Back to Journals » International Journal of General Medicine » Volume 15
Low Serum Total Protein at Admission Predicts in-Hospital Mortality Among General Inpatients: Historical Cohort Study
Authors Inoue M, Takeuchi J , Sakuma M, Nakamura T, Morimoto T
Received 18 August 2022
Accepted for publication 7 October 2022
Published 25 October 2022 Volume 2022:15 Pages 7941—7949
DOI https://doi.org/10.2147/IJGM.S385798
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Miharu Inoue,1 Jiro Takeuchi,2 Mio Sakuma,2 Tsukasa Nakamura,3 Takeshi Morimoto2
1Japanese Red Cross Aichi Medical Center Nagoya Daini Hospital, Nagoya, Japan; 2Department of Clinical Epidemiology, Hyogo Medical University, Nishinomiya, Japan; 3Department of Infectious Diseases, Shimane Prefectural Central Hospital, Izumo, Japan
Correspondence: Takeshi Morimoto, Department of Clinical Epidemiology, Hyogo Medical University, 1-1 Mukogawa, Nishinomiya, Hyogo, 663-8501, Japan, Tel +81-798-45-6879, Fax +81-798-45-6920, Email [email protected]
Purpose: Low total protein (TP) is associated with mortality among patients with specific diseases, but its association was uncertain among general patients. We evaluated the effects of low TP on in-hospital mortality among general inpatients.
Patients and Methods: We used data from the Japan Adverse Drug Events study series. We enrolled adult inpatients (≥ 16 years) admitted to a tertiary care hospital between September 1 and November 30, 2013. We excluded patients with multiple myeloma, pregnant women, and bone marrow graft donors. Patient data were extracted from electronic medical records. All patients were stratified into those with and without malignancy and divided into the low and normal TP groups. Low TP was defined as < 6.5 g/dL. We compared the in-hospital mortality of the low and normal TP groups stratified by the presence of malignancy.
Results: Among the 2235 enrolled patients (mean age, 67.8 years), the TP value was lower in 516 patients with malignancy than in 1719 patients without malignancy (6.6 g/dL vs 6.8 g/dL, P = 0.0002). Among patients without or with malignancy, 27% (462/1719) and 35% (183/516) were in the low TP group, respectively. Mortality was higher in the low TP group among patients without malignancy (23.2% vs 10.2%, P < 0.0001). Likewise, among patients with malignancy, mortality was higher in the low TP group (34.7% vs 11.3%, P = 0.0029). The adjusted hazard ratio of the low TP group was 1.75 (95% confidence interval, 1.04– 2.96) in patients without malignancy and 2.45 (95% confidence interval, 1.12– 5.37) in patients with malignancy, but the interaction was not significant (P = 0.23).
Conclusion: Low TP values were associated with higher in-hospital mortality among general inpatients, and this association was observed among patients with and those without malignancy. Routinely measured TP should be utilized to risk stratification on admission.
Keywords: admission, general patients, historical cohort study, mortality, total protein
Introduction
Total protein (TP) value represents patients’ nutritional conditions1 as well as immune or inflammatory status.2,3 A study including a cohort of 509 acute hip fracture patients showed that 81% of them had protein malnutrition, defined by TP<6.5 g/dl.1 Another study including 46 patients with traumatic spinal cord injury also reported that 49% of them were hypoproteinemic, defined by TP<6.5 g/dl and a significant relationship between the incidence of hypoproteinemia and injury level (p=0.006).4 Thus, malnutrition is common in patients with certain diseases1 but often unrecognized.5 Furthermore, Katsuki et al reported that lower total protein level was associated with poor outcome measured by modified Ranking Scale at 6 months after endoscopic removal of intracranial hematoma.6 These previous reports showed a low TP was associated with spinal cord injury stage and surgical risk of intracranial hemorrhage,4,6 and some other reports also suggested TP as a supplemental marker to predict the prognoses for some disorders, including ischemic stroke and chronic heart failure.5
TP could work as a supplemental marker to predict the prognoses because patients with low nutrition status may have sarcopenia and such patients with sarcopenia may have difficulty in performing rehabilitation due to loss of muscle bulk and function.6 However, the association between low TP and mortality among non-selective patients has not yet been evaluated, and the utility of the measurement of TP at admission for general inpatients was not investigated though TP is routinely measured in daily clinical practice.
