Back to Journals » OncoTargets and Therapy » Volume 15
Management Strategies of Breast Cancer Patients with BRCA1 and BRCA2 Pathogenic Germline Variants
Authors Edaily S , Abdel-Razeq H
Received 7 April 2022
Accepted for publication 13 July 2022
Published 27 July 2022 Volume 2022:15 Pages 815—826
DOI https://doi.org/10.2147/OTT.S369844
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sanjeev K. Srivastava
Sarah Edaily, Hikmat Abdel-Razeq
Department of Internal Medicine, King Hussein Cancer Center, Amman, Jordan
Correspondence: Hikmat Abdel-Razeq, Department of Internal Medicine, King Hussein Cancer Center, Queen Rania Al Abdullah Street, P.O. Box: 1269, Amman, 11941, Jordan, Tel +962-6 5300460, Ext: 1000, Email [email protected]
Abstract: Most of breast cancer cases are sporadic; however, 15– 20% are associated with family history, and some are inherited. Among those, deleterious mutations in BRCA1 and BRCA2 tumor suppressor genes are the most commonly encountered pathogenic germline variants (PGVs). Given the availability and affordability of multi-gene panel sequencing technologies, testing for PGVs is commonly practiced. With our enhanced understanding of cancer genetics and specific molecular alterations, the better acceptance of risk-directed screening and prevention, and the recent introduction of novel targeted therapies, management of BRCA-positive breast cancers is taking a new direction, focusing more on risk-reducing interventions, including mastectomy and salpingo-oophorectomy, and incorporating special treatment regimens, including platinum-based chemotherapy, and the recently-introduced PARP (poly (ADP)-ribose polymerase) inhibitors. Given the recent advances in reproductive technology and molecular medicine, younger women with PGVs may have the option of embryo selection through preimplantation genetic testing and diagnosis, thus preventing the potential transmission of the implicated genes to the next generations. In this review, we cover the clinical implications of identifying a pathogenic germline mutation in BRCA1 and BRCA2 genes in breast cancer patients, and their relatives, across the continuum of care – from cancer prevention and early detection, through active treatment and up to survivorship issues.
Keywords: breast cancer, BRCA1, BRCA2, germline mutation, risk-reducing surgery
Introduction
Breast cancer continues to be the most commonly diagnosed cancer among women worldwide.1,2 Though more than 80% of breast cancers are sporadic, 15–20% of such tumors are associated with family history of breast or other cancers, and some are inherited.3 Deleterious mutations in BRCA1 and BRCA2 tumor suppressor genes are the most common causes of hereditary breast and ovarian cancer syndrome. The respective protein products of each gene function as a gatekeeper involved in the repair of DNA double strand breaks by homologous recombination and ensure the faithful replication of the genetic material with each cell division.4 Cells that lack this highly sophisticated protective mechanism, due to germline mutation in one of these in genes, will be prone to more mutations leading to higher risk of developing certain malignancies, with the breast and ovaries being the most likely affected organs.4,5
Both BRCA1 and BRCA2 pathogenic variants are associated with high penetrance rate. In a prospective study from the United Kingdom (UK) of around 2000 BRCA1/2 mutation carriers, the estimated cumulative risk, by age 70, for BRCA1 mutation carriers was 60% (95% CI, 44–75%) for breast cancer, 59% (95% CI, 43–76%) for ovarian cancer, and 83% (95% CI, 69–94%) for contralateral breast cancer. On the other hand, women carrying BRCA2 mutation had a risk of 55% (95% CI, 41–70%) for breast cancer, 16.5% (95% CI, 7.5–34%) for ovarian cancer, and 62% (95% CI, 44–79.5%) for contralateral breast cancer.6 In a more recent prospective cohort study of around 6000 BRCA1 and 3800 BRCA2 female carriers, the cumulative breast cancer risk, up to age 80, was 72% (95% CI, 65–79%) among BRCA1 carriers and 69% (95% CI, 61–77%) among BRCA2 carriers. On the other hand, cumulative ovarian cancer risk was 44% (95% CI, 36–53%) and 17% (95% CI, 11–25%) among BRCA1 and BRCA2 carriers, respectively. Contralateral breast cancer risk, 20 years after index breast cancer diagnosis, was 40% (95% CI, 35–45%) for BRCA1 and 26% (95% CI, 20–33%) for BRCA2 carriers.7
Thanks to the availability and affordability of multi-gene panel sequencing technologies, and the recently established therapeutic implications of positive genetic testing in many cancer sites, including breast, ovarian, pancreatic and prostate cancers, identification of BRCA1/2 and other pathogenic germline variants (PGVs) has become more common.8
Until recently, the management of breast cancer in patients carrying a germline mutation in BRCA1 or BRCA2 genes was similar to that of other patients without these mutations, and was defined by tumor subtype and stage, among other patient- and tumor-related factors. However, the better understanding of cancer genetics and specific molecular alterations, the potential for risk-directed screening and prevention, and the recent introduction of novel targeted therapies, at various stages of disease management, led to better personalized management strategies.
In this paper, we cover the specific clinical implications of these inherited cancer predisposition syndromes in regard to prophylactic risk-reducing surgeries, specific concerns in systemic treatment, impacts on reproductive factors and other cancer survivorship issues.
