Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Knowledge, Attitude, Behavior, and Socioeconomic Conditions of People Living with HIV in Indonesia During the COVID-19 Pandemic: A Cross-Sectional Study
Authors Karjadi TH , Maria S, Yunihastuti E , Widhani A , Kurniati N, Imran D
Received 13 August 2021
Accepted for publication 12 November 2021
Published 14 December 2021 Volume 2021:13 Pages 1045—1054
DOI https://doi.org/10.2147/HIV.S333469
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Teguh Harjono Karjadi,1,2 Suzy Maria,1,2 Evy Yunihastuti,1,2 Alvina Widhani,1,2 Nia Kurniati,1,3 Darma Imran1,4
1Integrated HIV Center, Dr. Cipto Mangunkusumo General Hospital, Central Jakarta, DKI Jakarta, Indonesia; 2Allergy and Clinical Immunology Division, Internal Medicine Department, Faculty of Medicine of Universitas Indonesia, Central Jakarta, DKI Jakarta, Indonesia; 3Allergy and Clinical Immunology Division, Pediatric Department, Faculty of Medicine of Universitas Indonesia, Central Jakarta, DKI Jakarta, Indonesia; 4Infection and Immunology Division, Neurology Department, Faculty of Medicine of Universitas Indonesia, Central Jakarta, DKI Jakarta, Indonesia
Correspondence: Suzy Maria
Allergy and Clinical Immunology Division, Internal Medicine Department, Faculty of Medicine of Universitas Indonesia, Jalan Pangeran Diponegoro No. 71, Senen, Central Jakarta, Indonesia
Tel +62 21 3141160
Fax +62 21 3904546
Email [email protected]
Purpose: This study aimed to analyze the knowledge, attitude, and behavior of people living with HIV (PLWH) during the COVID-19 pandemic and the pandemic’s impact on their socioeconomic conditions, antiretroviral adherence, and worries.
Materials and Methods: This cross-sectional study was conducted in May–August 2020 at the Integrated HIV Center of Dr. Cipto Mangunkusumo General Hospital, Indonesia. The data were collected using an online questionnaire and an offline paper-based questionnaire.
Results: A total of 545 subjects participated in this study, 72.8% (397) of which were male. Most subjects were middle-aged (36– 55 years old) (66.5%). Many subjects reported to have experienced reduced incomes (49.2%) or losses of income (22.4%), while 15.6% reported losing their job during the COVID-19 pandemic. Most subjects (97%) wished to continue treatment despite the many obstacles, and the subjects’ knowledge about COVID-19 and its prevention was considerably good. More than 70% of subjects reported that they have been implementing the general precautions of the COVID-19 pandemic: maintaining distance, wearing a mask, washing hands, and avoiding crowds.
Conclusion: This study provides an overview of what PLWH are experiencing, which will allow for policy-making that can help them continue their treatment with consideration of the possibility of having to live a “new normal” future.
Keywords: knowledge, attitude, behavior, PLWH, COVID-19
Introduction
The first cases of coronavirus disease 2019 (COVID-19) infection were announced by the Indonesian government on March 2, 2020.1 Prior to this, the World Health Organization (WHO) had declared a global health emergency on January 30, 2020, due to the COVID-19 infection, which originated in China’s Wuhan province. By November 17, 2021, 4,251,945 cases had been confirmed in Indonesia.2 COVID-19 is an infectious disease caused by a coronavirus with symptoms ranging from mild to severe respiratory disease. Those who experience mild disease can recover without special treatment; however, the elderly, people with comorbidities, such as hypertension, diabetes mellitus, cardiovascular disease, chronic lung disease, and immunocompromised conditions are at risk of severe disease that often leads to death. Therefore, people living with HIV (PLWH) are at higher risk for COVID-19 complications.3–5 The first reported patient with coinfection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and human immunodeficiency virus (HIV) was diagnosed with HIV positivity after acquiring the coronavirus infection.6 Other case reports, case series, and comments followed this report.7 A case series obtained from Barcelona, Spain, reported that 1% (5 out of 543 cases) of hospitalized COVID-19 patients were PLWH.8 Aydın et al reported four cases of PLWH coinfected with SARS-CoV-2 in Turkey.9 Another study found a rate of coinfection in PLWH of 1.2–1.8% and its results did not support previous suggestions that PLWH might be protected from worse outcomes.10
Over the previous three decades, there has been a sixfold increase in the number of HIV counselling and testing clinics, a three-fold increase in the number of people screened for HIV, and a nearly three-fold increase in the number of clinics providing antiretroviral therapy (ART) services in Indonesia.11,12 However, the fear of contracting COVID-19 has led to lower engagement in care among PLWH in several countries. The reasons for this are not unexpected. People who live under the burden of a chronic virus are hesitant to engage in care when the prospect of being infected with a possibly more deadly virus is real.13 This fear has even led some patients to question the safety of going to hospitals or clinics to get ART. Since March 2020, the Indonesian government has implemented the social distancing policy through large-scale social restrictions to reduce the transmission of COVID-19.14 These large-scale social restrictions have also significantly hindered access to care. Even when people can access hospitals and clinics, the financial stress from loss of livelihoods makes it harder for them to pay for care. These conditions may considerably impact behavioral and mental health.15
