Back to Journals » Advances in Medical Education and Practice » Volume 7
Knowledge, awareness, and attitude regarding infection prevention and control among medical students: a call for educational intervention
Authors Ibrahim A, Shamseldin Elshafie S
Received 4 April 2016
Accepted for publication 31 May 2016
Published 22 August 2016 Volume 2016:7 Pages 505—510
DOI https://doi.org/10.2147/AMEP.S109830
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Awab Ali Ibrahim,1 Sittana Shamseldin Elshafie,2
1Department of Physiology and Biophysics, Weill Cornell Medical College in Qatar, 2Aspetar, Laboratory Department, Qatar Orthopedic and Sports Medicine Hospital, Doha, Qatar
Background: Medical students can be exposed to serious health care-associated infections, if they are not following infection prevention and control (IPC) measures. There is limited information regarding the knowledge, awareness, and practices of medical students regarding IPC and the educational approaches used to teach them these practices.
Aim: To evaluate the knowledge, awareness, and attitude of medical students toward IPC guidelines, and the learning approaches to help improve their knowledge.
Methods: A cross-sectional, interview-based survey included 73 medical students from Weill Cornell Medical College, Qatar. Students completed a questionnaire concerning awareness, knowledge, and attitude regarding IPC practices. Students’ knowledge was assessed by their correct answers to the survey questions.
Findings: A total of 48.44% of the respondents were aware of standard isolation precautions, 61.90% were satisfied with their training in IPC, 66.13% were exposed to hand hygiene training, while 85.48% had sufficient knowledge about hand hygiene and practiced it on a routine basis, but only 33.87% knew the duration of the hand hygiene procedure.
Conclusion: Knowledge, attitude, and awareness of IPC measures among Weill Cornell Medical Students in Qatar were found to be inadequate. Multifaceted training programs may have to target newly graduated medical practitioners or the training has to be included in the graduate medical curriculum to enable them to adopt and adhere to IPC guidelines.
Keywords: infection prevention, education, medical students
Introduction
Health care-associated infections (HCAIs) are important public health problems. They exert increased morbidity and mortality, and increase the health care cost, both in developed and developing countries. It was stated by the International Nosocomial Infection Control Consortium that the pooled rate of central line-associated blood stream infections in the intensive care units in Latin America, Asia, Africa, and Europe were 4.9 per 1,000 central line days, nearly fivefold higher than the rate reported from comparable US intensive care units. The overall rate of ventilator-associated pneumonia was also higher (16.8 vs 1.1 per 1,000 ventilator days), as was the rate of catheter-associated urinary tract infection (5.5 vs 1.3 per 1,000 catheter days).1–3 HCAIs are also associated with increased length of hospital stay,4,5 and the emergence of multidrug-resistant bacteria.6
At least 5%–10% of patients admitted to acute care hospitals acquire an infection. It is estimated that one out of every 20 hospitalized patients will contract an HCAI. The risk is substantial not only for patients, but also for health care workers (HCWs), including medical students.7–9 Hence, it is essential for medical students to have adequate knowledge about infection prevention and control (IPC) practices and to incorporate these in the professional training of medical students. Compliance on the part of the HCWs, including medical students, with standard precautions and hand hygiene has been recognized as an efficient means to prevent and control HCAIs.10 Such measures not only protect the patient and family, but also the HCWs, students, and environment.11
The undergraduate medical education is the formative phase and appropriate moment for acquiring the necessary knowledge and skills. There is lack of evidence regarding explicit infection control training in the curriculum of most medical undergraduate courses, which needs to be addressed if HCAI rates are to be reduced.12 Although medical students consider IPC practices, particularly hand hygiene, to be a relevant and important topic, they feel that learning about the topic may be compromised during their medical training due to the congested medical curriculum.13 Thus the teaching and training requirements of undergraduate medical students regarding these practices need to be assessed.
This study was undertaken to assess the knowledge, awareness, and attitude of the medical students toward basic infection control practices, such as standard precautions, hand hygiene, respiratory hygiene and cough etiquette, tuberculosis (TB) control, and use of personal protective equipment, and the learning approaches that help improve their knowledge and practices.
Materials and methods
A cross-sectional interview-based survey among medical students from Weill Cornell Medical College, Qatar, which runs a 6-year modular undergraduate medical program (2 years of basic sciences and 4 years of clinical training) was conducted using a validated questionnaire.
The questionnaire was developed by researchers with help from previous literature to cover key areas of IPC guidelines, including hand hygiene, knowledge about standard isolation precautions, respiratory hygiene and cough etiquette, use of personal protective equipment, cleaning and disinfection of medical equipment, as well as their satisfaction with their IPC teaching and education.
