;7:e014393. doi:10.1136/bmjopen-2016-014393
16. Gao J, Wang J, Zhu Y, Yu J. Validation of an information-motivation-behavioral skills model of self-care among Chinese adults with type 2 diabetes. BMC Public Health. 2013;13:100. doi:10.1186/1471-2458-13-100
17. Huang M, Zhao R, Li S, Jiang X, Barengo NC. Self-management behavior in patients with type 2 diabetes: a cross-sectional survey in western urban China. PLoS One. 2014;9(4):e95138. doi:10.1371/journal.pone.0095138
18. Yasui-Furukori N, Murakami H, Otaka H, et al. Coping behaviors and depressive status in individuals with type 2 diabetes mellitus. Ann Gen Psychiatry. 2019;18(1):11. doi:10.1186/s12991-019-0235-5
19. Salinero-Fort MA, Gómez-Campelo P, San Andrés-Rebollo FJ, et al. Prevalence of depression in patients with type 2 diabetes mellitus in Spain (the DIADEMA study): results from the MADIABETES cohort. BMJ Open. 2018;8(9):e020768. doi:10.1136/bmjopen-2017-020768
20. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–1078. doi:10.2337/diacare.24.6.1069
21. Sun N, Lou P, Shang Y, et al. Prevalence and determinants of depressive and anxiety symptoms in adults with type 2 diabetes in China: a cross-sectional study. BMJ Open. 2016;6:e012540. doi:10.1136/bmjopen-2016-012540
22. Lin K, Park C, Li M, et al. Effects of depression, diabetes distress, diabetes self-efficacy, and diabetes self-management on glycemic control among Chinese population with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2017;131:179–186. doi:10.1016/j.diabres.2017.03.013
23. Wu SF, Huang YC, Liang SY, Wang TJ, Lee MC, Tung HH. Relationships among depression, anxiety, self-care behaviour and diabetes education difficulties in patients with type-2 diabetes: a cross-sectional questionnaire survey. Int J Nurs Stud. 2011;48:1376–1383. doi:10.1016/j.ijnurstu.2011.04.008
24. Nguyen HD, Oh H, Kim M-S. Mixtures modeling identifies vitamin B1 and B3 intakes associated with depression. J Affect Disord. 2022;301:68–80. ISSN 0165-0327. doi:10.1016/j.jad.2021.12.133
25. Nguyen HD, Hojin O, Kim M-S. Higher intakes of nutrients are linked with a lower risk of cardiovascular diseases, type 2 diabetes mellitus, arthritis, and depression among Korean adults. Nutr Res. 2022;100:19–32. ISSN 0271-5317. doi:10.1016/j.nutres.2021.11.003
26. Duc H, Oh H, Yoon I, Kim M. Association between levels of thiamine intake, diabetes, cardiovascular diseases and depression in Korea: a national cross-sectional study. J Nutr Sci. 2021;10:E31. doi:10.1017/jns.2021.23
27. Wu SF, Huang YC, Lee MC, Wang TJ, Tung HH, Wu MP. Self-efficacy, self-care behavior, anxiety, and depression in Taiwanese with type 2 diabetes: a cross-sectional survey. Nurs Health Sci. 2013;15:213–219. doi:10.1111/nhs.12022
28. Cherry KE, Hawley KS, Jackson EM, Volaufova J, Su LJ, Jazwinski SM. Pictorial superiority effects in oldest-old people. Memory. 2008;16:728–741. doi:10.1080/09658210802215534
29. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi:10.2337/diacare.23.7.943
30. Markle-Reid M, Ploeg J, Fraser KD, et al. Community program improves quality of life and self-management in older adults with diabetes mellitus and comorbidity. J Am Geriatr Soc. 2018;66(2):263–273. doi:10.1111/jgs.15173
31. Zhang XX, Wu SY, Mang YNE, et al. Association between social support and self-management behaviors among patients with diabetes in community. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49:455–461. doi:10.3969/j.issn.1671-167X.2017.03.014
32. Cheng L, Leung DYP, Wu YN, Sit JWH, Yang MY, Li XM. Psychometric properties of the modified personal diabetes questionnaire among Chinese patients with type 2 diabetes. Eval Health Prof. 2018;41:3–24. doi:10.1177/0163278716664393
33. Wan Q, Shang S, Lai X, et al. Letter and validity study of self-management behavior scale for patients with type 2 diabetes mellitus. Chin J Pract Nurs. 2008;24(3):26–27.
34. Vivienne Wu SF, Courtney M, Edwards H, McDowell J, Shortridge-Baggett LM, Chang PJ. Development and validation of the Chinese version of the diabetes management self-efficacy scale. Int J Nurs Stud. 2008;45(4):534–542. doi:10.1016/j.ijnurstu.2006.08.020
35. Jia Z, Li X, Yuan X, et al. Depression is associated with diabetes status of family members: NHANES (1999–2016). J Affect Disord. 2019;249:121–126. doi:10.1016/j.jad.2019.02.019
36. Khamseh ME, Baradaran HR, Javanbakht A, Mirghorbani M, Yadollahi Z, Malek M. Comparison of the CES-D and PHQ-9 depression scales in people with type 2 diabetes in Tehran, Iran. BMC Psychiatry. 2011;11:61. doi:10.1186/1471-244X-11-61
37. Zhao X, Zhang D, Wu M, et al. Loneliness and depression symptoms among the elderly in nursing homes: a moderated mediation model of resilience and social support. Psychiatry Res. 2018;268:143–151. doi:10.1016/j.psychres.2018.07.011
38. Yao J, Wang H, Yin X, Yin J, Guo X, Sun Q. The association between self-efficacy and self-management behaviors among Chinese patients with type 2 diabetes. PLoS One. 2019;14:e0224869. doi:10.1371/journal.pone.0224869
39. Rami-Merhar B, Fröhlich-Reiterer E, Hofer SE. Diabetes mellitus in childhood and adolescence (Update 2019). Wien Klin Wochenschr. 2019;131(Suppl S1):85–90. doi:10.1007/s00508-018-1420-2
40. Park M, Reynolds CF. Depression among older adults with diabetes mellitus. Clin Geriatr Med. 2015;31(1):117–37, ix. doi:10.1016/j.cger.2014.08.022
41. Robertson SM, Stanley MA, Cully JA, Naik AD. Positive emotional health and diabetes care: concepts, measurement, and clinical implications. Psychosomatics. 2012;53(1):1–12. doi:10.1016/j.psym.2011.09.008
42. Chlebowy DO, Batscha C, Kubiak N, Crawford T. Relationships of depression, anxiety, and stress with adherence to self-management behaviors and diabetes measures in African American adults with type 2 diabetes. J Racial Ethn Health Disparities. 2019;6:71–76. doi:10.1007/s40615-018-0500-3
43. Schinckus L, Dangoisse F, Van den Broucke S, Mikolajczak M. When knowing is not enough: emotional distress and depression reduce the positive effects of health literacy on diabetes self-management. Patient Educ Couns. 2018;101(2):324–330. doi:10.1016/j.pec.2017.08.006
44. Zhai Y, Yu W, Mobile A. App for diabetes management: impact on self-efficacy among patients with type 2 diabetes at a community hospital. Med Sci Monit. 2020;26:e926719. doi:10.12659/MSM.926719
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