The search for pharmacological therapies against SARS-CoV-2 has initially focused mainly on repurposing drugs targeting other viruses, including antiretroviral drugs (ARV) used to treat HIV. Initial genomic analysis of SARS-CoV-2 has indicated that viral enzymes are similar in sequence to the respective enzymes in SARS and Middle East Respiratory Syndrome (MERS). Early optimism about protease inhibitors, such as lopinavir/ritonavir (LPV/r), arose from early guidance from Wuhan and prior data suggesting efficacy against SARS and MERS.16 It has been suggested that PLWH are not very likely to develop a severe form of COVID-19 infection because some ART regimens may have some activity against the coronavirus. These early findings may affect the attitude and behavior of PLWH during the COVID-19 pandemic. This study aimed to analyze the knowledge, attitude, and behavior of PLWH during the COVID-19 pandemic and the pandemic’s impact on their socioeconomic conditions, ARV adherence, and worries.13,17,18
Materials and Methods
This cross-sectional study was conducted in May–August 2020 on PLWH of the integrated HIV center of Dr. Cipto Mangunkusumo General Hospital, Indonesia. The integrated HIV center of Dr. Cipto Mangunkusumo General Hospital is a tertiary healthcare center, which provides care for PLWH who are referred from primary and secondary healthcare centers. Data collection was done using an online questionnaire through Google Form and an offline paper-based questionnaire, both of which were in the Indonesian language. The questionnaire is displayed in Supplementary File 1. Information about the study was given to the patients through chat messenger and those who were interested in joining the study registered via an online link. Paper-based questionnaires were also given to patients attending the clinic. A paper-based consent form or an e-consent form needed to be signed with signature or clicking a box before joining the study. The consent form included a disclaimer, which states that participation is voluntary and no penalties are involved in refusal to participate.
All patients diagnosed with HIV/AIDS (based on medical records) were eligible to participate in this study with no exclusion criteria. Data was collected on participant demographics including age, gender, medical record number, education, occupation, marital status, income in the past 1 year, income after the beginning of the COVID-19 pandemic, co-morbidities, ART regimens, CD4 count in the past 3 months, history of pneumococcal and influenza vaccines, and history of smoking. The groups are divided according to the standard of Indonesian Ministry of Education, where the obligated length of schooling, or “Wajib Belajar” is 12 years (equal to high-school graduate). To assess their knowledge of COVID-19, subjects were asked about COVID-19 transmission, symptoms, available therapies, and how to protect themselves and their family from COVID-19. There were five questions in this section. Subjects who had three or more correct answers were grouped into a good level of knowledge, while those having two or less correct answers were grouped into the poor level of knowledge. For behavior, subjects were asked about what precautions they took to avoid contracting COVID-19. Subjects were also asked about their COVID-19 concerns in multiple choice and scale questions, as well as their ART adherence and their efforts to sustain their ARV stock during the pandemic.
Data were analyzed using SPSS® 25 for Mac software (IBM Corp., Armonk, New York, USA). Variables were analyzed using chi-square test, Kruskall–Wallis test, and Mann–Whitney U-test (when data were not normally distributed). This study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of Faculty of Medicine, University of Indonesia.
Results
A total of 545 subjects participated in this study. There were 143 participants who took paper-based survey (26.2%). Dominant characteristics of the subjects included being male (72.8%), middle-aged (36–55 years old) (66.5%), married (49.5%), and a high-school graduate (49.5%). Only 26.5% of the subjects reported to have comorbidities, with hypertension (9.5%), tuberculosis (7.2%), and diabetes mellitus (3.5%) being the most reported. Most of the subjects (42.6%) claimed to have no history of smoking. Only 4.2% and 3.3% of the subjects had received pneumonia and influenza vaccinations, respectively. Detailed characteristics of the subjects are displayed in Table 1.
