Back to Journals » International Journal of Women's Health » Volume 12
Knowledge, Attitude, and Practice on Cervical Cancer Screening and Associated Factors Among Women Aged 15–49 Years in Adigrat Town, Northern Ethiopia, 2019: A Community-Based Cross-Sectional Study
Authors Tsegay A , Araya T , Amare K, G/tsadik F
Received 26 May 2020
Accepted for publication 29 October 2020
Published 5 January 2021 Volume 2020:12 Pages 1283—1298
DOI https://doi.org/10.2147/IJWH.S261204
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Abreha Tsegay,1 Tesfalem Araya,1 Kahsay Amare,2 Fisseha G/tsadik2
1Department of Psychiatry, College of Health Science, Mekelle University, Mekelle, Tigray, Ethiopia; 2Department of Public Health, College of Health Science, Adigrat University, Adigrat, Tigray, Ethiopia
Correspondence: Abreha Tsegay Email [email protected]
Background: Cervical cancer, mainly attributed to persistent infection with a high-risk oncogenic human papillomavirus (HPV), is one of the most common types of women’s cancer globally, with more than 90% of new cases occurring in developing and resource-limited countries. In Ethiopia, cervical cancer ranks as the most frequent cancer among women and cause for 4732 deaths annually.
Objective: To assess knowledge, attitude, practice towards screening on cervical cancer and associated factors among women aged 15– 49 years in Adigrat town, northern Tigray Ethiopia.
Methods: A community based quantitative study design was conducted among 617 samples in Adigrat town, northern Tigray Ethiopia. Data were collected using a structured, semi-structured, and pre-tested questionnaire. Associations between dependent and independent variables were tested using logistic regression with the assumptions of p-values < 0.05 and confidence interval 95% and considered to be statistically significant.
Results: This study indicated that 46.4%, 53.3%, 38.1% of participants had knowledge, positive attitude, and screened on cervical cancer, respectively. Diploma and above [AOR=3.7, 95% CI (1.443, 9.433) were significant factors associated with knowledge of cervical cancer screening utilization. Primary school (1– 8) [AOR=2.7, 95% CI (1.297, 5.699)], greater than 500 ETB household income [AOR = 4.8, 95% CI (2.783, 8.577)] were significant factors associated with attitude of cervical cancer screening utilization. Secondary school (9– 12) [AOR = 3.4, 95% CI (1.565, 7.458)], not knowledgeable of cervical cancer [AOR = 1.8, 95% CI (1.156, 2.698)] were significant factors associated with practice of cervical cancer screening utilization.
Conclusion: Factors like age, educational status, anyone knowing with cervical cancer and ever received cancer information had a significant association with knowledge of cervical cancer screening utilization. Educational status and perceived income of the household had a significant association with an attitude of cervical cancer screening utilization. Educational status perceived income of the household, anyone knowing with cervical cancer, ever received cancer information, and knowledge of cervical cancer screening utilization were predictors of cervical cancer screening practice.
