Back to Journals » Journal of Pain Research » Volume 16
Manual Palpation versus Ultrasound to Identify the Intervertebral Space for Spinal Anesthesia in Infants
Authors Du J, Roth C , Dontukurthy S , Tobias JD , Veneziano G
Received 6 October 2022
Accepted for publication 4 January 2023
Published 10 January 2023 Volume 2023:16 Pages 93—99
DOI https://doi.org/10.2147/JPR.S392438
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ellen M Soffin
Joanne Du,1 Catherine Roth,2 Sujana Dontukurthy,3 Joseph D Tobias,2,4 Giorgio Veneziano2,4
1The Ohio State University College of Medicine, Columbus, OH, USA; 2Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA; 3Department of Anesthesiology, Valley Children’s Hospital, Madera, CA, USA; 4Department of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
Correspondence: Giorgio Veneziano, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, 700 Children’s Dr, Columbus, OH, 43205, USA, Tel + 1 614-722-4200, Email [email protected]
Purpose: Awake spinal anesthesia continues as an alternative to general anesthesia for infants. Standard clinical practice includes the manual palpation of surface landmarks to identify the desired intervertebral space for lumbar puncture (LP). The current study investigates the accuracy of manual palpation for identifying the intended intervertebral site for LP, using ultrasonography for confirmation and to determine the interspace where the conus medullaris ends.
Patients and Methods: After informed parental consent, patients less than one year of age undergoing spinal anesthesia for lower abdominal, urologic, or lower extremity surgical procedures were included. Patients were held in the seated position and an attending pediatric anesthesiologist or pediatric anesthesiology fellow declared the vertebral interspace intended for needle insertion, palpated surface landmarks, and placed a mark at the site. A research anesthesiologist then determined the actual vertebral interspace of the marked site and the location of the conus medullaris using ultrasonography. The time to complete both techniques (manual palpation and ultrasonography) was recorded.
Results: The study cohort included 50 infants (median age of 7 months). Sixteen vertebral interspaces (32%) were inaccurately marked. One was marked two spaces higher than intended, ten were marked one space higher than intended, and five were marked one space lower than intended. In one patient, the intended vertebral interspace for the lumbar puncture overlaid the conus medullaris. The median time required was 25 seconds (IQR 14.3, 32) for palpation and 39 seconds (IQR 29, 63.8) for ultrasonography.
Conclusion: Manual palpation of surface landmarks to determine the correct interspace for LP for spinal anesthesia in infants is inaccurate. The time required to perform spinal ultrasonography in infants for determination of the optimal site for LP is brief and may be useful in ensuring accurate identification of the correct interspace and the location of the conus medullaris.
Keywords: spinal anesthesia, infant, ultrasonography, palpation, lumbar puncture, conus medullaris
Introduction
Spinal anesthesia remains a recognized and acceptable technique as an alternative to general anesthesia for sub-umbilical and lower extremity surgical procedures in infants. Although initially used to avoid the adverse physiologic effects of general anesthesia in patients with comorbid conditions or to avoid apnea following halothane anesthesia, there has been a renewed interest in its use given the potential long-term neurocognitive impact of general anesthetic agents in this population.1–6 Additionally, several other physiologic and postoperative benefits have been demonstrated with spinal anesthesia in infants, including avoidance of airway instrumentation, a decreased incidence of adverse cardiopulmonary outcomes, and cost savings when compared to general anesthesia.7,8
Performance of spinal anesthesia requires lumbar puncture (LP), identification of the intrathecal space, and injection of a local anesthetic agent (0.5% bupivacaine or ropivacaine). Current clinical practice for identifying the intervertebral space for spinal anesthesia is manual palpation. The anatomical landmarks for spinal anesthesia include palpating the iliac crests and identification of the intercristal line (Tuffier’s line) which bisects the L4 vertebral body or the L4-L5 intervertebral space depending on the patient’s age.9 Manual palpation may be inaccurate and high needle placement at or above the level of the conus medullaris has the potential for morbidity, including neurologic damage.10–14 While the incidence of spinal cord injury associated with infant spinal anesthesia is unknown, the practice appears safe as evidenced by the lack complications cited by multiple pediatric regional anesthesia databases.2,15 Despite the rarity, spinal cord injury from direct needle trauma or intramedullary injection of local anesthetic can be potentially devastating.16 Ultrasonography may provide a more precise method to identify the appropriate intervertebral interspace for spinal anesthesia and minimize the number of attempts for LP.
