Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Measuring Response to Adjunctive Therapy Among Individuals with Major Depressive Disorder
Authors Forma F, Liberman JN, Rui P, Wiggins E, Ruetsch C
Received 14 May 2022
Accepted for publication 17 September 2022
Published 28 October 2022 Volume 2022:18 Pages 2467—2475
DOI https://doi.org/10.2147/NDT.S369450
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Felicia Forma,1 Joshua N Liberman,2 Pinyao Rui,2 Emily Wiggins,2 Charles Ruetsch2
1Health Economics & Real-World Evidence, Formerly Otsuka Pharmaceutical Development & Commercialization, Inc, Princeton, NJ, USA; 2Health Analytics, LLC, Columbia, MD, USA
Correspondence: Joshua N Liberman, Tel +1 410-997-3314, Email [email protected]
Background: Incomplete or inadequate response to first-line antidepressant therapy (ADT) for major depressive disorder (MDD) is common. Response to adjunctive therapy is less understood.
Objective: To estimate response to adjunctive pharmacotherapy or psychotherapy among individuals with MDD on an antidepressant using the PHQ-9 questionnaire.
Methods: This was a retrospective cohort analysis using medical and pharmacy insurance claims among individuals with MDD or ADT who initiated adjunctive pharmacotherapy, psychotherapy, or both (dual). Eligible individuals initiated adjunctive therapy between 7/1/2014-12/31/2018. Symptom severity was measured by PHQ-9 score in the 6-month baseline and 12-month follow up. Multivariate logistic regression identified factors associated with improved symptom severity.
Results: Most (81.8%) of the 2389 participants initiated adjunctive pharmacotherapy, followed by psychotherapy (12.7%) and dual adjunctive (5.5%). Only 30.2% had both a baseline and follow-up PHQ-9 score. Among those with mild or more severe PHQ-9 baseline scores, 36.7% had the same or worse MDD severity during follow-up. Among those with moderate or more severe baseline scores, 28.1% had the same or worse MDD severity during follow-up.
Conclusion: Most individuals with moderate-to-severe MDD did not receive a follow-up questionnaire, suggesting incomplete monitoring of treatment response. Among those with a PHQ-9 following initiation of adjunctive therapy, many continued to report impactful symptoms. Future studies should explore alternate treatment approaches and methods to support the utilization of the PHQ-9 for monitoring treatment response.
Keywords: major depressive disorder, adjunctive therapy, PHQ-9, measurement-based care, psychotherapy
Introduction
A leading cause of disability worldwide,1 major depressive disorder (MDD) is characterized by depressed mood, impaired cognitive function, and disturbed sleep and appetite.2,3 The 12-month prevalence of MDD in the US is estimated to be 10.4% with lifetime prevalence estimated at 20.6%.4
Clinicians have multiple therapeutic options for the treatment of MDD. Nonetheless, first-line antidepressants are associated with a lack of adequate response in up to half of those with MDD.5–7 Among those with inadequate response to initial antidepressant therapy, the 2010 American Psychiatric Association guidelines recommend considering adjunctive therapy: adding a second medication and/or psychotherapy to the therapeutic regimen.3,8
The management and treatment of individuals with MDD can be challenging. Evaluating treatment response often depends upon subjective responses to a clinical interview by the patient or a caregiver. These subjective responses, even included in measurement-based care, are not standardized and thus are difficult to collect and use to manage therapy, leading to variability in measuring treatment response. There have been growing calls among mental health professionals to use measurement-based care, the routine collection of symptoms and function using standardized, validated questionnaires, in routine care.9,10 Measurement-based care (MBC) can provide enhanced precision and consistency in disease assessment, monitoring and assessing response to treatment in order to achieve optimal outcomes.11
The most commonly used questionnaire is the 9-item Patient Health Questionnaire (PHQ-9) a validated patient-reported outcome measure of depressive symptom frequency and severity.12 The PHQ-9 has a score range from 0 to 27 and sorts individuals into levels of depression severity: 0 to 4 (none/minimal disease); 5–9 (mild), 10–14 (moderate), 15–19 (moderately severe), and 20–27 (severe). The categories align with clinical decision support recommendations that provide guidance to clinicians.
In addition to supporting MBC, PHQ-9 data also provide an opportunity to assess population-level responses to treatment. To date, little is known about real-world response to adjunctive therapy for MDD measured by validated measures of depressive symptom frequency and severity. In this retrospective analysis of claims data, we estimated response to adjunctive pharmacotherapy or psychotherapy among individuals with MDD on an antidepressant using the PHQ-9.
