Back to Journals » Infection and Drug Resistance » Volume 16
Measles Outbreak Investigation in Garda Marta District, Southwestern Ethiopia, 2022: Community-Based Case-Control Study
Authors Bukuno S , Asholie A, Girma Z , Haji Y
Received 20 February 2023
Accepted for publication 22 April 2023
Published 4 May 2023 Volume 2023:16 Pages 2681—2694
DOI https://doi.org/10.2147/IDR.S405802
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Silas Bukuno,1 Agunie Asholie,2 Zeleke Girma,3 Yusuf Haji2
1Resident at Ethiopian Field Epidemiology and Laboratory Training Program, School of Public Health, Hawassa University, Hawassa, Ethiopia; 2College of Medicine and Health Science, School of Public Health, Hawassa University, Hawassa, Ethiopia; 3Department of Public Health, School of Public Health, Arba Minch University, Arba Minch, Ethiopia
Correspondence: Silas Bukuno, Tel +251932-21-4757, Email [email protected]
Background: A measles outbreak can occur in the presence of an increased number of unvaccinated children; however, the vaccine was available many decades ago, and it is the foremost cause of child mortality, claiming 568 lives (mostly children) worldwide each day. The investigation was aimed at assessing the magnitude and identifying contributing factors for the measles outbreak in the Garda Marta District of Gamo Zone, Southwestern Ethiopia.
Methods: From January 20 to February 10, 2022, a descriptive and unmatched case–control study was used to describe the measles outbreak and identify the associated risk factors for measles infection. The descriptive analysis employed all 140 cases from the line list, while the case–control study used 51 cases and 102 controls to investigate factors associated with measles infection. Epi-data version 4.6.0.6 was used to code and enter data, which was then exported to SPSS version 27 for analysis. A standardized questionnaire was used to collect data. To declare statistical significance for the association, multivariable logistic regression with an adjusted odds ratio (AOR) and 95% CI was used.
Results: From a total of 140 measles cases reported from October 12, 2021, to March 09, 2022, 75 (54%) were females. Marta Laddo kebele was most affected (104 cases). Being unvaccinated (AOR: 2.84, 95% CI: 1.10– 7.32), having a travel history (AOR: 4.24, 95% CI: 1.61– 11.15), having a contact history (AOR: 6.34, 95% CI: 2.35– 17.40), being unaware of the mode of transmission (AOR: 2.68, 95% CI: 1.16– 6.37), and having moderate acute malnutrition (AOR: 4.44, 95% CI: 1.74– 11.31) were factors significantly associated with the measles outbreak.
Conclusion: Being unvaccinated, travel history to measles outbreak area, contact history, knowledge of caretakers/mothers on the mode of transmission, and acute malnutrition were associated with the measles outbreak in the district. Therefore, strengthening routine measles immunization, mounting vaccination awareness and nutritional screening are recommended.
Keywords: measles outbreak, case control, Garda Marta, South Ethiopia
Introduction
Measles is an acute, highly infectious viral disease caused by the measles virus. It is transmitted mostly through respiratory secretions or aerosol discharge from a person infected with the disease to mucous membranes in the upper respiratory tract or the conjunctiva.1,2 It is characterized by its classic symptoms like fever, cough, coryza, conjunctivitis, and maculopapular rash.2,3 The incubation period of measles is about 10 to 12 days (range 7–18 days).3 Secondary attack rates among susceptible household contacts have been reported to be 75–90%.2 Measles’ serious complications include pneumonia, encephalitis and blindness.2–4 Malnourished children are at higher risk of developing complications and mortality from measles infection.3 In an impoverished nations such as Ethiopia, the case fatality rate from measles is reported to be 3–5%.2,3
Nevertheless, the vaccine was available many decades ago; still, it is the foremost cause of child morbidity and mortality.5 The World Health Organization (WHO) Regional Office for Africa (AFRO) established measles elimination: A strategy for the African Region in 2011 to have all member states of the WHO’s African region (AFR) free of the disease by the year 2020.6
As a member state, Ethiopia, currently, is implementing these regional plans in order to control and eventually eliminate measles by 2020. These strategies are improving measles vaccination (MCV1 and MCV2), assessing the impact of vaccination, and improving clinical case management.2
It has been recommended that a country must achieve and maintain 95% coverage with two timely doses of the measles-containing vaccine (MCV) to prevent measles morbidity and mortality; however, in 2021 performance for MCV1 vaccination reached 81% and MCV2 stands at just 71% according to WHO report.7
By the end of 2019, 178 Member States had made a second dose of measles vaccine part of routine immunization, and 71% of children had received two doses of measles vaccine in accordance with national immunization schedules.8 Despite all this progress, measles cases increased in all parts of the world in 2019, according to WHO data. Global measles cases quadrupled in the first three months of 2019 compared to the same period in 2018, with Africa experiencing the most dramatic 700% increase.9,10 Globally, a total of 869,770 measles cases were reported from 194 countries in 2019 with an incidence rate of 120 per 1 million, claiming more than 207,500 lives in 2019 alone.9 Nowadays, measles claims an estimated 568 lives (mostly children) worldwide each day.11
