Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Knowledge of Vaccination Against Influenza and Pneumococcus in Patients with Chronic Obstructive Pulmonary Disease in an Integrated Care Program
Authors Proaños NJ , González-García M , Crispín-Cruz D , Ali-Munive A, Villar JC, Torres-Duque CA , Casas A
Received 30 May 2023
Accepted for publication 29 September 2023
Published 13 October 2023 Volume 2023:18 Pages 2257—2265
DOI https://doi.org/10.2147/COPD.S421085
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Nadia Juliana Proaños,1,2 Mauricio González-García,1,2 Dayan Crispín-Cruz,1 Abraham Ali-Munive,1,2 Juan Carlos Villar,3 Carlos A Torres-Duque,1,2 Alejandro Casas1,2
1Programa AIREPOC y CINEUMO, Fundación Neumológica Colombiana, Bogotá, Colombia; 2Facultad de Medicina, Universidad de La Sabana, Chía, Colombia; 3Centro de Investigaciones, Fundación Cardioinfantil - Instituto de Cardiología, Bogotá, Colombia
Correspondence: Carlos A Torres-Duque, Email [email protected]
Purpose: To compare the level of knowledge in vaccination against influenza and pneumococcus of patients with chronic obstructive pulmonary disease (COPD) who are managed in an Integrated Care Program (ICP) with those who receive usual care (UC).
Methods: A telephone survey of patients diagnosed with COPD registered in public care networks or private institutions was done. A descriptive and comparative analysis of the characteristics of the ICP and UC groups was carried out. The relationship between belonging to an ICP and the level of knowledge about vaccination was evaluated using Propensity Score Matching (PSM) and multivariate logistic and ordinal regression models.
Results: Of 674 study participants, 27.2% were from the ICP group. ICP patients were older, more frequently men, from a higher socioeconomic stratum and a higher educational level (p< 0.05). 75.5% of the patients in the ICP group had a high level of vaccination knowledge compared to 42.7% in the UC group (p< 0.001). In the multivariate analysis, adjusting for sociodemographic variables, years of COPD diagnosis, and comorbidities, belonging to the ICP was associated with a higher probability of answering questions about vaccination correctly and having a high level of knowledge (OR 3.397, IC 95% 2.058– 5.608, p< 0.001).
Conclusion: Patients with COPD managed in an ICP have a higher level of knowledge in vaccination against influenza and pneumococcus, compared to patients in usual care.
Keywords: chronic obstructive pulmonary disease, knowledge, patient education, care patient
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading cause of mortality worldwide, 1 and in Colombia, 38 people die daily as a result of this disease, which is the fourth leading cause of death in the country.2 The estimated national prevalence is 8.9%, and in Bogotá DC, the capital city, it is 8.5%.3 COPD treatment focuses on reducing exacerbations, improving airflow obstruction, and restoring patients’ functional capacity.4 Pharmacological treatment includes the use of bronchodilators and sometimes inhaled corticosteroids,4 while non-pharmacological management centers on strategies such as smoking cessation, pulmonary rehabilitation, long-term oxygen use, nutritional counseling, and vaccination.4 All treatments should involve patient education as a cornerstone of comprehensive and integrated disease management for COPD.5
Education targeting patients with COPD aims to provide information and recommendations, mainly by healthcare professionals, focused on helping the patient understand the disease and promoting self-care and early recognition of exacerbation, under the assumption that education will lead to a change in the patient’s behavior, better treatment results, and an improved functional condition in the long term.4,6 These recommendations have resulted in potential mortality reduction, early initiation of treatment in subjects with exacerbations, which prevents severe complications,7 and decreased hospitalization rates.6,8 Other studies have presented conflicting results regarding the effectiveness of education for patients with COPD.9,10
A systematic review identified the main topics addressed in COPD education programs, ranging from the pathophysiology of the disease to the correct use of inhaled therapy, but found little information on vaccination education.11 Although structured comprehensive and integrated care programs exist for COPD, education for patients with COPD is scarce. A study in Spain found that only 17% of the participants had some knowledge about COPD, and as each decade of their lives progressed, their knowledge of their disease declined.12