The investigation of the impact of TP value at admission on in-hospital prognoses enables better risk stratification or management of all admitted patients in clinical practice. Thus, we conducted a historical cohort study to clarify the relationship between TP value at admission and in-hospital mortality among general inpatients.
Materials and Methods
Study Design and Patients
The data supporting this study are available from the corresponding author upon reasonable requests. We used data from the Japan Adverse Drug Events study series, which comprises cohort studies evaluating adverse drug events in Japan.7–9 We included all adult patients admitted to a tertiary care hospital over a 3-month period from September 1 to November 30, 2013. We excluded patients aged < 16 years on admission since they were not considered adults. Pregnant women and bone marrow graft donors were excluded because they are generally considered healthy. We excluded patients with multiple myeloma because a higher TP value indicates illness severity. Patients for whom TP values at admission were unavailable were excluded.
Ethical Approval
The study protocol complied with the ethical guidelines for medical and health research involving human subjects issued by the Ministry of Health, Labour and Welfare in Japan and the Declaration of Helsinki. This study was approved (R12-055) by the institutional review board at Hyogo Medical University and Shimane Prefectural Central Hospital which waived the requirement for informed consent because all data were obtained as part of daily routine practice.
Data Collection and Outcomes
We extracted information on patient characteristics and laboratory data from electronic medical records. First, we classified all patients into those with and those without malignancy based on the primary disease on admission for stratification. Because our data did not include patients’ history of malignancy, patients with a history of malignancy were considered to have no malignancy when admitted due to another non-malignant primary disease on admission regardless of their unknown past history of malignancy. We then sorted out diseases among patients without malignancy into diseases that were potentially related to a low TP or those were not related. The diseases potentially related to low TP included renal disease, liver disease, hypermetabolic disease, inflammatory bowel disease, burn injury, eating disorder, and alcoholism, and used to be adjusted.
We divided all patients into the low and normal TP groups, and defined a low TP as < 6.5 g/dL.1 The primary endpoint was in-hospital mortality, and we compared the in-hospital mortality between the low and normal TP groups stratified by the presence of malignancy.
Statistical Analysis
Descriptive statistics are presented as mean and standard deviation or median and interquartile range (IQR) for continuous variables and as numbers and percentages for categorical variables. We performed the t-test or Wilcoxon rank sum test for continuous variables and the chi-square test for categorical variables.
All patients were followed up until transfer, discharge, or death; the former two were considered censor for survival analyses. We used the Kaplan-Meier curve and Log rank test to evaluate in-hospital mortality among patients with low and normal TP stratified by the presence of malignancy. We used multivariate Cox proportional hazard models to estimate the effects of low TP on in-hospital mortality; the effects are expressed as hazard ratios (HRs) and their 95% confidence intervals (CIs) for those with and without malignancy separately. We included the following variables in the multivariate models for adjustment: age, sex, diseases potentially related to a low TP, systolic blood pressure, white blood cell count, and estimated glomerular filtration rate (eGFR). Systolic blood pressure reflected patients’ vital signs or shock status, white blood cell count reflected inflammatory or infectious diseases, and eGFR reflected renal function. We constructed the same Cox proportional hazard models to estimate the interaction p value between low TP and the presence of malignancy in all patients.
We used JMP Pro 14.2.0 (SAS Institute Inc., Cary, NC, USA) software for all analyses. Two-tailed p values < 0.05 were considered statistically significant.
Results
A total of 3120 patients were admitted during the study period, while 418 patients younger than 16 years, 365 pregnant women, and four bone marrow graft donors were excluded. We also excluded nine patients with multiple myeloma and 89 patients for whom TP values were missing. Overall, 2235 patients were enrolled in the study (Figure 1).
 |
Figure 1 Study flowchart. |
The mean patient age was 67.8 years; it was similar between those with and those without malignancy (67.9 years vs 67.7 years, respectively; P = 0.79). The percentage of men was 53.2%, and there were more men among those with malignancy than among those without malignancy (57.6% vs 52.0%, respectively; P = 0.025). The mean TP value was 6.75 g/dL; it was lower in patients with malignancy than in those without malignancy (6.6 g/dL vs 6.8 g/dL, respectively; P = 0.0002) (Table 1). Patients with malignancy had significantly lower hemoglobin levels and lower white blood cell counts, but other laboratory test values were numerically similar between those with and those without malignancy (Table 1).