In this prospective study, we sought to assess the accuracy of manual palpation in identifying the intended intervertebral space for LP in infants undergoing spinal anesthesia. Ultrasonography was used prior to needle insertion to determine the intervertebral space identified using surface landmarks and to assess the location of the conus medullaris.
Methods
This prospective study was approved by the Institutional Review Board of Nationwide Children’s Hospital (STUDY00000558), registered at clinicaltrials.gov (NCT04757805), and conducted in accordance with the Declaration of Helsinki. Patients less than one year of age scheduled for spinal anesthesia for lower abdominal, urologic, or lower extremity surgery were eligible. Informed consent was obtained from a parent or guardian after the patient’s arrival in the pre-operative room. In the operating room, the patient was placed in a sitting position in preparation for spinal anesthesia. The clinical anesthesia provider (pediatric anesthesiology attending or fellow) used manual palpation to identify the desired interspace for spinal needle insertion, which was selected at their discretion. The vertebral interspace chosen was declared to the research team and then marked with a pen. Subsequently, ultrasound identification of the intervertebral space was performed by a research anesthesiologist experienced in ultrasound imaging of the spine. The imaging was performed using a 6–13 MHz linear probe placed midline in the transverse plane starting at the top of the gluteal crease, identifying the sacrum, and then moving in the cephalad direction. From there, the intervertebral spaces were counted in the cephalad direction until the marked, intended space was reached. The vertebral interspace of the provider’s mark determined utilizing ultrasound was recorded and compared against the interspace declared. Additionally, the interspace where the conus medullaris terminated was identified by ultrasound. The time required to perform the manual palpation and the ultrasonography was documented by research staff in minutes and seconds. Timing started when palpation of the patient’s back began or when the ultrasound probe was placed on the patient’s back and stopped when the level of the vertebral interspace was verbally declared with either method. Subsequent anesthetic management did not vary from standard technique and was at the discretion of the anesthesia team, generally following our previously described practice for spinal anesthesia.17 Ultrasound was solely used for scanning of anatomical landmarks prior to performance of the lumbar puncture and not real-time ultrasound guidance during insertion of the needle. The clinical anesthesia provider was aware of the results obtained by spinal ultrasonography and made final determination of the site for needle insertion.
The accuracy of and time to complete manual palpation compared to ultrasonography was analyzed by patient variables, such as age, and provider variables, such as provider level. We calculated the number and percentage for categorical data and the mean, standard deviation (SD), median and interquartile range (IQR) for continuous data. Clinical choice of intervertebral space marked by attending anesthesiologist or fellow was compared using Fisher’s exact test. Accurate intervertebral space marked compared to inaccurate space marked categorized by age group was completed using Chi-square analysis. Time to complete the clinical choice of the intervertebral space and ultrasonography were compared using a paired t-test. Time to complete the clinical choice between provider types was compared using independent samples t-test. Manual palpation time and ultrasound time between age groups defined as 0–3 months, 3–6 months, 6–9 months, and 9–12 months were conducted using ANOVA tests. Statistical significance between length of patient and vertebral level of conus medullaris was compared using Pearson correlation. Statistical tests were performed using SPSS and SAS version 9.4 software (SAS Institute Inc).
Results
The study cohort included 50 patients under one year of age who underwent spinal anesthesia for lower abdominal and urologic surgery over a 9 month period. Age ranged from 2 to 12 months with a median age of 7 months (IQR 5, 9). Median patient weight was 7.8 kg (IQR 6.8, 9.0). All patients included in the cohort were male. Twenty-nine patients (58%) were assigned ASA class I, eighteen patients (36%) ASA class II, and three patients ASA class III (Table 1). Common surgical indications included elective circumcision, inguinal hernia, chordee, hidden penis, phimosis, and hypospadias. Examples of patient co-morbidities included prematurity, gastroesophageal reflux disease, ventricular septal defect, bronchopulmonary dysplasia, and hypopituitarism.