Keywords: cancer, knowledge, attitude, practice, screening, Ethiopia
Background
Cancer of the cervix, mainly attributed to persistent infection with a high-risk oncogenic Human papilloma-virus (HPV), is one of the most common types of women’s cancer globally, with more than 90% of new cases occurring in developing and resource-limited countries.1–3
It is also associated with a higher rate of mortality with over 150,000 global mortality reported only in 2012, of which 87% of death occurred in developing countries.1,2 Cervical cancer is the second most common malignancy and accounts for the greatest number of deaths from cancer in women worldwide.4
It causes 530,000 new cases and 280,000 deaths annually in adult women, of which 88% occur in low-income countries where access to pre-cancer screening and treatment is limited.5,6 The incidence and mortality in sub-Saharan Africa are among the highest in the world and accounts for over 70% of the global cervical cancer burden with 70,000 new cases annually.7,8
In Ethiopia, cervical cancer ranks as the most frequent cancer among women and cause for 4732 deaths annually.9–11 Among the general population, ~33.6% of women are estimated to harbor cervical human papillomavirus (HPV) infection at a given time.12,13
In many low-income countries, it was the most common female cancer, there were 572,624 new cases of cervical cancer and there were an estimated 265,672 deaths from cervical cancer worldwide accounting for 7.5% of all female cancer deaths. Mortality from cervical cancer varies 18-fold between the different regions of the world with about 87% of cervical cancer deaths occurring in the less developed regions.5
Currently, it is seen that the countries with the highest burden of cervical cancer are those not able to implement HPV vaccination due to its high costs and also effective screening practices due to lack of infrastructure, expertise, and so on.6
Cervical cancer is disproportionately high in developing countries, amounting to 86% and 88% of worldwide cases and deaths respectively.9 Besides, when cervical cancer is detected, women in developing countries often present with an advanced case that is not treatable.8 Overall, a proportional prevalence rate of cervical cancer was 52%, and cervical cancer was responsible for 275,000 deaths in 2008, about 88% of which occur in developing countries: 53,000 in Africa, 31,700 in Latin America and the Caribbean, and 159.800 in Asia.14
In Ethiopia, according to population-based cancer registry result from Addis Ababa, cervical cancer ranks as the second in its incidence among women and cause of 4732 deaths annually.15–18 Among the general population, 33.6% of women are estimated to harbor cervical human papillomavirus (HPV) infection at a given time.19,20
A study conducted in Finote Selam town, northwest Ethiopia, Nearly one third, 30.3% of the women knew about cervical cancer, and 58.1% had a favorable attitude towards cervical cancer screening.21
In the study conducted in Hossana Town, Hadiya zone, Southern Ethiopia, the proportion of health-seeking behavior for cervical cancer among the study participants was only 83 (14.2%). Of which, 76 (91.6%), of the participants who showed health-seeking behavior did so because other people recommended the service for them before the survey.22 In another study conducted in North West, Ethiopia 495 (78.7%), of them had heard about cervical cancer, and only 195 (31%) of them were knowledgeable about the disease.23
Despite this fact, very few women receive cervical cancer screening services in Ethiopia.15–17,23
Cervical cancer screening has been consistently shown to be effective in reducing the incidence rate or the occurrence of new cervical cancer cases and mortality from cervical cancer.20
Perhaps, cervical cancer screening facilities are limited because of poor infrastructure, staff, poor knowledge about cervical cancer, and illiteracy; the uptake of cervical cancer screening is poor among women who live in the places where the screening facilities are available.15–18,20,23–27
Challenges of cervical cancer screening in developing countries include limited access to health services and laboratories, no screening programs, limited or nonexistent awareness among populations and health workers, and poor referral and follow up.20,23,27–29
Despite the decreasing number of cervical cancer cases in Ethiopia, still, there is low knowledge about cervical cancer and poor attitude towards its screening. Programs targeting on increasing the knowledge and screening practice of women are crucial. Information about the level of knowledge, the risk factors, and screening behavior of the study subjects is paramount to provide targeted intervention. However, Information about knowledge and attitude towards screening of cervical cancer is limited in the country; particularly the study area. Thus, the findings from this study will provide the necessary information to fill this gap particularly for the primary care system strengthening to tackle this growing public health problem.
The study was moreover, helps policymakers and programmers to strengthen the existing screening programs in the country to improve the lives of the women by providing information about the level of knowledge, attitude, and practice on cervical cancer screening. Besides, the study gave insight and serve as baseline data for researchers and planning of another intervention plan like; health education and promotion regarding cervical cancer care activities.
Methods
Study Area
This study was conducted at Adigrat town which is located at 115 Km of the capital city of Tigray, and 889 Km far from Addis Ababa. Adigrat town has a total population of 97, 742 of whom 46,121 are male, 51,621 female, and 22,872 reproductive age women (15–49) years respectively. The town has with latitude of: 142,769 (1416ʹ36.840”N), longitude: 39, 4608 (3927ʹ38.880”E) and altitude: 2421m. According to 2011/2018 woreda health office information, Adigrat town has six kebeles (smallest administrative units) and several small ‘ketena, s with 22,214 numbers of households in the town. The town has one public General hospital, two health centers, and four private clinics.30
Study Design and Period
A community-based cross-sectional study was conducted from February 28 to June 30, 2019.