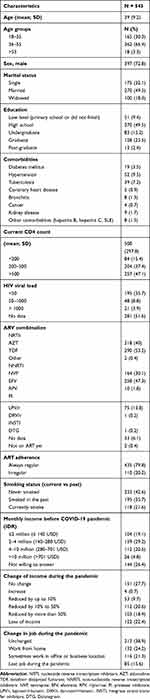 |
Table 1 Demographics of the Study Subjects |
ART in PLWH
Most subjects were on Tenofovir/TDF-based (53.2%) and Efavirenz-based (47.3%) regimens. Most subjects also reported regular ARV consumption (good ARV adherence) and CD4 counts of >200 cells/µL (84.5%). More than half of the subjects (51.6%) did not have HIV viral load data, while the available data varied between <1000 copy/mL in 44.5% of the subjects and >1000 copy/mL in 3.9% of the subjects. The detailed characteristics of ART and treatment response of the study subjects can be seen in Table 1.
The Influence of the Pandemic on the Jobs and Incomes of PLWH
About 49.2% of the subjects reported to have reduced income during the COVID-19 pandemic, while 22.4% of the subjects lost their incomes. Most subjects (97%) wished to continue treatment despite the many obstacles (loss of income, loss of jobs, and issues about transportation to clinic) they were facing.
In terms of employment, around 38.9% of the subjects did not experience any changes. However, 15.6% of the subjects lost their jobs. The detailed report can be seen in Table 1.
Knowledge of COVID-19 Infection and Its Impact on PLWH
Most subjects were able to answer questions about COVID-19 infection. Around 90.6% of the subjects answered the questions about COVID-19 transmission correctly and 80.6% of the subjects answered questions about symptoms correctly. However, when they were questioned about the impact of HIV infection on COVID-19, their responses were more varied. Interestingly, almost half of the subjects (45.3%) answered yes when they were asked, “Can ART prevent COVID-19 infection?”. The detailed results can be seen in Table 2.
 |
Table 2 Knowledge of COVID-19 and Impact of HIV Infection on COVID-19 |
Based on the bivariate analysis, it was found that the level of knowledge of COVID-19 was closely related to age (p value = 0.045). Interestingly, education was not directly associated with the level of knowledge of COVID-19 in this study. The detailed report can be seen in Table 3.
 |
Table 3 Characteristics of PLWH Based on Their Level of Knowledge of COVID-19 |
Behavior of Subjects During the COVID-19 Pandemic
Worry of Contracting the COVID-19 Virus
Around 56% of the subjects were worried about contracting COVID-19 to the point that it interfered with their daily activities. Another 37% stated that they worried but continued their daily activities, and 7% of the subjects reported not feeling worried. Interestingly, only the usage of LPV/r had a significant correlation with worrying about COVID-19 infection (p value = 0.042). The results of bivariate analysis can be seen in Table 4.
 |
Table 4 Characteristics of PLWH Based on Level of Worry of COVID-19 Infection |
Desire to Get Influenza and Pneumococcal Vaccines
Up to 55% of the subjects expressed wishes to get the influenza or pneumococcal vaccination, whereas the remaining 45% did not want to get these vaccinations.
Actions Taken During the COVID-19 Pandemic
Some subjects (25.1%) reported consistently consuming herbal medicine during the pandemic. In general, most subjects reported following the general precautions of the COVID-19 pandemic. More detailed responses provided by subjects can be seen in Figure 1.
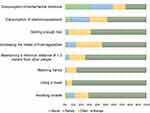 |
Figure 1 Actions that are taken during the COVID-19 pandemic. |
Behavior Associated with HIV Treatment During the COVID-19 Pandemic
Up to 97% of the subjects have continued to take ART during the pandemic, leaving only 3% who stopped taking ART. 60% of the subjects reported being worried about running out of ART stocks due to the pandemic. The COVID-19 pandemic has also resulted in a fear of visiting the hospital for 48% of the subjects. The subjects’ responses can be seen in detail in Figure 2. Those who fear visiting the hospital have made various efforts to avoid the interruption of ART consumption. Some have gone to other healthcare facilities to obtain ART, while others tried to contact the clinic or use telemedicine to have their ART delivered. These efforts can be seen in Figure 3.