Vaccination against the influenza virus significantly reduces the number of exacerbations [RR 0.24; IC95% (0.09–0.67)],13 hospitalizations, and deaths in COPD patients.14–16 Vaccination against Streptococcus pneumoniae decreases the incidence of community-acquired pneumonia [RR 0.24; IC95% (0.07–0.80)], bacteremia, and severe invasive diseases caused by this bacteria.15,17 These observations have been instrumental in the inclusion of recommendations that COPD patients be vaccinated in COPD clinical practice guidelines; however, vaccination rates remain low. One study noted that 41.1% of patients who agreed to be vaccinated did so on the recommendation of a doctor, while among those who refused the vaccine, 71.5% considered possible side effects, and 33.9% believed that the vaccine was ineffective. This partly explains the low vaccination coverage in older adults with chronic diseases who are at a higher risk of severe respiratory infections.18 However, some studies have described effective strategies that can be used to increase vaccination rates, such as the recommendation of the doctor and the vaccination offered during hospitalization,19 training sessions for the medical practice team reminders via text message, that could help increase vaccination coverage.20 In Colombia, clinical practice guidelines recommend annual vaccination against influenza in patients with stable COPD, to reduce the frequency of respiratory infections, and the pneumococcal vaccine in all patients with stable COPD under 65 years old, patients with FEV1 <40%, and in all patients over 65 years regardless of lung function, to reduce the frequency of community-acquired pneumonia.13,21,22 The type of vaccines (PCV13 and PPS23) and application Schedule are based on PAHO recommendations.23
In Colombia, COPD clinical practice guidelines recommend educational interventions to reduce the risk of hospital admissions,6 but currently, there is a low availability of COPD integrated care programs (ICP). A small number of healthcare institutions have ICP to attend chronic non-communicable diseases, ICP is offered to patients older than 40 years with a confirmed diagnosis of COPD by spirometry. Personalized and continuous care is provided by an interdisciplinary group of internists, pulmonologists, respiratory therapists, psychologists, and nutritionists to improve quality of life, prevent and avoid complications. Few studies have been conducted to assess the level of knowledge of patients and the impact of these programs on patients’ health outcomes. The objective of our study was to compare the level of knowledge of the importance of vaccination against influenza and pneumococcus among COPD patients who are cared for in an integrated care program (ICP) for patients with that of patients who receive the usual care (UC).
Materials and Methods
Study Design
This is a cross-sectional study that uses baseline information obtained from a subgroup of patients with COPD who participated in the “Impact of Information Strategies to Modify Knowledge, Attitudes, and Practices in Chronic Diseases in Bogotá—Vector Salud Bogotá” project, an experiment conducted by conglomerates. The main objective was to evaluate the impact of a series of evidence-based recommendations, using various information dissemination strategies, on the knowledge, attitudes, and practices related to seven non-communicable chronic diseases (NCDs), including COPD, among users of clinics and hospitals in the city of Bogotá.
Population and Sample
The participants in this study are adults diagnosed with COPD who are registered in the databases of public and private health service networks in Bogotá DC, Colombia. Consecutive sampling and phone calls were made to the registered population to secure informed consent. The study complies with the Declaration of Helsinki and was approved by the research committee and ethics committee for health research of the Secretaria Distrital de Salud Bogotá, Colombia. Register Number: 2016ER47349.
Procedures
After informed consent was obtained, a telephone questionnaire that included questions on sociodemographic information, clinical history, medical controls, and the frequency of exacerbations was administered to each participant. A second call included questions relating to the participants’ knowledge of their illness, vaccination, and medical follow-up. The telephone surveys were administered between August and October 2021, and the information was recorded on the Research Electronic Data Capture (REDCap) platform.24
The formulation of the questions in the measurement instrument was based on a review of the recommendations made in the Clinical Practice Guide issued by the Ministry of Health and Social Protection of Colombia. It was prepared by a group of experts, including internal medicine specialists and general practitioners. The questions related to vaccination were as follows: Question 1 (Q1): “Should people with COPD be vaccinated against pneumonia?” Question 2 (Q2): “Should people with COPD be vaccinated against flu (influenza virus) each year?” Question 3 (Q3): “Should all patients diagnosed with COPD be vaccinated against influenza (flu)?” Question 4 (Q4): “How often should a COPD patient get a flu shot (every year or another option)?” and Question 5 (Q5): “Does vaccination against influenza reduce exacerbations and hospitalizations in COPD patients?”