A measles outbreak can occur in the presence of an increased number of unvaccinated children; however, the effective MCV vaccine was available.12 For example, WHO-AFR experienced the highest measles incidence in 2019, with 567 cases per 1 million population.9 In the first three months of 2022, 20 African nations reported measles outbreaks to the WHO African Region. More than 17,000 measles cases were reported in the African region in the first six months of 2022, a more than threefold increase from the same period in 2021.13
In Ethiopia, the Expanded Program on Immunization (EPI) began with six diseases including measles almost forty years ago. It has now progressed to more than ten diseases in the country, increasing vaccine coverage through 2019.14–17 In Ethiopia, EPI program is mainly supported by WHO, global alliance for vaccine initiatives (GAVI) and United Nations Child Fund (UNICEF). Immunization services are provided in most of the health facilities and as an outreach service for communities residing beyond 5 km from the static health facilities. Currently, almost all of the public health facilities and some private hospitals provide immunization services, and all the three-tier health care delivery systems in Ethiopia provide Immunization services.18
The Ethiopian Demographic and Health Survey 2019 mini-report for measles vaccine first and second dose shows 59% and 9%, respectively, which was below the WHO cut point of 95% for immunization.16 Several reasons, including family understanding of the necessity for vaccination, financial constraints, vaccine stockouts, political affairs, and vaccine reluctance and misinformation, could limit access to immunization services in Ethiopia.19 Many studies have found that contact history, lack of immunization knowledge, illiteracy, low economic status, distance from a health facility, vitamin A deficiency, malnutrition, and low vaccination coverage are all linked to measles outbreaks.20–23 Measles outbreaks commonly occur in various areas of the country because of the low vaccination rate and poor living conditions.24 Ethiopia is one of the six nations with the greatest proportion of newborns worldwide who did not receive the measles vaccine in 2017.25 Ethiopia has a high frequency of measles with about 50 cases per 100,000 population reported annually.26 Hence, more than 7400 confirmed cases of the disease were reported from 2016 to 2018 in Ethiopia alone.27 Due to continued outbreaks throughout the regional states, this figure had climbed to 8202 as of August 2019.28
The Measles outbreak investigation study helps in the identification of risk categories, disease epidemiology, and sources of infection, as well as the direction of preventive efforts.29,30 This investigation aimed to assess the magnitude and contributing factors for the measles outbreak in Garda Marta District of Gamo Zone and generate evidence for the prevention and control of future outbreaks in 2022.
Materials and Methods
Study Settings
The investigation was conducted in the Garda Marta District of Gamo Zone from January 20, to February 10, 2022. It is one of the 20 districts of the Gamo Zone. The administration town, Gogale, is located at a distance of 130 km from the Zonal capital (Arba Minch) and 635 km away to the south of Addis Ababa (the Capital of Ethiopia). Based on the 2007 national census projection, the estimated total population of the district was 53,192 in 2022, of which 51% (27,128) were females. Of the total population, 15.61% (8303) were under five and 5.18% (2755) were under two-year children. The district is divided into 12 rural kebeles with a total of 2 health centers and 12 health posts. All public health facilities (Health Centers and Health Posts) provide immunization services and nutritional screening as per the national immunization program. There were no private health facilities in the district. Agriculture is the main source of livelihoods for the majority of the population in the district followed by cattle rearing. Garda Marta District is one of the drought-affected areas in the South Nations Nationalities and People’s (SNNP) Region. Figure 1 shows administrative map of the study area.
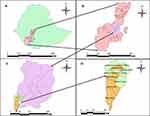 |
Figure 1 As indicated in Figure 1, (A) represents the Ethiopian boundary, (B) represents the South Nation Nationalities and Peoples’ (SNNP) Regional State, (C) represents the Gamo Zone, and (D) represents the administrative map of Garda Marta District. Area shaded with light yellow color for the study district (D) shows kebeles affected by the measles outbreak. |
Study Design
We employed a 1:2 unmatched case–control study design to identify the risk factors associated with measles infection. Furthermore, a cross-sectional study of cases registered on the measles line list was described interims of place, person and time to evaluate the frequency and distribution of the measles outbreak.
