Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
“Breathing New Life Into Chronic Obstructive Pulmonary Disease (COPD)” – Results From An Online Survey Of UK Patients
Authors Titmarsh S, Poliziani M, Russell RE
Received 6 July 2019
Accepted for publication 8 November 2019
Published 4 December 2019 Volume 2019:14 Pages 2799—2807
DOI https://doi.org/10.2147/COPD.S222139
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chunxue Bai
Steve Titmarsh,1 Michele Poliziani,2 Richard E Russell3
1M&F Health, London EC1N 8TE, UK; 2Opinion Health, London W1F 8QA, UK; 3Nuffield Department of Medicine, University of Oxford, Oxford OX3 7FZ, UK
Correspondence: Steve Titmarsh
M&F Health, 35–37 Kirby Street, London EC1N 8TE, UK
Tel +44 207 492 1793
Email [email protected]
Background: There is a lack of data on the impact of COPD on individuals, their illness, behavior and attitude to the disease.
Method: 500 UK patients with a primary care diagnosis of COPD responded to an online survey.
Results: 61.2% of respondents were female and 85.8% were between 50 and 80 years old. Two-thirds (67.8%) of respondents did not smoke at the time of the survey. Almost half of those surveyed (46.2%, n=231) used three inhalers, and 31% (n=155) agreed or strongly agreed with the statement “I feel that my treatment is not adequately controlling my condition”, while 39.4% (n=197) disagreed or strongly disagreed. 48.8% (n=244) agreed their COPD was well managed. Over half the sample (56.8%, n=284) said they never forgot to use their inhaler as prescribed. Checks on inhaler use by doctors or nurses were reported as every six months/twice a year by 24.4% (n=122) and once a year by 38.8% (n=194). However, 17.2% (n=86) said their technique had never been checked, and at their last annual review, a third (33.2%, n=166) did not receive inhaler technique advice. Exacerbations were reported to affect an average of 7.4 days a year. They led to time in hospital, time off work and significantly affected quality of life. Patients reported that their COPD affected all aspects of their daily lives to a greater or lesser extent, with some living in fear of what the impact of the next flare-up could bring.
Conclusion: COPD impairs people’s ability to carry out daily tasks, leads to hospital admission, time off work and even unemployment. Respondents reported stress, worry and depression or low mood because of their COPD. This study highlights areas of concern for patients not being addressed by health care practitioners, including: pulmonary rehabilitation referral, better information giving and medicines optimization.
Keywords: COPD, inhalers, exacerbations, quality of life, optimize
Introduction
It is estimated that approximately three million people in the UK have chronic obstructive pulmonary disease (COPD).1 Of those, around 1.2 million have been given a diagnosis,2 while almost two million others may not know they have the condition.1 COPD mostly affects people over the age of 35 years who are smokers or who have smoked.3 Other causes include breathing dust, fumes and chemicals; there are thought to be genetic predeterminants as well.4
COPD is estimated to kill almost 30,000 people annually in the UK.5 The condition costs the NHS £800 million each year and employers are thought to bear an annual £3.8 billion cost in lost productivity due to COPD.6
Patient involvement in treatment decisions is important. The National Institute for Health and Care Excellence (NICE) notes: people have the right to be involved in discussions and make informed decisions about their care.7
Patients’ views about their treatment and its impact on their COPD may provide insights into areas of management that could be improved. That in turn may help improve outcomes for patients. The results of the survey described in this paper aimed to provide some of those insights.
Method
A survey of 500 people diagnosed with COPD, based upon the presence of a primary care COPD diagnosis read code, was carried out via an online questionnaire to assess the impact of COPD on patients’ lives. (The sample was regionally representative but did not control for age/gender/ethnicity.) Questions were in the form of multiple choice and free text answers and were developed by M&F Health, Opinion Health and reviewed by Chiesi and the British Lung Foundation.
The questionnaire was sent to patients across the UK, by Opinion Health, via a website link within an email. Patients who were sent the link to the survey had previously agreed to be contacted about online surveys and consented to the survey when they took part. Participants were asked about their disease, including the diagnosis they received, its treatment and the impact it had on their daily lives, including employment and social lives as well as their quality of life. They were also asked about their understanding of COPD and the level of support and information available. Responses were collected and collated by Opinion Health.
The survey was conducted from late July until mid-August 2017. As the survey was viewed as patient market research, it did not require ethics committee approval.