 |
Table 1 Patient Characteristics Stratified by the Presence of Malignancy |
Among patients without malignancy, the low TP group was significantly older and had a lower body mass index (BMI), lower blood pressure, lower hemoglobin, higher white blood cell count, lower platelet count, higher glucose level, higher lactate dehydrogenase level, higher prothrombin time-international normalized ratio, and lower eGFR than the normal TP group. Similarly, patients with malignancy in the low TP group had a lower BMI, lower blood pressure, and lower hemoglobin levels (Table 2).
 |
Table 2 Patient Characteristics Between Patients with Low and Normal Total Protein |
The median length of hospital stay among patients without malignancy was 12 days and 9 days (P < 0.0001) in the low and normal TP groups, respectively, while those of patients with malignancy were 10 days in the low and normal TP groups (P = 0.77) (Table 3).
 |
Table 3 Length of Hospital Stay and in-Hospital Mortality |
A Kaplan-Meier curve for patients without malignancy showed that mortality in the low and normal TP groups were 7.0% and 2.1% at 14 days and 12.0% and 4.3% at 30 days, respectively (Log rank test, P < 0.0001) (Figure 2A). Among patients with malignancy, the mortality of the low and normal TP groups were 4.8% and 0.9% at 14 days and 17.8% and 9.2% at 30 days, respectively (Log rank test, P = 0.0029) (Figure 2B).
 |
Figure 2 In-hospital survival stratified by patients with and without malignancy. (A) Patients without malignancy. (B) Patients with malignancy. |
Crude HRs of low TP relative to the normal TP group were 2.91 (95% CI, 1.77–4.81) in patients without malignancy and 2.98 (95% CI, 1.40–6.34) in those with malignancy (Table 4). The adjusted HRs of the low TP relative to the normal TP group were 1.75 (95% CI, 1.04–2.96) in patients without malignancy and 2.45 (95% CI, 1.12–5.37) in those with malignancy after the adjustment for age, sex, low TP, diseases potentially related to low TP, systolic blood pressure, white blood cell count, and eGFR (Table 4). The interaction between low TP and the presence of malignancy was not significant (P = 0.23).
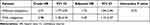 |
Table 4 Hazard Ratios of the Effect of Low Total Protein on Mortality |
Discussion
We explored the association between TP value at admission and in-hospital mortality among general inpatients at a general hospital and found that the TP value was lower among patients with malignancy than among those without malignancy. The mortality at 14 days after admission was higher among patients without malignancy, while that at 30 days after admission was higher among those with malignancy. Regardless of the presence of malignancy, a lower TP value was associated with higher in-hospital mortality. The adjusted HR of the low TP relative to the normal TP group was numerically higher among patients with malignancy.
Several previous studies suggested that a lower TP was associated with poor outcomes in selected patients, such as the worsening of acute heart failure,10 cardiovascular mortality among chronic heart failure patients,11 and worse neurological recovery after endoscopic hematoma removal for intracerebral hemorrhage,6 which are findings consistent with the results of this study. Conversely, to our knowledge, TP levels at admission among general inpatients and the relationship between TP and all-cause mortality were never reported; thus, this is the first study to evaluate the association between low TP and mortality among general patients.
Our results showed that patients with malignancy had lower TP levels than those without malignancy. Inflammation generally provokes hypermetabolism, which results in the loss of protein throughout the body.12 As elevated inflammation and an activated futile cycle utilize large amounts of protein, lipids, and glucose, patients with an active malignancy frequently develop cachexia, also known as energy-wasting syndrome, which accelerates TP loss.13 The decrease in nutritional intake also contributes to low TP in patients with and without malignancy. In this study, among patients with and without malignancy, the low TP group showed a lower BMI and blood pressure. Because TP includes albumin, which maintains colloid osmotic pressure, a lower TP level is related to a lower blood pressure.14 Patients with low TP levels generally have a low BMI because BMI and TP are correlated with protein intake. In addition, lower BMI induces frailty, which leads to a poor prognosis,15 and patients with a lower BMI may have inflammation related to decreased TP levels.16 Malnutrition reportedly weakens the immune system by reducing the number of T lymphocytes and antibody affinity, leading to insufficient T lymphocyte responses to cytokines.2 Therefore, patients with low TP levels may show lower BMI and blood pressure and poorer immune responses, all of which are related to higher mortality.17,18
Our study findings suggest that TP value at admission could be used for a screening to predict patient prognoses as an indicator of nutritional, immune, or inflammatory status and initiate therapeutic interventions. Some protein-related items such as albumin, gamma gap, and albumin-globulin ratio have attracted considerable attention as indicators of patient prognoses;19–21 in this study, TP was also considered useful for the comprehensive assessment of patient conditions. The results of this study are useful for medical professionals as well as patients and their families because when patients show low TP values, doctors can intervene with the nutrition support team and their families can encourage patients to eat more and improve their nutritional status.