The survey is also used to explore the students’ views regarding effective teaching and learning mechanisms for improving knowledge, fostering correct attitude and practices among medical students. The information deduced may be used to identify areas of improvement in medical students’ training.
The 22-item survey questionnaire was distributed to all the medical students via email. Only 73 out of 170 students responded. A pilot study was conducted by distribution of 20 questionnaires to 20 interns to assess the validity, reliability, and bias of the questionnaire.
Data entry was done through EpiData 3.1 (Epidata Association, Copenhagen, Denmark) twice. The two authors entered the same data and the data files were compared to rule out errors in entering the data. Data were analyzed using SPSS version 16 (SPSS Inc., Chicago, IL, USA). Percentages were calculated for the entire variables. Relevant tables and figures were computed.
The study was approved by Weill Cornell Medical College-Qatar Ethics Review Board, which waived the need for consent. The students’ response to the questionnaire was also regarded as consent.
Results
The study group comprised 73 medical students out of a total of 170 students (42.94%). Characteristics of the responding students are presented in Table 1. A total of 31 (48.44%) respondents were aware about standard isolation precautions as a minimum requirement for the care of all patients irrespective of their diagnosis. A total of 41 (66.13%) respondents were exposed to hand hygiene training, while 53 (85.48%) had sufficient knowledge about hand hygiene, and hand hygiene is embedded in their routine clinical practice. A total of 45 (75.00%) wash their hands before and after each patient encounter (Table 2).
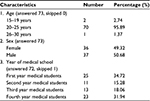  | Table 1 Characteristics of the responding students |
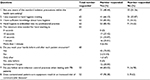  | Table 2 Responses of the medical students Abbreviation: TB, tuberculosis. |
However, only 21 (33.87%) respondents were aware that a minimum of 15 seconds is needed for adequate hand hygiene (Table 2). The respondents were asked about their knowledge of respiratory hygiene and cough etiquette; 52 (98.11%) were aware of the protocol to cough and sneeze on a napkin and wash hands, but only 31 (58.49%) were aware of alternatives if napkins were not available, that is, to cough/sneeze over shoulder, and 30 (56.60%) keep a distance of >3 feet from others when coughing (Table 3).
  | Table 3 Students’ knowledge regarding respiratory hygiene and cough etiquette |
Their knowledge regarding the transmission of pulmonary TB and the use of strict infection control procedures when interacting with TB patients was relatively high, 44 (83.02%) (Table 2), but there was mixed knowledge regarding the use of N95 mask (Table 4), and the use of jewelry and artificial nails (Table 5).
  | Table 4 Students responses: evaluate the following statements about the N95 mask |
  | Table 5 Students responses: in your opinion, which of the following is associated with an increased risk for spread of diseases? |
The responding medical students had significantly more knowledge regarding appropriate use of attire and spread of communicable diseases through used medical equipment; 47 (90.38%) (Table 2). When students were asked about satisfaction with their training in IPC practices, only 39 (61.90%) students were satisfied with their training in basic IPC measures and 23 (35.38%) think classmates and/or senior doctors act as role models of the practices of IPC (Figures 1 and 2).
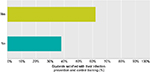  | Figure 1 Are you satisfied with your training in basic infection prevention and control measures? |
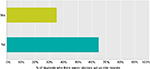  | Figure 2 Do classmates and/or senior doctors act as role models in the practices of infection prevention and control. |
Discussion
Exposure to infectious diseases is one of the most frequently identified occupational hazards facing medical students and HCWs in general. Awareness and adequate knowledge about prevention of such infections are important requirements for all medical students.
The response rate of the students was 76.04%, but not all of them responded to all questions. Much information could have been missed from those who did not answer some of the important survey questions.
This type of survey is the most feasible approach to explore students’ knowledge and awareness, although exchange of responses could have happened despite the clear request not to do so. We anticipated that the anonymity arrangement gave confidence to participate and give truthful responses.
We are not oblivious to the fact that practices are better observed than self-reported as an effective way to measure compliance,14,15 thus what was reported may not be as factual as what might have been observed. Awareness of observation may influence students’ behavior. However, the effect of being monitored (the Hawthorne effect) has also been reported to improve compliance.16
Standard isolation precautions guideline is the gold standard of infection prevention. The knowledge of students regarding standard isolation precautions was very low (48.44%), while their general awareness regarding IPC practices related to hand hygiene, use of appropriate attire, respiratory hygiene and cough etiquette, and TB control was reasonably high, which is similar to that found in other studies in India17,18 and the People’s Republic of China.19 However, when questions were asked regarding details of practices, for example, duration of effective hand hygiene procedure, respiratory hygiene and cough etiquette procedure, and the use of N95 mask for TB control, the level of knowledge decreased significantly. Similar findings were observed by studies in India17,18 and the UK.20–22
Though overall knowledge is less than desired, the disparity between knowledge and practices clearly shows that knowledge of infection control guidelines and a positive attitude toward infection control measures alone does not influence compliance with the approved infection control guidelines.
