Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Median Nerve Affection in Hypertensive Patients with and without Diabetes High-Resolution Ultrasound Assessment
Authors Esmat A, Elshamy MI, Mohamed Zakaria D, Shady Z, Roshdy Mohamed E, El-Khouly N, Hassan MM, El-Senosy FM
Received 18 September 2021
Accepted for publication 13 November 2021
Published 15 January 2022 Volume 2022:15 Pages 183—188
DOI https://doi.org/10.2147/DMSO.S340111
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Ahmed Esmat,1 Mahmoud I Elshamy,2 Doaa Mohamed Zakaria,3 Zakarya Shady,4 Eman Roshdy Mohamed,3 Nashwa El-Khouly,3 Marwa M Hassan,3 Fatma M El-Senosy3
1Department of Neurology, Al-Azhar University, Faculty of Medicine, Cairo, Egypt; 2Department of Radiology, Al-Azhar University, Faculty of Medicine, Cairo, Egypt; 3Department of Internal Medicine, Faculty of Medicine (Girls), Al-Azhar University, Cairo, Egypt; 4Department of Internal Medicine, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Correspondence: Zakarya Shady Tel +201001281304
Email [email protected]
Purpose: Diabetes is a documented risk factor for peripheral neuropathy. It was reported that associated hypertension could increase this risk. The present study aimed to assess the effect of hypertension and diabetes on median nerve using high-resolution ultrasound.
Methods: The study includes 50 hypertensive patients (HTN group), 50 diabetic patients (DM group), 50 patients with coexisting diabetes and hypertension (HTN + DM group) and 50 healthy controls. Median nerve affection in the studied groups was studied by vibration perception thresholds (VPT). The median nerve cross-sectional area was determined at the nerve cross-sectional area of the median nerve at the carpal tunnel by high-resolution ultrasound. Clinical symptoms were assessed using Toronto Clinical Severity Score (TCSS).
Results: There was significantly higher median nerve CSA in all patient groups in comparison to controls. HTN + DM group had significantly higher median nerve CSA when compared with DM group. Patients with peripheral neuropathy in HTN + DM and DM groups had significantly higher median nerve CSA than patients without. Using ROC curve analysis, it was shown that median CSA could successfully distinguish patients with peripheral neuropathy from patients without in HTN + DM group [AUC (95% CI): 0.71 (0.54– 0.89)] and in DM group [AUC (95% CI): 0.86 (0.72– 0.99)].
Conclusion: Hypertensive patients with and without diabetes have significantly higher median nerve CSA when compared with controls.
Keywords: hypertension, peripheral neuropathy, high-resolution ultrasound, diabetes mellitus, median nerve
Introduction
Hypertension (HTN) is the leading global risk factor for cardiovascular and all-cause mortality. While the wide use of antihypertensive medications resulted in near-constant global mean blood pressure in the past decades, the prevalence of HTN continues to rise in alarming rates. It’s estimated that more than 30% of adults were diagnosed with hypertension worldwide in 2010.1 Beyond the cardiovascular consequences, HTN is also related to chronic kidney disease and end-stage renal disease. Neurologically, HTN is by far, the main risk factor for cerebrovascular stroke.2 Also, HTN has been linked to age-related cognitive impairment and dementia.3
Coexistence of HTN and diabetes mellitus (DM) is a common encounter. More than two thirds of DM patients develop arterial HTN which aggravates the micro- and macrovascular complications in those patients. On the other side of the coin, DM in HTN patients is associated with increased risk for cardiovascular disease. Both conditions share many pathological mechanisms and inter-related consequences.4
However, while the literature is replete with studies investigating various aspects of pathogenesis, diagnosis and management of diabetic peripheral neuropathy (DPN),5,6 little is known about peripheral nerve affection related to hypertension per se. Interestingly, experimental studies suggested that hypertensive rats developed significant functional and structural peripheral nerve changes largely similar to that developed by diabetic rats. Moreover, it was reported that these changes were amplified by coexistence of the two conditions.7,8 In the clinical setting, HTN is widely reported as a significant risk factor of DPN.9,10
Recent developments in high-resolution ultrasound (HRUS) enabled clinicians to add sonographic imaging features of the peripheral nervous system to the clinical findings and electrophysiological data thus improving the diagnostic performance of many pathologies of the peripheral nerves.11 In patients with DPN, HRUS could detect significant increase in the cross-sectional area (CSA) of the affected peripheral nerves.12
The present study aimed to explore the effects of HTN on the median nerve in the presence or absence of DM.