Data Sources
All four kebeles in the Garda Marta District affected by the measles outbreak, as shown in Figure 1 with a light orange color, were data sources for current study.
Study Subjects
Any person, including children affected by measles, was the subject of the study. Cases on the line list and active cases in the community were interviewed using structured questionnaires to get information on the risk factors associated with the outbreak. Demographic data on patient characteristics, such as: date of onset, date of visit to health facilities, outcomes, and vaccination status were gathered. Further information on the cold chain management and patient handling was also collected.
Laboratory Methods
A 5 mL of blood sample was properly collected from six suspected measles cases using syringe and needle by venipuncture and poured into a sterile tube labeled with patient identification and collection date. After separating the serum from red cells, labeled test tubes are kept in vaccine carrier which has four conditioned ice packs in four of its sides. Then, the specimen and copy of case investigation form were sent to the SNNP regional public health institute laboratory for an IgM antibody test. Six of the samples tested positive for IgM antibodies.
Criteria for Inclusion and Exclusion
Inclusion for Cases
Any person who developed fever, maculopapular rash and/or cough, coryza, or conjunctivitis or laboratory confirmed measles IgM was included in the study.
Exclusion
Those who have vaccination history in the past two weeks were excluded because they may develop measles symptoms as a result of an adverse event following immunization.
Inclusion for Controls
Those who do not fulfil the measles case definition and those who had no previous history of measles infection were included as controls in the study.
Exclusion
Those who had previous history of measles infection were excluded because they develop immunity against measles.
Sample Size Determination and Sampling Techniques
All 140 suspected measles cases recorded on the line list were included in the descriptive study. The sample size for the case–control study was calculated using the Epi Info software version 7.2 under the assumption of double population proportion formula. To calculate the sample size: proportion of control exposed for three exposure variables (age of mothers, distance from health facility, and age of patient), AOR, 95% CI, power 80% and the ratio of a case to control 1:2 were taken into account. Finally, the age of the patient with a sample size of 153 was selected. This sample size was finally splinted into 51 cases and 102 controls. We identified cases for a case–control study from the line list and by conducting an active case search in the community. Cases identified in both ways were interviewed in the community. For every single case, two controls who did not fulfill the measles case definition and those who had no previous history of measles infection were selected from the same community a few distances from the cases.
Enrolment of Cases and Controls
Cases
Cases were enrolled based on laboratory confirmed measles IgM or linked to confirmed cases epidemiologically.
Controls
Residents of Garda Marta District who were living in the same kebele with the cases and who did not fulfil the case definition of measles were considered as controls.
Operational Definition
Suspected Measles Case
A suspect case is any rash illness with fever.2
Confirmed Measles Case
A suspected case with laboratory confirmation (positive IgM antibody) or epidemiologically linked to confirmed cases in an outbreak.2
Epidemiologically Linked Case
A clinical case of measles that was geographically and temporally associated, with dates of rash development occurring 7–21 days apart from a laboratory-confirmed case or another epidemiologically linked measles case.2
Measles Death
When a person with confirmed measles (clinically, laboratory, or epidemiologically) dies within 30 days of rash development and is not the result of other associated causes.2
Data Collection Tools and Techniques
A structured questionnaire adapted from other literature31 with some modifications as per the local context was utilized to address the study objectives. Information on socio-demographic variables, access to health facilities, nutritional status, and other risk factors for measles infection was gathered through interviews with mothers/caregivers of children. Immunization information was collected by observing immunization cards and asking about history of vaccination. We identified cases from case registration book (line list) in the district health office and active case searches in the community. Controls were selected from the same community a few distances from cases.
Data Processing and Analysis
Tables and graphs were used to analyze line list data in MS Office 2010 for the descriptive study. A descriptive study of measles cases was characterized by person, place, and time. Data from the case–control study were reviewed for completeness before being coded and input into Epi-data version 4.6.0.6 and exported to SPSS version 27 for analysis. The Hosmer and Lemeshow goodness-of-fit test was used to evaluate model fitness. To analyze the strength of connections between the outcome and predictor factors at P-value, adjusted odds ratios (AOR) with matching 95% confidence intervals (CIs) were utilized. To identify independent factors associated with measles infection, explanatory variables that were significantly associated with the outcome variable in the bivariate logistic regression at p <0.25 were entered into a multivariable logistic regression model using the backward elimination stepwise method. A p-value of <0.05 was considered significant.
Data Quality Management
To avoid misclassification bias, standard case definitions were first used to select cases from the community. All community cases were registered using the line list and an active case search. Similarly, all controls were selected from the same neighborhood to ensure the representativeness of the study findings. Furthermore, the principal investigator collected data.
