Back to Journals » International Journal of General Medicine » Volume 14
LncRNA RP11-248E9.5 and RP11-456D7.1 are Valuable for the Diagnosis of Childhood Pneumonia
Authors Chen X, Liu Q, Chen J, Liu Y
Received 9 November 2020
Accepted for publication 5 February 2021
Published 17 March 2021 Volume 2021:14 Pages 895—902
DOI https://doi.org/10.2147/IJGM.S291239
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xiudong Chen, Qing Liu, Juan Chen, Yuhai Liu
Department of Pediatric, Zaozhuang Maternal and Child Health Care Hospital, Zaozhuang City, Shandong Province, 277100, People’s Republic of China
Correspondence: Yuhai Liu
Department of Pediatric, Zaozhuang Maternal and Child Health Care Hospital, No. 25, Wenhua East Road, Shizhong District, Zaozhuang City, Shandong Province, 277100, People’s Republic of China
Tel +86-13969417606
Email [email protected]
Background: Pneumonia is a common infection of the lung parenchyma in children, and early and accurate diagnosis of childhood pneumonia (CP) is important for implementing appropriate preventive and treatment strategies. This study aimed to evaluate the diagnostic value of the combination of long non-coding RNA (lncRNA) RP11-248E9.5, RP11-456D7.1, c-reactive protein (CRP), neutrophil-to-lymphocyte ratio (NLR), and platelet-to-lymphocyte ratio (PLR) in CP.
Patients and Methods: A total of 50 healthy children (HC) and 100 CP patients were enrolled. The serum expression of RP11-248e9.5 and RP11-456d7.1 was detected by qRT-PCR. The white blood cell (WBC), hemoglobin (HB), platelet (PLT), neutrophil, and lymphocyte were analyzed by automated hematology analyzer. The serum levels of CRP and procalcitonin (PCT) were analyzed by automatic biochemical analyzer. The receiver operating characteristic (ROC) curves were applied to evaluate the diagnostic value in CP.
Results: The NLR and PLR, expression of RP11-248E9.5 and RP11-456D7.1, and serum levels of CRP and PCT were significantly higher in the CP group than those in the HC group. Both RP11-248E9.5 (AUC, 0.86; sensitivity, 84%; specificity, 78%) and RP11-456D7.1 (AUC, 0.89; sensitivity, 79%; specificity, 92%) exhibited certain diagnostic value in CP. The diagnostic values of PCT, CRP, NLR and PLR in CP were limited by low sensitivity (≤ 71%). The combination of multiple indicators improved the diagnostic value. The combination of RP11-248E9.5, RP11-456D7.1, CRP, NLR, and PLR had the best diagnostic value in CP (AUC, 0.992; Sensitivity, 0.97; Specificity, 0.99).
Conclusion: The combination of RP11-248E9.5, RP11-456D7.1, CRP, NLR, and PLR was a potential diagnostic strategy for CP.
Keywords: childhood pneumonia, long non-coding RNA, C-reactive protein, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio
Introduction
Pneumonia is the most common cause of childhood death around the world.1 It has been reported that 16% of children under 5 years die of pneumonia every year.2 The early symptoms of childhood pneumonia (CP) are not obvious, exhibiting mild respiratory symptoms. Patients with CP present cough and difficulty breathing with the disease procession.3 Although the symptoms of advanced CP are obvious and easy to find,4 the best period of treatment is missed. Until now, the missed diagnosis is a critical risk factor for death in children with CP complicated by acute respiratory infections.5 It is vital to explore potential biomarkers for the early diagnosis of CP.
Clinically, the diagnostic criteria for CP mainly includes the symptoms of cough, fever, abnormal breathing, the changes of inflammatory factors and platelet (PLT), and the patchy shadow on chest X-ray.3 Diverse biomarkers in blood have been proved to have potential diagnostic value on CP. For instance, PCT has moderate diagnostic accuracy for bacterial pneumonia in children.6 C-reactive protein (CRP) has good value in differentiating bacterial and non-bacterial CP.7 Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) are important in the diagnosis and prognostic evaluation of pneumonia.8,9 However, these indicators are also changed in many other diseases,10–12 which limited their application alone in the diagnosis of CP.