Subjects and Methods
The present study was conducted at Al-Azhar University Hospitals, Cairo, Egypt in the period from January, 2019 through December, 2020. The study protocol was approved by the ethical committee of Al-Azhar Faculty of Medicine and informed consent was obtained from all participants.
The study includes 50 hypertensive patients, 50 diabetic patients, 50 patients with coexisting diabetes and hypertension and 50 healthy controls. Hypertension was diagnosis according to the American College of Cardiology/American Heart Association 2017 guidelines.13 Diagnosis of T2DM was based on the American Diabetes Association recommendations for classification and diagnosis of diabetes.14
All groups were matched regarding age and sex distribution and patients’ groups were matched regarding the duration of the group’s clinical condition. Exclusion criteria were carpal tunnel syndrome, history of forearm or hand fractures or other causes of median nerve affection.
All participants were subjected to careful history taking, thorough clinical examination and standard laboratory assessment including fasting blood sugar, HbA1c, lipid profile, renal functions and liver functions. Median nerve affection in the studied groups was studied electrophysiologically by vibration perception thresholds (VPT). The median nerve cross-sectional area was determined at the nerve cross-sectional area of the median nerve at the carpal tunnel by high-resolution ultrasound. Diagnosis of peripheral neuropathy (PN) if present was established on the basis of abnormal nerve conduction velocity together with symptoms and signs of PN. The clinical manifestations of PN were reported using the validated translated Arabic version of Michigan Neuropathy Screening Instrument. It’s a 15-item yes/no questionnaire in addition to clinical examination.15,16 For grading of PN severity, we used the Toronto Clinical Scoring System (TCSS) that integrates neurological symptoms and neurological testing scores. According to this tool, patients were classified to have mild, moderate or severe PN.18
Data obtained from the present study were expressed as number and percent or mean and standard deviation. Statistical comparisons were achieved using t test, Fisher’s exact test, or chi-square test. Correlations were performed using Pearson’s correlation coefficient. Receiver operator characteristic (ROC) curve analysis was used to identify the diagnostic performance of investigations under assessment. All statistical operations were computed using SPSS 25 (IBM, IL, USA) with p value less than 0.05 considered statistically significant.
Results
The present study was conducted on 50 hypertensive patients (HTN group), 50 hypertensive patients with coexisting type 2 diabetes (HTN + DM group), 50 diabetic patients (DM group) and 50 healthy controls. All groups were matched for age and sex distribution and the three patient groups were matched for disease duration.
Comparison between the studied groups regarding the clinical and laboratory data is shown in Table 1. Patients in the HTN + DM group had higher frequency of cases with peripheral neuropathy when compared with patients in the DM only group without statistical significance (34.0% versus 22.0%, p=18). However, it was shown that HTN + DM group had significantly higher frequency of cases with severe neuropathy. It was also shown that HTN + DM and DM groups had significantly higher TCSS when compared with other groups. In addition, it was shown that patients in the HTN + DM and DM groups had significantly higher VPT values when compared with other groups (Table 1).
 |
Table 1 Comparison Between the Studied Groups Regarding the Clinical Data |
In the present study, comparison between the studied groups regarding the median nerve CSA at the carpal tunnel revealed significantly higher median nerve CSA in all patients’ groups in comparison to controls. Moreover, it was shown that HTN + DM group had significantly higher median nerve CSA when compared with DM group. Interestingly, patients in the HTN only group had significantly higher median nerve VPT and CSA when compared with controls (Table 1, Figure 1).
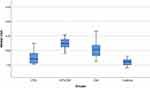 |
Figure 1 Median nerve CSA in the studied groups. |
Of note, it was also shown that patients with peripheral neuropathy in HTN + DM and DM groups had significantly higher median nerve CSA than patients without (12.9 ± 2.4 versus 11.1 ± 1.1, p=0.008 and). Using ROC curve analysis, it was shown that median CSA could successfully distinguish patients with peripheral neuropathy from patients without in HTN + DM group [AUC (95% CI): 0.71 (0.54–0.89)] (Figure 2) and in DM group [AUC (95% CI): 0.86 (0.72–0.99)] (Figure 3).