Results
All results are patient-reported: they do not come from the primary care database or patient records. In all, 1648 email invitations to take part in the survey were sent out; of 1143 responses, there were 500 completed surveys.
Of the 500 patients surveyed, 332 (136 male, 196 female) reported being diagnosed with COPD alone (see Figure 1). Other patient-reported respiratory diagnoses included: chronic bronchitis (n=19), emphysema (n=59), asthma (n=42) and bronchiectasis (n=12).
 |
Figure 1 Patient-reported diagnosis. |
Respondents ranged in age from less than 35 years old to more than 81 years old: 61.2% (n=306) were female and 38.8% (n=194) male. They identified as predominantly white (98.6%, n=493) (see Table 1). Of the six subjects aged <35 years, 1 had COPD, 3 had chronic bronchitis and 2 had asthma.
 |
Table 1 Patient Characteristics |
Date Of Diagnosis
42% (42.3% male, 41.5% female) of subjects were diagnosed between 1 and 5 years before the survey took place, 27.6% (28.4% male, 27.1% female) between 6 and 10 years and 22.2% (23.7%, 21.2%) over 10 years before taking part in the survey (see Figure 2). There were no differences in the time of diagnosis between males and females. Current smokers tended to have been diagnosed more recently as smokers tend to quit over time; thus, levels of non- (ex) smokers were higher in those diagnosed earlier.
 |
Figure 2 Time since COPD diagnosis. |
Smoking History
At the time of the survey, just over two-thirds (67.8%; 72.2% male, 65% female) of the respondents were ex-smokers, while almost a third (32.2%, n=161; 27.8% male, 35% female) reported they were current smokers at the time of the survey despite being diagnosed with COPD. Of the 339 not smoking at the time of the survey, 299 (88.2%; 126 male, 173 female) reported that they had smoked at some stage, and almost half (47.5%; 52.4% male, 43.9% female) had quit smoking 7 years or more before the study.
At diagnosis, 387 (145 male, 242 female) participants said they were given help with or advice about stopping smoking. At their last annual review, 265 (91 male, 174 female) reported receiving advice or help relating to stopping smoking.
Management
Number Of Inhalers
All those responding to the survey had been prescribed an inhaler: almost half (n=231, 46.2%; 41.8% male, 49% female) used three inhalers, 37.6% (38.7% male, 36.9% female) used two and 15% (18.0% male, 13.1% female) used one. Two patients were using five inhalers. The number of inhalers used was not associated with whether people were smoking or the length of time since diagnosis.
Exacerbations/Flare-Ups
The 500 respondents reported a total of 3705 days affected by flare-ups. That is on average 7.4 each year. Males had 5.79 and females 8.44 events on average.
For those who had been in hospital due to COPD exacerbations, the average length of stay was 2 (sd 1.9) days, with men staying longer than women (2.2 (sd 1.8) days versus 1.76 (1.3) days). Many respondents had been seen in hospital and discharged on the same day (n=319; 122 male, 197 female).
When describing how a flare-up makes them feel: 23.4% (22.2% male, 24.2% female) of respondents felt nervous, 51% (50% male, 51.6% female) felt anxious, 41% were scared (36.1% male, 44.4% female) and stressed (43.3% male; 39.9% female) with 30.6% (33.0% male, 29.1% female) saying they felt annoyed or irritable about flare-ups.
When responding about how they would feel about a future flare-up: 56.8% were nervous (25.8% male, 21.6% female) or anxious (30.4% male, 35.6% female), 47.8% (45.4% male, 49.3% female) were worried about being able to breathe and 22.8% (21.1% male, 23.9% female) were feeling depressed about future flare-ups. 33.8% (35.6% male, 32.7% female) were not worried about a flare-up until it happens. Anxiety and nervousness were higher in the smokers compared with non-smokers (67.7% vs 51.6%): there was a statistically significant (p<0.05) group-wise difference between the nervousness of smokers (31.7%) versus non-smokers (19.2%).