The study patients were grouped into those who were part of the COPD ICP and those who were receiving the usual care (UC). The patients in the ICP group were part of the Comprehensive Care, Rehabilitation, and Education Program for COPD Patients (AIREPOC) of the Fundación Neumológica Colombiana. This specialized outpatient institution provides an integrated (interdisciplinary) comprehensive care model (seeing the patient as a person and not just as a disease) and follows the precepts of the WHO chronic care model.25,26 The purpose is to offer continuous COPD patient-centered care that seeks to improve patients’ quality of life and reduce severe disease exacerbations through education, self-care, and pulmonary rehabilitation. The target population is patients over 40 years of age with COPD diagnosed by spirometry, and the educational program includes instructional sessions on COPD signs and symptoms, diagnosis, recommendations, drug treatment, inhalation technique, oxygen therapy, bronchial hygiene, pulmonary rehabilitation, vaccination, smoking cessation, and exacerbations. The ICP is developed in 5 face-to-face phases, from the correct classification of patients with COPD, evaluation by a medical doctor, individual and group education sessions, paraclinical control at least every 2 months, and priority attention for exacerbation. The patient ends their time in the ICP when they have achieved control and stability of COPD.
Statistical Analysis
The categorical variables were described in absolute and relative frequencies, continuous variables were described in mean and standard deviation or median and percentiles. For comparisons between the ICP and UC groups, the chi-square test or Fisher’s exact test was used for the qualitative variables, and the Student’s t-test or Mann–Whitney U-test was used for the continuous variables according to distribution.
To determine the relationship between the level of vaccination knowledge and being in an ICP, multivariate logistic regression models were performed for each of the five questions on vaccination knowledge, using the correct answer to each question as the dependent variable. The independent variables included in the model were age, sex, socioeconomic level, education level, years since COPD diagnosis, comorbidities, and participation in an ICP. Variables with a p value <0.25 in the bivariate analysis were included in the final model. The goodness of fit of the model was evaluated using a Hosmer–Lemeshow test. A propensity score matching (PSM) analysis was performed to balance the differences in baseline characteristics between the ICP and UC groups. The propensity score was used as a covariate in each logistic regression model. To determine the variables associated with a high level of vaccination knowledge, an ordinal regression model was performed, and the Akaike information criterion (AIC) was used to assess fit. The patients’ level of knowledge was classified into three categories according to the number of questions answered correctly, as follows: 1) low level: zero or one correct answer, 2) medium: two or three correct answers, and 3) high: four or five correct answers. The tests were two-tailed, setting a p value <0.05 as the level of statistical significance, and the analyses were performed using R studio27 and Stata 17 Corp.28
Results
A total of 674 patients were included in the study: 27.3% in the ICP group and 72.7% in the UC group, with a median age of 71.6 years in both groups. Patients in the ICP group were older (75.9 [69.7–81.7] vs 70.4 [64.1–77.0], p < 0.001). Of the patients, 52.9% were female, and there were more women in the UC group (27.2 vs 62.6, p <0.001). Of the participants in both groups, 72.2% had completed elementary school, and 67.3% were in socioeconomic level 1–2. The most frequent comorbidities were arterial hypertension (59.2%) and type 2 diabetes (23.0%), with a lower proportion of patients with coronary disease (8.6%) and dyslipidemia (6.8%) (Table 1).
 |
Table 1 Characteristics of the Participants |
The percentage of correct answers was higher than 50% in Q1, Q2, Q3, and Q4, while 47.3% was in Q5 in the total group. The proportion of correct answers was higher in the ICP group than in the UC for all questions (Figure 1). The analysis, in terms of the number of correct answers, showed that 51.6% of the total group had a high level of knowledge, and the proportion of patients with a high level of knowledge was greater in the ICP group than in the UC group (75.5% vs 42.7% [p<0.001]) (Figure 2).
