Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Learning from the Experiences in the COVID-19 Pandemic – Impact on Quality of Life and Challenges for the Staff of a Dermatological Hospital and Rehabilitation Center in Germany: A Retrospective Analysis
Authors Kuhls LJ, Demiri J, Weidlich A, Weidlich S, Trinkaus J, Steinbrink K , Augustin M , Tsianakas A
Received 2 August 2023
Accepted for publication 10 October 2023
Published 13 November 2023 Volume 2023:16 Pages 3279—3290
DOI https://doi.org/10.2147/CCID.S429065
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Lorenz Julius Kuhls,1 Jeta Demiri,1 Adam Weidlich,1 Susanne Weidlich,1 Janin Trinkaus,1 Kerstin Steinbrink,2 Matthias Augustin,3 Athanasios Tsianakas1
1Department of Dermatology and Allergology, Fachklinik Bad Bentheim, Bad Bentheim, Germany; 2Department of Dermatology, University Hospital Münster, Münster, Germany; 3Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany
Correspondence: Athanasios Tsianakas; Lorenz Julius Kuhls, Department of Dermatology and Allergology, Fachklinik Bad Bentheim, Bad Bentheim, 48455, Germany, Tel/Fax +49 5922 74-52 10, Email [email protected]; [email protected]
Purpose: During the COVID-19 pandemic, infections could also be detected among the staff and patients of the dermatological hospital Bad Bentheim (Germany). This retrospective analysis aims to better understand the impact of the pandemic on health care workers. The results could help improve future pandemic plans and measures to protect health care workers.
Patients and Methods: In 2020, the whole staff (460 participants) of the dermatological hospital Bad Bentheim had been offered the option to be tested with respect to the antibody status on SARS-CoV-2 (IgG, IgM). The data were collected by means of a blood sample and subsequent questionnaires (22 questions for employees with positive SARS-CoV-2 serology) regarding disease severity, symptoms, disease duration, chains of infection, psychological and physical burden. Both groups were divided by positive or negative serology and data analysis was performed using an independent t-test.
Results: It was shown that a COVID-19 Infection clinically presented itself as a respiratory tract infection, differed significantly in severity and duration, but also the long-term consequences in employees with proven COVID-19 disease (n=14, 3.7%) from the employees with non-COVID-19 respiratory diseases (33.6% of the seronegative employees). In addition, there was a significant psychological impairment and burden of COVID-19-affected employees. Our study showed unique insights into infection chains, disease courses, disease severity, symptoms and a significant psychological impairment and burden of COVID-19-affected employees among the COVID-19 positive staff.
Conclusion: Our study shows deep insights into infection chains, disease courses, disease severity and symptoms among the COVID-19 positive staff and led to change of behavior with the disease itself and among the health care professionals. This knowledge has the potential to positively influence the handling of similar future events.
Plain Language Summary: Due to the nature of the Corona pandemic with massive effects, especially in the environment of health care facilities, we provide a detailed insight into the stresses on employees in a dermatological acute and rehabilitation clinic. To recognize their stress and to monitor the maintenance and quality of patient care, it is important to focus especially on the effects of an infection with SARS-CoV-2 of these employees and to analyze them. This revealed insights into the disease trajectories of staff infected with COVID-19 with significant differences compared to healthy individuals. Starting with physical symptoms and ending with psychological stress.