Fear of flare-ups was shown to have an impact on patient quality of life (see Figure 3). 17.6% (16% male, 18.6% female) reported that this fear affected getting up in the morning a lot, almost totally or totally; 22.4% (20.1% male, 23.9% female) said it affected getting dressed a lot, almost totally or totally; 40.8% (43.5% male, 44.4% female) felt that the fear of having a flare-up affected their ability to do their shopping; 26.4% (22.1 male, 29% female) felt their ability to cook was compromised by a fear of flare-ups; 48.6% (45.9% male, 50.4% female) reported that even walking up and down stairs was impacted a lot, almost totally or totally, and 25.6% (22.2% male, 27.7% female) said a flare-up impacted walking about in the house a lot, almost totally or totally. This fear also affected social activities (41.2%; 40.2% male, 41.8% female) and gardening (45.6%; 46.9% male, 44.8% female) as well as sleeping (27.8%; 22.7% male, 31.1% female) and in their personal relationships (30.2%; 31.5% male, 29.4% female). Sexual intimacy was impacted upon by the fear of flare-ups in 38.6% (43.3% male, 35.6% female) and housework in 38.6% (32.5% male, 42.5% female).
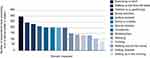 |
Figure 3 Impact of the fear of flare-ups. |
Patients’ Views Of Efficacy Of Treatment/Rehabilitation
Opinion appeared to be divided as to the efficacy of respondents’ treatment: 31% (n=155; 58 male, 97 female) agreed or strongly agreed and 39.4% (n=197; 78 male, 119 female) disagreed or strongly disagreed with the statement “I feel that my treatment is not adequately controlling my condition.” Although 48.8% (n=244; 100 male, 144 female) of respondents agreed or strongly agreed that their COPD was well managed and felt they could get on with their life, 22.2% (n=111; 32 male, 79 female) disagreed or strongly disagreed with this statement.
In terms of specific symptoms, 75.2% (73.7% male, 76.2% female) felt their inhaler treatment controlled their breathlessness very well or quite well, 60.8% (61.3% male, 60.5% female) felt it controlled their wheezing very well or quite well and 70.6% (72.6% male, 69.3% female) felt their inhaler treatment had prevented flare-ups quite well or very well in the last year and only 3.4% (3.1% male, 3.6% female) felt that they did not do this at all. 59.2% (n=119; 49% male, 50% female) of respondents who had done pulmonary rehabilitation felt that this was effective in preventing flare-ups.
Adherence
Checks on inhaler technique by doctors or nurses varied but the most commonly reported intervals were every six months/twice a year (24.4%, n=122; 56 male, 66 female) and once a year (38.8%, n=194; 68 male, 126 female) (see Figure 4). However, 86 (17.2%; 29 male, 57 female) respondents said their technique had never been checked, and at their last annual review, a third (33.2%, n=166; 55 male, 111 female) said their nurse or doctor did not provide advice on inhaler technique.
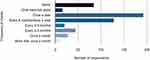 |
Figure 4 Frequency of inhaler technique check. |
Encouragingly, over half of the sample (56.8%, n=284; 110 male, 174 female) said they never forgot to use their inhaler as prescribed, with 56.9% of those using two inhalers and 63.6% of those using three inhalers reporting that they never forgot to use them as prescribed – a statistically significant difference (p<0.05).
Days In Hospital
The majority of respondents did not need access to accident and emergency services following a flare-up (75%, n=377; 143 male, 234 female). If hospitalization was necessary following a flare-up, 69% required a stay of less than 1 week (range: 1–6 days, n=125; 49 male, 76 female). In the last 12 months, 28.6% (n=143; 57 male, 86 female) of patients said they had seen a hospital doctor as an outpatient because of their COPD. Of those, 68.5% (n=98; 38 male, 60 female) had attended once or twice, and 26.6% (n=38; 14 male, 24 female) had outpatient appointments with a doctor three to four times, while seven patients had been five or more times.
Pulmonary Rehabilitation
When asked “Have you ever been referred by your doctor, nurse or respiratory team for pulmonary rehabilitation/special exercise classes to help your lungs?” 56% (n=280; 105 male, 175 female) of respondents said “no”. Of those who were referred, around one in five (n=49/220; 14/89 male; 35/131 female) did not attend or attended only one session; 65.9% (n=145; 63 male, 82 female) completed the full course.
Impact Of COPD On Quality Of Life
Respondents said they had experienced stress or worry (39.4%, n=197; 57 male, 140 female), depression or low mood (39%, n=195; 66 male, 129 female), panic (21%, n=105; 28 male, 77 female), fear of breathlessness or flare-ups (29.4%, n=147; 49 male, 98 female), fear of dying (17.2%, n=86; 27 male, 59 female), loss of control or independence (20.6%, n=103; 28 male, 75 female), low self-esteem or loss of dignity (25.2%, n=126; 33 male, 93 female), anger or frustration (30.4%, n=152; 57 male, 95 female) or hopelessness (26.4%, n=132; 41 male, 91 female) twice a week in the previous month. These feelings were more common among smokers than non-smokers.