There were many areas of concern, such as only 66.13% of the participating students were exposed to hand hygiene training and 75.00% washed their hands before patient encounter. A total of 35.38% of respondents found their classmates and senior medical doctors act as role models. A role model is important for the subconscious teaching that should go on during clinical practices. A change of culture and training in relation to IPC is needed, so that good IPC practices are modeled by seniors to cultivate and sustain such practices in medical students.23
Multiple sources of information, teaching and training medical students are available. The evidence for the most appropriate method of teaching and learning for medical students has been conflicting. The effect of the variety of teaching types reported by students, in various studies, was unclear.20 A study in the People’s Republic of China had clearly demonstrated that a one-time intervention program had no effect on knowledge.19 A UK study demonstrated that structured teaching programs are effective.24,25 Calabro et al showed that a single infection control educational intervention provided in medical schools is inadequate to teach students about infection control and safety techniques.26
Increasing the emphasis on IPC in the undergraduate curriculum through frequent education and assessment, particularly in the clinical setting, and by peers and seniors acting as role models, may improve students’ knowledge, attitude and practices, and facilitate patient safety culture, thereby impacting HCAI acquisition rates and improving patient’s outcome. Scenario-based learning, assessment, both summative and formative, reflections, and online teaching in conjunction with face-to-face learning (blended learning) are all suggested examples of effective methods of teaching IPC practices.20,27–30
We believe that the results of the study may be generalized to medical, dental, and nursing graduates, and all HCWs. The obvious limitation of our study was the lack of pre- and post-educational surveys in the same sample. The study was made on the assumption that the study group had been exposed to IPC policies and guidelines. The compliance with the infection control practices was measured based on their responses. A more effective way of measuring compliance would have been to monitor them.
Conclusion
The study points to inadequate knowledge, awareness, and practices of IPC guidelines among Weill Cornell Medical College, Qatar, students. Only through proper education of future HCWs, the burden of HCAIs can be reduced. We recommend performing infection control education programs to increase safety of our graduates and patients. The medical education program should be started at the college level before starting the clinical practice years along with seminars and feedback, which highlight importance of IPC guidelines. Education should be enhanced by peers, seniors, and HCWs by acting as role models of infection control. Multiple bundles or groups of measures have been developed to control and prevent HCAIs. Such bundles must be introduced to the medical students early in their career to apply when they start their clinical care, to improve patient’s safety.31
Acknowledgment
We would like to thank all students who participated in the survey.
Disclosure
The authors report no conflicts of interest in this work.
References
Rosenthal VD, Ramachandran B, Villamil-Gomez W, et al. Impact of a multidimensional infection control strategy on central line-associated bloodstream infection rates in pediatric intensive care units of five developing countries: findings of the International Nosocomial Infection Control Consortium (INICC). Infection. 2012;40(4):415–423. | ||
Dudeck MA, Edwards JR, Allen-Bridson K, et al. National Healthcare Safety Network report, data summary for 2013, Device-associated module. Am J Infect Control. 2015;43(3):206–221. | ||
Al-Mousa HH, Omar AA, Rosenthal VD, et al. Device-associated infection rates, bacterial resistance, length of stay, and mortality in Kuwait: International Nosocomial Infection Consortium findings. Am J Infect Control. 2016;44(4):444–449. | ||
Zilberberg MD, Shorr AF. Economic aspects of preventing health care-associated infections in the intensive care unit. Crit Care Clin. 2012;28(1):89–97. | ||
Rosenthal VD, Guzman S, Migone O, Crnich CJ. The attributable cost, length of hospital stay, and mortality of central line-associated bloodstream infection in intensive care departments in Argentina: A prospective, matched analysis. Am J Infect Control. 2003;31(8):475–480. | ||
Rosenthal VD, Maki DG, Mehta Y, et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 43 countries for 2007–2012. Device-associated module. Am J Infect Control. 2014;42(9):942–956. | ||