Methods
Study Design
This study was a retrospective cohort analysis of individuals with MDD on an antidepressant medication (ADT) who received either a second pharmacotherapy, psychotherapy, or both a second ADT and psychotherapy (also known as “dual adjunctives”). As the analytical dataset did not include personal identifiable information, the research protocol received an exempt determination by the Advarra Institutional Review Board. All data was protected and stored on HIPAA-compliant servers and all privacy regulations for the data were followed.
Identification and Selection of Study Participants
The sampling frame was the national sample of individuals identifiable in a commercially available database of medical and pharmacy insurance claims licensed from Clarivate (www.clarivate.com/products/real-world-data/). The full study period was January 1, 2014, through December 31, 2019. The case-finding period was July 1, 2014, through December 31, 2018, and was used to identify the adjunctive therapy event date (index). The baseline and follow-up periods were the 6 months prior to and 12 months following the index event. The following mutually exclusive adjunctive populations were identified:
- Pharmacotherapy: defined by the addition of a second pharmacotherapy to the initial ADT;
- Psychotherapy: addition of psychotherapy to the initial ADT;
- Dual adjunctives: addition of a second pharmacotherapy and psychotherapy to the initial ADT. This could mean a 2nd pharmacotherapy was added following addition of psychotherapy to an individual’s initial ADT or vice versa (psychotherapy was added to a 2nd pharmacotherapy was added to the initial ADT).
Eligible adults had two or more outpatient claims (or one inpatient claim) associated with MDD diagnosis codes (ICD-9-CM (296.2x or 296.3x) or ICD-10-CM (F32.x, F33.x) excluding MDD with psychotic features) on claims separated by at least 30 days; evidence of adjunctive therapy in the period between July 1, 2014 and December 31, 2018; claim(s) for ADT before and after initiation of adjunctive therapy, defined as 50% adherence to an ADT in the 56 days (8 weeks) immediately prior to and following the initiation of adjunctive therapy; ≥1 valid PHQ-9 scale score; and ≥1 medical or pharmacy claim in each calendar quarter beginning 6 months prior to and continuing 12-months following the index event; and no evidence of psychotherapy in the 3 months prior to index. Continual benefits eligibility was defined as presence of ≥1 medical or pharmacy claim per quarter, beginning 6 months prior to index and continuing through 12 months post-index. The pharmacotherapy population had ≥50% adherence to adjunctive pharmacotherapy in the 8 weeks post-index and the psychotherapy population had ≥1 additional psychotherapy claims in the 56 days following index. The dual adjunctive group included individuals who had psychotherapy added following the addition of adjunctive pharmacotherapy to their initial ADT or who had a second pharmacotherapy added following the addition of adjunctive psychotherapy to their initial ADT. Eligible index antidepressant included alpha-2 receptor antagonists, monoamine oxidase inhibitors (MAOIs), serotonin modulators, selective serotonin reuptake inhibitors (SSRI), serotonin and norepinephrine reuptake inhibitors (SNRI), tricyclics, tetracyclics, and other ADTs (e.g. bupropion). Eligible adjunctive therapy included any of the ADT classes, atypical antipsychotics, lithium, and psychotherapy, defined by CPT codes 90832, 90834, 90837, 90839, 90840, 90845, 90847, 90849, 90853, and 96152. Study participants were excluded if they had evidence of a paid insurance claim by Medicare or ≥2 claims associated with bipolar or other depression disorders, dementia, psychosis, schizophrenia, or dissociative and conversion disorders.