Keywords: COVID-19, SARS-CoV-2, immunoassay, infection chain, hospital staff
Introduction
After the first description of a series of cases of pneumonia caused by the novel SARS-CoV-2 (severe acute respiratory syndrome coronavirus type 2),1,2 the first description of a case of COVID-19 (coronavirus disease 2019) occurred in Germany on January 27, .2020.3 From March 2020, the rapid spread of the virus also occurred in Germany as part of the pandemic situation that continues to this day. Also, in the specialist clinic Bad Bentheim, located in the west of Lower Saxony, with a dermatological hospital for in-patients plus a dermatological rehabilitation center, the first positive cases occurred in March 2020 both among patients and employees with corresponding physical, and psychological consequences. The pandemic itself can lead to a pronounced general uncertainty and fear of infection.4,5 This was also evident among the staff of the institution with strongly expressed fears regarding future dealings with patients, but also with regard to dealings between staff members. Uncertainty also prevailed regarding a possible SARS-CoV-2 disease that had already been contracted and the hope of attainment of immunity. To counteract this situation, the entire staff was offered the opportunity to be tested for SARS-CoV-2 infection after the first wave of infection had subsided in summer 2020 and to participate in a survey on physical and psychological stress. Research questions were, on the one hand, the evaluation of the chains of infection (patients/colleagues/private environment) and recording of the symptoms, severity and duration of the disease. On the other hand, the aspects of psychological stress as well as the handling of the pandemic situation and the result of the infection status of the affected employees were to be analyzed. Given the emergence of SARS-CoV-2 as recently as late 2019, such a study of an entire health care institution workforce, including the aforementioned survey, is unique. Although national and international studies on immune responses of a workforce can now be found in the literature, these studies on screening in health care institutions are purely epidemiological in nature and do not go beyond the mere descriptive analysis of an infection situation.6–8
Despite the advances in research and treatment of COVID-19, there are still many limitations and uncertainties that hospital staff face in their daily work. The high risk of transmission and infection among hospital staff, especially in settings with inadequate infection prevention and control measures, high workload, and staff shortages as well as the psychological and emotional impact of COVID-19 on hospital staff, who may experience stress, anxiety, burnout, moral distress, compassion fatigue, grief, and trauma.
The aim of this study is to analyze especially these problems hospital workers face and support them with adequate resources, guidance, training, and mental health services.
The results of our investigation are presented below.
Materials and Methods
The quantitative cross-sectional study was conducted monocentrically at the Fachklinik Bad Bentheim after approval by the Ethics Committee of the Medical Association of Lower Saxony (Germany) in accordance with the Declaration of Helsinki. The sample size are all employees of the Fachklinik Bad Bentheim who had reached the age of 18 and wished to participate in the study were eligible for participation. The target sample size was 460 participants. The data was collected by means of a blood sample and subsequent questionnaires. The study is thus observational and is divided into the following two steps:
Step 1: Initially, after detailed information over a period of 4 weeks (June 2020), all employees of the clinic were asked to voluntarily provide a blood sample (approx. 7 mL serum blood). The blood sample was taken to detect any SARS-CoV-2 infection that may have already been passed. In the context of the clarification, a query in connection with the virus (eg, already accomplished throat swab with PCR proof of SARS-CoV-2, contacts to persons ill with COVID-19, journeys into risk areas) took place at the same time.
Step 2: Subsequently, the verifiably tested positive persons (IgG positive; in case of IgM positive only, retesting after 4 weeks, evaluation as positive only in case of IgG positivity; test kit Medac Snibe CLIA Immunoassay IgG and IgM) were further questioned 22 questions on the topics of health status, infection chain, symptoms, severity, and duration of the disease as well as on the psychological burden and impact on the occupational activity (questionnaire for seropositive employees – see Supplement 1).
Tested negative employees also received a questionnaire of 10 questions as a reference group (questionnaire for seronegative employees – see Supplement 2). This questionnaire asked about the occurrence of other respiratory tract infections during the same observation period (February to June 2020) and their symptoms, severity and duration. Furthermore, employees who had been tested negative were asked how they personally conceived the blood test result and whether this may have changed their attitude towards work. They were also asked whether they trusted the results of the blood test.
The questions are mainly based on the standardized and validated questionnaire of the Hamburg City Health Study (with the kind permission of Professor Dr Matthias Augustin, University Hospital Hamburg-Eppendorf, Germany).9 Its Version 1.0 from 05.06.2020, responsible PD Dr med. Athanasios Tsianakas. The finally used questionnaire has not been validated in whole since it was a unique questionnaire in an acute situation (COVID-19 pandemic) with no chance for prior testing or validation in a pilot project.