Source Population
The source population was all women aged 15–49 years living in Adigrat town.
Study Population
The study population was all women aged 15–49 years living in Adigrat town randomly selected kebeles.
Eligibility Criteria
Inclusion Criteria
All women aged 15–49 years living in Adigrat town at least for six months.
Exclusion Criteria
Women aged 15–49 years living in Adigrat town, which was too ill or not consenting to participate will be exempted from the study.
Sampling Technique and Sample Size Determination
The sample required for the study was conducted using a formula for a single population proportion with the prevalence of knowledge about cervical cancer screening 30.3%, and attitude towards screening of cervical cancer 58.1%,21 with 95% confidence interval, and 5% margin of error. Since the highest proportion was the attitude towards screening cervical cancer, taking prevalence of 58.1%, the required sample size was 374. After adding a 10% non-response rate and multiplying with a design effect of 1.5, then the final sample size was 617.
A multi-stage sampling technique was used. From the six kebeles, three kebeles were selected using a simple random sampling technique, the three randomly selected kebeles contains 11,698 households and 12,045 women (15–49) years. Finally, the households selected using a systematic random sampling technique by taking every 3rd household interval. In cases where there is more than one eligible women (15–49) year in the same house, a lottery method was applied to pick one woman. The number of eligible reproductive women (15–49) years from each study kebeles was selected based on proportional allocation to sample size (Figure 1).
 |
Figure 1 Schematic presentation of the sampling procedure of this study. Abbreviation: HH, household. |
Data Collection Instrument
A structured and pre-tested questionnaire was used for data collection. The questionnaire was first prepared in English and then translated into Tigrigna and back-translated into English by different qualified individuals to check the consistency. The training was given for data collectors and supervisors. Women were interviewed by six trained midwifery/nurses that deliver reproductive health service at the time of data collection, data collectors using face to face interview technique. Besides, trained supervisors who have a master of public health (MPH) level professionals and principal investigators were supervised the work.
Study Variables
Dependent Variable
- Knowledge of cervical cancer screening.
- Attitude towards its cervical cancer screening.
- Practice towards its cervical cancer screening.
Independent Variables
- Socio-demographic status: age, educational status, occupation, religion, family perceived income status, marital status, ethnicity, number of children.
- Reproductive history includes parity, age at the start of sexual intercourse, age at marriage, previous screened cervical cancer, time since last screening, result of the last screen for cervical cancer, ever history of pelvic infection, ever history of the sexually transmitted disease (STD), ever history of STD in sexual partner, ever human immunodeficiency virus (HIV) test, HIV status, history of abortion, multiple sexual partners, cause of cervical cancer, symptoms, treatment options, prevention method, reasons for not being screened and oral contraceptive use.
- Other factors are included knowing someone with cervical cancer, source of information about cervical cancer, knowledge of cervical cancer, ever history of smoke.
Operational Definition
Cervix: an opening of the uterus.
Cancer screening: a procedure that is performed to identify the presence of an abnormal cell in a particular tissue.
Knowledgeable of cervical cancer screening: those respondents who were scored mean and the above mean of the cervical cancer screening knowledge assessing questions.
Not knowledgeable of cervical cancer screening: those respondents who scored below the mean of the cervical cancer screening knowledge assessing questions.
Attitude: opinion, way of thinking behavior reflecting about cervical cancer screening.
Attitude: will be assessed by questions on Likert’s scale. And the mean score was calculated to use as a cut point.
Positive attitude: refers to for those scored the mean and above mean.
Negative attitude: refers to those scored below the mean.
Practice: those respondents who screen for cervical cancer at least once.
Not practice: those respondents who screen for cervical cancer at more than once.