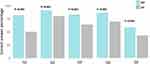 |
Figure 1 Bar graph of the percentage of correct answers questions 1 to 5 by ICP and UC. |
 |
Figure 2 Stacked bar chart of the level of vaccination knowledge in the ICP and UC groups. |
In all the multivariate models, the fact of belonging to the ICP group was associated with a higher probability of correctly answering the questions about vaccination (Table 2) (Figure 3). The PSM obtained similar results in the logistic regression models. For Q1, Q2, Q3, and Q4, being in an ICP was related to correctly answering questions on vaccination knowledge, while for Q5, the difference was not statistically significant (Table 2). In the ordinal logistic regression model, a relationship was found between belonging to an ICP group and having a high level of knowledge (Odds Ratio (OR) 3.397 95% CI [2.058–5.608]; p < 0.001, AIC = 1.226).
 |
Table 2 Multivariate Model and Propensity Score Matching of Correctly Answering the Vaccination Questions |
 |
Figure 3 Odds ratios and confidence intervals of multivariate models for factors associated with the probability of correctly answering vaccination questions 1 to 5. |
Discussion
The main finding of our study was that patients with COPD who received care in a structured program of comprehensive and integrated care had a higher level of knowledge about the importance of vaccination against influenza and pneumococcus for COPD patients than patients who were receiving the usual care. Although the differences between the ICP and UC groups were marked in terms of education and socioeconomic levels, the multivariate models, which were adjusted for possible confounding variables, consistently confirmed that receiving continued care in an ICP was associated with a higher probability of correctly answering questions on the use of vaccination in COPD. In the ICP group, 75.5% of the patients had a high level of knowledge compared to 42.7% of the patients in the UC group (p<0.001). This finding is relevant because it provides scientific evidence on the importance of education as part of comprehensive and integrated care programs for COPD.
The importance of educational programs has been described in previous studies.8,11,29 The objective of these programs is to achieve improved outcomes related mainly to the rate of exacerbations and the number of visits to emergency services.30–33 Other studies have found no differences in the outcomes of interest.9,32,34 The Global initiative for Chronic Obstructive lung Disease (GOLD)4 and American Thoracic Society and European Respiratory Society (ATS/ERS)35 guidelines describe the significance of educating patients about the importance of vaccination and state that low- and middle-income countries should provide personalized counseling and support materials such as booklets or brochures, among other resources. These strategies have been shown to improve knowledge, quality of life, and health-related outcomes.36 Few education studies for patients with COPD include the importance of vaccination,10 which may impact outcomes such as severe respiratory infection,29,37 because other items such as drug treatment and knowledge about the disease are considered to be more critical. Our findings are consistent with the literature, which has shown that integrated care programs, which include education about the disease as an integral part of the care model adapted to each latitude and with different educational methodologies, improve the level of patients’ knowledge and, in many cases, are associated with better outcomes.29,38,39
A study on asthma and COPD found that fewer than 50% of the subjects had received pneumococcal and influenza vaccination. The main reason was, the lack of information, in 87.6% of the patients while 37% did not consider it a reason for getting vaccinated.40 A Canadian study that surveyed patients diagnosed with COPD to assess their level of knowledge found that, while 60% of the participants received education from health professionals, only 5% received education from a pulmonologist; 49% reported that their main source of information was reading and the media and 23% reported that they received information from a clinic or hospital.41 In our study, education in the ICP group was conducted through group or individual sessions with health professionals, such as pulmonologists, internists, and respiratory therapists, which could explain the percentage of correct answers and the high level of knowledge of the patients in this group.
No differences were found between the ICP and UC groups in terms of the number of years since being diagnosed with COPD. A study that examined the level of knowledge in patients with COPD and their companions found that the more years since diagnosis, the higher the probability of providing correct answers in the general knowledge questionnaire.42 This could be related to the years that the subjects have been exposed to the disease and to recommendations delivered over these years by health professionals.