Pathological Features of BRCA-Associated Breast Cancer
Many studies have shown that breast cancer among patients with BRCA1 or BRCA2 pathogenic variants may carry special pathological features that may impact on the aggressiveness of anti-cancer therapy.4,9 In a study that reviewed pathological features of BRCA1 and BRCA2-associated breast cancer among 5000 patients, tumors in BRCA1 carriers were more of higher grade and of triple-negative (TN) subtype, whereas hormone receptor-positive tumors were detected more often among BRCA2 carriers. Additionally, BRCA2-associated cancers were more likely to contain calcifications that can be easily detected by mammography.10,11 Another prospective study enrolled a cohort of 1143 young females; 131 (11%) were BRCA1 or BRCA2 mutation carriers. BRCA1-associated tumors were more likely to be triple-negative, while those associated with BRCA2 were described as aggressive hormone receptor-positive tumors (luminal B-like).12 In another retrospective study, 391 BRCA-negative women were compared to 86 women who carried a pathogenic BRCA mutation. Triple-negative disease was diagnosed in 57.1% of the BRCA1-positive patients, in 23.3% of the BRCA2-positive patients, and in 13.8% of the BRCA-negative patients. Additionally, patients with BRCA1 mutation had higher nuclear grade, while frequency of estrogen receptors (ER) expression was not significantly different between mutation carriers and noncarriers, and clinical stage at diagnosis was almost similar between carriers and noncarriers.13
Variation in pathological features of patients with mutated BRCA1 or BRCA2 can be better appreciated in studies that addressed the utilization of 21-gene recurrence score (RS) assay in such patients. A review from Memorial Sloan Kettering Cancer Center of BRCA mutation carriers with hormone receptor-positive, node-negative breast cancer who had Oncotype-DX® testing showed that median RS was higher in cases versus controls (24 vs 16; P<0.0001), with 28% having high-risk disease, 56% intermediate-risk and only 16% having low-risk disease. Investigators concluded that germline BRCA1/2-mutated hormone receptor-positive tumors have intrinsically less favorable biology and most patients have benefited from chemotherapy.14 In a similar more recent study from MD Anderson Cancer Center (MDACC), investigators evaluated a cohort of 745 patients with early-stage ER-positive, HER2-negative invasive breast cancer who had both Oncotype-DX Breast Recurrence Score® analysis and genetic testing for hereditary breast and ovarian cancer syndrome. A total of 33 (4.4%) had pathogenic BRCA1/2 mutations (8 BRCA1, 25 BRCA2). Patients with BRCA1/2 mutations were younger, had less progesterone receptor (PR) expression, higher nuclear grade, and higher Oncotype DX Breast Recurrence Scores® (with median RS of 29, compared to 16 in patients without mutations, P<0.0001). Despite more aggressive treatment (more adjuvant chemotherapy), disease recurrence developed in 18% of patients with BRCA mutations and 9% of patient without. However, multivariate analysis of recurrence-free survival (RFS) was not significant, hazard ratio (HR) 1.519 [95% confidence interval (CI), 0.64–3.58; P=0.3401].15
Prognosis and Survival
Questions regarding treatment outcomes and prognosis of patients with germline pathogenic variants in BRCA1 or BRCA2, compared to the majority of the others with wild type (WT), are frequently asked by patients and their relatives. Published data are not consistent, and answers are, obviously, not easy.
In a meta-analysis of 16 trials with more than 10,000 breast cancer patients included, pathogenic BRCA1/2 mutations (n=1325 patients, 13%) were not associated with worse OS (HR 1.06, 95% CI, 0.84–1.34, P=0.61). Additionally, worse OS was observed with increased ER expression in BRCA1 cohorts, but not in patients with BRCA2.16 Another prospective study from the UK followed 2733 patient with breast cancer diagnosis at age 40 or younger, and pathogenic BRCA1/2 mutations were detected in 338 (12%) women. At a median follow-up of 8.2 years, no significant OS difference was detected between BRCA-mutated and WT young patients.17
Differences in treatment outcomes between BRCA1 and BRCA2 was evaluated using data from the Danish Breast Cancer Group database which showed lower 10-year OS and DFS for BRCA1 breast cancer patients (n=141): 78% (95% CI, 69–85%) and 74% (95% CI, 64–81%), respectively, compared to 88% (95% CI, 78–94%) and 84% (95% CI, 74–91%) for BRCA2 patients (n=96).18
In a Chinese cohort of 480 women, BRCA mutation carriers had more lymph node involvement at diagnosis (66.7% vs 42.6%; P=0.011), and significantly worse breast cancer specific outcomes with 5-year disease-free survival of 73.3% compared with 91.1% in non-carriers (P=0.013). Even after adjustment for other clinical prognostic factors, having BRCA mutation remained an independent factor for poor prognosis.19
A meta-analysis of 60 studies evaluated the effect of germline BRCA1/2 mutations on prognosis of breast cancer patients, and found that BRCA1 mutation carriers had a shorter OS compared with sporadic cases (HR 1.30, 95% CI, 1.11–1.52) and worse breast cancer-specific survival in patients with stage I–III (HR 1.45, 95% CI, 1.01–2.07). Similarly, BRCA2 carriers had worse breast cancer-specific survival (HR 1.29, 95% CI, 1.03–1.62), but no difference in OS was detected. However, patients with triple-negative disease and BRCA1/2 mutations had better OS than sporadic cases (HR 0.49, 95% CI, 0.26–0.92).20 Another meta-analysis of 34 studies reached similar conclusions; BRCA mutations were associated with shorter OS (BRCA1: HR=1.69, 95% CI, 1.35–2.12, P<0.001; BRCA2: HR=1.50, 95% CI, 1.03–2.19, P=0.034), but with nonsignificant difference in breast cancer specific survival (BRCA1: HR=1.14, 95% CI, 0.81–1.16, P=0.448; BRCA2: HR=1.16; 95% CI, 0.82–1.66, P=0.401) or event-free survival (BRCA1: HR=1.10, 95% CI, 0.86–1.41, P=0.438; BRCA2: HR=1.09; 95% CI, 0.81–1.47, P=0.558).21
More recently, a small study reviewed retrospectively the efficacy of endocrine therapy plus CDK 4/6 inhibitors in patients with HR-positive/HER2-negative advanced breast cancer. A total of 217 patients were included; 15 (6.9%) carried germline BRCA1/2, ATM or CHEK2 pathogenic variants. The majority of the patients (n=164, 75.6%) received CDK4/6 plus endocrine therapy as a first line. Median progression-free survival (PFS) was significantly shorter in patients with germline pathogenic variants (10.2 months), compared with WT and untested patients (15.6 and 17.6 months, respectively), P=0.002. Similarly, median OS was worse in patients with germline pathogenic variants compared to those without (P=0.006). In multivariate analysis, mutation status was an independent prognostic factor of both PFS (P=0.020) and OS (P=0.012).22
Risk-Reducing Surgery
Risk-Reducing Mastectomy
Risk-reducing mastectomy provides maximum breast cancer risk reduction in BRCA mutation carriers in both retrospective and prospective data, with at least 90% risk reduction. Additionally, surgery has significant impact on quality of life by reducing the level of anxiety and fear of getting breast cancer.23 There are different surgical approaches for prophylactic mastectomy, but the gold standard is nipple-sparing, skin-sparing mastectomy with excellent oncological and esthetic results. The procedure is usually done through an inframammary, radial or axillary incision with skin carefully dissected off breast tissue with removal of the entire breast glands.23
Mastectomy versus breast-conserving surgery (BCS) was not compared in randomized controlled trials. However, a systematic review of 18 studies published in 2019 compared BCS and mastectomy and showed almost comparable OS results from pooled analysis, with higher ipsilateral recurrence in the BCS group. Researchers concluded that BCS can be offered for select patients with BRCA mutation after proper counseling and with intensive follow-up.24 In another systematic review, 23 observational studies were analyzed to compare difference in outcomes between BCS and mastectomy in BRCA1/2 mutation carriers. A total of 3807 patients were included; 2200 (57.7%) had BRCA1 mutations while 1212 (31.8%) had BRCA2 mutations, and median age at diagnosis was 41 years. Mastectomy was performed on 1408 (41.5%) patients, while 2157 (56.7%) had BCS. Risk of locoregional recurrence was increased in the BCS group, but incidence of contralateral breast cancer, disease-free survival and disease-specific survival were not statistically different, and nor was the OS (HR: 1.10, 95% CI, 0.72–1.69, P=0.660) (Table 1).25 Data from the Danish Breast Cancer Group, however, showed that risk-reducing contralateral mastectomy results in a significantly reduced risk of death (adjusted OS HR 0.42, 95% CI, 0.21–0.84, P=0.01).18
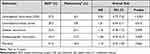 |
Table 1 Differences in Treatment Outcomes Between BCS and Mastectomy |
Risk-reduction decisions among cancer-free pathogenic BRCA1/2 mutation carriers from a single institution showed that 66% of 106 women went for surveillance only, while 34% opted for prophylactic mastectomy. Three factors were found to be significantly affecting women’s decision to have surgery: family member diagnosed with breast cancer below the age of 50 (OR: 4.67 [95% CI, 1.86–11.68]), P=0.001), a relative died from cancer before age of 50 (OR: 2.26 [95% CI, 0.92–5.55], P=0.07) and having previous prophylactic oophorectomy (OR: 3.72 [95% CI, 1.49–9.31], P=0.005). Patients aged 30 or less were more likely to choose surveillance (OR: 0.2 [95% CI, 0.05–0.75], P=0.02).26
In another study, prophylactic mastectomy was compared with therapeutic mastectomy in 30,803 patients from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database: 30,644 (99.5%) had therapeutic mastectomy, and only 159 (0.5%) had prophylactic mastectomy. Surgery duration was significantly longer in prophylactic mastectomy (265 vs 166 minutes; P<0.01), with no significant difference in mortality. After adjustment for age and surgery time, the prophylactic surgeries showed increase in thrombosis risk.27
Risk-Reducing Salpingo-Oophorectomy (RRSO)
Risk-reducing salpingo-oophorectomy (RRSO) was addressed in the literature, highlighting two major points: first its effect on breast cancer recurrence and survival; and second, its obvious anticipated effect on reducing, or eliminating, ovarian cancer.