Data Collection Tools and Procedures
A structured and pre-tested questionnaire was used for data collection. The questionnaire was first prepared in English and then translated into Tigrigna and back-translated into English by different qualified individuals to check the consistency. The training was given for data collectors and supervisors. Women were interviewed by six trained midwiferies/nurses that deliver reproductive health service at the time of data collection, data collectors using face to face interview technique. Also, trained supervisors who have MPH level professionals and principal investigators were supervised the work.
Data Collection Tools and Quality Controls
To achieve good data quality:
- The questionnaire was prepared in English and translated into Tigrigna and back-translated to English to keep the consistency of the data.
- A structured questionnaire that is adapted from different literature is used.
- The training was provided to the selected data collectors and supervisors for three days about the objective and process of data collection, including pre-testing. If there were problems in the questionnaire explanation was provided.
- Pre-testing was done with 5% of the questionnaires, in a similar area that is not included in the study.
Data Analysis
- The collected data were entered, edited, and cleaned in Microsoft excel window 2007 and then it was exported to STATA Version 11 for analysis. After the data is preprocessed then descriptive statistics of the study variables were presented using frequencies and percentages for the categorical variables. The presence of an association between knowledge of cervical cancer, attitude, and practice to its screening and the independent variables was tested using cross-tabulation with the chi-square test at P-value < 0.05 significance level.
- As the dependent variable cervical cancer is with two categories, binary logistic regression analysis was used. In the bivariate logistic regression, the level of significance of the association between the dependent and each independent variable was considered at P-value < 0.05, and the factors with this level of significance were made to pass on to the next level of analysis. In the multivariable logistic regression analysis, the Stepwise forward predictor inclusion method was used to develop the main-effect model for the dependent variable cervical cancer. The presence and significance of interaction terms and confounding effects on the main effect model were checked using the Log-likelihood ratio test and the percentage change in beta values of the independent variables.
- Multi-collinearity between independent variables also checked using variance inflation factors considering multi-co linearity at variance inflation factor (VIF) >10. The presence and influence of outliers were checked using residuals cooks distance and influence statistic. A comparison between models was made using the log-likelihood ratio test. The goodness of fit of the model was checked using the Hosmer Lemeshow test of goodness of fit. The proportion of correctly classified observations was checked using the classification table, and the prediction power of the model was checked using the area under the receiver operating characteristics (ROC) curve.
Ethical Consideration
Ethical approval was obtained from the ethical review committee of Adigrat University and the Tigray Regional Health Bureau, which was confirmed to the principles embodied in the Declaration of Helsinki. Official permission was also obtained from the principals of the health facilities before approaching the study participants. The objective and purpose of the study were clearly explained to the study subjects to obtain written informed consent before data collection. Participants were also informed that they can discontinue or decline to participate in the study at any time. Confidentiality of the information was maintained and the data were recorded anonymously throughout the study.
Dissemination of Study Findings
The findings will present to Adigrat University and Tigray Regional Health Bureau (TRHB). The result will be disseminated and communicated to relevant bodies including the study town health office, in addition to this TRHB and different related organizations. The result will be presented in different related seminars or workshops, and in the end, after a lot of effort will be sending for the publication.
Expected Outputs
-Knowledge of cervical cancer was assessed.
-Attitude towards its screening cervical cancer was identified.
-Practice towards its screening of cervical cancer was identified.
-Factors of cervical cancer were assessed.
-The result was announced to concerned governmental and non-governmental organizations working on maternal health care particularly cervical cancer.
Result
Socio-Demographic Characteristics of the Study Subjects
A total of 612 women participated in the study with a response rate of 99.2%. The age distribution of the respondents showed that 274 (44.8%) and 232 (37.9%) were Less than 29 years and 29 up to 39 years of age respectively. The mean age of participants was 31.3±8.0 SD years, with a minimum of 15 and a maximum of 49 years. About 541 (88.4%) of the study subjects were orthodox Christian followers, 41 (6.7%) were catholic and 30 (4.9%) Muslim. More than half of the study subjects were 376 (61.4%) married and 236 (38.6%) were single.