Long non-coding RNAs (LncRNAs) are a kind of non-coding RNAs that participates in the progression of different diseases.13,14 Some lncRNAs have been identified as potential diagnostic markers in pneumonia.15–18 Zhou et al have found that overexpression of lncRNA SNHG16 is related to LPS-induced acute pneumonia.15 Nong et al have displayed that lncRNA NEAT1 plays an important role in the development of pneumonia.16 Zhang et al have reported that lncRNA MIAT2 has been determined to be associated with the onset of neonatal pneumonia.17 Recently, Huang et al have found that lncRNA RP11-248E9.5 and lncRNA RP11-456D7.1 are up-regulated in both the mild and severe pneumonia.19 However, the diagnostic values of RP11-248E9.5 and RP11-456D7.1, as well as the combination with traditional indicators in CP are still unclear.
In this study, we evaluated the diagnostic values of RP11-248E9.5 and RP11-456D7.1, and the combination with traditional indicators (CRP, NLR, and PLR) in CP. Our findings may reveal a potential diagnostic strategy for CP.
Patients and Methods
Clinical Samples
A total of 100 CP patients (3.12 ± 2.02 years old) were collected at our hospital from April 2018 to March 2019, and 50 healthy children (3.24 ± 1.84 years old) were collected as healthy control (HC). CP was defined according to the World health organization’s guidelines for acute respiratory infection.20 All CP patients met the following criteria: 1) The symptoms of cough, fever, and abnormal breathing, and fixed medium and small alveolar sounds in lung; 2) increased neutrophils (> 8×109/L) and PLTs (> 300×109/L) increased significantly; 3) patchy shadows observed by Chest X-ray. Patients with chronic renal or hepatic disease, hematological diseases, inflammatory bowel disease, chronic obstructive pulmonary disease, asthma, and congenital diseases were excluded from this study. This study was approved by the Medical Ethics Committee of our Hospital in accordance with the Declaration of Helsinki. Written informed consent was obtained from the guardians of all patients and HCs.
Detection of Serum Markers
Venous blood samples were collected from patients in the morning with an empty stomach, and the serum was separated by 20 min of centrifugation at 3000 rpm. The white blood cell (WBC), hemoglobin (HB), neutrophil, lymphocyte and PLT were analyzed by BC-6800 Automated Hematology Analyzer (Sun bright, Shanghai, China). NLR and PLR were calculated as the ratio of the neutrophils and PLTs to lymphocytes. The serum levels of C-reactive protein (CRP) and procalcitonin (PCT) were detected by an automatic biochemical analyzer (AU5811, Beckman Coulter, Brea, CA, USA).
Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR)
The total RNAs were extracted from serum using miRcute Serum/Plasma miRNA Isolation Kit (Tiangen, Beijing, China), and were reverse-transcribed into cDNAs using Prime Script RT reagent kit (Tiangen). qRT-PCR was performed using miRcute PlusmiRNA qPCR Detection Kit (Tiangen). The reaction program was 95°C for 2 min and 30 cycles of 95°C for 30 s, 60°C for 30 s and 72°C for 1 min. GAPDH was used as an internal reference. The relative expression level was calculated using the 2−ΔΔCt method. Primer sequences were enlisted in Table 1.
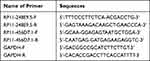 |
Table 1 Primer Sequences Used in qRT-PCR |
Statistical Analysis
All statistical analysis was performed using SPSS 23.0 (Version X; IBM, Armonk, NY, USA). Qualitative data were analyzed using the χ2 test. Quantitative data were presented as the mean ± standard deviation (SD), and comparison between different groups was analyzed by Student’s t-test (two groups) or one-way ANOVA followed by Tukey’s post hoc test (more than two groups). Receiver operating characteristic (ROC) curves were plotted to evaluate the diagnostic value on CP. P < 0.05 was considered to be statistically significant.