Several limitations inherent to the study design must be acknowledged. First, we collected data on TP values only once (at admission) and did not consider changes that occurred during the hospital stay. We recognize the potential variation and importance of follow-up of any measurements; however, many physicians used the initial data for risk stratification, and the primary purpose of this study was to predict the in-hospital mortality based on the TP level at admission. Moreover, we did not routinely measure serum albumin levels at admission. Albumin has been generally used to estimate patients’ nutritional status; thus, we should further investigate whether TP values can be replaced with albumin values to predict in-hospital mortality in the same setting. Second, we classified all patients with their primary diseases at admission into those with malignancy or those without malignancy. We did not take into account the history of malignancy in non-malignancy group. Similarly, the classification of diseases potentially related to low TP might not be accurate and such classification could be misclassified. However, there were no alternative ways to accurately classify the data, and some misclassifications could weaken the effect size if misclassification randomly occurred bidirectionally. Third, we did not include other risk score for general patients, such as CONtrolling NUTritional status (CONUT) score or Charlson Comorbidity Index.22,23 The incremental value of TP to other risk scores should be considered in the future studies. Because TP is generally measured routinely, the utilization of such simple measurement could be prioritized in daily clinical practice. Fourth, we did not evaluate other outcomes than mortality. The baseline TP might be associated with the changes in symptoms and such associations could be observed in some categories of diseases. The impact of TP at baseline on other outcomes should be challenge in clinical practice and future studies. Finally, we conducted this study at a single hospital in Japan without validation cohort. In addition, the length of hospital stay was relatively long. Further similar studies in different settings should be conducted to test the applicability of our results to general medical practice worldwide.
Conclusion
Our study revealed that a lower TP level at admission was associated with higher in-hospital all-cause mortality among general inpatients at general hospitals and that patients with malignancy tended to show lower TP levels at admission than those without malignancy, which indicates that attention should be paid to TP values to increase our understanding of the prognostic value of patients with different diseases.
Acknowledgments
This study used data from the Japan Adverse Drug Effects (JADE) study with Decision Support. We are indebted to Dr. Shinji Kosaka, Dr. Kiyoshi Kikuchi, Mr. Eisaku Hirano, Mr. Kazuo Takeshita, Mr. Tomohiro Sonoyama, Mr. Shuichi Kurahashi, Mr. Koichiro Ichiki, and Mr. Akito Uchio for their support for the JADE study with Decision Support.