Concerning their educational status 243 (39.7%) and were secondary schooling whereas 203 (33.2%) were primary schooling and 117 (19.1%) college diploma and above. More than half of the study participants 365 (59.6%) and 247 (40.4%) were unemployed and employed respectively. More than half of the study subjects have household monthly income of less than 200 and Greater than 500 Ethiopian birr were 99 (16.2) and 459 (75.0%) (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Reproductive Age (15–49) Years Women on Cervical Cancer in Adigrat Town Eastern Zone, Tigray, Ethiopia, November 2019 |
Knowledge of Cervical Cancer Screening Utilization Service
More than half of the respondents have heard about cancer and cervical cancer screening 487 (79.6%) and 432 (70.6%) respectively. Having multiple sexual partners 373 (37.3%), sexual transmitted disease 237 (38.7%), early age marriage 195 (31.9%), prolonged oral contraceptive use 118 (19.3% and early sexual intercourse 99 (15.8%) were risk factors of cervical cancer mentioned by the respondents. About signs and symptoms of cervical cancer mentioned by the respondents were; vulvar itching or burning sensation 306 (50.0%), abnormal vaginal discharge 156 (25.5%), bleeding or pain after sexual intercourse 153 (25.0%), pelvic/back or leg pain 130 (21.2%), excessive vaginal discharge 105 (17.2%) and post-menopausal bleeding 103 (16.8%). Concerning the prevention of cervical cancer were cervical cancer screening 273 (44.6%), reduce the number of sexual partners 340 (55.6%), being faithful to partner 221 (36.1%). Regarding treatment; the respondents mentioned radiation therapy 98 (16.0%), surgery 73 (11.9%), chemotherapy 191 (31.2%) and do not know 328 (53.6%) respectively as treatment options.
The overall knowledge of respondents 284 (46.4%) and 328 (53.6%) were knowledgeable and not knowledgeable about cervical cancer screening utilization service respectively (Table 2). The frequency of cervical cancer screening; more than half and once every year were 68.14% and 21.08% respectively (Figure 2). Source of information about cervical cancer screening; the figure below depicts from media and health workers were 347 (56.7%) and 246 (40.3%) respectively (Figure 3).
 |
 |
 |
Table 2 Knowledge of Respondents About Risk Factors, Signs and Symptoms, and Methods of Prevention and Treatment of Cervical Cancer in Adigrat Town, Eastern, Tigray, Ethiopia, November 2019 |
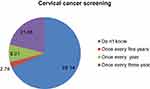 |
Figure 2 Frequency of cervical cancer screening among 15–49 years in Adigrat town, Eastern zonal Tigray, Ethiopia, 2019. |
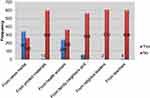 |
Figure 3 Source of information about cervical cancer screening on women 15–49 years in Adigrat Town Eastern zone Tigray, Ethiopia, 2019. |
The Attitude of Cervical Cancer Screening Utilization Service
Of the respondents, 225 (36.8%) due to a healthy, screening of cervical cancer was not agreed upon. About 334 (54.6%) and 398 (65.0%) of participants’ HPV infection and HIV/AIDS were agreed on the major risk factor for the development of cervical cancer respectively. Using birth control pills for a long time and any reproductive age woman 205 (33.5%) and 254 (41.5%) were susceptible to develop cervical cancer. Cervical cancer can be severe and may be hazardous and precancerous cervical cancer screening may be beneficial 559 (91.3%) and 565 (92.3%) were agreed. In general 326 (53.3%) of the respondents have a positive attitude towards screening for cervical cancer, while the rest 286 (46.7%) have a negative attitude towards screening for cervical cancer (Table 3).
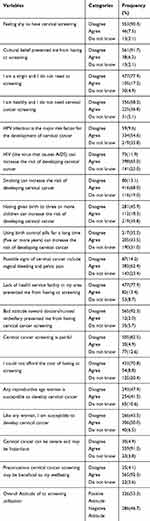 |
Table 3 Attitude of Respondents on Cervical Cancer Screening Utilization in Adigrat Town, Eastern, Tigray, Ethiopia, November 2019 |
The Practice of Cervical Cancer Screening Utilization Service
The practice of respondents towards screening for cervical cancer from the total study population was only 233 (38.1%) have been screened for Cervical Cancer. The rest had not been screened.