Data analysis was performed using an independent t-test. The t-tests test whether independent groups differ with respect to the mean of a metric characteristic. Groups were divided by positive or negative serology. All statistical tests were two-sided with a significance level of 0.05. In addition, bar graphs were created to provide a visual check between groups.
Results
A total of 383 (83%) of the 460 employees of the Fachklinik Bad Bentheim took part in the study. A positive serology (IgG positive) and thus a proven infection, showed 14 of the 383 employees (3.7%). Among them were 10 women and 4 men with a respective average age of 43 years (vs 45 years for IgG-negative employees). Only in 5 of these 14 employees had the infection been known in advance (confirmation by PCR throat swab).
The response rate of the questionnaires of the tested positive group was 100%. Of the total of 369 employees with negative serology, 271 completed the assigned questionnaire (73.4%, of which 74% were women and 26% men).
Thirteen of the 14 employees who had been tested positively could recall an acute episode of illness since February 2020. However, also 13 out of 14 employees (92.9%) considered themselves to be back in good to excellent health at the time of the survey (Figure 1).
 |
Figure 1 Current health status of employees tested positive for IgG (n=14). |
Half of the employees with a positive serology (n=7) stated that they had had close contact to a person who had been tested positively for SARS-CoV-2. The contact occurred in all of the cases without protective face masks (100%) and in 50% in addition without observing the minimum distance of 1.5 meters. The source of infection is largely seen to be patients or colleagues (Figure 2). In order to investigate the question of how the Corona pandemic might endanger jobs, the employees with a positive serology were asked about their assessment of whether they saw their jobs or their professional existence as being at risk. Here, 10 out of 14 answered that they would rather not agree or not at all agree with this endangerment, 3 would rather agree and one of the respondents fully agreed (Figure 3). This therefore equates to a percentage of 28.6% who answered in the affirmative that they were at risk. Only two of the employees with positive serology also saw their partner’s job or professional existence at risk.
 |
Figure 2 Suspected source of infection of IgG-positive tested employees (n=14). |
 |
Figure 3 View of IgG-positive tested employees, whether there is a threat to the job/professional existence (n=14). |
Furthermore, the employees with a positive serology were asked which complaints had affected them in the last 2 weeks and if yes in which frequency; multiple answers were possible (Table 1). The interrogation showed that a large proportion (in %) of the 14 employees who had been tested positive suffered from symptoms such as little interest/enjoyment in activities, low spirits, sleep complaints as well as tiredness and lack of energy on at least some days. In particular, 5 out of 14 employees suffered from fatigue on more than half of the days.
 |
Table 1 Frequency of Complaints Within the Last 2 Weeks in IgG-Positive Tested Employees (n=14) |
It was also asked to what extent these employees had experienced feelings of lack of company, social isolation, or being left out in the last 4 weeks (Figure 4). Compared to the time before the Corona pandemic, one or more of these feelings had tended to increase for 8 of the 14 individuals. In addition, the tested positive employees were asked which events generally frightened them (Figure 5). This showed that the fear of the corona virus was comparable to that of cancer, stroke or heart attack. In the course of the questionnaires, both the employees with positive and negative serology for SARS-CoV infection were asked whether they could recall at least one specific episode of illness in the period from February to June 2020 (present in 13 of the employees with a positive serology). Of the employees with negative serology, 91 out of 271 (33.6%) reported at least one episode of illness in the mentioned period (mainly February and March, 43 and 57 events, respectively). While the tested positive employees felt acutely ill for 14 days during their illness (range 2–38 days), this figure averaged 10 days (2–84 days) for the employees with negative serology. The difference was not significant (p=0.255). 41% (37/91) of the seronegative group reported a period of general fatigue and weakness after the acute phase of illness had subsided, with an average duration of 12 days. In the seropositive group, however, 8 out of 14 (57%) reported a period of general weakness after the acute phase of illness had subsided (one employee of the tested positive group did not recall any phase of illness). The average duration here was 29 days (statistically significantly longer than in the seronegative group, p=0.001) and in 2 of the 14 employees the fatigue or weakness lasted until the day of the interview.