Almost half of the patients felt their COPD had a “quite big” (24%, n=120; 50 male, 70 female) or moderate (25.6%, n=128; 50 male, 78 female) impact on their family or loved ones. While 13.6% (n=68; 31 male, 37 female) judged the impact to be “huge”.
Patients reported that their COPD affected all aspects of their daily lives to a greater or lesser extent (see Figure 5), from walking up and down the stairs to shopping to social activities to housework to hobbies such as gardening and sexual intimacy.
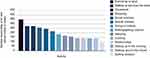 |
Figure 5 Impact of COPD on daily life. |
Impact Of COPD On Employment
Of the 380 people in the sample not employed at the time of responding, 27.1% reported that their unemployment was because of their COPD.
Of the 120 people employed at the time of the questionnaire, just over a third (36.7%, n=44; 18 male, 26 female) had not had time off work due to their COPD in the past year. In the previous year, 73 (60.8%; 28 male, 45 female) people had taken two or more days off work because of their COPD. Among the 120 in work at the time of the survey, 17 (14.2%; 8 male, 9 female) said they had to change jobs, 22 (18.3%; 9 male, 13 female) had to change their hours and seven had to take a pay cut as a result of their condition.
Understanding, Information And Support
Most patients had not heard of COPD (37.4%, n=187; 84 male, 103 female) or had heard of it but did not know much about it (38.6%, n=193; 72 male, 121 female) before they were diagnosed. The majority (69.4%, n=347; 147 male, 200 female) felt they received enough information when COPD was first explained to them and a similar number (69.6%, n=348; 124 male, 224 female) searched for additional information, usually via the internet (91.4%, n=318; 112 male, 206 female) or reading material/leaflets from the local surgery (24.7%, n=86; 37 male, 49 female). On a scale of 1 to 5, where 1 is not at all and 5 is completely, 163 (32.6%; 59 male, 104 female) respondents said they completely understood the condition, while only 11 (2.2%; 3 male, 8 female) said they did not understand it at all.
Almost six of 10 (59.6%; 53.6% male, 63.4% female) of those surveyed agreed or strongly agreed that there was not enough support available to help people with COPD better manage their condition, with 57.8% (53.1% male, 60.8% female) agreeing or strongly agreeing that there was not enough support available for those caring for people with COPD (75% [69.6% male, 78.8% female] of participants were not given advice about how to tell relatives about COPD). A similar proportion (62%; 58.8% male, 64% female) agreed or strongly agreed that there was not enough information available about the condition for people with COPD.
At their last annual review, more people reported not receiving information than those who reported receiving information on: controlling breathing; healthy weight and diet; exercise or pulmonary rehabilitation; managing flare-ups; taking care of their feelings/emotional well-being and telling loved ones about their diagnosis.
Discussion
From the responses to the survey it would appear that COPD is often a delayed diagnosis, as many patients reported a relatively recent diagnosis. This is significant as the impact of the disease is often debilitating8,9
Patient engagement with their treatment is an important aspect of clinical care in COPD.7 Adherence to medication is influenced by the quality of communication between patients and health care providers; better overall communication is associated with improved adherence. Poor adherence has a direct impact on morbidity, hospital visits and quality of life.10
Medication adherence levels among COPD patients are reportedly generally poor, at around 50%.10 In this survey, self-reported adherence was in line with, if not better than that (depending on the definition of adherence used). This is reassuring however the tool used has the potential for selection bias, in that those who respond to the questionnaire are potentially more likely to either adhere with the medication or report that they do.
Patients’ perceptions of the efficacy of their treatment seemed to be mixed, with almost a third agreeing or strongly agreeing that their treatment was not adequately controlling their condition. Almost half of the respondents agreed or strongly agreed that their COPD was well managed and felt they could get on with their life. There is clearly a burden of disease that is not fully addressed by the respondents’ current therapy. They are often managing to continue with a relatively normal life.