 |
Figure 2 ROC curve for median nerve CSA distinguishes patients with peripheral neuropathy in HTN + DM group. |
 |
Figure 3 ROC curve for median nerve CSA distinguishes patients with peripheral neuropathy in DM group. |
Correlations between median nerve CSA and the clinical and laboratory data in the studied groups are shown in Table 2. Remarkably, in HTN group, median nerve CSA showed significant direct correlation with VPT. In HTN + DM group, median nerve CSA had significant direct correlation with TCSS, HbA1c and VPT. In DM group, median nerve CSA had significant direct correlation with disease duration, TCSS and VPT.
 |
Table 2 Correlation Between Median Nerve CSA and Clinical Data in the Studied Patients |
Discussion
The association between hypertension and development of DPN was previously reported in type 117,19 and type 2 diabetic patients.20–22 The present study provided a high-resolution ultrasound demonstration of the effect of hypertension on peripheral nerves in patients with and without associated DM. The study found significantly higher median nerve CSA in all patients groups in comparison to controls. Moreover, it was shown that HTN + DM group had significantly higher median nerve CSA when compared with DM group. To the best of our knowledge, this is a novel finding that may help to understand the role of hypertension in development of DPN.
The value of median nerve ultrasonographic assessment in the diagnosis of peripheral neuropathy was previously established.23 Also, the study of Su et al24 recognized the role of median nerve CSA assessed by ultrasound at the pisiform level in identification of subclinical peripheral neuropathy.
In line with our findings, the study of Legrady et al25 identified increased perception threshold values on peroneal nerve in hypertensive non-diabetic patients in comparison to healthy controls supporting the vascular roles in the development of DPN.
The altered physiology of median nerve in diabetic patients was reported by the study of Horinouchi et al.26 In agreement with these conclusions, the study of Attah et al27 noted that a significant increase in median nerve CSA at the carpal tunnel in diabetic patients and the presence of DPN resulted in further increase in median nerve CSA. However, they noted no association between median nerve CSA and glycemic control or disease duration.
Interestingly and in support of our work, the experimental study of Gregory et al8 found that hypertension superimposed on diabetes augments the detrimental effects of diminished nerve blood flow, slow nerve conduction, axonal atrophy and thinning of myelinated fibers. These findings were confirmed by the study of De Visser et al.7
The present study may have significant clinical implications. Our study indicates that increased median nerve CSA in diabetic and hypertensive patients usually precedes the development of clinically manifest PN. For peripheral nerve affection, this is known as subclinical neuropathy by some authors. Considering the significant burden of DPN, early detection using HRUS may be useful for early control of the predisposing factors particularly in high-risk patients.
Moreover, the present study identified median nerve affection in HTN patients in the absence of DM. This new finding needs more exploration to identify the possible risk factors and the probable outcome in the long-term.
Conclusively, our study reported significant increase in median nerve CSA in HTN and DM patients as detected by HRUS. These changes are related to the clinical manifestations and are worsened when the two conditions co-exist.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:1–15. doi:10.1038/s41581-019-0226-4
2. Chin JH, Bhatt JM, Lloyd-Smith AJ. Hypertension—A global neurological problem. JAMA Neurol. 2017;74(4):381–382. doi:10.1001/jamaneurol.2016.4718
3. Iadecola C, Gottesman RF. Neurovascular and cognitive dysfunction in hypertension: epidemiology, pathobiology, and treatment. Circ res. 2019;124(7):1025–1044. doi:10.1161/CIRCRESAHA.118.313260
4. Pavlou DI, Paschou SA, Anagnostis P, et al. Hypertension in patients with type 2 diabetes mellitus: targets and management. Maturitas. 2018;112:71–77. doi:10.1016/j.maturitas.2018.03.013
5. Feldman EL, Callaghan BC, Pop-Busui R, et al. Diabetic neuropathy. Nat Rev Dis Primers. 2019;5(1):41. doi:10.1038/s41572-019-0092-1