Ayub A, Goyal A, Kotwal A, Kulkarni A, Kotwal A, Mahen A. Infection control practices in healthcare: Teaching and learning requirements of medical undergraduate. Med J Armed Forces India. 2013;69(2):107–112. | ||
Lozzari S, Allegranzi B, Cocia E. Making hospital safer: the need for a global strategy for infection control in healthcare settings. World Hosp Health Serv. 2004;40(2):36–42. | ||
Vincent J L. Nosocomial infections in adult intensive care units. Lancet. 2003;361(9374):2068–2077. | ||
Clarke SP, Rackell Jl, Sloane DM, Aiken LH. Organizational climate, staffing and safety equipment as predictors of needle-stick injury and near-misses in hospital nurses. Am J Infect Control. 2002;30(4):207–216. | ||
Garner JS. Guidelines for isolation precautions in hospitals. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1996;17(1):53–80. | ||
Garcia-Zapata MRC, Silva Sousa AC, Guimaraes JV, Tipple AV, Prado MA, Garcia-Zapata MTA. Standard precautions: knowledge and practice among nursing and medical students in a teaching hospital in Brazil. Int J Infect Control. 2010;6(1). | ||
Melenhorst WB, Poos HP, Meessen NE. Medical students need more education on hygiene behaviour. Am J Infect Control. 2009;37(10):868–869. | ||
Kamulegeya A, Kizito AN, Balidawa H. Ugandan medical and health sciences interns’ infection control knowledge and practices. J Infect Dev Ctries. 2013;7(10):726–733. | ||
Jenner E.A, Fletcher B.C, Watson P, Jones F.A, Miller L, Scott GM. Discrepancy between self-reported and observed hand hygiene behaviour in healthcare professionals. J Hosp Infect. 2006;63(4):418–422. | ||
MaCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, Fisher P. The Hawthorne Effect: a randomised controlled trial. BMC Med Rev Methodol. 2007;7:30. | ||
Kotwal A, Tareja DK. Healthcare workers and universal precautions perception and determinants of non-compliance. Indian J Community Med. 2010;35(4):551–553. | ||
Kermode M, Jolley D, Langkhan M, Thomas M.S, Crofts N. Occupational exposure to blood and risk of blood borne viruses infection among healthcare workers in rural North Indian healthcare settings. An Infect Control. 2005;33(1):34–41. | ||
Zhang Z, Yamamoto T, Wu XN, Moji K, Cai GX, Kuroiwa G. Educational intervention for preventing blood borne infections among medical students in China. J Hosp Infect. 2010;75(1):47–51. | ||
Feather A, Stone SP, Wessier A, Boursicot KA, Pratt C. “Now please wash your hands”: the hand washing behaviour of final MBBS candidates. J Hosp Infect. 2000;45(1):62–64. | ||
Chaco J, Isaac R. Percutaneous injuries among medical interns and their knowledge and practice of post-exposure prophylaxis for HIV. Indian J Public Health. 2007;51(2):127–129. | ||
Amin TT, Al Noaim KI, Bu Saad MA, Al Malhm TA, Al Mulhim AA, Al Alwas MA. Standard precautions and infection control; medical students’ knowledge and behavior at Saudi University: the need for change. Glob J Health Sci. 2013;5(4):114–125. | ||
Mann CM, Wood A. How much do medical students know about infection control? J Hosp Infect. 2006;64(4):366–370. | ||
Phillips G, Ker J. Champion students! Experience with a standardized infection control training package for medical students. J Hosp Infect. 2006;62(4):518–528. | ||
Brien DO, Richard J, Walton KE, Phillips MGA, Humphreys H. Survey of teaching/learning of healthcare associated infections in UK and Irish medical schools. J Hosp Infect. 2009;73(2):171–175. | ||
Calabro K, Bright K, Kouzekanani K. Long term effectiveness of infection control training among fourth-year medical students. Med Educ Online. 2005:1–7. Available from: http://www.med.ed.nline.org. Accessed March 4, 2016. | ||
Kaur R, Razee H, Seale H. Facilitators and barriers around teaching concepts of hand hygiene to undergraduate medical students. J Hosp Infect. 2014;88(1):28–33. | ||
Hunt DCE, Mohammudally A, Stone SP, Dacre J. Hand hygiene behaviour, attitudes and believes in first year clinical medical students. J Hosp Infect. 2005;59(4):371–373. | ||
Lehmann R, Bosse HM, Huwendiek S. Blended learning using virtual patients and skills laboratory training. Med Educ. 2010;44(5):521–522. | ||
Pereira JA, Pleguezuelos E, Meri A, Molina-Ros A, Molina-Tomas MC, Masdeu C. Effectiveness of using blended learning strategies for teaching and learning human anatomy. Med Educ. 2007;41(2):189–195. | ||
Rosenthal VD, Duenas L, Sobreyra-Oropeza M, et al. Findings of the International Nosocomial Infection Control Consortium (INICC), part III: effectiveness of a multidimensional infection control approach to reduce central line-associated bloodstream infections in the neonatal intensive care units of 4 developing countries. Infect Control Hosp Epidemiol. 2013;34(3):229–237. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