Pulmonary rehabilitation is one of the most effective therapies for COPD. It improves exercise tolerance, quality of life and reduces exacerbation rates. It has been shown to be cost-effective with every patient completing rehabilitation saving money over the next year in a reduction in direct health care costs.11 Moreover, the latest national pulmonary rehabilitation audit showed that if a course is completed, then over half of the patients achieve the minimally clinical important difference in outcome for exercise tests in endurance, symptoms and quality of life.12 In short, pulmonary rehabilitation works. In our survey, more than half of patients said they had never been referred for rehabilitation and of those who were, around 20% did not attend the sessions. Yet NICE states that pulmonary rehabilitation should be "available to all appropriate people with COPD, including people who have had a recent hospitalisation for an acute exacerbation."8 states that: “Pulmonary rehabilitation should be made available to all appropriate people with COPD, including those who have had a recent hospitalization for an acute exacerbation.” There is clearly a need to improve the selection of candidates for pulmonary rehabilitation and offer this remarkable intervention to all eligible subjects.13,14
In terms of follow-up, 86 (17.2%) respondents said their inhaler technique had never been checked, and at their last annual review, a third (33.3%, n=166) said their nurse or doctor did not provide advice on inhaler technique. Inhaler checks are critical to achieving a reasonable rate of adherence, and studies have demonstrated that checking technique and training does improve inhaler technique in the long term and improve clinical outcomes.15,16
The impact of COPD in terms of clinic visits, effect on daily activities and quality of life is evident in the responses to the survey. The impact on work was clear with 380 people in the sample not employed at the time of responding, 27.1% of whom reporting that their unemployment was as a result of their COPD. In the previous year, 60.8% of people had taken two or more days off work because of their COPD. The potential impact to society of COPD is enormous and under-recognized with the indirect costs of COPD often overwhelming the more obvious direct health care costs.
Flare-ups are common and have a serious impact on life.17–20 Our data demonstrated that many respondents felt that their treatment was effective in preventing flare-ups with similar findings for pulmonary rehabilitation. Fear of flare-ups had a major negative impact on patients’ lives. These data are further strengthened by the finding that levels of stress/anxiety and worry are high among COPD subjects and they are worried about the disease and its flare-ups. The significant finding of hopelessness is common, and subjects are afraid of flare-ups and hospitalization.21–24 This is an area which is rarely addressed by health care practitioners. We do not explore patients' fears and rarely address this on their terms. We believe that these data should give practitioners a mandate and the confidence to ask a patient about their fears, and this may be especially relevant after an exacerbation has occurred. There is a need to respond through information giving and where necessary arranging for psychological intervention in those with potential anxiety disorders.
Awareness of COPD among patients before they were diagnosed was poor in general and patients looked at a variety of sources for information. There is an opportunity to improve and standardize information provided as many patients use GP surgeries as their source. Given this, ensuring that the best possible information is available would be a reasonable intervention to consider nationally. The level of emotional/well-being support that respondents reported receiving was inadequate (30%) and there needs to be more guidance for patients on speaking to others about their disease.
The survey highlights some of the challenges facing healthcare professionals who manage COPD and the people who live with it. The results should be considered in light of some of the limitations of the work. For example, self-reported measures are inherently imperfect and tend to overestimate adherence when compared with other methods.25 The sample surveyed was representative of the COPD UK population with a sampling error ± 4.4%. However, the sample was not controlled for gender, ethnicity, region (or any other covariate that is likely to impact on skewing the data). The research approach was not designed to be representative of these subgroups. Data for disease severity were not collected. Neither did the survey reflect the ratio of gender of people with COPD in the UK: the effect of this in terms of non-responder bias is unknown. The survey was conducted online only, so people with COPD who were unable to access it could not take part. That said, we believe that the data are significant and identify areas that health care practitioners could prioritize to improve care for all those with COPD.
Conclusion
From the survey responses, it is evident that COPD impacts many aspects of the lives of those who have the condition. The disease impairs people’s ability to carry out daily tasks, leads to hospital admission, time off work and even unemployment. Respondents also reported experiencing stress or worry, and depression or low mood because of their COPD.
It is not possible to judge the appropriateness of management approaches without greater insight into patients’ clinical conditions, but the responses to this survey seem to indicate that there may be scope for improvements in areas such as referral for pulmonary rehabilitation, more robust patient follow-up, addressing patients fears, patient support and information and medicines optimization.
Disclosure
Mr Steve Titmarsh and Mr Richard E Russell report personal fees from Chiesi Limited to draft this article. Mr Michele Poliziani inputted into the article and reviewed its content as part of his work on the patient survey. Editorial assistance was provided by M&F Health, London on behalf of Chiesi Limited. The authors report no other conflicts of interest in this work.