Measurement
Treatment response was measured by PHQ-9 score. The PHQ-9 scale is a validated, self-administered questionnaire12–14 that measures the impact of nine depressive symptoms on functioning during the past two weeks. The PHQ-9 scale ranges from 0 (no symptoms) to 27 (severe, frequent symptoms). Response array is on a Likert scale ranging from not at all, several days, more than half the days, and nearly every day.15 Scores can be assessed in raw form or grouped: 0 to 4 (none/minimal disease); 5–9 (mild), 10–14 (moderate), 15–19 (moderately severe), and 20–27 (severe).12,15 A decline in the PHQ-9 score of ≥5 points qualifies as a clinically significant response to depression treatment.12 In the United States, the Healthcare Effectiveness Data and Information Set (HEDIS) is a widely used set of performance measures, supported by the National Committee for Quality Assurance (NCQA).16
For individuals with a baseline PHQ-9 score of 10 or higher, the Healthcare Effectiveness Data and Information Set (HEDIS) measure “depression remission or response (DRR) for adolescents and adults” was derived, with separate measures for percentage with a follow-up score in 4–8 months, percentage with follow-up score <5, and percentage of > 50%+ reduction.16
Statistical Analysis
Demographic variables included age, sex, and type of insurance (commercial insurance or Medicaid: state-sponsored insurance for eligible individuals based on low income, disabilities, etc.). Psychiatric comorbidities, measured across the 18-month study period, included generalized anxiety disorder, substance-related disorders, insomnia, alcohol-related disorders, PTSD, dysthymic disorder, and panic disorder. MDD severity level (mild, moderate, severe, in remission, unspecified) was derived from ICD diagnosis codes in the period prior to adjunctive therapy. Individuals were on an ADT and received adjunctive therapy (either a 2nd pharmacotherapy or psychotherapy). Individuals with multiple severity classifications were assigned the most severe diagnosis. A psychiatrist visit was defined as a visit to a provider with a psychiatry specialty taxonomy code any time in the 18-month study period.
Frequencies and percentages were calculated for categorical variables and means and standard deviations for continuous variables. Differences between categorical variables were tested with Chi-squared tests. Differences between continuous variables were tested with two-sided t-tests for normally distributed variables and Wilcoxon Mann–Whitney U-tests for skewed variables. Two separate multivariate logistic regression models were used to identify factors associated with: 1) achieving optimal treatment response following the addition of adjunctive therapy, defined as a PHQ-9 score of <5 in the follow-up period, and 2) realizing a reduction in PHQ-9 scores between baseline and follow up resulting in movement to a lower severity category. Both regression models applied backwards stepwise variable selection. The threshold for significance was set at 0.05. All analyses were performed with SAS software, v9.4, SAS Institute Inc., Cary, NC, USA.
Results
There were 10,731,976 individuals who met MDD eligibility criteria between July 1, 2014 and December 31, 2018. Individuals were excluded if they were not ≥18 years of age as of the initial MDD diagnosis date, had an exclusion diagnosis or who did not have an ADT drug claim from July 1, 2014, to December 31, 2018. All cases were required to have received adjunctive therapy following an ADT, have evidence of benefits eligibility each quarter of the study period and be insured wither though Medicaid or commercial health insurance. All cases were required to have had a PHQ-9 score during the 18-month study period providing a final analysis cohort of 2389 individuals (Figure 1).
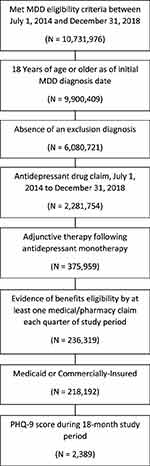 |
Figure 1 Flow Diagram of the Selection of Study Participants. |
The study cohort consisted of 1,792 (75%) females and 597 (25%) males. The average age of the study cohort was 48.2 years of age; 274 (11.5%) individuals were between 18 and 30 years of age; 877 (36.7%) were between 31 and 49 year of age; 1,084 (45.4%) were between 50 and 64 years of age; and 154 (6.4%) were 65 years of age and older (Table 1).
 |
Table 1 Demographic Characteristics and Comorbidities Among Eligible Participants with MDD and ≥PHQ-9 Score During the 18-Month Study Period |
Of the eligible individuals, 1,701 (71.2%) had commercial insurance, while 688 (28.8%) were on Medicaid. In terms of type of adjunctive therapy received, 303 (12.7%) individuals received adjunctive psychotherapy only, 1955 (81.8%) received a 2nd pharmacotherapy only, and 131 (5.5%) were “dual adjunctives” and received both. Of the available PHQ-9 scores, 689 (28.8%) had baseline only scores, 979 (41%) had follow-up only scores, and 721 (30.2%) had both baseline and follow-up scores. Of those who had a recent MDD diagnosis prior to index, the MDD severities provided were: 1,471 (61.6%) unspecified, 247 (10.3%) severe, 545 (22.8%) moderate, and 126 (5.3%) mild or in remission. In terms of psychiatric comorbidities, most individuals had a diagnosis of generalized anxiety disorder (GAD) in addition to MDD, and the most common medical comorbidities were hypertension and hyperlipidemia (Table 1).