 |
Figure 4 Feelings during the last 4 weeks in IgG-positive tested employees (n=14). |
 |
Figure 5 Fear of events (IgG-positive tested employees, n=14). |
Furthermore, both cohorts were asked about symptoms during the acute phase of the disease (Table 2). There was a significant difference between the groups for the symptom’s “rhinitis” (more frequent in the seronegative group, p=0.026), “olfactory disturbance” (more frequent in the seropositive group, p=0.021) and “other symptoms” (more frequent in the seropositive group, p=0.035). The seropositive group also reported symptoms such as thoracic tenderness, exanthema, paresthesia, hair loss, digital thrombi (COVID toes), sneezing, and increased blood pressure. All additionally mentioned symptoms were mentioned only once.
 |
Table 2 Symptoms During the Acute Phase of the Disease (IgG-Positive versus -Negative Tested Employees, 14 versus 91) |
Regarding the severity of the feeling of illness, the employees with positive serology showed a more severe feeling of illness compared to those who had been tested negative (46.2% versus 15.4%), Table 3. Both cohorts showed a similar frequency whether they were unable to work during the period of illness (employees who tested positive in 61.6% versus those who tested negative in 58.2%). The questionnaires also took into account how the result of the blood test was conceived by the employees (Table 4), multiple answers were possible. The question was asked of all employees, ie, also of those who had not experienced an episode of illness. For the positive cohort, significantly higher values were found for the feeling “caused anxiety” (p<0.001), but also “relief” (p=0.029). In addition, both groups were asked whether their attitude towards work changed after the blood result was announced. Table 5 shows the possible answers to this question. Again, multiple answers were possible. A significant difference between the groups existed only for the answer “more relaxed” (p=0.017) with higher values for those with a positive serology. The answer option “disappointed” was only reserved for the tested negative group. The tested positive employees also indicated that they had become more cautious and accurate as a result of the blood result. These responses are also reflected in the “Other” statements among the tested negative employees. They state that they have become more hygiene-conscious and more careful.
 |
Table 3 Severity of Acute Illness (IgG -ositive versus -Negative Tested Employees, 14 vs 91) |
 |
Table 4 Blood Test Result Uptake (IgG-Positive vs Negative Tested Staff, 14 vs 271) |
 |
Table 5 Work Attitude After Blood Result Announcement (IgG-Positive vs -Negative Tested Employees, 14 vs 271) |
Finally, both groups were asked whether they trusted the result of the blood test. In the case of the tested positive employees, 10 out of 14 employees (71%) stated this. In the tested negative group, 84.9% trusted the result of the test, 14.4% were unsure and only 0.7%, ie, 2 employees, did not trust the blood test (Table 6).
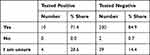 |
Table 6 Credibility of Blood Test Results Blood Test Results (IgG-Positive vs -Negative Tested Employees, 14 vs 271) |
Discussion
The presented results show the acute symptoms but also the later (psychological) stress of employees of a dermatological health care facility in Germany who fell ill with SARS-CoV2 in comparison to the employees who did not fall ill during the first half of the year 2020 corresponding to the beginning of the pandemic. Due to the explosive nature of the current Corona pandemic with its massive impact on the health and economy of the entire world population till today, investigations into the infection situation, but above all into its effects on the people affected, have the highest priority. Since especially in the environment of health care facilities such as acute or rehabilitation clinics the employees are confronted with the fates of traumatized and chronically ill people on a daily basis, it is even more important to also address the psychological stresses of these employees and to analyze the effects of extraordinary stresses such as that of an infection with SARS-CoV-2. Overall, the study met with a high level of acceptance within the staff of the clinic, with a participation rate of 83%. It must be mentioned that this population is of course not representative of the normal population but can only represent the population working in a (dermatological) health care facility in Germany. This means that the elderly population, which is particularly vulnerable with regard to SARS-CoV2, was excluded. For example, it is known that for people over 65 years of age, age is the strongest predictor for intensive care treatment. Seventy-one percent of the tested positive employees suspected that the infection had occurred via their professional environment. This assumption is based on the knowledge of positive cases in the close collegial or patient environment. As a special feature, it must be emphasized here that the general hygiene and safety measures such as the wearing of medical or FFP2 masks and the observance of minimum distances were not yet known at the time of the infection of our study participants in spring 2020 and therefore had not been taken. Thus, in all 7 cases with suspected sources of infection via patients, the minimum distance was not maintained as part of medical care and no protective mask was worn. This increased risk potential of people working in the health care sector could also be shown in an observational study from the USA and can be well explained by the close physical contacts between practitioner and patient.10 This increased risk explains the high rates of health care workers among SARS- CoV-2 positive cases for example in Spain (20.4%) or Italy (10.7%).11–13 These high rates of disease also cause high numbers of deaths among health care workers, as shown, for example, by a publication of the World Health Organization (WHO) in September 2021.14 The population-based number of deaths due to COVID-19 in health care workers till May 2021 was estimated to be about 115 493. In the medical field, it was not until calendar week 16 (mid-April) in 2020 that the implementation of recommendations and measures to control COVID-19 outbreaks, including the wearing of oral-nasal protection, appeared to have a positive impact.15,16 Other protective measures such as vaccinations had not been developed yet at that time point.