Results
The Characteristics of CP Patients
The clinicopathological characteristics of all cases were shown in Table 2. There were no significantly differences in the age, gender, pneumonia type, and HB between the CP and HC groups. The levels of WBC and PLT in the CP group were markedly higher than those in the HC group (P < 0.0001, Table 2).
 |
Table 2 Comparison of Clinical Cases Between Health Control and Childhood Pneumonia Patients |
The Levels of PCT, CRP, NLR, PLR, RP11-248E9.5, and RP11-456D7.1 in CP Patients
As displayed in Figure 1A and B, the serum levels of PCT and CRP were significantly higher in the CP group than that in the HC group (P < 0.05). The NLR and PLR in the CP group were also remarkably higher than those in the HC group (P < 0.05, Figure 1C and D). In addition, the expression of RP11-248E9.5 and RP11-456D7.1 in the CP group was significantly higher than that in the HC group (P < 0.05, Figure 1E and F). Patients were then classified into three categories based on pathogens. The results displayed that there were no significantly differences in the expression of RP11-248E9.5 and RP11-456D7.1 among children with bacterial, viral, and mycoplasma pneumonia (P > 0.05, Table 3).
 |
Table 3 Comparison of LncRNA RP11-248E9.5 and RP11-456D7.1 in Children with Different Types of Pneumonia |
The Diagnostic Values of PCT, CRP, NLR, PLR, RP11-248E9.5, and RP11-456D7.1 in CP
The diagnostic values of PCT, CRP, NLR, PLR, RP11-248E9.5, and RP11-456D7.1 in CP were evaluated by ROC curves. As shown in Figure 2A–F and Table 4, RP11-456D7.1 (0.89) exhibited the highest AUC, followed by RP11-248E9.5 (0.86), PCT (0.8093), NLR (0.8063), CRP (0.7827), and PLR (0.7316). The sensitivity of PCT, CRP, NLR, and PLR in the diagnosis of CP were all ≤ 71%. The sensitivity and specificity of RP11-248E9.5 in the diagnosis of CP were 84% and 78%, respectively. The sensitivity and specificity of RP11-456D7.1 in the diagnosis of CP were 79% and 92%, respectively.
 |
Table 4 The Diagnostic Value of Five Serum Markers in Diagnosis of Childhood Pneumonia (CP) |
The Diagnostic Values of Indicator Combinations in CP
To improve the diagnostic values of RP11-248E9.5 and RP11-456D7.1 in CP, RP11-248E9.5 and RP11-456D7.1 were combined with CRP, NLR, and PLR. As shown in Figure 3A–E and Table 5, the AUC of the combination of traditional indicators (CRP, NLR, and PLR) was 0.8936. The AUC of the combination of RP11-248E9.5 and RP11-456D7.1 was 0.9608. The combination with traditional indicators increased the diagnostic values of RP11-248E9.5 and RP11-456D7.1. The AUC of the combination of RP11-248E9.5, CRP, NLR, and PLR, and the combination of RP11-456D7.1, CRP, NLR, and PLR were 0.963 and 0.9668, respectively. The combination of the above five indexes had the best diagnostic value in CP (AUC = 0.992, sensitivity = 0.97, specificity = 0.99).
 |
Table 5 The Diagnostic Value of RP11-248E9.5 and RP11-456D7.1 Combined with CRP, NLR and PLR in Diagnosis of Childhood Pneumonia |
Discussion
Pneumonia is a serious infection in the lung and remains a major cause of childhood mortality, especially in children under 5 years old.21 In the present study, the NLR and PLR, serum levels of PCT and CRP, and expression of RP11-248E9.5 and RP11-456D7.1 in CP children were significantly higher than those in HC children. RP11-248E9.5 and RP11-456D7.1 were proved to have a certain value in the diagnosis of CP, and their combination with traditional indicators can further improve the diagnostic value.