The educational level of patients in the ICP group was higher, as 64% had completed high school, but the educational level was not found to be related to answering the vaccination questions correctly. In a previous study that gauged patients’ level of knowledge about vaccination against pneumococcus and influenza, vaccination rate, and the effectiveness of vaccines in patients with COPD,37 no relationship was found between educational level and level of knowledge of vaccination, described a vaccination rate of 51.1% and found that 84.6% of the patients who were informed by physicians about the importance of vaccination followed their doctor’s recommendation and were vaccinated.37 These findings suggest the importance of constantly educating and recommending vaccinations to COPD patients. In contrast, a study that assessed general knowledge in COPD patients using the Mount Sinai Hospital Questionnaire (MSHQ) and the Lung Information Needs Questionnaire (LINQ)5 identified a positive relationship between having completed high school and the MSHQ total score. However, neither of these questionnaires included questions related to vaccination.
In a study on patients’ knowledge and behaviors related to influenza vaccination in veteran patients of two institutions who did not have a COPD diagnosis, where influenza vaccination programs included educational mailings and annual publicity, the participants answered more than 80% of the questions related to influenza vaccination correctly. Having previously received recommendations from doctors or nurses (OR 7.09 [4.2–11.9]; p = 0.002) and having previously been vaccinated (OR 6.36 [4.83–8.37]; p <0.001) were found to relate to a higher probability of being vaccinated,43 although the vaccination rate was around 50%.
In 2012, the World Health Organization (WHO) prepared the chronic care model, which focuses on the health of patients with chronic non-communicable diseases.26 ICPs have been developed following the WHO’s recommendations, seeking to improve patient’s quality of life, avoid clinical complications, and reduce hospital admission rates. Our study found that an ICP for COPD patients fosters a higher level of awareness of the importance of influenza and pneumococcal vaccination. These results echo previously reported results and provide a strong rationale for creating structured chronic care programs that can impact patients’ health and the financial resources of hospitals.
A significant strength of the study is that it is the first analysis performed in Colombia assessing the impact of an ICP on vaccination knowledge in patients with COPD. A significant number of patients were included, and an organized survey was used that allowed for the collection of relevant information, including demographic data, time since disease diagnosis, comorbidities, and level of knowledge of vaccination.
Our study has several weaknesses. COPD severity levels are not described because patients were identified based on medical records followed by confirmation by telephone with the patients. Significant differences were found between the two groups in terms of sociodemographic characteristics, however the different methods of statistical analysis used—adjusting for the confounding variables—consistently showed that the ICP group had a higher level of knowledge. Additionally, we do not have data on clinical outcomes, such as exacerbations, emergency care, or rate of vaccination, that can be modified by the vaccination strategy.
Conclusion
Our study showed that COPD patients who are cared for (or managed) continuously in an ICP have a higher level of knowledge of the importance of influenza and pneumococcal vaccination than patients who receive the usual care. More follow-up studies are required to assess the impact of comprehensive care programs on the health outcomes of these patients.
Funding
This is a substudy of the Study Impact of information strategies to modify knowledge attitudes and practices in chronic diseases in Bogotá. Project received funding from the “Sistema General de Regalías de Colombia” (BPIN code 2016000100037).
Disclosure
The authors report no conflicts of interest in this work.
References
1. The Global Health Observatory, Global Health Estimates: life expectancy and leading causes of death and disability. 2019; https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates.
2. Ministerio de Salud. EPOC: datos y cifras a nivel Global. 2022; https://www.minsalud.gov.co/Regiones/Paginas/MinSalud-promueve-control-de-enfermedad-pulmonar-obstructiva-crónica---EPOC.aspx.
3. Caballero A, Torres-Duque CA, Jaramillo C, et al. Prevalence of COPD in five Colombian cities situated at low, medium, and high altitude (PREPOCOL study). Chest. 2008;133(2):343–349. doi:10.1378/chest.07-1361
4. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease (2023 Report). Global initiative for Chronic Obstructive Lung Disease (GOLD). 2023. https://goldcopd.org/2023-gold-report-2/.
5. Scott AS, Baltzan MA, Dajczman E, Wolkove N. Patient knowledge in chronic obstructive pulmonary disease: back to basics. COPD. 2011;8(5):375–379. doi:10.3109/15412555.2011.605402
6. Guía de práctica clínica basada en la evidencia para la prevención, diagnóstico, tratamiento y seguimiento de la enfermedad pulmonar obstructiva crónica (EPOC) en población adulta. Colciencias MdSyPS-, ed2014: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/INEC/IETS/GPC-EPOC-completa.pdf.