However, attitudes towards work have not changed based on our test results. This is remarkable, as other studies (not primarily in the health care sector) show that attitudes towards work have changed significantly since the pandemic. In particular, digital transformation and home office seem to play a major role.17 In health care professions, however, little has changed, which in turn fits in with our findings. With regard to the symptoms of the tested positive and symptomatic employees in comparison to the tested negative employees, who had also shown symptoms of illness during the period under investigation, there were clear differences in the symptom spectrum. For example, there were significant differences in the symptom of olfactory dysfunction, which was significantly more common in the employees who tested positive than in those who tested negative (30.8% vs 9.8%). Conversely, the symptom of rhinitis was significantly more common in those who tested negative than in those who tested positive (62.6% vs 30.8%). More common, but not significant, symptoms in those who tested positive were fever, chills, taste disturbance, and also gastrointestinal symptoms such as nausea and diarrhea. The occurrence of olfactory and gustatory disturbances in up to 75.7% has been described in many international studies.18,19 In contrast, eg the German National Health Care Institute (Robert Koch Institute, RKI) describes as epidemiological profile of SARS-CoV-2 and COVID-19, loss of smell and/or taste as only to be found in 20%.20 This rather low figure compared to our rate can be explained by the fact that although the RKI has been recording the symptoms of COVID-19 sufferers since the 19th calendar week of 2020, these are however only recorded via the reporting system and here symptoms are recorded less frequently and accurately than in clinical studies, for example.
Regarding the severity of the feeling of illness, it was found that the employees with COVID-19 reported a severe feeling of illness more often than those tested negatively (46.2% vs 15.4%). Also, the mean duration of acute symptoms of illness was longer in those who had been tested positively, 14 versus 10 in those with a negative serology. This is consistent with the known severe disease courses, for example, in the comparison of COVID-19 to influenza.21 Despite all the differences in symptom expression and disease severity, however, no clear distinction can be made clinically between COVID-19, influenza and other “flu-like” diseases.22
With regard to the persistence of general fatigue and weakness after the acute symptoms of the disease had subsided, this was reported by 57% of those with positive serology, but only by 42% of those who had been tested negative. This fatigue also lasted significantly longer (29 vs 12 days) in the tested positive employees. Encouragingly, the vast majority of participants (13/14) reported being back in good health at the time of the survey. But a feeling of general lassitude was nevertheless reported by 2 of the 14 staff who tested positive (14%) as persisting up to the time of the interview. One of these two employees also reported suffering from effluvium as well as new-onset paresthesia of the hands and feet, in addition to persistent marked fatigue (during the resolution of acute COVID-19 symptoms, this employee had experienced the appearance of COVID toes, a livid discoloration of the toes and sometimes the fingers, explained by a lymphocytic vasculitis23 as well as partial thromboembolic vascular occlusion.24). This clinical feature of COVID-19-associated cutaneous manifestations, a chilblain-like acral lesions, is one of the more frequent manifestations together with maculopapular eruptions.25 The pronounced fatigue symptoms lasting for weeks and months are very compatible with the occurrence of a so-called “long COVID” or “post-COVID syndrome”. These terms describe the long-term consequences of COVID-19 disease.26 These sequelae occur both after hospitalization in more severe and in milder courses.27 The long-term symptoms mainly include chronic fatigue, but also impaired memory, memory problems or word-finding disorders. In addition, somatic symptoms such as shortness of breath, but also depressive symptoms are common. Risk factors for the development of long COVID appear to be advanced age, high BMI and pre-existing lung diseases.28