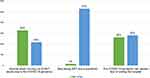 |
Figure 2 Behaviors regarding HIV treatment. |
 |
Figure 3 Efforts to prevent stop taking ART interruption. |
Discussion
During this COVID-19 pandemic, which has been ongoing for more than a year, the Indonesian government has implemented the social distancing policy through large-scale social restrictions to reduce the transmission of COVID-19. This policy, while beneficial for COVID-19 prevention, has had negative effects on the daily lives of PLWH. Difficulties, in particular, relate to the ability to maintain ART consumption and worries of contracting the COVID-19. A study by Fodjo et al in Belgium and Brazil reported that COVID-19 and its associated restrictive measures have adversely affected the well-being and follow-up of PLWH.19
The subjects that took our survey were mostly men and most of them were married. For monthly income, the percentages of subjects with incomes above and below the regional minimum wage were 51% and 49%, respectively. This indicates that half the subjects were in the lower economic class.20
The majority of subjects in this study were in first-line ART (86.2%) as reflected by the use of Lopinavir/r (a protease inhibitor) as the second line in Indonesia at as much as 13.8%. For CD4 lymphocyte levels in the last 3 months, most subjects had >200 cells/µL: 37.4% of the subjects had CD4 counts of 200–500 cells/µL (advanced to mild immune deficiency) and 47.1% of the subjects had CD4 counts of >500 cells/µL. In regards to how regularly the subjects took ARV, 79.8% took it regularly (exhibited good adherence). In general, the results of the therapy above were quite good, although the analysis must be cross-checked with the results of viral load suppression. In this study, most subjects did not remember their last viral load (51.6%) or had not had it checked in the last 3 months.
COVID-19 has also impacted on the income and work of the subjects. Most have experienced decreases in income (71.6%) and work (45.5% did receive full working hours but did not get a full income), and in fact 15.6% of the subjects had lost their jobs. Considering that half the subjects were from the lower economic class and experienced decreases in income or even loss of job, the government needs to address the impacts of this pandemic; citizens are being burdened with additional costs to buy masks and other means of self-protection, as well as living costs and health costs if they are sick.
Regarding COVID-19 infection, most subjects quite understood the way in which this virus is transmitted; however, their knowledge on how to respond to being infected was almost equally split between accurate and inaccurate information. In terms of the behavior of the subjects during this pandemic, 56% of the subjects reported feeling anxious but said it did not affect their daily life and a further 7% of the subjects reported not feeling worried at all. Thus, a total of 63% of the subjects still had the courage to carry out their daily activities. On the other hand, there was a fairly large portion, 37% of the subjects, who felt worried to the point that it affected their daily activities and even made them refrain from visiting health facilities. This was evident in the next question in which 48% of the subjects reported being afraid to go to the hospital. Fear of visiting the hospital could disrupt the subjects’ ART continuity. This problem could be addressed by administering multi-month dispensing ARV, utilizing online media to communicate with health services, and sending ARV via courier services, so that treatment continuity can be guaranteed. Indonesian Ministry of Health created a new set of policies in April 2020, which allows PLWH in a stable condition and without opportunistic infections or comorbidities to access multi-month ARV dispensing, up to 3 months.21
The majority of subjects took appropriate actions to avoid COVID-19 infection. Seventy percent of the subjects avoided COVID-19 infection by always wearing a mask, washing their hands, maintaining their distance, and avoiding crowds. Meanwhile, other efforts, such as taking vitamins, herbal medicines, consuming fruits and vegetables, and getting adequate rest were done by less than 60% of the subjects. The 26.5% of the subjects with comorbid diseases were at a greater risk of getting severe disease if they were infected with the COVID-19 virus. The government’s message to the public has been in accordance with the recommendations of WHO: to maintain distance, avoid crowds, wash hands, and wear masks.
This study found that age was closely related to the level of knowledge of COVID-19 (p value = 0.045), even though the difference in mean age between the groups was not clinically important (39 years old for poor level of knowledge and 41 years old for a good level of knowledge). In a study by Stephenson et al of US gay, bisexual, and other men who have sex with men (GBMSMs), subjects aged over 25 reported COVID-19 to be more severe than HIV than subjects aged 18–24. This study mentioned that younger subjects might have a greater sense of optimism bias and did not feel at risk of COVID-19 infection.22 Interestingly, education was not directly associated with level of knowledge of COVID-19 in this study.