6. Zakin E, Abrams R, Simpson DM, et al. Diabetic neuropathy.
7. De Visser A, Hemming A, Yang C, et al. The adjuvant effect of hypertension upon diabetic peripheral neuropathy in experimental type 2 diabetes. Neurobiol Dis. 2014;62:18–30. doi:10.1016/j.nbd.2013.07.019
8. Gregory JA, Jolivalt CG, Goor J, et al. Hypertension-induced peripheral neuropathy and the combined effects of hypertension and diabetes on nerve structure and function in rats. Acta Neuropathol. 2012;124(4):561–573. doi:10.1007/s00401-012-1012-6
9. Grisold A, Callaghan BC, Feldman EL. Mediators of diabetic neuropathy-is hyperglycemia the only culprit? Curr Opin Endocrinol Diabetes Obes. 2017;24(2):103. doi:10.1097/MED.0000000000000320
10. Huang L, Zhang Y, Wang Y, et al. Diabetic peripheral neuropathy is associated with higher systolic blood pressure in adults with type 2 diabetes with and without hypertension in the Chinese han population. Can J Diabetes. 2020;44(7):615–623. doi:10.1016/j.jcjd.2019.11.005
11. Mah JK, van Alfen N. Neuromuscular ultrasound: clinical applications and diagnostic values. Can J Neurol Sci. 2018;45(6):605–619. doi:10.1017/cjn.2018.314
12. Singh Y, Dixit R, Singh S, et al. High resolution ultrasonography of peripheral nerves in diabetic peripheral neuropathy. Neurol India. 2019;67(Supplement):S71–S76. doi:10.4103/0028-3886.250719
13. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: executive Summary: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324. doi:10.1161/HYP.0000000000000066
14. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S13–S27. doi:10.2337/dc18-S002
15. Feldman EL, Stevens MJ, Thomas PK, Brown MB, Canal N, Greene DA. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care. 1994;17(11):1281–1289. doi:10.2337/diacare.17.11.1281
16. Mohammad MT, Muhaidat J, Momani MS, et al. Translation and psychometric properties of the Arabic version of michigan neuropathy screening instrument in type 2 diabetes. J Diabetes Res. 2019;2019:2673105. doi:10.1155/2019/2673105
17. Forrest KY, Maser RE, Pambianco G, et al. Hypertension as a risk factor for diabetic neuropathy: a prospective study. Diabetes. 1997;46(4):665–670. doi:10.2337/diab.46.4.665
18. Bril V, Perkins BA. Validation of the Toronto clinical scoring system for diabetic polyneuropathy. Diabetes Care. 2002;25(11):2048–2052. PMID: 12401755. doi:10.2337/diacare.25.11.2048
19. Ponirakis G, Petropoulos IN, Alam U, et al. Hypertension contributes to neuropathy in patients with type 1 diabetes. Am J Hypertens. 2019;32(8):796–803. doi:10.1093/ajh/hpz058
20. Huang ZH, Li SQ, Kou Y, et al. Risk factors for the recurrence of diabetic foot ulcers among diabetic patients: a meta-analysis. Int Wound J. 2019;16(6):1373–1382. doi:10.1111/iwj.13200
21. Jarmuzewska E, Ghidoni A, Mangoni AA. Hypertension and sensorimotor peripheral neuropathy in type 2 diabetes. Eur Neurol. 2007;57(2):91–95. doi:10.1159/000098058
22. Nielsen JV. Peripheral neuropathy, hypertension, foot ulcers and amputations among Saudi Arabian patients with type 2 diabetes. Diabetes Res Clin Pract. 1998;41(1):63–69. doi:10.1016/S0168-8227(98)00059-X
23. Rajabally YA, Morlese J, Kathuria D, et al. Median nerve ultrasonography in distinguishing neuropathy sub-types: a pilot study. Acta Neurol Scand. 2012;125(4):254–259. doi:10.1111/j.1600-0404.2011.01527.x
24. Su PH, Chen WS, Wang TG, et al. Correlation between subclinical median neuropathy and the cross-sectional area of the median nerve at the wrist. Ultrasound Med Biol. 2013;39(6):975–980. doi:10.1016/j.ultrasmedbio.2013.01.001
25. Legrady P, Bajcsi D, Lengyel C, et al. Investigation of cardiac autonomic and peripheral sensory neuropathy in diabetic and nondiabetic patients with hypertension. Clin Exp Hypertens. 2013;35(6):465–469. doi:10.3109/10641963.2012.758272
26. Horinouchi S, Deguchi T, Arimura K, et al. Median neuropathy at the wrist as an early manifestation of diabetic neuropathy. J Diabetes Investig. 2014;5(6):709–713. doi:10.1111/jdi.12211
27. Attah FA, Asaleye CM, Omisore AD, et al. Relationship between sonographically measured median nerve cross-sectional area and presence of peripheral neuropathy in diabetic subjects. World J Diabetes. 2019;10(1):47–56. doi:10.4239/wjd.v10.i1.47
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