However, not only the infection itself but the entire situation related to COVID-19 poses a major challenge to the population. Our study shows that the fear of COVID-19 (in IgG-positive tested employees) is comparable to the fear of cancer, strokes or heart attacks. A survey of 1003 men and women by the Forsa Institute on behalf of the German health insurance company DAK-Gesundheit had shown in October 2020 that Germans were most afraid of cancer (72%), in our study 50%, fear of COVID-19 ranked seventh with 37% in the Forsa survey (40% in our study).29 However, these figures are difficult to compare with our survey, because in our study only the employees with positive serology were asked. It should also be mentioned at this point that overall, a bias could possibly result from the large difference between the two cohorts in our study (seropositive and seronegative).
In addition, the study looked at the psychological stress of the respondents. Compared to the time before the Corona pandemic, feelings of social isolation, lack of company and being left out had become stronger among the employees with positive serology (57%). In particular, the feeling of lack of company had sometimes occurred in 71% of the IgG positive in the last 4 weeks (this could also hardly be due to the quarantine of the 5 known PCR smear positive among the 14 seropositive staff, as this period had been longer). This is also reflected in many other psychological studies. COVID-19 not only causes physical health problems but also leads to a range of psychological symptoms.30 In particular, low social resources, low economic resources, and higher exposure to stressors (eg, job loss) lead to a greater burden of depression symptoms.31
In our survey, only a minority of 28.6% of the employees with positive serology saw their job as at risk, and 7% saw both their job and their partner’s job as at risk. Studies show that job concerns increased during the pandemic, especially among people who have difficulty living on their income.32 Overall, 55% of the Germans worry about their job security, although individual areas vary greatly.33 Among the employees of our clinic, the concern seems to be comparably low, which could be due to the fact that they work in a system-relevant sector. However, it is also a challenge for health care workers to remain mentally healthy in times of the pandemic and to reduce the risk of developing depression, anxiety or burnout.34 At the end of the study, the participants were asked how they received the results of the blood test. Here it was found that in both the IgG-negative and IgG-positive groups, the results were only received with a positive feeling by less than half of the employees (47.2% vs 43.0%). It is notable that in the IgG-positive group, individuals were more likely to feel a sense of relief (50.0% vs 24.0%) but also anxiety (21.4% vs 1.1%) compared to the IgG-negative group. This shows how differently people react to the same disease, but also how attitudes towards COVID-19 have changed over the course of the pandemic. Whereas at the beginning of the pandemic many citizens and doctors still postulated that “everyone would go through the disease”, the mood changed towards the attitude of preferring to avoid the disease in order to avoid long-term consequences and acute complications, among other things. The employees’ feedback on how credible the blood results appeared to them is thought-provoking. Only 71.4% of the IgG-positive and 84.9% of the IgG-negative trusted the result of the blood test. This may be an expression of an increasingly critical approach to facts in our society, whereby a basic skepticism should always be appropriate even with scientific data.35 Pointing out the results from the last two table, our data suggest that the employees who tested positive for COVID-19 antibodies experienced more psychological and emotional impacts from the blood test result than those who tested negative. The positive cohort reported higher levels of anxiety, but also relief, possibly indicating a mixed reaction to the confirmation of their infection. They also expressed more changes in their attitude towards work, such as being more relaxed and less fearful. This could reflect a sense of gratitude for surviving the infection, as well as a heightened awareness of the risks and precautions involved in their work environment. This observation should be considered during decision-making, if testing should be regularly done, in other pandemic situations. It may increase the well-being and productivity of the health care workers.