The lowest PHQ-9 score following 1 month of adjunctive therapy was seen in those with severe MDD who received dual adjunctive therapy group, moderately severe MDD who received adjunctive psychotherapy, the moderate MDD group who received adjunctive pharmacotherapy, the mild MDD group who received adjunctive psychotherapy, and none/minimal MDD group who received adjunctive pharmacotherapy (Figure 2). Among those with mild or more severe PHQ-9 baseline scores, 36.7% had the same or worse MDD severity during follow-up. Among those with moderate or more severe baseline scores, 28.1% had the same or worse MDD severity during follow-up (Table 2).
 |
Table 2 Baseline and Lowest Follow-Up PHQ-9 Scores Following Adjunctive Therapy Among the 721 Individuals with Scores in Both Periods |
HEDIS performance measures were also assessed for those who had a baseline PHQ-9 score of ≥10. Of those with commercial insurance (n=488), 155 (31.8%, 95% CI 27.8–36.0) had a PHQ-9 score 4–8 months later, 26 (16.8%, 95% CI 11.6–23.2) individuals had a PHQ-9 score <5, and 60 (38.7%, 95% CI 31.6–47.1) individuals had a ≥50% reduction in PHQ-9 score. Of those with Medicaid (n=256), 73 individuals (28.5%, 95% CI 23.2-34.0) had a PHQ-9 score 4–8 months later. 10 (13.7%, 95% CI 6.8–21.9) had a PHQ-9 <5 and 15 (20.5%, 95% CI 12.3–30.1) had a ≥50% reduction in PHQ-9 score (Table 3).
 |
Table 3 HEDIS Performance Among Individuals with a Baseline PHQ-9 Score of 10+ |
Discussion
Findings from this analysis suggest that, even after adding adjunctive therapy, a substantial proportion of individuals with MDD continue to have depressive symptoms. PHQ-9 scores reported after adjunctive therapy initiation indicated that nearly 37% of individuals with MDD continued to have moderate or more severe MDD symptoms. Further, in individuals with both a baseline and a follow-up PHQ-9 score, an estimated 28.1% reported little to no improvement in symptom severity.
Numerous studies have evaluated factors associated with treatment response. Our findings suggest that psychiatric comorbidity burden is associated with lower likelihood of response and that psychiatric care is associated with higher likelihood of response. Further, only a single medical comorbidity, low back pain, a chronic pain condition that affects daily functioning, quality-of-life, and employment was inversely associated with treatment response. It is also interesting to note that most clinicians did not specify the severity of MDD in the selection of the ICD code submitted on the medical claim. However, this coding did appear to align with treatment response and a more systematic selection of severity-specific ICD codes might improve the precision of treatment and management of MDD.
These real-world results are consistent with results from randomized clinical studies of adjunctive therapy, which consistently report that adjunctive therapies, particularly with atypical antipsychotics, are an effective treatment strategy for some but do not resolve all symptoms for all individuals.17,18
There is substantially less real-world evidence documentation of the impact of adjunctive psychotherapy. These results suggest that adjunctive psychotherapy is comparable to adjunctive pharmacotherapy in improving MDD symptoms, but that dual adjunctive therapy may be substantially more effective. These results are consistent with reports that pharmacotherapy and psychotherapy are comparable19 and that combined therapies are more effective than individual therapies.20,21 However, evidence from systematic literature reviews of randomized clinical trials comparing treatment response among individuals with adjunctive psychotherapy to individuals on antidepressant treatment alone report conflicting results. In a review of 14 trials, Xiang et al22 reported that there is no evidence that pharmacotherapy in combination with psychotherapy was superior to individual treatment modalities in children and adolescents with MDD. In contrast, in a meta-analysis of 23 randomized controlled trials Karyotaki et al23 reported that combination pharmacotherapy and psychotherapy was superior to antidepressant medication alone in the acute phase of illness. In a 2014 meta-analysis of 52 studies among adults with either depressive or anxiety disorder, Cuijpers et al24 also reported the superiority of combination therapy.
The collective body of evidence, including these results, reinforces that MDD is a challenging condition to manage. ADTs are limited in efficacy and tolerability.25 In addition, ADT medication adherence is poor, typically due to negative side effects, depression severity, physician and patient communication, and other psychiatric comorbidities.26 An additional challenge is the time constraint presented in primary care, as well as the cycling in-and-out of care faced by individuals who have MDD due to feeling hopeless or discouraged over treatment failure.18 To address these challenges, there is a growing recognition that alternative and expanded models of care are required. In a recent report, Huijbregts et al27 studied a collaborative care vs care as usual model that require an extended care team to manage individuals with MDD. The study confirmed the complexity of the condition and that medication or psychotherapy alone is not sufficient to achieve optimal outcomes.