Ethical Considerations
The Gamo Zone Health Department Ethics Review Committee granted their approval under the reference number GZH1/175/14, and the study was carried out in conformity with the Declaration of Helsinki for human subjects. Similarly, oral consent was obtained from all informants or caretakers during data collection. The ethical review committee accepted individual verbal informed consent since it is an outbreak investigation with only minor health risks to participants and does not involve a technique for which written agreement is generally required outside of the inquiry environment. Furthermore, the study was done in rural areas where many individuals were unable to read and write, making it impossible for them to complete the information sheet. Moreover, for participants under the age of 18, assent was first obtained from respondents and lastly their mothers or caretakers provided oral consent on their behalf.
Prior to data collection, we informed participants about the study’s purpose and their readiness to engage in the study. We have granted the autonomy to withdraw from the interview at any time if they are not comfortable. We assured confidentiality by using codes instead of any personal identifier.
Results
Descriptive Epidemiology
The index case was a 35 years old male adult identified on October 12, 2021. He had a travel history to Doyso kebele of Maale District (South Omo Zone) one week before the onset of illness and has unknown vaccination status against measles.
A total of 140 measles cases and one death with a crude case fatality rate (CFR) of 0.7% were registered from October 12 to March 09, 2022, in the Garda Marta District of Gamo Zone. The outbreak started on September 28, 2021, and reached its peak level on December 21, 2021. Of the total cases, 75 (54%) were female. Only 28 (20%) were treated as an outpatient and the rest 80% of measles cases were treated as inpatients from a total of 140 cases. Six cases (4%) were laboratory confirmed, and 134 (96%) cases were epidemiologically linked. The overall attack rate (AR) of the outbreak was 26/10,000 and higher among 0–59-month-old children (90/10,000).
Cases by Place, Person, and Time
Cases by Place
The current outbreak affected four kebeles of the district, of which two (Garda 01 and Gogale 01) were urban areas and the AR of all affected kebeles was 89/10,000 population. The highest number of cases was observed in Marta Laddo with an AR of 179/10,000 followed by Male Wudde kebele with an AR of 68/10,000. These two kebeles have many pockets that are difficult to access by transportation, which makes it challenging to offer routine immunization.
Cases by Person
From a total of 140 cases, female cases account for 75 (54%). Regarding measles cases by age category 0–59 and 60–168 months were the most affected in the current outbreak with 54% and 24%, respectively. Figure 2 shows the number of measles cases by age category. All cases have Gamo ethnic backgrounds. The AR in males and females was 2.5/1000 population and 2.8/1000 population, respectively. In general, the AR was higher among 0–59 month’s old children (90/10,000). The total AR was 26 per 10,000 people, with a 0.7% case fatality rate (1 death/140 cases).
 |
Figure 2 Measles cases by age category in Garda Marta District of Gamo Zone, South Ethiopia, 2022. |
Cases by Time
The outbreak started on September 28, 2021, and ended on March 6, 2022. The first measles case was reported on October 12, 2021, from Marta Laddo kebele of Marta Garda District. The Epi curve contains several peaks with a propagated kind of transmission. The outbreak of measles in the Garda Marta District is seen in (Figure 3).
 |
Figure 3 Epidemiological curve of measles outbreak in Garda Marta District of Gamo Zone, South Ethiopia, 2022. |
Age and Sex Case Fatality Rate
From a total of 140 cases, a single measles-related death of a 9-month-old female patient was reported and the case fatality rate of the outbreak was 0.7%.
Symptom Development
All 140 cases developed measles symptoms like fever, maculopapular rash, cough, and runny nose. During active case search in the community, all cases we found were developed typical symptoms of the disease. The percentage of measles cases with signs and symptoms is shown in (Table 1).
 |
Table 1 Percentage of Measles Cases Who Developed Sign and Symptoms |
Vaccination Status of Cases
Ten (7%) of the 140 measles cases were not eligible for the MCV1 vaccine, while 63 (45%) were vaccinated for the first dose or more. Nearly half, 67(48%) of cases were not immunized against measles. Figure 4 depicts the vaccination status of measles patients.
 |
Figure 4 Vaccination status of measles cases in Garda Marta District of Gamo Zone, South Ethiopia, 2022. |
Public Health Interventions
Measles cases were treated with drugs (antibiotics, oral rehydration salt, tetracycline eye ointment, vitamin A, and Therapeutic Food (RUTF) for malnourished children) to prevent future transmission and reduce morbidity and mortality. The district conducted a vigorous measles case search and management effort in all afflicted kebeles until the final claim of zero reports was made. Measles prevention and control methods were promoted through health education and community involvement. Furthermore, as part of the outbreak response, children aged 6 months to 14 years received mass immunization.