7. Rose L, Istanboulian L, Carriere L, et al. Program of Integrated Care for Patients with Chronic Obstructive Pulmonary Disease and Multiple Comorbidities (PIC COPD +): a randomised controlled trial. Eur Respir J. 2018;51(1):1701567. doi:10.1183/13993003.01567-2017
8. Casas A, Troosters T, Garcia-Aymerich J, et al. Integrated care prevents hospitalisations for exacerbations in COPD patients. Eur Respir J. 2006;28(1):123–130. doi:10.1183/09031936.06.00063205
9. Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;2014(3):Cd002990. doi:10.1002/14651858.CD002990.pub3
10. Rice KL, Dewan NA, Bloomfield HE, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2010;182(7):890–896. doi:10.1164/rccm.200910-1579OC
11. Stoilkova A, Janssen DJ, Wouters EF. Educational programmes in COPD management interventions: a systematic review. Respir Med. 2013;107(11):1637–1650. doi:10.1016/j.rmed.2013.08.006
12. Soriano JB, Calle M, Montemayor T, Álvarez-Sala JL, Ruiz-Manzano J, Miravitlles M. Conocimientos de la población general sobre la enfermedad pulmonar obstructiva crónica y sus determinantes: situación actual y cambios recientes. Arch de Bronconeumología. 2012;48(9):308–315. doi:10.1016/j.arbres.2012.04.008
13. Londoño D, Garcia O Guía de prática clínica basada en la evidencia para la prevención, diagnóstico, tratamiento y seguimiento de la Enfermedad Pulmonar obstructiva Crónica en población adulta. Sistema General de Seguridad Social en Salud - Colombia 2014; https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/INEC/IETS/GPC-EPOC-completa.pdf.
14. Wongsurakiat P, Maranetra KN, Wasi C. Acute respiratory illness in patients with COPD and the effectiveness of influenza vaccination: a randomized controlled study. Chest. 2004;125(6):2011–2020. doi:10.1378/chest.125.6.2011
15. Poole PJ, Chacko E, Wood-Baker RW, Cates CJ, Influenza vaccine for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2000;4:Cd002733. doi:10.1002/14651858.CD002733
16. Bekkat-Berkani R, Wilkinson T, Buchy P, et al. Seasonal influenza vaccination in patients with COPD: a systematic literature review. BMC Pulm Med. 2017;17(1):79. doi:10.1186/s12890-017-0420-8
17. Bonten MJ, Huijts SM, Bolkenbaas M, et al. Polysaccharide conjugate vaccine against pneumococcal pneumonia in adults. N Engl J Med. 2015;372(12):1114–1125. doi:10.1056/NEJMoa1408544
18. Kharroubi G, Cherif I, Bouabid L, et al. Influenza vaccination knowledge, attitudes, and practices among Tunisian elderly with chronic diseases. BMC Geriatr. 2021;21(1):700. doi:10.1186/s12877-021-02667-z
19. Gallone MS, Infantino V, Ferorelli D, Stefanizzi P, De Nitto S, Tafuri S. Vaccination coverage in patients affected by chronic diseases: a 2014 cross-sectional study among subjects hospitalized at Bari Policlinico General Hospital. Am J Infect Control. 2018;46(1):e9–e11. doi:10.1016/j.ajic.2017.10.004
20. Sanftenberg L, Brombacher F, Schelling J, Klug SJ, Gensichen J. Increasing Influenza Vaccination Rates in People With Chronic Illness. Dtsch Arztebl Int. 2019;116(39):645–652. doi:10.3238/arztebl.2019.0645
21. Singh D, Agusti A, Anzueto A, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5). doi:10.1183/13993003.00164-2019
22. Ignatova GL, Avdeev SN, Antonov VN. Comparative effectiveness of pneumococcal vaccination with PPV23 and PCV13 in COPD patients over a 5-year follow-up cohort study. Sci Rep. 2021;11(1):15948. doi:10.1038/s41598-021-95129-w
23. Salud OPdl. Inmunizacion de las Americas. 2021; https://iris.paho.org/handle/10665.2/55370.
24. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
25. Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320(7234):569–572. doi:10.1136/bmj.320.7234.569
26. Cuidados Innovadores para las Condiciones Crónicas. 2013; https://www3.paho.org/hq/dmdocuments/2013/CuidadosInnovadores-v5.pdf.