The impact of oophorectomy on survival of breast cancer patients with a BRCA1 or BRCA2 mutation was addressed in many studies. Many of these studies and registries have shown that RRSO provides significant reduction in breast cancer risk.28 In one retrospective study, 676 women with early-stage breast cancer and a BRCA1 or BRCA2 mutation were observed for up to 20 years after diagnosis. Bilateral risk-reducing oophorectomy was performed on 345 (51.0%) patients following their breast cancer diagnosis, while the others (n=331, 49.0%) opted to retain both ovaries. The 20-year survival for the entire cohort was 77.4%. The adjusted hazard ratio for death attributed to breast cancer in women who underwent oophorectomy was 0.57 (95% CI, 0.23–1.43; P=0.23) for BRCA2 carriers and 0.38 (95% CI, 0.19–0.77; P=0.007) for BRCA1 carriers.29 However, one prospective observational study reached different conclusions. In this study, 2272 BRCA1 and 1605 BRCA2 mutation carriers were followed for a mean of around 5 years, and 426 women developed breast cancer. Effect of RRSO were evaluated, and no significant benefit was noted in the BRCA1 cohort (HR=1.23; 95% CI, 0.94–1.61) or BRCA2 (HR=0.88; 95% CI, 0.62–1.24). However, BRCA2 mutation carriers had a potential benefit 5 years after RRSO.30
Satisfaction of women following RRSO was much better than following prophylactic mastectomy. In a survey of 174 BRCA mutation carriers, 95% of them underwent prophylactic mastectomy and believed that this surgery can reduce breast cancer risk, but only 65% were completely satisfied from a cosmetic perspective. On the other hand, 90.5% of women who underwent RRSO would choose to do it again due to decreased anxiety about risk of ovarian cancer, though early menopausal symptoms had a significant impact on their quality of life and only 21% used treatments to relieve them.31
Medical Treatment
Advanced-Stage Disease
The largest trial that addressed the benefit of platinum compound in the treatment of BRCA-positive breast cancer was the TNT study which was a phase 3 randomized controlled trial conducted at 74 hospitals throughout the UK. The study compared carboplatin with docetaxel, a standard treatment for recurrent unresectable or metastatic triple-negative breast cancer. A total of 376 patients were randomized to receive carboplatin or docetaxel, both as single agent every three weeks until disease progression or intractable toxicity. The trial population largely comprised patients with TN breast cancer, and 43 (11.4%) had germline BRCA1 (n=31) or BRCA2 (n=12) mutation. Among the whole study group, there was no difference between the overall response rate (ORR) to carboplatin or to docetaxel (ORR, 31.4% in the carboplatin group versus 34.0% in the carboplatin group). Median PFS among patients allocated to carboplatin was 3.1 months (95% CI, 2.4–4.2), and 4.4 months (95% CI, 4.1–5.1) for those allocated to docetaxel, P=0.40. Additionally, no difference was found in OS in both groups. On the other hand, patients with deleterious BRCA1/2 germline mutation had a significantly better response to carboplatin than to docetaxel (ORR, 68% versus 33.3%, P=0.03). Results remained significant (P=0.01) after adjustment for known prognostic factors. Progression-free survival was also longer in subjects with a BRCA1/2 germline mutation who were treated with carboplatin (median PFS, 6.8 months for carboplatin versus 4.4 months for docetaxel, P=0.002). However, no difference was found between groups in OS, which is obviously confounded by the crossover design of the study.32
In another phase 2 nonrandomized trial, cisplatin was given to 20 BRCA1-mutated patients with metastatic breast cancer. The overall response rate was 80%, and OS at 3 years was 25%.33 Response rate was also higher in a subgroup analysis from a multicenter phase 2 trial where cisplatin or carboplatin was given as first- or second-line treatment for patients with metastatic breast cancer; response rate was around 54% in patients with pathogenic germline BRCA1/2 mutations.34
PARP (poly (ADP)-ribose polymerase) inhibitors were also tried in patients with mutated BRCA1/2 advanced-stage breast cancer. The OlympiAD trial was a randomized phase 3 trial in which olaparib, at a dose of 300 mg twice daily, was compared to single agent palliative chemotherapy (capecitabine, eribulin or vinorelbine) in a cohort of 302 patients with pathogenic germline BRCA1/2 mutation, HER2-negative metastatic breast cancer who received no more than two previous lines of chemotherapy in the metastatic setting. The study met its primary end point of PFS with a median PFS of 7 months versus 4.2 months (HR 0.58, 95% CI, 0.43–0.80).35 However, there was no OS advantage even with an updated analysis of the study.36
Talazoparib, another PARP inhibitor, was also studied in a phase 3 randomized trial, EMBRACA. In this open-label, randomized, phase 3 trial, 431 patients with HER2-negative locally advanced or metastatic breast cancer and deleterious or suspected deleterious germline BRCA1/2 mutation were randomized to receive talazoparib at 1 mg orally once daily (n=287), or single agent chemotherapy (capecitabine, eribulin, gemcitabine or vinorelbine; n=144). Patients were allowed to be enrolled if they had received up to 3 previous cytotoxic regimens for advanced disease including a taxane, anthracycline or both. Treatment was continued until disease progression or unacceptable toxicity. Talazoparib showed statistically significant PFS benefit of 3 months (8.6 versus 5.6 months, HR 0.54, 95% CI, 0.41–0.71).37 Similar to olaparib, talazoparib failed to show significant OS benefit in an updated analysis of the trial.38