Further, care models are best implemented using assessment tools such as the PHQ-9. Measurement-based care has been shown to improve psychotherapy outcomes, identify those who are improving or deteriorating, improve role functioning, and symptom reduction monitoring in patients with psychiatric disorders.9,28 Individuals who complete self-reported rating scales, like the PHQ-9, become more knowledgeable about their disorders, aware of their symptoms over time, and can identify relapse or reoccurrence.9 Despite these findings, measurement-based care scores may be difficult to locate in EHRs.29 These findings confirmed inconsistent use of the PHQ-9 to monitor treatment response and disease progression.
Given the low rate of PHQ-9 administration, the low compliance with HEDIS-recommended measures of quality depression care using the PHQ-9 were unsurprising. However, research indicates that compliance with these HEDIS measures can translate into direct clinical and financial value. Bhattacharjee et al30 reported that adherence to HEDIS ADT management recommendations was associated with reductions in hospitalization risk among adults with comorbid MDD and dementia.
Study Limitations
The study used an open dataset; the sample was not controlled for insurance benefits eligibility. In addition, many scores may not have been recorded in electronic health records or stored in clinical narrative and thereby not available to code in this data set. This limitation contributed to a low eligibility rate, which led to a small sample size that limited the power to detect significant differences and may lead to a study sample that is not generalizable to the general population of individuals with MDD. Finally, while claims data represent medication and therapy services purchasing behavior, the data do not guarantee medication was consumed or the therapy was committed to.
Conclusions
Despite the availability of several adjunctive treatment approaches for MDD including ADTs and psychotherapy or both, this analysis showed that a substantial proportion of individuals have persistent MDD symptoms which may impact daily functioning. There was a greater percentage of those with Medicaid who persisted with severe illness compared to those with commercial health insurance. Older adults and those with commercial insurance were more likely to have PHQ-9 follow-up scores indicating remission while those with severe MDD, low back pain, and PTSD were less likely to have scores indicating remission. In addition, the PHQ-9 is underutilized as a treatment progress tracking tool to evaluate treatment response. Most individuals with an elevated PHQ-9 score did not have a follow-up administered, which suggests incomplete monitoring of treatment response. Individuals with more severe symptoms were more likely to have follow-up PHQ-9 administered compared to those with less severe symptoms. Compliance with HEDIS-recommended measures of PHQ-9 monitoring was low. Future studies should explore alternate approaches to the treatment of MDD as well as the utilization of the PHQ-9 as a treatment progress tracking tool.
Funding
This work was supported by Otsuka Pharmaceutical Development & Commercialization, Inc.
Disclosure
Ms Felicia Forma is an employee of Otsuka Pharmaceuticals Development & Commercialization, Inc., during the conduct of the study. Dr Joshua N Liberman, Ms Pinyao Rui, Ms Emily Wiggins, Dr Charles Ruetsch are employees of Health Analytics, LLC. Dr Charles Ruetsch reports personal fees from Otsuka America, during the conduct of the study; personal fees from Otsuka America, Janssen, and Orexo, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517. doi:10.1001/jama.2017.3826
2. Otte C, Gold SM, Penninx BW, et al. Major depressive disorder. Nat Rev Dis Primers. 2016;2(1). doi:10.1038/nrdp.2016.65
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
4. Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. doi:10.1001/jamapsychiatry.2017.4602
5. Hiranyatheb T, Nakawiro D, Wongpakaran T, et al. The impact of residual symptoms on relapse and quality of life among Thai depressive patients. Neuropsychiatr Dis Treat. 2016;12:3175–3181. doi:10.2147/NDT.S124277
6. Nil R, Lütolf S, Seifritz E. Residual symptoms and functionality in depressed outpatients: a one-year observational study in Switzerland with escitalopram. J Affect Disord. 2016;197:245–250. doi:10.1016/j.jad.2016.02.062
7. Rush AJ. STAR*D: what have we learned? Am J Psychiatry. 2007;164(2):201–204. doi:10.1176/ajp.2007.164.2.201
8. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
9. Fortney JC, Unützer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2017;68(2):179–188. doi:10.1176/appi.ps.201500439
10. Greden JF. The national network of depression centers: progress through partnership. Depress Anxiety. 2011;28(8):615–621. doi:10.1002/da.20862
11. Harding KJ, Rush AJ, Arbuckle M, Trivedi MH, Pincus HA. Measurement-based care in psychiatric practice: a policy framework for implementation. J Clin Psychiatry. 2011;72(8):1136–1143. doi:10.4088/JCP.10r06282whi
12. Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509–515. doi:10.3928/0048-5713-20020901-06
13. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–1744. doi:10.1001/jama.282.18.1737
14. Spitzer RL, Williams JBW, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD Patient Health Questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183(3):759–769. doi:10.1067/mob.2000.106580
15. Zimmerman M. Using the 9-Item patient health questionnaire to screen for and monitor depression. JAMA. 2019;322(21):2125–2126. doi:10.1001/jama.2019.15883