A positive finding from this study is that 97% of the subjects were still committed to take ART during this pandemic, and 77% did visit healthcare facilities or accessed assistance in various other wise ways, such as having official online hospital consultations and getting medicines through expeditions. However, a small proportion of subjects did things that were not recommended, such as reducing the dose and frequency of taking ARV, borrowing ARV from friends, and even deciding to stop taking the drugs until the pandemic was over. These methods will cause resistance, which will lead to treatment failure. It can be concluded that the ART adherence of PLWH in this study is considerably high. This high adherence can be explained by an increased engagement in healthy behavior, which has been prompted by a high-risk perception of COVID-19, using the health belief model.23 Furthermore, it has been suggested that ARV may be effective against SARS-CoV-216,23,24,25 and this information may also be known by the PLWH yielding an improvement in their compliance. The belief that ARV is a cure for COVID-19 can be seen in this study—the bivariate analysis of the use of LPV/r was significantly associated with the absence of fear of being infected with COVID-19.
The concern of the subjects about the depletion of ARV stocks (60%) needs to be addressed by the clinic manager through the provision of sound information regarding the stock of ARV. This thought may arise because ARV in Indonesia is provided free of charge, but the handling of COVID-19 has depleted large amounts of money from the government budget.
Around 55% of the subjects had received pneumococcal and influenza vaccinations. This is important to note as a study in Brazil showed that COVID-19 patients with a history of influenza vaccination were not likely to have severe clinical conditions when they were infected.26 A similar analogy has been applied to a history of pneumococcal vaccination. These two vaccines will reduce the number of patients being treated for respiratory problems and, in a state of COVID-19 pandemic, facilities for the treatment of respiratory diseases can be maximized if influenza and pneumococcal morbidity rates are reduced.27
There are several limitations to this study. Some of the data were collected online and therefore only represents those with access to the internet. Because this study did not include a healthy control group, it is impossible to distinguish between healthy people and PLWH in some non-HIV-related characteristics, such as economic status. The study also had self-reporting bias. Face-to-face interviews may be able to decrease answer falsification, however during an outbreak, online surveys are safer for the subjects and provide the chance to access a large sample of a specific stigmatized population, such as PLWH.
Conclusion
This COVID-19 pandemic is still ongoing and many PLWH are still experiencing difficulties in continuing their treatment. Our results fill gaps on data about the knowledge, attitude, behavior, and socioeconomic conditions of people living with HIV in Indonesia during the COVID-19 pandemic. As we discussed in our study, future policies and interventions should take into account the socioeconomic conditions and misunderstandings that PLWH confront in order to assist them in continuing their treatment and improving retention in care.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Almuttaqi AI. Kekacauan Respons terhadap COVID-19 di Indonesia. THC Insights [Internet]; 2020. Available from: https://www.habibiecenter.or.id/img/publication/66f28c42de71fefe1c6fcdee37a5c1a6.pdf.
2. COVID-19 SP. Peta Sebaran | Satgas Penanganan COVID-19 [Internet]. November 17, 2021. Available from: https://covid19.go.id/peta-sebaran.
3. World Health Organization. Coronavirus disease (COVID-19): HIV and antiretrovirals [Internet]. Coronavirus disease (COVID-19): HIV and antiretrovirals. 2020. Available from: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-hiv-and-antiretrovirals.
4. Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi:10.1056/NEJMoa2002032
5. Cooper TJ, Woodward BL, Alom S, Harky A. Coronavirus disease 2019 (COVID-19) outcomes in HIV/AIDS patients: a systematic review. HIV Med. 2020;21:567–577. doi:10.1111/hiv.12911
6. Zhu F, Cao Y, Xu S, Zhou M. Co-infection of SARS-CoV-2 and HIV in a patient in Wuhan city, China. J Med Virol. 2020;92::529–530. doi:10.1002/jmv.25732
7. Kuman Tunçel Ö, Pullukçu H, Erdem H, Kurtaran B, Taşbakan S, Taşbakan M. COVID-19 related anxiety in people living with HIV: an online cross-sectional study. Turk J Med Sci. 2020;50:1792–1800. doi:10.3906/sag-2006-140
8. Blanco JL, Ambrosioni J, Garcia F, et al. COVID-19 in patients with HIV: clinical case series. Lancet HIV. 2020;7:e314–e316. doi:10.1016/S2352-3018(20)30111-9
9. Altuntas Aydin O, Kumbasar Karaosmanoglu H, Kart Yasar K. HIV/SARS-CoV-2 coinfected patients in Istanbul, Turkey. J Med Virol. 2020;92:2288–2290. doi:10.1002/jmv.25955
10. Vizcarra P, Pérez-Elías MJ, Quereda C, et al. Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort. Lancet HIV. 2020;7:e554–e564. doi:10.1016/S2352-3018(20)30164-8
11. Tarigan YN, Woodman RJ, Miller ER, Wisaksana R, Ward PR. Impact of strategic use of antiretroviral therapy intervention to the HIV continuum of care in 13 cities in Indonesia: an interrupted time series analysis. AIDS Res Ther. 2021;18:22. doi:10.1186/s12981-021-00340-4
12. Sub Directorate of HIV-AIDS and STI M of H. National action plan for HIV-AIDS control year 2015–2019 (in Bahasa Indonesia). Ministry of Health (ID); 2015.