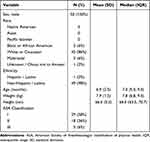 |
Table 1 Patient Characteristics (n=50) |
Manual palpation was performed by an attending pediatric anesthesiologist in 36 (72%) patients and by a pediatric anesthesiology fellow in 14 (28%) patients. Median years of experience in performing pediatric spinal anesthesia was five years (IQR 3, 10).
The clinical provider declared the intended, marked vertebral interspace as L4-5 in 24 instances, L3-4 in 25 instances, and L2-3 in one case (Table 2). Ultrasonography of the spine revealed that 16 of the 50 (32%) marked sites were at vertebral interspaces that did not correlate with the interspace declared by the clinical provider. Sites marked by attendings resulted in 12 of 36 (33%) inaccurate manual palpations and for fellows accounted for 4 of 14 (29%) inaccurate manual palpations. There was no statistical difference between these groups. When accounting for age groupings for manual palpations, zero of three (0%) were marked inaccurately for the 0–3 month age range, two of 13 (15%) were inaccurate for the 3–6 month age range, 12 of 22 (55%) were inaccurate for the 6–9 month range, and two of 12 (17%) were inaccurate for the 9–12 month range. There was a statistically significant difference between age groups (p = 0.023).
 |
Table 2 Characteristics of Procedure |
Among the vertebral interspaces incorrectly identified, 11 marked sites were more cephalad than intended by the clinical provider. Ten were more cephalad by one interspace and one site was more cephalad than intended by two interspaces. In the case marked incorrectly by two cephalad spaces, the marked space was indicated as L4-L5 when the actual space was L2-L3. Five of the 15 marked sites were declared more caudad than the actual space, with all five being marked as L3-L4 when the actual space was L4-L5. The actual intervertebral spaces that were marked as determined by ultrasonography were L4-5 in twenty-one patients (42%), L3-4 in twenty-four patients (48%) and L2-3 in five patients (10%) infants. The interspace where the conus medullaris terminated was T12-L1 in nine (18%), L1-L2 in twenty-seven (54%), L2-L3 in nine (18%), L3-L4 in three (6%), and unable to be obtained in two (4%) patients. There was only one patient in whom the intended, marked vertebral interspace for the LP overlay the conus medullaris.
The median time required to mark by manual palpation was 25 seconds (IQR 14, 32) compared to 38.5 seconds (IQR 29, 64) to perform ultrasonography (p < 0.001). The median time for an attending pediatric anesthesiologist to palpate was 20 seconds (IQR 13, 32) and 29 seconds for a pediatric anesthesiology fellow (IQR 23, 36) (p = 0.383). There was no statistically significant difference between age groups 0–3 months, 3–6 months, 6–9 months, 9–12 months in time to palpate (p = 0.884) or to perform ultrasonography (p = 0.064). There was a correlation between length of the patient and anatomical level of the conus medullaris with increased patient length in centimeters correlating with more cephalad vertebral interspace termination of the conus medullaris (p = 0.023).
Discussion
In this prospective study, our results demonstrate that the use of manual palpation for the determination of the intervertebral space for infant spinal anesthesia is often unreliable, with nearly one-third (32%) of infants experiencing inaccurate identification of the intended site. In infants, with more caudal termination of the conus medullaris, this unreliability could lead to an increased risk of spinal cord injury.18 Although reports of injury are exceedingly rare, the increasing clinical applications of spinal anesthesia in infants and potentially catastrophic nature of the spinal cord injury provide further impetus to discovering more accurate methods of intervertebral space identification in this population.
The majority of patients in this study were found to have the conus medullaris terminating above the L2-L3 interspace; however, as has been noted in other studies using various techniques for radiologic imaging, there is significant variation in the anatomy of the spinal cord and its relationship to the vertebral column with the spinal cord ending at L3 at birth and approaching L1 by 6–12 months.6 In our cohort of 50 infants, the conus medullaris was identified at vertebral levels varying from T12-L1 to L3-4.