Analytic Epidemiology
Socio-Demographic Characteristic
There were 51 cases and 102 controls in total, with a case-to-control ratio of 1:2. Males account for 51% and 54% of cases and controls, respectively. In the analysis, about 49% (25 of the cases) and 47% (48 of the controls) were in the age category of 1–4 years of age. Concerning occupation, 49% (25) of cases and 46% (47) of controls were farmers. Moreover, 49% (25) of cases and 46% (47) of controls have no formal education (Table 2).
 |
Table 2 Candidate Variables in Bivariate Logistic Regression for the Multivariate Analysis |
Vaccine Effectiveness
Vaccine efficacy (VE) was assessed in children aged 9 to 59 months, because the regular immunization in Ethiopia begins at 9 months. Analysis of case–control investigation data for children aged 9–59 months shows 39% (20/51) of cases compared to 21% (21/102) of controls had a history of measles vaccination (AOR: 0.402, 95% CI: 0.19–0.84) for vaccinated. Based on this information, the estimated measles VE was 60%. The following formula was used to calculate VE from the case–control study.32
Bivariate and Multivariate Analysis
Table 2 displays the bivariate analysis of all variables with COR and 95% CIs, and a p-value of <0.25 was used for multivariate analysis. All candidate variables selected from the bivariate analysis were entered into a logistic regression for multivariate analysis to identify the independent predictors of measles infection.
After controlling for potential confounding factors, five variables were found to be statistically associated with measles infections. Hence, being unvaccinated increases the likelihood of contracting measles by 2.84 (AOR: 2.84, 95% CI: 1.10–7.32) times compared to those who had a vaccination history. The odds of measles infections among individuals who had a travel history to the area were 4.24 folds (AOR: 4.24, 95% CI: 1.62–11.15) compared to those who had not traveled. Having a contact history with a measles case increases the odds of contracting measles by 6.34 (AOR: 6.34, 95% CI: 2.35–17.40) times compared to others who do not have a contact history with a measles case. Those who did not know the mode of measles transmission were about three (AOR: 2.68, 95% CI: 1.13–6.37) times more likely to have diseases as compared to those who knew the mode of transmission. Those who have moderate acute malnutrition were four times more likely to be infected with measles compared to the normal ones (AOR: 4.44, 95% CI: 1.74–11.31) (Table 3).
 |
Table 3 Variables Independently Associated with Measles Infection in Multivariable Logistic Regression |
Discussions
A total of 140 suspected Measles cases were reported from the Garda Marta District of Gamo Zone from October 12, 2021, to March 09, 2022, with an overall attack rate and case fatality rate of 26/10,000 and 0.7%, respectively. A high AR was observed in the age category of 0–59 months. This study findings were in line with the finding of studies conducted in Guji and Bale Zones of the Oromia Region.5,8 This might be due to the relatively high number of unvaccinated children and low effectiveness of the measles vaccine in the district, which makes <5 children more vulnerable. All cases (100%) developed measles symptoms like fever, maculopapular rash, cough, and runny nose.
The case fatality rate of this investigation was 0.7%, which is approximated by the measles outbreak investigation study conducted in Ginir (CFR = 0.5%)24 and India (CFR = 0.78%).33
Our study finding was lower than the result of study finding conducted in India and Ethiopia33,34 and also lower compared with the expected CFR from measles between 3% and 6% in Ethiopia.1 Low CFR could be due to deaths not being registered at the community level, whereas, the data only count deaths at the health facility level. Moreover, it might be due to the establishment of a strong clinical case management system during an outbreak.
However, WHO34 recommends achievement and maintenance of MCV2 Vaccination coverage ≥95% supported by supplementary immunization activities to eliminate measles, the average achievement of the district for MCV1 was 85% for the last four consecutive years (2018–2021 GC). Therefore, this achievement is lower than the WHO cut point and it is not likely to develop herd immunity in the community. As a result, outbreaks of vaccine-preventable diseases are more likely to occur in low-performing districts. The estimated vaccine effectiveness of our investigation was 60% among cases observed in children in the age group of 9–59 months. This number is below the standard cut point of WHO. This finding was also less than the study conducted in South Eastern and southwestern Ethiopia.8,24,35
Low performance (<85%) of vaccine effectiveness in the district might be because of factors like poor vaccine storage, transportation, and poor cold chain management. Moreover, there was no refrigerator at kebeles where an outbreak occurred, as a result, vaccines were transported by motorcycle or foot from cluster health centers to kebeles with vaccine carriers and then stay for more than six hours in the vaccination site without changing ice packs in high environmental temperature.