In a meta-analysis of the EMBRACA and the OlympiAD trials – the 2 major randomized controlled trials on PARP inhibitors used to treat advanced breast cancer – major hematologic adverse events, including anemia, neutropenia and decreased white cell count, were analyzed as a primary safety outcome, while fatigue and headache were considered as secondary safety outcome measures. Additionally, discontinuation rate and time to QoL deterioration were compared between the two PARP inhibitors. Olaparib caused less grade 3–4 anemia (OR=0.34, 95% CI, 0.003–34.94) and less grade 3–4 neutropenia (OR=0.57, 95% CI, 0.06–5.75) compared to talazoparib. In secondary safety analysis, olaparib was associated with higher grade 3–4 fatigue (OR=6.79, 95% CI, 0.44–262.48) and less headache (OR=0.14, 95% CI, 0.003–4.17). Time to clinically meaningful QoL deterioration was shorter with olaparib (HR=1.16, 95% CI, 0.19–7.17) when compared to talazoparib. The authors concluded that both talazoparib and olaparib were well tolerated, with no significant risk of discontinuation, and either agent can be used in the setting of metastatic or advanced HER2-negative breast cancer with BRCA1/2 mutation with similar expected efficacy and safety.39
Another PARP inhibitor, veliparib, was evaluated in a randomized, double-blind, phase 3 trial (BROCADE3) in 509 patients with pathogenic germline BRCA1/2 mutations and advanced HER2-negative breast cancer. A maximum of 2 prior lines of chemotherapy for advanced disease were allowed. Patients were randomized to carboplatin and paclitaxel combined with veliparib or with placebo until disease progression. Median PFS was 14.5 months (95% CI, 12.5–17.7) in the veliparib arm compared to 12.6 months (95% CI, 10.6–14.4) in the control arm (HR 0.71 [95% CI, 0.57–0.88], P=0.0016).40 In an exploratory analysis of the subset of patients who discontinued carboplatin and paclitaxel before disease progression and were continued on a higher dose of veliparib (300–400 mg twice daily continuously, n=136) or placebo (n=58), as maintenance, median PFS was 25.7 months with veliparib compared to 14.6 months with placebo. Adverse events in the maintenance phase were primarily gastrointestinal, while the most common grade 3 and 4 adverse events were neutropenia and anemia.41 Table 2 summarizes major studies that addressed treatment of advanced-stage breast cancer with pathogenic BRCA1/2 variants.
 |
Table 2 Treatment of Early-Stage Breast Cancer with Pathogenic BRCA1/2 Variants |
Early-Stage Disease
In the non-metastatic setting, platinum agents showed remarkable activity in BRCA1/2-mutated breast cancers. In an observational study in BRCA1-mutated patients with breast cancer, high rates of pCR were observed in a small group of patients who received neoadjuvant cisplatin (pCR in 10 of 12 patients, 83%), compared with 7% among those treated with cyclophosphamide, methotrexate and fluorouracil (CMF); 8% with doxorubicin and docetaxel; and 22% with doxorubicin and cyclophosphamide with and without fluorouracil.42 Another study confirmed pCR of 61% among 107 patients with pathogenic BRCA1 mutation after neoadjuvant cisplatin chemotherapy.43 In a secondary analysis of GeparSixto randomized trial, 50 patients with pathogenic BRCA1 or BRCA2 germline mutations attained higher pCR rate compared with patients without such mutations, but this rate was not increased by adding carboplatin to neoadjuvant chemotherapy.44
PARP inhibitors were also tried in the setting of high-risk early-stage breast cancer with germline BRCA1/2 mutations and HER2-negative disease. Following the completion of standard local treatment and neoadjuvant or adjuvant therapy, 1836 patients were randomized to receive adjuvant olaparib for one year versus placebo in a randomized phase 3 trial (OlympiA). The 3-year invasive disease-free survival (iDFS) was significantly higher in the olaparib arm (85.9% versus 77.1%, P<0.001). Additionally, the 3-year distant disease-free survival (dDFS) was 87.5% in the olaparib arm versus 80.4% with placebo, P<0.001. Though the 3-year OS was better in the olaparib arm (92.0% versus 88.3%, P=0.02), it did not reach a prespecified P-value of less than 0.01.45 However, the results of the second preplanned event-driven analysis for OS were recently released. After a median follow-up of 3.5 years, there were 109 deaths in the placebo arm and 75 deaths in the olaparib arm; the 3-year OS rates were 89.1% and 92.0%, respectively (HR=0.68; 95% CI=0.47–0.97, P=0.0009), crossing the pre-specified significance boundary.46 Table 3 summarizes major studies that addressed treatment of early-stage breast cancer with pathogenic BRCA1/2 variants.
 |
Table 3 Treatment of Advanced-Stage Breast Cancer with Pathogenic BRCA1/2 Variants |
Survivorship Issues
Bone Health
Women undergoing prophylactic oophorectomy while in their 40s are at higher risk for osteopenia and osteoporosis.47,48 Post-oophorectomy bone mineral density (BMD) measurements were assessed in a retrospective cohort of 95 women who had prophylactic oophorectomy at a mean age of 48 years. A significant annual decrease in BMD from baseline was noted among both pre- and postmenopausal women at time of surgery. Self-reported hormonal therapy use was significantly associated with less bone loss.49 Another retrospective study from Northern California reviewed bone health-related issues among 225 women who underwent RRSO due to pathogenic BRCA1 or BRCA2 mutations. The median time from RRSO to bone disease diagnosis was 29 months (range 1–170). After a median follow-up of 41 months from testing, 55.6% had osteopenia, 12.1% osteoporosis and 4% had atraumatic fracture.50
Recent evidence suggests that dysregulated RANK/RANKL system is a potential cause of breast cancer in women carrying BRCA1 mutations as these patients were found to have significantly lower levels of osteoprotegerin, which means less inhibition of RANKL-mediated signaling. As such, researchers are studying the potential role of denosumab in chemoprevention in such women.51–53 Besides regulating osteoclast differentiation and activation, the RANK/RANKL system has an important role in mammary gland physiology and in hormone-dependent epithelial cell proliferation during pregnancy. Hence, dysregulations in the RANKL/RANK system can play a role in breast cancer pathogenesis.54 Additionally, the role of dysregulated RANKL/RANK system is well established in the process of bone metastasis development. Such observations support the importance of RANKL inhibition in breast cancer prevention and therapy in both early and advanced-stage disease.