Conclusion of the study showed deep insights into infection chains, disease courses, disease severity and symptoms among the COVID-19 positive staff. In detail, the different symptom patterns between COVID-19 and non-COVID-19 upper respiratory tract infections could be detected, and it showed the handling with and the psychological consequences of a sudden and unplanned new disease on health care workers in a dermatological setting. The shown data can help to better understand people`s behavior and might help to deal with in a better way in the case of future similar events.
Consent Statement
All participants provided informed consent.
Acknowledgments
The results of the study are partly the content of the dissertation work of the first author Lorenz Julius Kuhls.
Funding
The study was not funded.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Huang C, Wang Y, Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
2. Phan LT, Nguyen TV, Luong QC, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382(9):872–874. doi:10.1056/NEJMc2001272
3. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi:10.1056/NEJMc2001468
4. Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293:113382. doi:10.1016/j.psychres.2020.113382
5. Dragioti E, Tsartsalis D, Mentis M, Mantzoukas S, Gouva M. Impact of the COVID-19 pandemic on the mental health of hospital staff: an umbrella review of 44 meta-analyses. Int J Nurs Stud. 2022;131:104272. doi:10.1016/j.ijnurstu.2022.104272
6. Behrens GMN, Cossmann A, Stankov MV, et al. Perceived versus proven SARS-CoV-2-specific immune responses in health-care professionals. Infection. 2020;48(4):631–634. doi:10.1007/s15010-020-01461-0
7. Kern PM, Müller -H-H, Menzel T, Weisser H. Study on immunity against SARS-CoV-2 No significant humoral immunity against SARS-CoV-2 in the medical staff of a maximum care hospital and in the urban region of Fulda. Der Klinikarzt. 2020;49(06):268–273. doi:10.1055/a-1198-1243
8. Fukuda H, Seyama K, Ito K, et al. SARS-CoV-2 seroprevalence in healthcare workers at a frontline hospital in Tokyo. Sci Rep. 2021;11(1):8380. doi:10.1038/s41598-021-87688-9
9. Jagodzinski A, Johansen C, Koch-Gromus U, et al. Rationale and design of the Hamburg city health study. Eur J Epidemiol. 2020;35(2):169–181. doi:10.1007/s10654-019-00577-4
10. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi:10.1016/S2468-2667(20)30164-X
11. Homepage Spanish National Institute of Health Carlos III; ISCIII. 2023 [cited January 15, 2023]. Available from: https://www.isciii.es/Paginas/Inicio.aspx.
12. Homepage of the National Italian Society of Human and Dental Medicine. [cited January 15, 2023]. Available from: https://portale.fnomceo.it/.
13. German S1 AWMF Guideline SARS-CoV-2 infection in healthcare workers - importance of RT-PCR testing. [cited January 15, 2023]. Available from: https://register.awmf.org/de/leitlinien/detail/040-015.
14. World Health Organisation. Working paper 1, September 2021: The impact of COVID-19 on health and care workers: a closer look at deaths. [cited February 22, 2022]. Available from: https://apps.who.int/iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf.
15. Li Y, Liang M, Gao L, et al. Face masks to prevent transmission of COVID-19: a systematic review and meta-analysis. Am J Infect Control. 2021;49(7):900–906. doi:10.1016/j.ajic.2020.12.007
16. Robert Koch Institute (RKI). Epidemiological Bulletin 38/2020 (17/09/2020) Infection setting of COVID-19 outbreaks in Germany. [cited February 20, 2022]. Available from: https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2020/Ausgaben/38_20.pdf?__blob=publicationFile.
17. HDI Occupations Study 2020 (02/09/2020) Corona is radically changing the world of work. [cited January 15,2023]. Available from: https://www.berufe-studie.de/corona-veraendert-arbeitswelt.html.