16. NCQA. HEDIS and performance measurement. NCQA. Available from: https://www.ncqa.org/hedis/.
17. Rafeyan R, Papakostas GI, Jackson WC, Trivedi MH. Inadequate response to treatment in major depressive disorder: augmentation and adjunctive strategies. J Clin Psychiatry. 2020;81(3):OT19037BR3. doi:10.4088/JCP.OT19037BR3
18. Papakostas GI, Jackson WC, Rafeyan R, Trivedi MH. Overcoming challenges to treat inadequate response in major depressive disorder. J Clin Psychiatry. 2020;81(3):OT19037BR4. doi:10.4088/JCP.OT19037BR4
19. Kocsis JH, Gelenberg AJ, Rothbaum BO, et al. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: the REVAMP Trial. Arch Gen Psychiatry. 2009;66(11):1178–1188. doi:10.1001/archgenpsychiatry.2009.144
20. Friedman MA, Detweiler-Bedell JB, Leventhal HE, Horne R, Keitner GI, Miller IW. Combined psychotherapy and pharmacotherapy for the treatment of major depressive disorder. Clin Psychol. 2004;11(1):47–68. doi:10.1093/clipsy.bph052
21. Wiles N, Thomas LJ, Abel A, et al. Cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment resistant depression in primary care: the CoBalT randomised controlled trial protocol. Contemp Clin Trials. 2012;33(2):312–319. doi:10.1016/j.cct.2011.10.016
22. Xiang Y, Cuijpers P, Teng T, et al. Comparative short-term efficacy and acceptability of a combination of pharmacotherapy and psychotherapy for depressive disorder in children and adolescents: a systematic review and meta-analysis. BMC Psychiatry. 2022;22:139.
23. Karyotaki E, Smit Y, Henningsen KJ, et al. Combining pharmacotherapy and psychotherapy or monotherapy for major depression? A meta-analysis on the long-term effects. J Affect Disord. 2016;194:144–152.
24. Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds III CF. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry. 2014;13:56–67.
25. Kaster MP, Moretti M, Cunha MP, Rodrigues AL. Novel approaches for the management of depressive disorders. Eur J Pharmacol. 2016;771:236–240. doi:10.1016/j.ejphar.2015.12.029
26. Baeza-Velasco C, Olié E, Béziat S, Guillaume S, Courtet P. Determinants of suboptimal medication adherence in patients with a major depressive episode. Depress Anxiety. 2019;36(3):244–251. doi:10.1002/da.22852
27. Huijbregts KM, de Jong FJ, van Marwijk HW, et al. A target-driven collaborative care model for Major Depressive Disorder is effective in primary care in the Netherlands. A randomized clinical trial from the depression initiative. J Affect Disord. 2013;146(3):328–337. doi:10.1016/j.jad.2012.09.015
28. Aboraya A, Nasrallah HA, Elswick DE, et al. Measurement-based Care in Psychiatry-Past, Present, and Future. Innov Clin Neurosci. 2018;15(11–12):13–26.
29. Pincus HA, Scholle SH, Spaeth-Rublee B, Hepner KA, Brown J. Quality measures for mental health and substance use: gaps, opportunities, and challenges. Health Aff. 2016;35(6):1000–1008. doi:10.1377/hlthaff.2016.0027
30. Bhattacharjee S, Naeem S, Knapp SM, et al. Health outcomes associated with adherence to antidepressant use during acute and continuation phases of depression treatment among older adults with dementia and major depressive disorder. J Clin Med. 2020;9(10):3358. doi:10.3390/jcm9103358
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.