References
1. National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in adults. (QS10). July 2011. Available from: www.nice.org.uk/guidance/qs10/chapter/Introduction. Accessed November, 2019
2. British Lung Foundation. Chronic obstructive pulmonary disease (COPD) statistics. Available from: https://statistics.blf.org.uk/copd?_ga=2.268039752.797162991.1506599531-826828642.1506599531.
3. British Lung Foundation. What is COPD? Available from: www.blf.org.uk/support-for-you/copd/causes.
4. Holm KE, Plaufcan MR, Ford DW, et al. The Impact of Age on Outcomes in Chronic Obstructive Pulmonary Disease Differs by Relationship Status. J Behav Med. 2014;37(4):654–663. doi:10.1007/s10865-013-9516-7
5. Snell N, Strachan D, Hubbard R, et al. S32 Epidemiology of chronic obstructive pulmonary disease (COPD) in the UK: findings from the British lung foundation’s ‘respiratory health of the nation’ project. Thorax 2016;71:A20. doi:10.1136/thoraxjnl-2016-209333.38
6. COPD Commissioning Toolkit: a resource for commissioners. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/212876/chronic-obstructive-pulmonary-disease-COPD-commissioning-toolkit.pdf. http://www.respiratoryfutures.org.uk/media/1139/copd-commissioning-toolkit.pdf.
7. National Institute for Health and Care Excellence (NICE). Chronic obstructive pulmonary disease in over 16s: diagnosis and management (NG115). December 2018. Available at: www.nice.org.uk/guidance/ng115. Accessed November, 2019
8. Jones RCM, Price D, Ryan D, et al. Opportunities to diagnose chronic obstructive pulmonary disease in routine care in the UK: a retrospective study of a clinical cohort. Lancet Respir Med. 2014;2(4):267–276. doi:10.1016/S2213-2600(14)70008-6
9. Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulmon Dis. 2014;9:889–904. doi:10.2147/COPD.S62750
10. Borbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63(9):831–838. doi:10.1136/thx.2007.086041
11. Griffiths TL, Phillips CJ, Davies S, et al. Cost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programme. Thorax 2001;56:779–784. doi:10.1136/thorax.56.10.779
12. Steiner M, Holzhauer-Barrie J, Lowe D, et al. Clinical outcomes of pulmonary rehabilitation. Results for the UK national COPD audit. Am J Respir Crit Care Med. 2016;193:A4515.
13. Russell RE. Chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2014;20(2):127–131. doi:10.1097/MCP.0000000000000030
14. Goldstein RS. Rehabilitation in end-stage COPD. Monaldi Arch Chest Dis. 1995;50(1):41–46.
15. Pinnock H, Fletcher M, Holmes S, et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J. 2010;19:1. doi:10.4104/pcrj.2010.00021
16. Lavorini F, Usmani OS. Correct inhalation technique is critical in achieving good asthma control. Prim Care Respir J. 2013;22(4):385–386. doi:10.4104/pcrj.2013.00097
17. Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764. doi:10.2147/COPD.S36997.
18. Pavord ID, Jones PW, Burgel P-R, Rabe KF. Exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. 2016;11(Spec Is):21–30. doi:10.2147/COPD.S85978.
19. Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. doi:10.1056/NEJMoa0909883.
20. Wedzicha JA, Donaldson GC. Exacerbations of chronic obstructive pulmonary disease. Respir Care. 2003;48(12):1204–1213. discussion 1213–1215.
21. Kaplan A, Small I. Our patients’ fears may be getting the better of them: how do we deal with it? Prim Care Respir J. 2011;20(3):233–234. doi:10.4104/pcrj.2011.00068
22. Barnes N, Calverley PMA, Kaplan A, Rabe KF. Chronic obstructive pulmonary disease and exacerbations: patient insights from the global hidden depths of COPD survey. BMC Pulm Med. 2013;13:54. doi:10.1186/1471-2466-13-54
23. Kessler R, Stahl E, Vogelmeier C, et al. Patient understanding, detection, and experience of COPD exacerbations: an observational, interview-based study. Chest. 2006;130(1):133–142. doi:10.1378/chest.130.1.133
24. Halpin D, Hyland M, Blake S, et al. Understanding fear and anxiety in patients at the time of an exacerbation of chronic obstructive pulmonary disease: a qualitative study. JRSM Open. 2015;6(12):2054270415614543. doi:10.1177/2054270415614543
25. Stirratt MJ, Dunbar-Jacob J, Crane HM,
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