During the course of this study, the potentially enhanced safety of utilizing spinal ultrasonography was demonstrated in one patient in which the attending anesthesiologist declared the intended, marked interspace as L3-4, but ultrasonography revealed the site to be L2-3 with a visible conus medullaris. The conus medullaris existing in the same space as the marked intervertebral space was interpreted as a risk for needle entry into the spinal cord in this patient. The anesthesiologist was made aware of the situation and the lumbar puncture for spinal anesthesia was performed uneventfully at a lower interspace level.
The difference in time to perform manual palpation and ultrasonography, although statistically significant, was not clinically significant in that both techniques typically required less than a minute. While ultrasonography requires special equipment and probe preparation, the time required to perform the assessment is not a barrier to use in this manner when performed by practitioners experienced with ultrasound-guided regional anesthesia. However, it should be recognized that as part of this clinical research study, the ultrasound of the vertebral column was performed by a pediatric anesthesiologist with advanced training in regional anesthesia and ultrasonography. As an advanced skill, there are time and education commitments required to learning and maintaining skills with ultrasonography.
Accurate identification of vertebral levels by surface landmarks has been shown to be generally inaccurate in adults.10–12 However, few studies exist examining the accuracy of landmark palpation in determining vertebral levels in infants or children. One observational study found that 37% of assessments in children 0–12 years of were inaccurate by ≥1 vertebral level.19 Baxter et al found that the potential sites for LP were identified as more cephalad than intended in 11 of 30 neonates in the lateral position.20
Ultrasonography has previously been demonstrated as a valuable pre-procedural tool in infants undergoing LP, allowing visualization of reference structures, such as the dura mater, intrathecal space, nerve roots, and the conus medullaris. Ultrasound imaging prior to needle insertion can significantly increase the incidence of successful LP in infants.21,22 Descriptions of the applications of ultrasonography for spinal anesthesia in infants are less abundant. Cristiani et al performed spinal ultrasonography on 14 pre-term infants weighing 1575–5800 grams to identify a suitable needle insertion site for spinal anesthesia. Spinal anesthesia was successful in 86% of patients within three attempts without complications.23 Hayes et al compared manual palpation and ultrasound for accuracy in identifying the L3-4 intervertebral space for spinal anesthesia in 30 children less than 12 years of age.19 The two methods were assessed using fluoroscopy for confirmation. Inaccurate assessment (≥ 1 level) by the landmark palpation occurred in 37% of cases compared to 27% with ultrasonography. Less experienced anesthesiologists (residents and fellows) made a disproportionate number of inaccurate measurements compared to consultants. The BMI-for-age percentile and weight-for-length percentile were higher in patients in whom either technique was inaccurate. Ultrasound-guidance has has been demonstrated as beneficial for various other pediatric regional anesthetic techniques. Dorsal penile nerve blocks (DPNB) were frequently administered by the landmark technique for hypospadias surgery prior to the implementation of US-guided DPNB with in-plane technique that Yiğit et al described as being effective in identifying the dorsal nerve without harm to the penile structures.24 Ozen et al recommended caudal block under ultrasound guidance to prevent unsuccessful interventions by allowing caudal site visualization, particularly in pediatric patients whose sacral horns are difficult to palpate.25
Our study differs by investigating the accuracy of palpation of surface landmarks for spinal anesthesia in a larger cohort comprised exclusively of infants. Notably, the quality of ultrasound imaging of the spine changes considerably after the first year of life. Infants, due to incomplete ossification of the vertebra, have spines which allow greater ultrasound beam penetration resulting in enriched acoustic windows (Figure 1). The enhanced visual detail may facilitate ascertainment of vertebral level in infants compared to older children. This investigation used ultrasonography for confirmation of the intervertebral level indicated by the clinical provider, rather than attempting to examine the accuracy of the ultrasound method itself. The research anesthesiologists performing the ultrasonography in this investigation were experienced with neuraxial imaging. Additionally unique to this study is that the clinical providers were not asked to identify a certain vertebral interspace, but continued to follow their standard clinical practice for identifying an appropriate needle insertion site, choosing it based on their own clinical practice. The result was a variety of intended interspaces including one practitioner who chose the L2-3 interspace, emphasizing a spectrum of clinical practice exists amongst pediatric anesthesiologists when administering spinal anesthesia to infants.