13. Prabhu S, Poongulali S, Kumarasamy N. Impact of COVID-19 on people living with HIV: a review. J Virus Erad. 2020;6:100019. doi:10.1016/j.jve.2020.100019
14. Kemenko PMK RI. Pembatasan Sosial Berskala Besar | kementerian Koordinator Bidang Pembangunan Manusia dan Kebudayaan [Internet]. 2020. Available from: https://www.kemenkopmk.go.id/pembatasan-sosial-berskala-besar.
15. Ballivian J, Alcaide ML, Cecchini D, Jones DL, Abbamonte JM, Cassetti I. Impact of COVID–19-related stress and lockdown on mental health among people living with HIV in Argentina. J Acquir Immune Defic Syndr. 2020;85:475–482.
16. Horby PW, Mafham M, Bell JL, et al. Lopinavir–ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2020;396:1345–1352. doi:10.1016/S0140-6736(20)32013-4
17. World Health Organization. WHO: access to HIV medicines severely impacted by COVID-19 as AIDS response stalls [Internet]. 2020. Available from: https://www.who.int/news/item/06-07-2020-who-access-to-hiv-medicines-severely-impacted-by-covid-19-as-aids-response-stalls.
18. Lagat H, Sharma M, Kariithi E, et al. Impact of the COVID-19 pandemic on HIV testing and assisted partner notification services, Western Kenya. AIDS Behav. 2020;24:3010–3013. doi:10.1007/s10461-020-02938-7
19. Siewe Fodjo JN, de Moura Villela EF, Van Hees S, et al. Impact of the COVID-19 pandemic on the medical follow-up and psychosocial well-being of people living with HIV: a cross-sectional survey. J Acquir Immune Defic Syndr. 2020;85:257–262.
20. Raharjo DB, Muflih FF. Sah! UMP DKI Jakarta 2020 Naik Jadi Rp 4,2 Juta [Internet]. suara.com. 2019. Available from: https://www.suara.com/news/2019/11/01/161344/sah-ump-dki-jakarta-2020-naik-jadi-rp-42-juta.
21. Indonesian Ministry of Health. HIV-AIDS health service protocol during COVID-19 pandemic (in Bahasa Indonesia) [Internet]; 2020. Available from: https://infeksiemerging.kemkes.go.id/download/Protokol_Pelaksanaan_Layanan_HIV_AIDS_selama_pandemi_covid_19.pdf.
22. Stephenson R, Chavanduka TMD, Rosso MT, et al. Sex in the time of COVID-19: results of an online survey of gay, bisexual and other men who have sex with men’s experience of sex and HIV prevention during the US COVID-19 epidemic. AIDS Behav. 2020. doi:10.1007/s10461-020-03024-8
23. Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br J Health Psychol. 2014;19:592–605. doi:10.1111/bjhp.12058
24. Klement-Frutos E, Burrel S, Peytavin G, et al. Early administration of ritonavir-boosted lopinavir could prevent severe COVID-19. J Infect. 2020. doi:10.1016/j.jinf.2020.05.039
25. Del Amo J, Polo R, Moreno S, et al. Incidence and severity of COVID-19 in HIV-positive persons receiving antiretroviral therapy. Ann Intern Med. 2020;173:536–541. doi:10.7326/M20-3689
26. Fink G, Orlova-Fink N, Schindler T, et al. Inactivated trivalent influenza vaccination is associated with lower mortality among patients with COVID-19 in Brazil. BMJ Evid Based Med. 2020. doi:10.1136/bmjebm-2020-111549
27. Mendelson M. Could enhanced influenza and pneumococcal vaccination programs help limit the potential damage from SARS-CoV-2 to fragile health systems of southern hemisphere countries this winter? Int J Infect Dis. 2020;94:32–33. doi:10.1016/j.ijid.2020.03.030
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