Several factors were associated with measles outbreak in the current study. For example, the possibility of contracting measles was about 3 times more likely in those who were unvaccinated than in those who have a vaccination history. Our study finding is similar with the study conducted in Ethiopia, Nigeria, and Zimbabwe where the number of unvaccinated increased by 5, 14, and 3 times, respectively.24,36,37 Low average coverage of MCV1 in the last four consecutive years in the district might have contributed to this. As low coverage increases susceptibility to measles infection, high coverage with two doses of the measles vaccine ensures herd immunity and decreases the spread of infection.35
Individuals who had a history of traveling 7–18 days before the onset of illness to a measles-active area were 4.24 times more likely to have measles compared to their counterparts. Our study findings are similar to the results of the study conducted in northern Ethiopia and China.34,38 The justification for this result is that, as measles is highly contagious and transmitted from person to person, travelers are more susceptible to measles.
Having a history of contact with a confirmed measles case increases the odds of contracting measles by about six times, compared to those who do not have contact with a measles case. Our findings are consistent with studies conducted in the Bale Zone of the Oromia region and Oromia Zone of the Amhara region where risks increased by 3.24 and 3 times, respectively.34,39 This is due to the fact that the virus is highly contagious and being transferred through direct or indirect contact with infected people’s respiratory secretions, which enhances the spread of measles transmission.
Individuals whose mothers/caregivers do not know the mode of transmission of measles are 2.68 times more likely to be infected than their counter parts. Consistent results were reported by previous similar studies conducted in Ethiopia.40,41
Moderate acute malnutrition increases the likelihood of measles infection. This outbreak investigation result is in line with a study conducted in southeastern Ethiopia, Yemen, and northeastern Ethiopia.8,42,43 Evidences from previous studies conducted in India and Nigeria found a link between measles and malnutrition that malnourished children are more likely than well-nourished children to get severe measles infections.2,44
Strengths and Limitations of the Study
The study revealed the specific causes of the confirmed measles outbreak in the study area, which is the strength of the study. Recall bias during data collection for variables like immunization status and the number of vaccination doses taken can be a limitation. The other challenge was the incompleteness of immunization registration data and the absence of child immunization cards.
Conclusions
This outbreak highly affected Marta Laddo Kebele and children of ages 0–59 months, with highest attack rates. Factors statistically significantly associated with measles outbreak in the district were being unvaccinated, travel history to active measles case sites, having a contact history with measles cases, the knowledge of caretakers/mothers on the mode of transmission and acute malnutrition. Therefore, strengthening routine immunization, including SIA, in the affected kebeles, improving vaccine effectiveness by improving cold chain management, vaccine storage, and transportation, and promoting awareness of the importance of vaccinating children are important preventive measures that should be implemented to prevent and control measles outbreak. In addition, local planners and other partners should consider neglected residents living in pocket areas in the district, especially in terms of access to efficient and sustainable routine immunization services. Moreover, other cohort study designs might be employed to identify other factors that our study could not address.
Abbreviations
AR, Attack Rate; CFR, Case Fatality Rate; PHEM, Public Health Emergency Management; GAVI, Global Alliance for Vaccine Initiative; IgM, Immunoglobulin M; MCV1, Measles-Containing-Vaccine first-dose; MCV2, Measles-Containing-Vaccine second-dose; SIAs, Supplemental Immunization Activities; WHO-AFR, World Health Organization in the African Region; UNICEF, United Nations Child Fund; WHO, World Health Organization.
Acknowledgments
We are also grateful to the Ethiopian Field Epidemiology and Laboratory Training Program and Hawassa University. Our appreciation also goes to PHEM officers of the Gamo Zone Health Department and Garda Marta District Health Office for their cooperation in this study. Finally, we would thank the study participants without whom this finding could not be made.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. EPHI. Public health emergency management guidelines for Ethiopia; 2012. Available from: https://www.ephi.gov.et/images/guidelines/phem-guideline-final.pdf.
2. EHNRI. Guideline on measles surveillance and outbreak management. Third edition. Addis Ababa, Ethiopia; 2012. Available from: https://www.ephi.gov.et/images/guidelines/guideline-on-measles-surveillance-and-outbreak-management2012.pdf.
3. WHO. African regional guidelines for measles and rubella surveillance. Geneva; 2015. Available from: https://www.afro.who.int/sites/default/files/2017-06/who-african-regional-measles-and-rubella-surveillance-guidelines_updated-draft-version-april-2015_1.pdf.
4. WHO. Guidelines for epidemic preparedness and response to measles outbreaks. Geneva 27, Switzerland: World Health Organization; 1999. Available from: https://apps.who.int/iris/handle/10665/66034.