Funding
This work was supported by JSPS KAKENHI (Grant Numbers JP18H03032; and JP21H03176).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Díaz de Bustamante M, Alarcón T, Menéndez-Colino R, Ramírez-Martín R, Otero Á, González-Montalvo JI. Prevalence of malnutrition in a cohort of 509 patients with acute Hip fracture: the importance of a comprehensive assessment. Eur J Clin Nutr. 2018;72(1):77–81. doi:10.1038/ejcn.2017.72
2. Chandra RK. Nutrition and the immune system: an introduction. Am J Clin Nutr. 1997;66(2):460s–463s. doi:10.1093/ajcn/66.2.460S
3. Bharadwaj S, Ginoya S, Tandon P, et al. Malnutrition: laboratory markers vs nutritional assessment. Gastroenterol Rep. 2016;4(4):272–280. doi:10.1093/gastro/gow013
4. Lipetz JS, Kirshblum SC, O’Connor KC, Voorman SJ, Johnston MV. Anemia and serum protein deficiencies in patients with traumatic spinal cord injury. J Spinal Cord Med. 1997;20(3):335–340. doi:10.1080/10790268.1997.11719485
5. Zhang H, Shu Y, Zhang J, Tong E. Dynamics of nutritional status in dying patients with acute cerebral infarction in central China: a preliminary study. Neurol Res. 2011;33(5):503–507. doi:10.1179/016164111X13007856084160
6. Katsuki M, Kakizawa Y, Nishikawa A, Yamamoto Y, Uchiyama T. Lower total protein and absence of neuronavigation are novel poor prognostic factors of endoscopic hematoma removal for intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2020;29(9):105050. doi:10.1016/j.jstrokecerebrovasdis.2020.105050
7. Morimoto T, Sakuma M, Matsui K, et al. Incidence of adverse drug events and medication errors in Japan: the JADE study. J Gen Intern Med. 2011;26(2):148–153. doi:10.1007/s11606-010-1518-3
8. Ohta Y, Sakuma M, Koike K, Bates DW, Morimoto T. Influence of adverse drug events on morbidity and mortality in intensive care units: the JADE study. Int J Qual Health Care. 2014;26(6):573–578. doi:10.1093/intqhc/mzu081
9. Yamamoto M, Ohta Y, Sakuma M, Takeuchi J, Matsumoto C, Morimoto T. Association between heart rate on admission and in-hospital mortality among general inpatients: insights from Japan Adverse Drug Events (JADE) study. Medicine. 2019;98(16):e15165. doi:10.1097/MD.0000000000015165
10. van Deursen VM, Edwards C, Cotter G, et al. Liver function, in-hospital, and post-discharge clinical outcome in patients with acute heart failure-results from the relaxin for the treatment of patients with acute heart failure study. J Card Fail. 2014;20(6):407–413. doi:10.1016/j.cardfail.2014.03.003
11. Avaliani T, Talakvadze T, Tabagari S. Influence of nutritional state on outcome in patients with chronic heart failure. Georgian Med News. 2019;288:61–66.
12. Kaysen GA, Greene T, Daugirdas JT, et al. Longitudinal and cross-sectional effects of C-reactive protein, equilibrated normalized protein catabolic rate, and serum bicarbonate on creatinine and albumin levels in dialysis patients. Am J Kidney Dis. 2003;42(6):1200–1211. doi:10.1053/j.ajkd.2003.08.021
13. Argilés JM, Busquets S, Stemmler B, López-Soriano FJ. Cancer cachexia: understanding the molecular basis. Nat Rev Cancer. 2014;14(11):754–762. doi:10.1038/nrc3829
14. Høstmark AT, Tomten SE, Berg JE. Serum albumin and blood pressure: a population-based, cross-sectional study. J Hypertens. 2005;23(4):725–730. doi:10.1097/01.hjh.0000163139.44094.1d
15. Lee Y, Kim J, Han ES, Ryu M, Cho Y, Chae S. Frailty and body mass index as predictors of 3-year mortality in older adults living in the community. Gerontology. 2014;60(6):475–482. doi:10.1159/000362330
16. Nakajima K, Yamaoka H, Morita K, et al. Elderly people with low body weight may have subtle low-grade inflammation. Obesity. 2009;17(4):803–808. doi:10.1038/oby.2008.596
17. Freedman DM, Ron E, Ballard-Barbash R, Doody MM, Linet MS. Body mass index and all-cause mortality in a nationwide US cohort. Int J Obes. 2006;30(5):822–829. doi:10.1038/sj.ijo.0803193
18. Leonardi-Bee J, Bath PM, Phillips SJ, Sandercock PA; Group IC. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke. 2002;33(5):1315–1320. doi:10.1161/01.str.0000014509.11540.66
19. Zhu L, Chen M, Lin X. Serum albumin level for prediction of all-cause mortality in acute coronary syndrome patients: a meta-analysis. Biosci Rep. 2020;40(1). doi:10.1042/BSR20190881
20. Loprinzi PD, Addoh O. The gamma gap and all-cause mortality risk: considerations of physical activity. Int J Clin Pract. 2016;70(7):625–629. doi:10.1111/ijcp.12817
21. Wu PP, Hsieh YP, Kor CT, Chiu PF. Association between albumin-globulin ratio and mortality in patients with chronic kidney disease. J Clin Med. 2019;8(11):1991. doi:10.3390/jcm8111991
22. Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20(1):38–45.
23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