 |
Figure 1 Ultrasound imaging in the transverse view of neonatal spine. (A) Below the conus medullaris. (B) Above the conus medullaris. |
Our study cohort consisted of a largely healthy, completely male population which may limit conclusions about generalizability. The entire cohort in this study were males presenting for urological procedures, with the most common procedures being circumcision/circumcision repair (26%) and hidden penis repair (26%). Other procedures included inguinal hernia, orchiopexy, chordee release, cystoscopy, and hypospadias repair. The 100% male study cohort occurred by chance and can be further explained by the predominance of urologic surgeries occurring in males in the infant population as well as our clinical practice where spinal anesthesia is offered to this patient population given the preference of our surgical colleagues. The ultrasonography used to determine the intervertebral space identified via manual palpation was not correlated with other radiographic techniques; however, ultrasonography was successfully performed in less than one minute in all patients with no question regarding its accuracy. In addition, our research anesthesiologists had experience with neuraxial ultrasonography, which may not be the case with all providers and may limit the ability to apply this method broadly.
This prospective observational study of infants undergoing spinal anesthesia highlights the inaccuracy of manual palpation in identifying the intended intervertebral space for needle entry. With the majority of our cohort having their conus medullaris detectable until L2-L3 level, the risk of inadvertent spinal cord puncture remains a potential concern. Given that time to perform ultrasonography paralleled that of manual palpation, ultrasonography offers a viable and more accurate alternative to identify the appropriate interspace for spinal anesthesia.
Data Sharing Statement
Data supporting the results reported in this study are stored in a secure, password-protected electronic database. Access to supporting data is available upon reasonable request by contacting the corresponding author.
Ethical Approval and Clinical Trial Registration
This study was approved by the Institutional Review Board of Nationwide Children’s Hospital (STUDY00000558) and registered at clinicaltrials.gov (NCT04757805).
Patient Consent Statement
Participation in this study was voluntary and proceeded only after informed, written consent was obtained from the patient’s parent or legal guardian.
Funding
No funding sources to disclose for this study.
Disclosure
The authors have no conflicts of interest in this work.
References
1. Tobias JD. Spinal anesthesia in infants and children. Paediatr Anaesth. 2000;10:5–16. doi:10.1046/j.1460-9592.2000.00460.x
2. Williams RK, Adams DC, Aladjem EV, et al. The safety and efficacy of spinal anesthesia for surgery in infants: the Vermont infant spinal registry. Anesth Analg. 2006;102:67–71. doi:10.1213/01.ANE.0000159162.86033.21
3. Abajian JC, Mellish RW, Browne AF, Perkins FM, Lambert DH, Mazuzan JE
4. Welborn LG, Rice LJ, Hannallah RS, Broadman LM, Ruttimann UE, Fink R. Postoperative apnea in former preterm infants: prospective comparison of spinal and general anesthesia. Anesthesiology. 1990;72:838–842. doi:10.1097/00000542-199005000-00012
5. Whitaker EE, Wiemann BZ, DaJusta DG, et al. Spinal anesthesia for pediatric urological surgery: reducing the theoretic neurotoxic effects of general anesthesia. J Pediatr Urol. 2017;13:396–400. doi:10.1016/j.jpurol.2017.06.006
6. Verma D, Naithani U, Gokula C, Harsha H. Spinal anesthesia in infants and children: a one year prospective audit. Anesth Essays Res. 2014;8:324–329. doi:10.4103/0259-1162.143124
7. McCann ME, Withington DE, Arnup SJ, et al.; GAS Consortium. Differences in blood pressure in infants after general anesthesia compared to awake regional anesthesia (GAS study-A prospective randomized trial). Anesth Analg. 2017;125:837–845. doi:10.1213/ANE.0000000000001870
8. Davidson AJ, Morton NS, Arnup SJ, et al. General anesthesia compared to Spinal anesthesia (GAS) Consortium. Apnea after awake regional and general anesthesia in infants: the general anesthesia compared to spinal anesthesia study--comparing apnea and neurodevelopmental outcomes, a randomized controlled trial. Anesthesiology. 2015;123:38–54. doi:10.1097/ALN.0000000000000709