5. Belda K, Tegegne AA, Mersha AM, Bayenessagne MG, Hussein I, Bezabeh B. Measles outbreak investigation in Guji zone of Oromia Region, Ethiopia. Pan Afr Med J. 2017;27(Suppl 2). doi:10.11604/pamj.supp.2017.27.2.10705
6. Africa WROf. World Health Organization. Congo (Brazzaville): 2011 measles elimination by 2020: a strategy for the African region report of the secretariat. Available from: https://wwwafrowhoint/sites/default/files/sessions/working_documents/AFR-RC61-8-Measles-elimination-by-2020---strategy-forthe-African-Region---with-Resolutionpdf.
7. Rachlin A, Danovaro-Hilliday MC, Murphy P, Sodha SV, Wallace AS; CDC. Routine vaccination coverage — worldwide, 2021. MMWR Morb Mortal Wkly Rep. 2022;71:1396–1400. doi:10.15585/mmwr.mm7144a2
8. WHO. National immunization coverage scorecards estimate for 2019. Geneva: World Health Organization; 2020. License: CC BY-NC-SA 3.0 IGO. Available from: https://apps.who.int/iris/rest/bitstreams/1321938/retrieve.
9. Patel MK, Goodson JL, Alexander JP, et al.; CDC. Progress toward regional measles elimination — worldwide, 2000–2019. MMWR Morb Mortal Wkly Rep. 2020;69(45):1700–1705. doi:10.15585/mmwr.mm6945a6
10. World Health Organization. Measles fact sheet: Switzerland, Geneva; 2019. Available from: https://www.who.int/news/item/15-05-2019-new-measles-surveillance-data-for-2019.
11. Centers for disease control and prevention. Global measles and rubella updates; 2022.
12. World Health Organization. Emergencies preparedness and response. Measles-global situation; 2019. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/WHO%20_%20Measles%20%E2%80%93%20Global%20situation.pdf.
13. World Health Organization. World Health Organization regional office for Africa; 2022. Available from: https://www.afro.who.int/news/vaccine-preventable-disease-outbreaks-riseafrica#:~:text=Almost%2017%20500%20cases%20of,first%20three%20months%20of%202021.
14. Ethiopia Public Health Training Initiative. Expanded program in immunization: for the Ethiopian health center team. Gondar University College; 2002. Available from: https://www.cartercenter.org/resources/pdfs/health/ephti/library/modules/Degree/Mod_Exp_Imm_final.pdf.
15. World Health Organization. World Health Organization vaccine-preventable diseases: monitoring system. 2019 global summary; 2019. Available from: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=ETH.
16. Ethiopian Public Health Institute (EPHI) and ICF. Ethiopia Mini-Demographic and Health Survey 2019: Key Indicators. EPHI and ICF International; 2019.
17. Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic Health Survey 2016. Central Statistics Agency and ICF International; 2016.
18. Ethiopia National Expanded Program on Immunization. Comprehensive multi-year plan 2016–2020. Addis Ababa: Federal Ministry of Health; 2015 Available from: https://extranet.who.int/countryplanningcycles/sites/default/files/country_docs/Ethiopia/ethiop_cmyp_latest_revised_may_12_2015.pdf.
19. WHO. Immunization agenda 2030. World Health Organization; 2018. Available from: https://www.who.int/immunization/immunization_agenda_2030/en/.
20. Chung E-K, Rhee J-A, Baik Y-H. The effect of team-based learning in medical ethics education. Med Teach. 2009;31(11):1013–1017.
21. WHO. Regional Office for Europe. Guidelines for measles and rubella outbreak investigation and response in the WHO European region; 2013. Available from: https://www.euro.who.int/__data/assets/pdf_file/0003/217164/OutbreakGuidelines-updated.pdf.
22. W/Kidan F, Getachew D, Mekonnen B, Woldeselassie Hammeso W. Risk factors of measles outbreak among students of Mizan-Tepi University, Tepi Campus, Southwest Ethiopia. Infect Drug Resist. 2021;Volume 14:963–970. doi:10.2147/IDR.S296928
23. Kalil FS, Gemeda DH, Bedaso MH, Wario SK. Measles outbreak investigation in Ginnir district of Bale zone, Oromia region, Southeast Ethiopia, May 2019. Pan Afr Med J. 2020;36:1. doi:10.11604/pamj.2020.36.20.21169
24. EPHTI Hailu D, Alano A, G/Mariam A, Abicho T. Measles; for the Ethiopian health center team; 2005. Ethiopia public health training initiative, the carter center, the Ethiopia ministry of health, and the Ethiopia ministry of education. Available from: https://www.cartercenter.org/resources/pdfs/health/ephti/library/modules/degree/mod_measles_final.pdf.