18. Yan CH, Faraji F, Prajapati DP, Ostrander BT, DeConde AS. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int Forum Allergy Rhinol. 2020;10(7):821–831. doi:10.1002/alr.22592
19. Tong JY, Wong A, Zhu D, Fastenberg JH, Tham T. The prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020;163(1):3–11. doi:10.1177/0194599820926473
20. Robert Koch Institute (RKI) Epidemiological profile of SARS-CoV-2 and COVID-19. [cited July 24, 2021]. Available from: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Steckbrief.html.
21. Ludwig M, Jacob J, Basedow F, Andersohn F, Walker J. Clinical outcomes and characteristics of patients hospitalized for Influenza or COVID-19 in Germany. Int J Infect Dis. 2021;103:316–322. doi:10.1016/j.ijid.2020.11.204
22. Dietrich L, Abreu De Azevedo M, Wirz S, et al. Infections in practice-part 1 “Clinical and diagnostic” COVID-19, influenza and influenza-like illness. Prim Hosp Care (De) Inn Med. 2020;20(12):377–382.
23. Maronese CA, Zelin E, Avallone G, et al. Cutaneous vasculitis and vasculopathy in the era of COVID-19 pandemic. Front Med. 2022;9:996288. doi:10.3389/fmed.2022.996288
24. Gianotti R, Recalcati S, Fantini F, et al. Histopathological study of a broad spectrum of skin dermatoses in patients affected or highly suspected of infection by COVID-19 in the Northern Part of Italy: analysis of the Many Faces of the Viral-Induced Skin Diseases in Previous and New Reported Cases. Am J Dermatopathol. 2020;42(8):564–570. doi:10.1097/DAD.0000000000001707
25. Genovese G, Moltrasio C, Berti E, Marzano AV. Skin Manifestations Associated with COVID-19: Current Knowledge and Future Perspectives. Dermatology. 2021;237:1–12.
26. Overview | COVID-19 rapid guideline: managing the long-term effects of COVID-19 | guidance | NICE; 2023 [cited January 15, 2023]. Available from: https://www.nice.org.uk/guidance/ng188.
27. Pierce JD, Shen Q, Cintron SA, Hiebert JB. Post-COVID-19 syndrome. Nurs Res. 2022;71(2):164–174. doi:10.1097/NNR.0000000000000565
28. Kokolevich ZM, Crowe M, Mendez D, Biros E, Reznik JE. Most common long COVID physical symptoms in working age adults who experienced mild COVID-19 infection: a scoping review. Healthcare. 2022:10:2577.
29. Forsa Institute survey commissioned by the health insurance company DAK-Gesundheit (13.11.2020): Every third German is afraid of COVID-19. [cited January 15, 2023]. Available from: https://www.dak.de/dak/bundesthemen/jeder-dritte-deutsche-hat-angst-vor-covid-19-2380380.html#/.
30. Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57. doi:10.1186/s12992-020-00589-w
31. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 Pandemic. JAMA network open. 2020;3:e2019686.
32. Social Science Research Center Berlin (WZB), Results of the online survey corona-alltag.de (15.04.2020): Erwerbsarbeit in Zeiten von Corona. [cited January 15, 2023]. Available from: https://wzb.eu/de/pressemitteilung/erwerbsarbeit-in-zeiten-von-corona.
33. Randstad Labor Barometer (Covid-19 Edition/June 2020) by Randstad Deutschland GmbH & Co. KG. Great concern about job loss due to Corona 55% of Germans fear job insecurity due to the Corona pandemic. [cited January 15, 2023]. Available from: https://www.presseportal.de/pm/13588/4651564.
34. Vinkers CH, van Amelsvoort T, Bisson JI, et al. Stress resilience during the coronavirus pandemic. Eur Neuropsychopharmacol. 2020;35:12–16. doi:10.1016/j.euroneuro.2020.05.003
35. Süddeutsche Zeitung. Those who have an opinion ignore the facts; September 09, 2013 [cited January 15, 2023]. Available from: https://www.sueddeutsche.de/wissen/psychologie-des-starrkopfs-was-kuemmern-uns-die-fakten-wenn-wir-eine-meinung-haben-1.1765779.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