LncRNAs are involved in the occurrence and progression of pneumonia.15–18 Recently, Huang et al have found that RP11-248E9.5 and RP11-456D7.1 are up-regulated in pneumonia, and there is a difference in the expression of RP11-248E9.5 and RP11-456D7.1 between mild and severe pneumonia.19 In our study, the expression of RP11-248E9.5 and RP11-456D7.1 was significantly higher in CP patients than those in HC. We speculated that monitoring the expression of RP11-248E9.5 and RP11-456D7.1 may aid in the diagnosis of CP to a certain extent. The diagnostic values of RP11-248E9.5 and RP11-456D7.1 in CP were further analyzed. The ROC curve analysis indicated that both RP11-248E9.5 and RP11-456D7.1 had certain diagnostic values for CP. The AUC of RP11-248E9.5 and RP11-456D7.1 were both higher than 0.8. The sensitivity and specificity values of RP11-248E9.5 were 84% and 78% and the sensitivity and specificity of RP11-456D7.1 were 79% and 92%, respectively. These data indicated that RP11-248E9.5 and RP11-456D7.1 may be potential diagnostic markers of CP. Until now, the knowledge on the molecular mechanisms of RP11-248E9.5 and RP11-456D7.1 in pneumonia is still limited. Based on previous studies, we speculated that RP11-248E9.5 may be involved in pneumonia through regulating QRFP/G-protein coupled receptor signaling pathway, and RP11-456D7.1 may be involved in pneumonia via targeting CCL21.19 The detail molecular mechanisms of these two lncRNAs in CP need to be further explored.
CRP is a non-specific marker of inflammation, and its level is relatively low in the blood of healthy people. CRP increases sharply in a short time when organs or tissues are damaged or infected, which plays a protective role in the process of human natural immunity.22 Notably, the increased level of CRP is also closely to be associated with co-infections of different pathogens in CP.23 CRP has been reported to be valuable in distinguishing bacterial from the respiratory syncytial virus-associated pneumonia among children.24 In our study, the CRP level in CP patients was markedly higher than that in HC. In addition, ROC curve analysis showed that the AUC of CRP in the diagnosis of CP was 0.7827, and the sensitivity and specificity were only 71% and 76%, respectively. These results indicated that CRP alone is limited in the diagnosis of CP. In inflammatory diseases, the characteristics of NLR are increased neutrophils and decreased lymphocytes.25 A high level of NLR is usually associated with inflammation in pneumonia.26 Bekdas et al have found that the combination of NLR and CRP/mean PLT volume ratio can be used for the differential diagnosis of bacterial and viral pneumonia in children.27 PLR is another marker for disclosing the changes in PLT and lymphocyte counts caused by acute inflammatory states.28 PLR is positively correlated with CRP in pneumonia, and the activated PLT can trigger inflammation.29 Kartal et al have concluded that elevated PLR has diagnostic value to identify community-acquired pneumonia.8 In this study, the levels of NLR and PLR were significantly increased in CP patients. However, NLR and PLR were not sensitive and specific enough in diagnosis of CP (NLR: sensitivity, 71%; specificity, 84%; PLR: sensitivity, 64%; specificity, 84%).
Due to the diversity of pathogenic factors and clinical manifestations of CP, the application value of single traditional indicator in the diagnosis of CP is challenged seriously. The combined application of multiple indicators is imperative which can greatly improve the diagnostic value of individual indicators alone.30 Liu et al have reported that PCT in combination with hs-CRP facilitates the early diagnosis of pneumonia complicated by sepsis in new-born.31 In our study, the diagnostic values of the combinations of CRP, NLR, PLR, RP11-248E9.5 and/or RP11-456D7.1 were further evaluated. Compared with the combination of traditional indicators (CRP, NLR, and PLR), the AUC of the combination of RP11-248E9.5 and traditional indicators was increased by 7.77%, and the AUC of the combination of RP11-456D7.1 and traditional indicators was increased by 8.19%. In addition, the combination of five indexes had the best diagnosis value in CP with an AUC of 0.992. These results indicated that the combination of multiple indicators may improve the diagnostic efficacy of a single indicator. To sum up, the combination of RP11-248E9.5, RP11-456D7.1, CRP, NLR, and PLR was recommended in the diagnosis of CP. However, this set of biomarkers may be complicated in clinical practice. More simplified diagnostic strategies still need to be studied in the future.