Some data also suggested an association between levels of expression of different RANK pathway molecules and breast cancer aggressiveness, development of bone metastasis and overall prognosis, though evidence is still conflicting and inconsistent.55–59
Fertility and Reproduction
Healthy women and cancer patients who carry pathogenic BRCA1/2 mutations need special counseling for reproductive issues; several questions should be addressed in depth with both groups. The influence of pregnancy on the risk of breast or ovarian cancer is a concern for both healthy women and breast cancer patients with BRCA1/2 mutations. Though the issue is still controversial, one study suggested a differential association with parity between BRCA1 and BRCA2 mutation carriers.60,61
Breastfeeding, on the other hand, can be protective. In a case-control study of more than 1500 pairs of women with BRCA1 or BRCA2 pathogenic mutations and matching patients with breast cancer and unaffected carriers of respective mutation as controls, investigators found significant reduction in breast cancer risk in BRCA1 carriers with reduction increased by increased duration of breast feeding: a 32% reduction in risk for one year of breastfeeding (OR=0.68; 95% CI, 0.52–0.91; P=0.008). Breastfeeding for ≥2 years conferred even a greater reduction in risk (OR=0.51; 95% CI, 0.35–0.74). However, no significant difference was found among the BRCA2 cohort.62
The optimal timing for risk-reducing bilateral mastectomies in healthy BRCA1/2 mutation carriers is more difficult to determine, as earlier removal of breast tissue before pregnancy can reduce the breast cancer risk; on the other hand, this will deprive the mother and her baby of the benefits of breastfeeding, so counseling of these young women should include personal preferences beside her expected risk based on mutation, age, breast density and family history.63 Additionally, data showed no difference in survival of patients carrying pathogenic BRCA mutations if they became pregnant after breast cancer diagnosis.64,65 Timing of contralateral risk-reducing mastectomy should take into consideration the expected patient prognosis from the first breast cancer. Another reason to advise women carrying pathogenic BRCA1/2 mutations to complete reproductive life as early as possible is the concern, although controversial, that these pathogenic mutations can decrease the ovarian reserve in healthy carriers.66
Healthy women and cancer patients carrying pathogenic BRCA1/2 mutations can safely undergo fertility preservation by oocyte or embryo cryopreservation, but not ovarian tissue preservation, and data also showed that treatment of infertility, including IVF, can be safely implemented.63,67
For women who choose to delay risk-reducing mastectomy an intensive surveillance approach should be carried out including annual mammography and breast MRI alternating every six months starting at age of 25–30 years or earlier based on the earliest age of cancer diagnosis in the family, and to avoid delays in diagnosis patients and physicians should be aware of the possibility of breast cancer occurrence during pregnancy and breastfeeding.68–70
Given the recent advances in molecular medicine and reproductive technology, BRCA-pathogenic variant carriers of reproductive age may have the option of Preimplantation Genetic Testing for Monogenic disorders (PGT-M). The Ethics Taskforce of the European Society of Human Reproduction and Embryology (ESHRE), in 2003, has considered PGT-M acceptable for hereditary breast and ovarian cancers,71 and, in 2008, Jasper et al reported the first live birth following PGT-M for a woman carrier of BRCA1 pathogenic variant.71,72 Since then, multiple studies have documented the success and the feasibility of PGT-M for women with BRCA pathogenic variants.73 Women’s attitude toward PGT-M is very variable and may be influenced by their age, family size and personal and family history of cancer.74–76 Cost of the procedure may also affect the uptake.
Lifestyle Modifications
Several studies have tried to investigate if harmful lifestyle factors such as obesity, smoking, alcohol and physical inactivity can influence cancer prevalence among BRCA1/2 mutation carriers. In the Lifestyle Intervention Study in Women with Hereditary Breast and Ovarian Cancer (LIBRE), researchers collected data from 68 BRCA1 and BRCA2 mutation carriers. At study entry, factors such as medical history, lifestyle behavior and socioeconomic status were retrospectively documented by interview, and the current BMI was recorded. The baseline measurements were compared within the cohort, and presented with reference values for the German population. Participants who had higher physical activity during their adolescence showed a significantly lower cancer prevalence (P=0.019). A significant difference in cancer occurrence was observed between smokers and non-smokers (P<0.001). Mutation carriers with no disease had a significantly higher physical activity level than diseased mutation carriers (P=0.046).77,78 Using a large international pooled cohort of BRCA1 and BRCA2 mutation carriers, another study confirmed the association between smoking of more than 5 years' duration before a first full-term pregnancy (FFTP), but not alcohol consumption, and risk of breast cancer. The study included was conducted retrospectively (5707 BRCA1 mutation carriers and 3525 BRCA2 mutation carriers) and prospectively (2276 BRCA1 mutation carriers and 1610 BRCA2 mutation carriers).79
In a recent review, researchers reviewed data from 16 clinical trials trying to collect evidence regarding impact of lifestyle factors, or mainly metabolic effects, in women carrying pathogenic BRCA1/2 mutations on the risk of developing breast cancer. The authors concluded that smoking, obesity and sedentary life, especially in postmenopausal women, may be associated with increased risk, though the data are still controversial.80
Future Directions and Conclusions
Testing of patients with breast cancer for pathogenic germline variants, mostly BRCA1 and BRCA2, is widely available and has become more affordable. Implications of positive testing goes far beyond cancer prevention for patients and their relatives. Recent data have suggested that cancer patients, like those with breast, ovarian, pancreatic and prostate cancer who carry pathogenic variants, might be treated differently using many of the recently introduced drugs, in both early and advanced-stage disease. Clinical oncologists should widen the spectrum of cancer care offered to include extensive discussion of potential genetic and inherited etiology for the cancer they have.
Abbreviations
BCS, breast-conserving surgery; BMD, bone mineral density; CDK 4/6, cyclin-dependent kinase 4/6; DFS, disease-free survival; dDFS, distant disease-free survival; ER, estrogen receptor; FFTP, first full-term pregnancy; iDFS, invasive disease-free survival; IVF, in vitro fertilization; HR, hormone receptor; ORR, overall response rate; OS, overall survival; PARP, poly(ADP)ribose polymerase; PFS, progression-free survival; PR, progesterone receptor; PGV, pathogenic germline variants; pCR, pathologic complete response; QoL, quality of life; RANK, receptor activator of nuclear factor kappa-B; RANKL, receptor activator of nuclear factor kappa-B ligand; RRSO, risk-reducing salpingo-oophorectomy; RS, recurrence score; TN, triple-negative; WT, wild type.