9. Goyal R, Jindal K, Baj B, Singh S, Kumar S. Pediatric spinal anesthesia. Indian J Anaesth. 2008;52:264–270.
10. Whitty R, Moore M, Macarthur A. Identification of the lumbar interspinous spaces: palpation versus ultrasound. Anesth Analg. 2008;106:538–540. doi:10.1213/ane.0b013e31816069d9
11. Hosokawa Y, Okutomi T, Hyuga S, Kato R, Kuczkowski KM. The concordance rate of L3/4 intervertebral lumbar level estimated by palpation and ultrasonography in Japanese parturients. J Matern Fetal Neonatal Med. 2020;33:2354–2358. doi:10.1080/14767058.2018.1550063
12. Duniec L, Nowakowski P, Kosson D, Łazowski T. Anatomical landmarks based assessment of intravertebral space level for lumbar puncture is misleading in more than 30%. Anaesthesiol Intensive Ther. 2013;45:1–6. doi:10.5603/AIT.2013.0001
13. Agarwal A, Kishore K. Complications and controversies of regional anaesthesia: a review. Indian J Anaesth. 2009;53:543–553.
14. Hamandi K, Mottershead J, Lewis T, Ormerod IC, Ferguson IT. Irreversible damage to the spinal cord following spinal anesthesia. Neurology. 2002;59:624–626. doi:10.1212/WNL.59.4.624
15. Walker BJ, Long JB, Sathyamoorthy M, et al. Pediatric regional anesthesia network investigators. Complications in pediatric regional anesthesia: an analysis of more than 100,000 blocks from the pediatric regional anesthesia network. Anesthesiology. 2018;129(4):721–732. doi:10.1097/ALN.0000000000002372
16. Reynolds F. Damage to the conus medullaris following spinal anaesthesia. Anaesthesia. 2001;56(3):238–247. doi:10.1046/j.1365-2044.2001.01422-2.x
17. Trifa M, Tumin D, Whitaker EE, Bhalla T, Jayanthi VR, Tobias JD. Spinal anesthesia for surgery longer than 60 min in infants: experience from the first 2 years of a spinal anesthesia program. J Anesth. 2018;32:637–640. doi:10.1007/s00540-018-2517-5
18. Kelleher S, Boretsky K, Alrayashi W. Images in anesthesiology: use of ultrasound to facilitate neonatal spinal anesthesia. Anesthesiology. 2017;126(3):561. doi:10.1097/ALN.0000000000001468
19. Hayes J, Borges B, Armstrong D, et al. Accuracy of manual palpation vs ultrasound for identifying the L3-L4 intervertebral space level in children. Paediatr Anaesth. 2014;24:510–515. doi:10.1111/pan.12355
20. Baxter B, Evans J, Morris R, et al. Neonatal lumbar puncture: are clinical landmarks accurate? Arch Dis Child Fetal Neonatal Ed. 2016;101:F448–50. doi:10.1136/archdischild-2015-308894
21. Neal JT, Kaplan SL, Woodford AL, Desai K, Zorc JJ, Chen AE. The effect of bedside ultrasonographic skin marking on infant lumbar puncture success: a randomized controlled trial. Ann Emerg Med. 2017;69(5):610–619. doi:10.1016/j.annemergmed.2016.09.014
22. Gorn M, Kunkov S, Crain EF. Prospective investigation of a novel ultrasound-assisted lumbar puncture technique on infants in the pediatric Emergency Department. Acad Emerg Med. 2017;24:6–12. doi:10.1111/acem.13099
23. Cristiani F, Henderson R, Lauber C, Boretsky K. Success of bedside ultrasound to identify puncture site for spinal anesthesia in neonates and infants. Reg Anesth Pain Med. 2019;44:893–895. doi:10.1136/rapm-2019-100672
24. Yiğit D, Özen V, Kandirici A, Dokucu Aİ. Ultrasound-guided dorsal penile nerve block is a safe block in hypospadias surgery: a retrospective clinical study. Medicine. 2022;101(26):e29700. doi:10.1097/MD.0000000000029700
25. Ozen V. Comparison of the postoperative analgesic effects of US-guided caudal block and US-guided pudendal nerve block in circumcision. Int J Clin Pract. 2021;75(10):e14366. doi:10.1111/ijcp.14366
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