Conclusion
The NLR and PLR, serum levels of PCT and CRP, and expression of RP11-248E9.5 and RP11-456D7.1 were remarkably increased in CP patients. RP11-248E9.5 and RP11-456D7.1 have a certain value in the diagnosis of CP. The combinations of RP11-248E9.5 and RP11-456D7.1 with conventional indicators (CRP, NLR, and PLR) greatly improved the diagnostic efficiency. The combination of RP11-248E9.5, RP11-456D7.1, CRP, NLR, and PLR is recommended in the diagnosis of CP.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Informed Consent
This study was approved by the Medical Ethics Committee of Zaozhuang Maternal and Child Health Care Hospital in accordance with the Declaration of Helsinki. Written informed consent was obtained from the guardians of all patients and HCs.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2(1):25–32. doi:10.1016/S1473-3099(01)00170-0
2. Hug L, Sharrow D, You D. Levels & trends in child mortality: report 2017. Estimates developed by the UN inter-agency group for child mortality estimation; 2017.
3. Shah SN, Bachur RG, Simel DL, Neuman MI. Childhood Pneumonia. JAMA. 2017;318(5):490. doi:10.1001/jama.2017.9428
4. Palafox M, Guiscafré H, Reyes H, Munoz O, Martínez H. Diagnostic value of tachypnoea in pneumonia defined radiologically. Arch Dis Child. 2000;82(1):41–45. doi:10.1136/adc.82.1.41
5. Hortensia R, Perez-Cuevas R, Salmeron J, Tome P, Guiscafre H, Gutierrez G. Infant mortality due to acute respiratory infections: the influence of primary care processes. Health Policy Plan. 1997;12(3):214–223. doi:10.1093/heapol/12.3.214
6. Tsou PY, Rafael J, Ma YK, et al. Diagnostic accuracy of procalcitonin for bacterial pneumonia in children - a systematic review and meta-analysis. Infect Dis. 2020;52(10):683–697. doi:10.1080/23744235.2020.1788719
7. Gauchan E, Adhikari S. C-reactive protein versus neutrophil/lymphocyte ratio in differentiating bacterial and non-bacterial pneumonia in children. J Nepal Health Res Counc. 2016;14(34):154–158.
8. Kartal O, Kartal AT. Value of neutrophil to lymphocyte and platelet to lymphocyte ratios in pneumonia. Bratisl Lek Listy. 2017;118(9):513–516. doi:10.4149/BLL_2017_099
9. Zhang HF, Ge YL, Wang HY, et al. Neutrophil-to-lymphocyte ratio improves the accuracy and sensitivity of pneumonia severity index in predicting 30-day mortality of CAP patients. Clin Lab. 2019;65(10):190226. doi:10.7754/Clin.Lab.2019.190226
10. Danilov C, Ihle C, Fernandez FF, Blumenstock G, Wirth T, Eberhardt O. Pseudo paralysis of the shoulder and increased C-reactive protein are predictive factors for septic shoulder in children superior to other clinical symptoms: a retrospective case series of 25 patients. J Child Orthop. 2020;14(1):85–90. doi:10.1302/1863-2548.14.190126
11. Dursun A, Ozsoylu S, Akyildiz BN. Neutrophil-to-lymphocyte ratio and mean platelet volume can be useful markers to predict sepsis in children. Pak J Med Sci. 2018;34(4):918–922. doi:10.12669/pjms.344.14547
12. Aktar F, Tekin R. Mean platelet volume, neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in determining the diagnosis or outcome in children with snakebite. Arch Argent Pediatr. 2017;115(6):576–580. doi:10.5546/aap.2017.eng.576
13. Li J, Meng H, Bai Y, Wang K. Regulation of lncRNA and its role in cancer metastasis. Oncol Res. 2016;23(5):205–217. doi:10.3727/096504016X14549667334007
14. Tsai MC, Spitale RC, Chang HY. Long intergenic noncoding RNAs: new links in cancer progression. Cancer Res. 2011;71(1):3–7. doi:10.1158/0008-5472.CAN-10-2483
15. Zhou Z, Zhu Y, Gao G, Zhang Y. Long noncoding RNA SNHG16 targets miR-146a-5p/CCL5 to regulate LPS-induced WI-38 cell apoptosis and inflammation in acute pneumonia. Life Sci. 2019;228:189–197. doi:10.1016/j.lfs.2019.05.008
16. Nong W. Long non-coding RNA NEAT1/miR-193a-3p regulates LPS-induced apoptosis and inflammatory injury in WI-38 cells through TLR4/NF-κB signaling. Am J Transl Res. 2019;11(9):5944–5955.