Acknowledgments
The authors would like to thank Ms. Ryan Bater, Mrs. Alice Hadaddin and Ms. Ayat Taqash for their help in preparing this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
SE has no conflict of interest to report, HA received institutional research grant from Pfizer.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Lei S, Zheng R, Zhang S, et al. Global patterns of breast cancer incidence and mortality: a population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. 2021;41(11):1183–1194. doi:10.1002/cac2.12207
3. Evans O, Gaba F, Manchanda R. Population-based genetic testing for Women’s cancer prevention. Best Pract Res Clin Obstet Gynaecol. 2020;65:139–153. doi:10.1016/j.bpobgyn.2020.02.007
4. Hodgson A, Turashvili G. Pathology of hereditary breast and ovarian cancer. Front Oncol. 2020;10:531790. doi:10.3389/fonc.2020.531790
5. Li S, Silvestri V, Leslie G, et al. Cancer risks associated with BRCA1 and BRCA2 pathogenic variants. J Clin Oncol. 2022;25:JCO2102112. doi:10.1200/JCO.21.02112
6. Mavaddat N, Peock S, Frost D, et al. Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst. 2013;105(11):812–822. doi:10.1093/jnci/djt095
7. Kuchenbaecker KB, Hopper JL, Barnes DR, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317(23):2402. doi:10.1001/jama.2017.7112
8. Pothuri B. BRCA1- and BRCA2-related mutations: therapeutic implications in ovarian cancer. Ann Oncol. 2013;24:viii22–viii27. doi:10.1093/annonc/mdt307
9. Chappuis PO, Nethercot V, Foulkes WD. Clinico-pathological characteristics of BRCA1- and BRCA2-related breast cancer. Semin Surg Oncol. 2000;18(4):287–295. doi:10.1002/(SICI)1098-2388(200006)18:4<287::AID-SSU3>3.0.CO;2-5
10. Yoshida R. Hereditary breast and ovarian cancer (HBOC): review of its molecular characteristics, screening, treatment, and prognosis. Breast Cancer. 2020;28(6):1167–1180. doi:10.1007/s12282-020-01148-2
11. Krammer J, Pinker-Domenig K, Robson ME, et al. Breast cancer detection and tumor characteristics in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat. 2017;163(3):565–571. doi:10.1007/s10549-017-4198-4
12. Guzmán-Arocho YD, Rosenberg SM, Garber JE, et al. Clinicopathological features and BRCA1 and BRCA2 mutation status in a prospective cohort of young women with breast cancer. Br J Cancer. 2021;126(2):302–309. doi:10.1038/s41416-021-01597-2
13. Atchley DP, Albarracin CT, Lopez A, et al. Clinical and pathologic characteristics of patients with BRCA-positive and BRCA-negative breast cancer. J Clin Oncol. 2008;26(26):4282–4288. doi:10.1200/JCO.2008.16.6231
14. Shah PD, Patil S, Dickler MN, Offit K, Hudis CA, Robson ME. Twenty-one-gene recurrence score assay inBRCA-associated versus sporadic breast cancers: differences based on germline mutation status. Cancer. 2016;122(8):1178–1184. doi:10.1002/cncr.29903
15. Layman RM, Lin H, Barrera AMG, Karuturi MS, Yam C, Arun BK. Clinical outcomes and Oncotype DX Breast Recurrence Score® in early-stage BRCA-associated hormone receptor-positive breast cancer. Cancer Med. 2022;11:1474–1483. doi:10.1002/cam4.4566
16. Templeton AJ, Gonzalez LD, Vera-Badillo FE, et al. Interaction between hormonal receptor status, age and survival in patients with BRCA1/2 germline mutations: a systematic review and meta-regression. PLoS One. 2016;11(5):e0154789. doi:10.1371/journal.pone.0154789
17. Copson ER, Maishman TC, Tapper WJ, et al. Germline BRCA mutation and outcome in young-onset breast cancer (POSH): a prospective cohort study. Lancet Oncol. 2018;19(2):169–180. doi:10.1016/S1470-2045(17)
18. Soenderstrup IMH, Laenkholm AV, Jensen MB, et al. Clinical and molecular characterization of BRCA-associated breast cancer: results from the DBCG. Acta Oncologica. 2017;57(1):95–101. doi:10.1080/0284186X.2017.1398415
19. Wang YA, Jian JW, Hung CF, et al. Germline breast cancer susceptibility gene mutations and breast cancer outcomes. BMC Cancer. 2018;18(1):315. doi:10.1186/s12885-018-4229-5
20. Baretta Z, Mocellin S, Goldin E, Olopade OI, Huo D. Effect of BRCA germline mutations on breast cancer prognosis. Medicine. 2016;95(40):e4975. doi:10.1097/MD.0000000000004975
21. Zhu Y, Wu J, Zhang C, et al. BRCA mutations and survival in breast cancer: an updated systematic review and meta-analysis. Oncotarget. 2016;7(43):70113–70127. doi:10.18632/oncotarget.12158
22. Bruno L, Ostinelli A, Waisberg F, et al. Cyclin-dependent kinase 4/6 inhibitor outcomes in patients with advanced breast cancer carrying germline pathogenic variants in DNA repair-related genes. JCO Precis Oncol. 2022;6:e2100140. doi:10.1200/PO.21.00140
23. Franceschini G, Masetti R. What the surgeons should know about the bilateral prophylactic mastectomy in BRCA mutation carriers. Eur J Breast Health. 2019;15(2):135–136. doi:10.5152/ejbh.2019.4651
24. Co M, Liu T, Leung J, et al. Breast conserving surgery for BRCA mutation carriers-a systematic review. Clin Breast Cancer. 2020;20(3):e244–e250. doi:10.1016/j.clbc.2019.07.014
25. Davey MG, Davey CM, Ryan ÉJ, Lowery AJ, Kerin MJ. Combined breast conservation therapy versus mastectomy for BRCA mutation carriers - A systematic review and meta-analysis. Breast. 2021;56:26–34. doi:10.1016/j.breast.2021.02.001
26. Johns D, Agarwal J, Anderson L, Ying J, Kohlmann W. Breast cancer risk reduction decisions of the BRCA-positive patient: an observational study at a single institution. J Womens Health. 2017;26(6):702–706. doi:10.1089/jwh.2016.5931
27. Hendrix RJ, Lee C, Friedrich AK, Rouanet E, Larkin AC, LaFemina J. Prophylactic versus therapeutic mastectomy: a contemporary analysis of the ACS-NSQIP database. Clin Breast Cancer. 2019;19(3):e428–e432. doi:10.1016/j.clbc.2019.01.008
28. Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing Salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst. 2009;101(2):80–87. doi:10.1093/jnci/djn442
29. Metcalfe K, Lynch HT, Foulkes WD, et al. Effect of oophorectomy on survival after breast cancer inBRCA1andBRCA2Mutation carriers. JAMA Oncol. 2015;1(3):306. doi:10.1001/jamaoncol.2015.0658
30. Mavaddat N, Antoniou AC, Mooij TM, et al. Risk-reducing salpingo-oophorectomy, natural menopause, and breast cancer risk: an international prospective cohort of BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. 2020;22(1):8. doi:10.1186/s13058-020-1247-4
31. D’Alonzo M, Piva E, Pecchio S, et al. Satisfaction and impact on quality of life of clinical and instrumental surveillance and prophylactic surgery in BRCA-mutation carriers. Clin Breast Cancer. 2018;18(6):e1361–e1366. doi:10.1016/j.clbc.2018.07.015