27. R Core Team (2023). _R: A Language and Environment for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
28. College Station. Stata Statistical Software: Release 17 [Computer Program]. College Station; 2021.
29. Worth H, Dhein Y. Does patient education modify behaviour in the management of COPD? Patient Educ Couns. 2004;52(3):267–270. doi:10.1016/S0738-3991(03)00101-0
30. Bourbeau J, Farias R, Li PZ, et al. The Quebec Respiratory Health Education Network: integrating a model of self-management education in COPD primary care. Chron Respir Dis. 2018;15(2):103–113. doi:10.1177/1479972317723237
31. Rootmensen GN, van Keimpema AR, Looysen EE, van der Schaaf L, de Haan RJ, Jansen HM. The effects of additional care by a pulmonary nurse for asthma and COPD patients at an outpatient clinic: results from a double blind, randomized trial. Chest. 2021:244S.
32. Siddique HH, Olson RH, Parenti CM, et al. Randomized trial of pragmatic education for low-risk COPD patients: impact on hospitalizations and emergency department visits. Int J Chron Obstruct Pulmon Dis. 2012;7:719–728. doi:10.2147/COPD.S36025
33. Rea H, McAuley S, Stewart A, Lamont C, Roseman P, Didsbury P. A chronic disease management programme can reduce days in hospital for patients with chronic obstructive pulmonary disease. Intern Med J. 2004;34(11):608–614. doi:10.1111/j.1445-5994.2004.00672.x
34. Fan VS, Gaziano JM, Lew R, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med. 2012;156(10):673–683. doi:10.7326/0003-4819-156-10-201205150-00003
35. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64. doi:10.1164/rccm.201309-1634ST
36. Robertson NM, Siddharthan T, Pollard SL, et al. Development and Validity Assessment of a Chronic Obstructive Pulmonary Disease Knowledge Questionnaire in Low- and Middle-Income Countries. Ann Am Thorac Soc. 2021;18(8):1298–1305. doi:10.1513/AnnalsATS.202007-884OC
37. Cimen P, Unlu M, Kirakli C, et al. Should Patients With COPD Be Vaccinated? Respir Care. 2015;60(2):239–243. doi:10.4187/respcare.03350
38. Cosío BG, Shafiek H, Verdú J, et al. Implementation of an Integrated Care Model for Frequent-Exacerbator COPD Patients: a Controlled Prospective Study. Arch Bronconeumol. 2021;57(9):577–583. doi:10.1016/j.arbres.2021.01.025
39. Koff PB, Min SJ, Freitag TJ, et al. Impact of Proactive Integrated Care on Chronic Obstructive Pulmonary Disease. Chronic Obstr Pulm Dis. 2021;8(1):100–116. doi:10.15326/jcopdf.2020.0139
40. Schoefer Y, Schaberg T, Raspe H, Schaefer T. Determinants of influenza and pneumococcal vaccination in patients with chronic lung diseases. J Infect. 2007;55(4):347–352. doi:10.1016/j.jinf.2007.06.002
41. Hernandez P, Balter M, Bourbeau J, Hodder R. Living with chronic obstructive pulmonary disease: a survey of patients’ knowledge and attitudes. Respir Med. 2009;103(7):1004–1012. doi:10.1016/j.rmed.2009.01.018
42. Nakken N, Janssen DJA, van den Bogaart EHA, et al. Knowledge gaps in patients with COPD and their proxies. BMC Pulm Med. 2017;17(1):136. doi:10.1186/s12890-017-0481-8
43. Nichol KL, Lofgren RP, Gapinski J. Influenza vaccination. Knowledge, attitudes, and behavior among high-risk outpatients. Arch Intern Med. 1992;152(1):106–110. doi:10.1001/archinte.1992.00400130124015
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