17. Zhang H, Zhao J, Shao P. Long noncoding RNA MIAT2 alleviates lipopolysaccharide-induced inflammatory damage in WI-38 cells by sponging microRNA-15. J Cell Physiol. 2020;235(4):3690–3697. doi:10.1002/jcp.29263
18. Chi X, Ding B, Zhang L, Zhang J, Wang J, Zhang W. lncRNA GAS5 promotes M1 macrophage polarization via miR-455-5p/SOCS3 pathway in childhood pneumonia. J Cell Physiol. 2019;234(8):13242–13251. doi:10.1002/jcp.27996
19. Huang S, Feng C, Chen L, et al. Identification of potential key long non-coding RNAs and target genes associated with pneumonia using long non-coding RNA sequencing (lncRNA-Seq): a preliminary study. Med Sci Monit. 2016;22:3394–3408. doi:10.12659/MSM.900783
20. Scott JAG, Wonodi C, Moïsi JC, et al. The definition of pneumonia, the assessment of severity, and clinical standardization in the pneumonia etiology research for child health study. Clin Infect Dis. 2012;54(suppl_2):S109–S116. doi:10.1093/cid/cir1065
21. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the sustainable development goals. Lancet. 2016;388(10063):3027–3035. doi:10.1016/S0140-6736(16)31593-8
22. Zhao J-L, Wang X, Wang Y-S. Relationships between Th1/Th2 cytokine profiles and chest radiographic manifestations in childhood mycoplasma pneumoniae pneumonia. Ther Clin Risk Manag. 2016;12:1683–1692. doi:10.2147/TCRM.S121928
23. Nathan AM, Teh CSJ, Jabar KA, et al. Bacterial pneumonia and its associated factors in children from a developing country: a prospective cohort study. PLoS One. 2020;15(2):e0228056. doi:10.1371/journal.pone.0228056
24. Higdon MM, Le T, O’Brien KL, et al. Association of C-Reactive protein with bacterial and respiratory syncytial virus-associated pneumonia among children Aged <5 years in the PERCH study. Clin Infect Dis. 2017;64(suppl_3):S378–S386. doi:10.1093/cid/cix150
25. Jimenez MF, Watson RW, Parodo J, et al. Dysregulated expression of neutrophil apoptosis in the systemic inflammatory response syndrome. Arch Surg. 1997;132(12):1263–1269. doi:10.1001/archsurg.1997.01430360009002
26. Lee JH, Yoon SY, Kim HS, Lim CS. Characteristics of the mean platelet volume, neutrophil to lymphocyte ratio, and C-reactive protein compared to the procalcitonin level in pneumonia patients. Platelets. 2014;26(3):278–280. doi:10.3109/09537104.2013.875138
27. Bekdas M, Goksugur SB, Sarac EG, Erkocoglu M, Demircioglu F. Neutrophil/lymphocyte and C-reactive protein/mean platelet volume ratios in differentiating between viral and bacterial pneumonias and diagnosing early complications in children. Saudi Med J. 2014;35(5):442–447.
28. Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The platelet-to-lymphocyte ratio as an inflammatory marker in Rheumatic diseases. Ann Lab Med. 2019;39(4):345–357. doi:10.3343/alm.2019.39.4.345
29. Lee JH, Song S, Yoon SY, Lim CS, Song JW, Kim HS. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as diagnostic markers for pneumonia severity. Br J Biomed Sci. 2016;73(3):140–142. doi:10.1080/09674845.2016.1209898
30. Tantai J, Hu D, Yang Y, Geng J. Combined identification of long non-coding RNA XIST and HIF1A-AS1 in serum as an effective screening for non-small cell lung cancer. Int J Clin Exp Pathol. 2015;8(7):7887–7895.
31. Liu GB, Cui XQ, Wang ZB, Wen L, Duan HL. Detection of serum procalcitonin and hypersensitive C-reactive protein in patients with pneumonia and sepsis. J Biol Regul Homeost Agents. 2018;32(5):1165–1169.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