32. Tutt A, Tovey H, Cheang MCU, et al. Carboplatin in BRCA1/2-mutated and triple-negative breast cancer BRCAness subgroups: the TNT trial. Nat Med. 2018;24(5):628–637. doi:10.1038/s41591-018-0009-7
33. Byrski T, Dent R, Blecharz P, et al. Results of a Phase II open-label, non-randomized trial of cisplatin chemotherapy in patients with BRCA1-positive metastatic breast cancer. Breast Cancer Res. 2012;14(4). doi:10.1186/bcr3231
34. Isakoff SJ, Mayer EL, He L, et al. TBCRC009: a multicenter phase ii clinical trial of platinum monotherapy with biomarker assessment in metastatic triple-negative breast cancer. J Clin Oncol. 2015;33(17):1902–1909. doi:10.1200/JCO.2014.57.6660
35. Robson M, Im SA, Senkus E, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377(6):523–533. doi:10.1056/NEJMoa1706450
36. Robson ME, Tung N, Conte P, et al. OlympiAD final overall survival and tolerability results: olaparib versus chemotherapy treatment of physician’s choice in patients with a germline BRCA mutation and HER2-negative metastatic breast cancer. Ann Oncol. 2019;30(4):558–566. doi:10.1056/NEJMoa1706450
37. Litton JK, Rugo HS, Ettl J, et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N Engl J Med. 2018;379(8):753–763. doi:10.1056/NEJMoa1802905
38. Litton JK, Hurvitz SA, Mina LA, et al. Talazoparib versus chemotherapy in patients with germline BRCA1/2-mutated HER2-negative advanced breast cancer: final overall survival results from the EMBRACA trial. Ann Oncol. 2020;31(11):1526–1535. doi:10.1016/j.annonc.2020.08.2098
39. Wang J, Zhang Y, Yuan L, Ren L, Zhang Y, Qi X. Comparative efficacy, safety, and acceptability of single-agent poly (ADP-ribose) polymerase (PARP) inhibitors in BRCA-mutated HER2-negative metastatic or advanced breast cancer: a network meta-analysis. Aging. 2020;13(1):450–459. doi:10.18632/aging.202152
40. Diéras V, Han HS, Kaufman B, et al. Veliparib with carboplatin and paclitaxel in BRCA-mutated advanced breast cancer (BROCADE3): a randomised, double-blind, placebo-controlled, Phase 3 trial. Lancet Oncol. 2020;21(10):1269–1282. doi:10.1016/S1470-2045(20)30447-2
41. Han HS, Arun BK, Kaufman B, et al. Veliparib monotherapy following carboplatin/paclitaxel plus veliparib combination therapy in patients with germline BRCA-associated advanced breast cancer: results of exploratory analyses from the phase III BROCADE3 trial. Ann Oncol. 2022;33(3):299–309. doi:10.1016/j.annonc.2021.11.018
42. Byrski T, Gronwald J, Huzarski T, et al. Pathologic complete response rates in young women with BRCA1-positive breast cancers after neoadjuvant chemotherapy. J Clin Oncol. 2010;28(3):375–379. doi:10.1200/JCO.2008.20.7019
43. Byrski T, Huzarski T, Dent R, et al. Pathologic complete response to neoadjuvant cisplatin in BRCA1-positive breast cancer patients. Breast Cancer Res Treat. 2014;147(2):401–405. doi:10.1007/s10549-014-3100-x
44. Hahnen E, Lederer B, Hauke J, et al. Germline mutation status, pathological complete response, and disease-free survival in triple-negative breast cancer. JAMA Oncol. 2017;3(10):1378. doi:10.1001/jamaoncol.2017.1007
45. Tutt ANJ, Garber JE, Kaufman B, et al. Adjuvant olaparib for patients with BRCA1- or BRCA2- mutated breast cancer. N Engl J Med. 2021;384(25):2394–2405. doi:10.1056/EJMoa2105215
46. Tutt A, Garber J, Gelber R, et al. VP1-2022: pre-specified event driven analysis of Overall Survival (OS) in the OlympiA phase III trial of adjuvant olaparib (OL) in germline BRCA1/2 mutation (gBRCAm) associated breast cancer. ESMO Virtual Plenary; 2022. Available from: https://oncologypro.esmo.org/meeting-resources/esmo-virtual-plenary-resources/olympia-phase-iii-pre-specified-event-driven-analysis-of-overall-survival-of-olaparib-in-gbrcam-breast-cancer.
47. Terra L, Hooning MJ, Heemskerk-Gerritsen BAM, et al. Long-term morbidity and health after early menopause due to oophorectomy in women at increased risk of ovarian cancer: protocol for a nationwide cross-sectional study with prospective follow-up (HARMOny Study). JMIR Res Protoc. 2021;10(1):e24414. doi:10.2196/24414
48. Mai PL, Huang HQ, Wenzel LB, et al. Prospective follow-up of quality of life for participants undergoing risk-reducing salpingo-oophorectomy or ovarian cancer screening in GOG-0199: an NRG oncology/GOG study. Gynecol Oncol. 2020;156(1):131–139. doi:10.1016/j.ygyno.2019.10.026
49. Kotsopoulos J, Hall E, Finch A, et al. Changes in bone mineral density after prophylactic bilateral salpingo-oophorectomy in carriers of a BRCA mutation. JAMA Ntwk Open. 2019;2(8):e198420. doi:10.1001/jamanetworkopen.2019.8420
50. Garcia C, Lyon L, Conell C, Littell RD, Powell CB. Osteoporosis risk and management in BRCA1 and BRCA2 carriers who undergo risk-reducing salpingo-oophorectomy. Gynecol Oncol. 2015;138(3):723–726. doi:10.1016/j.ygyno.2015.06.020
51. Kotsopoulos J, Singer C, Narod SA. Can we prevent BRCA1-associated breast cancer by RANKL inhibition? Breast Cancer Res Treat. 2016;161(1):11–16. doi:10.1007/s10549-016-4029-z
52. Nolan E, Vaillant F, Branstetter D, et al. RANK ligand as a potential target for breast cancer prevention in BRCA1-mutation carriers. Nat Med. 2016;22(8):933–939. doi:10.1038/nm.4118
53. Widschwendter M, Burnell M, Fraser L, et al. Osteoprotegerin (OPG), the endogenous inhibitor of receptor activator of NF-kB ligand (RANKL), is dysregulated in BRCA mutation carriers. EBioMedicine. 2015;2(10):1331–1339. doi:10.1016/j.ebiom.2015.08.037
54. Infante M, Fabi A, Cognetti F, Gorini S, Caprio M, Fabbri A. RANKL/RANK/OPG system beyond bone remodeling: involvement in breast cancer and clinical perspectives. J Exp Clin Cancer Res. 2019;38(1). doi:10.1186/s13046-018-1001-2
55. Casimiro S, Vilhais G, Gomes I, Costa L. The roadmap of RANKL/RANK pathway in cancer. Cells. 2021;10(8):1978. doi:10.3390/cells10081978
56. Santini D, Schiavon G, Vincenzi B, et al. Receptor activator of NF-kB (RANK) expression in primary tumors associates with bone metastasis occurrence in breast cancer patients. PLoS One. 2011;6(4):e19234. doi:10.1371/journal.pone.0019234
57. Zhang L, Teng Y, Zhang Y, et al. Receptor activator for nuclear factor k B expression predicts poor prognosis in breast cancer patients with bone metastasis but not in patients with visceral metastasis. J Clin Pathol. 2011;65(1):36–40. doi:10.1136/jclinpath-2011-200312
58. Owen S, Ye L, Sanders AJ, Mason MD, Jiang WG. Expression profile of receptor activator of nuclear-kB (RANK), RANK ligand (RANKL) and osteoprotegerin (OPG) in breast cancer. Anticancer Res. 2012;33(1):199–206.