25. Dabbagh A, Laws RL, Steulet C, et al.; CDC. Progress toward regional measles elimination — worldwide, 2000–2017. MMWR Morb Mortal Wkly Rep. 2018;67(47):1323–1329. doi:10.15585/mmwr.mm6747a6
26. WHO. WHO-GAVI Joint Statement: Ethiopia Launches Measles Vaccine’s Second Dose on 11th February 2019. Addis Ababa, Ethiopia; 2012.
27. World Health Organization. Global Measles and Rubella Update November 2018. Geneva, Switzerland: WHO; 2018.
28. WHO Ethiopia World Health Organization. Health cluster bulletin #7; 2019.
29. World Health Organization. Regional office for the western Pacific. Measles elimination field guide. Available from: https://apps.who.int/iris/handle/10665/207664.
30. Nelson A. Coordinated effort needed to improve health care quality. QA Rev. 1989;1(5):1.
31. Majwala RK, Nakiire L, Kadobera D, et al. Measles outbreak propagated by children congregating at water collection points in Mayuge District, eastern Uganda, July–October, 2016. BMC Infect Dis. 2018;18:1–7. doi:10.1186/s12879-018-3304-5
32. Orenstein WA, Bernier RH, Dondero TJ, et al; WHO. Field evaluation of vaccine efficacy. Bull World Health Organ. 1985;63(6):1055–1068. PMID: 3879673; PMCID: PMC2536484.
33. Murhekar MV, Ahmad M, Shukla H, et al. Measles case fatality rate in Bihar, India, 2011–12. PLoS One. 2014;9(5):e96668. doi:10.1371/journal.pone.0096668
34. Tariku MK, Misikir SW. Measles outbreak investigation in Artuma Fursi Woreda, Oromia zone, Amhara region, Ethiopia, 2018: a case control study. BMC Res Notes. 2019;12:1–6. doi:10.1186/s13104-019-4806-y
35. Bekele BB, Legese T, Daniel A, Kumalo A, Yimam H, Lamaro T. Determinants of measles recurrent outbreak in South West Ethiopia: an obstacle for implementation of infectious disease eradication in the country. EC Microbiol. 2018;14(10):699–706.
36. Babalola OJ, Ibrahim IN, Kusfa IU, et al. Measles outbreak investigation in an urban slum of Kaduna Metropolis, Kaduna State, Nigeria, March 2015. Pan Afr Med J. 2019;32(1). doi:10.11604/pamj.2019.32.150.15764
37. Pomerai KW, Mudyiradima RF, Gombe NT. Measles outbreak investigation in Zaka, Masvingo province, Zimbabwe, 2010. BMC Res Notes. 2012;5(1):1–6. doi:10.1186/1756-0500-5-687
38. Wagner AL, Boulton ML, Gillespie BW, et al. Risk factors for measles among adults in Tianjin, China: who should be controls in a case-control study? PLoS One. 2017;12(9):e0185465. doi:10.1371/journal.pone.0185465
39. Tsegaye G, Gezahagn Y, Bedada S, Berhanu N, Gudina G, Mulatu G. Epidemiology of measles in Bale Zone, Southeast Ethiopia: analysis of surveillance data from 2013 to 2019. Risk Manag Healthc Policy. 2021;Volume 14:4093–4103. doi:10.2147/RMHP.S325173
40. Abebe AM, Mengistu T, Mekuria AD. Measles case, immunization coverage and its determinant factors among 12–23 month children, in Bassona Worena Woreda, Amhara Region, Ethiopia, 2018. BMC Res Notes. 2019;12:1–6. doi:10.1186/s13104-019-4104-8
41. Kassahun MB, Biks GA, Teferra AS. Level of immunization coverage and associated factors among children aged 12–23 months in Lay Armachiho District, North Gondar Zone, Northwest Ethiopia: a community based cross sectional study. BMC Res Notes. 2015;8:1–10. doi:10.1186/s13104-015-1192-y
42. Nassar AAH, Al Amad MA, Qasim M, Dureab F. Risk factors for measles outbreak in Ataq and Habban districts, Shabwah governorate, Yemen, February to May 2018. BMC Infect Dis. 2021;21(1):551. doi:10.1186/s12879-021-06207-3
43. Ayele WM. Malnutrition precipitated measles outbreak in Gewane District, Afar Regional State, Northeastern Ethiopia, 2016; 2020.
44. Ogbu TJ. Severity of measles in malnutrition. Nutr Rev. 1982;40(7):203–205. doi:10.1111/j.1753-4887.1982.tb05310.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