59. Pfitzner BM, Branstetter D, Loibl S, et al. RANK expression as a prognostic and predictive marker in breast cancer. Breast Cancer Res Treat. 2014;145(2):307–315. doi:10.1007/s10549-014-2955-1
60. Terry MB, Liao Y, Kast K, et al. The influence of number and timing of pregnancies on breast cancer risk for women with BRCA1 or BRCA2 mutations. JNCI Cancer Spectrum. 2017;2(4):pky078. doi:10.1093/jncics/pky078
61. Cullinane CA, Lubinski J, Neuhausen SL, et al. Effect of pregnancy as a risk factor for breast cancer in BRCA1/BRCA2 mutation carriers. Int J Cancer. 2005;117(6):988–991. doi:10.1002/ijc.21273
62. Kotsopoulos J, Lubinski J, Salmena L, et al. Breastfeeding and the risk of breast cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. 2012;14(2). doi:10.1093/jnci/djh211
63. Buonomo B, Massarotti C, Dellino M, et al. Reproductive issues in carriers of germline pathogenic variants in the BRCA1/2 genes: an expert meeting. BMC Med. 2021;19(1). doi:10.1186/s12916-021-02081-7
64. Lambertini M, Ameye L, Hamy AS, et al. Pregnancy after breast cancer in patients with germline BRCA mutations. J Clin Oncol. 2020;38(26):3012–3023. doi:10.1200/JCO.19.02399
65. Valentini A, Lubinski J, Byrski T, et al. The impact of pregnancy on breast cancer survival in women who carry a BRCA1 or BRCA2 mutation. Breast Cancer Res Treat. 2013;142(1):177–185. doi:10.1007/s10549-013-2729-1
66. Merlino L, Chiné A, Galli C, Piccioni MG. BRCA1/2 genes mutations, ovarian reserve and female reproductive outcomes: a systematic review of the literature. Minerva Ginecol. 2020;72(5). doi:10.23736/S0026-4784.20.04624-9
67. Gronwald J, Glass K, Rosen B, et al. Treatment of infertility does not increase the risk of ovarian cancer among women with BRCA1 or BRCA2 mutation. Fertil Steril. 2016;105(3):781–785. doi:10.1016/j.fertnstert.2015.11.034
68. Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. J Am Coll Radiol. 2018;15:408–414. doi:10.1016/j.jacr.2017.11.034
69. American Cancer Society recommendations for the early detection of breast cancer. Available from: https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html.
70. NCCN guidelines version 2.2022. Genetic/familial high-risk assessment: breast, ovarian, and pancreatic cancers. Available from: https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf.
71. Shenfield F, Pennings G, Devroey P, et al. Taskforce 5: reimplementation genetic diagnosis. Human Reprod. 2003;18(3):649–651. doi:10.1093/humrep/deg110
72. Jasper MJ, Liebelt J, Hussey ND. Preimplantation genetic diagnosis for BRCA1 exon 13 duplication mutation using linked polymorphic markers resulting in a live birth. Prenat Diagn. 2008;28(4):292–298. doi:10.1002/pd.1925
73. Derks-Smeets IAP, de Die-Smulders CEM, Mackens S, et al. Hereditary breast and ovarian cancer and reproduction: an observational study on the suitability of preimplantation genetic diagnosis for both asymptomatic carriers and breast cancer survivors. Breast Cancer Res Treat. 2014;145(3):673–681. doi:10.1007/s10549-014-2951-5
74. Donnelly LS, Watson M, Moynihan C, et al. Reproductive decision-making in young female carriers of a BRCA mutation. Human Reprod. 2013;28(4):1006–1012. doi:10.1093/humrep/des441
75. Rich TA, Liu M, Etzel CJ, et al. Comparison of attitudes regarding preimplantation genetic diagnosis among patients with hereditary cancer syndromes. Fam Cancer. 2013;13(2):291–299. doi:10.1007/s10689-013-9685-0
76. Gietel-Habets JJG, de Die-Smulders CEM, Derks-Smeets IAP, et al. Awareness and attitude regarding reproductive options of persons carrying a BRCA mutation and their partners. Human Reprod. 2017;32(3):588–597. doi:10.1093/humrep/dew352
77. Kiechle M, Engel C, Berling A, et al. Lifestyle intervention in BRCA1/2 mutation carriers: study protocol for a prospective, randomized, controlled clinical feasibility trial (LIBRE-1 study). Pilot Feasibil Stud. 2016;2(1). doi:10.1186/s40814-016-0114-7
78. Grill S, Yahiaoui-Doktor M, Dukatz R, et al. Smoking and physical inactivity increase cancer prevalence in BRCA-1 and BRCA-2 mutation carriers: results from a retrospective observational analysis. Arch Gynecol Obstet. 2017;296(6):1135–1144. doi:10.1007/s00404-017-4546-y
79. Li H, Terry MB, Antoniou AC, et al. Alcohol consumption, cigarette smoking, and risk of breast cancer for BRCA1 and BRCA2 mutation carriers: results from the BRCA1 and BRCA2 cohort consortium. Cancer Epidemiol Biomarkers Prev. 2020;29(2):368–378. doi:10.1158/1055-9965.EPI-19-0546
80. Daniele A, Divella R, Pilato B, et al. Can harmful lifestyle, obesity and weight changes increase the risk of breast cancer in BRCA 1 and BRCA 2 mutation carriers? A mini review. Hered Cancer Clin Pract. 2021;19(1). doi:10.1186/s13053-021-00199-6
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