Concerning reproductive health screening such as HIV/STI 471 (77.0%) was screened and 64 (10.5%) screened for cancer of the cervix. Women 25 and above years 317 (51.8%) and prostitute women 195 (31.9%) were screened for cervical cancer. About 466 (76.1%) respondents were willing to be screened shortly (Table 4).
 |
Table 4 Respondents on Cervical Cancer Screening Practice in Adigrat Town, Eastern, Tigray, Ethiopia, November 2019 |
Factors Associated with Women’s Reproductive Age (15–49) Years Knowledge on Cervical Cancer Screening
The bivariate analysis showed that variables, such as age, religion, education, occupation, and household family size, monthly perceived income, knowing anyone who had cervical cancer, family history of cervical cancer, and ever heard about cancer were significantly associated with the knowledge score of cervical cancer screening at P-value of less than 0.05.
In the multivariable analysis, age, educational status, knowing someone with cervical cancer, and ever received cancer information remained a significant association with the screening of cervical cancer. Participants with the age of greater than 40 years were about 60%, (AOR = 0.4, 95% CI: 0.204, 0.704) to be knowledgeable on cervical cancer screening compared with less than 29 years when controlling the other variables, respondents who attended diploma and above school were nearly four times (AOR = 3.7, 95% CI: 1.443, 9.433) more likely to be knowledgeable on cervical cancer screening than those who are illiterate with controlling the other variables.
Respondents knowing anyone who had cervical cancer were about to 86%, (AOR = 0.14, 95% CI: 0.065, 0.304) to be knowledgeable on cervical cancer screening than those who did not know anyone with cervical cancer controlling the other variables. In the present study, women who had ever received cancer information were 60%, (AOR = 0.4, 95% CI: 0.233, 0.593) knowledgeable on cervical cancer screening than those who did not ever receive cancer information when controlling the other variables (Table 5).
 |
Table 5 The Association Between Knowledge of Cervical Cancer Screening Utilization with Different Variables of Women 15–49 Years Age, Adigrat Town, Tigray Regional State Eastern Zone, 2019 |
Factors Associated with Women’s Reproductive Age (15–49) Years Attitude on Cervical Cancer Screening
According to the bivariate analysis, the educational status of respondents, willing to screen near the future, and perceived household monthly income was significantly associated with attitude to cervical cancer screening at a P-value of less than 0.05. In the multivariable analysis, three variables, such as educational status and perceived household monthly income became significant with the attitude towards cervical cancer screening at a P-value of less than 0.05. Participants who attended primary, secondary and diploma and above schooling were 2.7, 2.6 and 2.9 times [(AOR = 2.7,95% CI:1.29,5.9), AOR = 2.6,95% CI: 1.25,5.45) and AOR = 2.9,95% CI:1.32,6.49)] more likely to have a positive attitude towards cervical cancer screening utilization than those who are illiterate in education when controlling the other variables and participants perceived monthly income 200 up to 500 ET and greater than 500 ETB were five and four times [(AOR = 5, 95% CI:2.51,11.47) and (AOR= 4.8, 95% CI: 2.78,8.58)] more likely to have a positive attitude towards cervical cancer screening utilization comparing with respondents have monthly income less than 200 ETB when controlling the other variables (Table 6).
 |
Table 6 The Association Between the Attitude of Cervical Cancer Screening Utilization with Different Variables of Women 15–49 Years Age, Adigrat Town, Tigray Regional State Eastern Zone, 2019 |
Factors Associated with Women’s Reproductive Age (15–49) Years Practiced on Cervical Cancer Screening
According to the bivariate analysis, educational status of respondents, occupational status of respondents, perceived household monthly income, knowing anyone with cervical cancer, family history of cervical cancer, ever received information about cervical cancer screening, and knowledge of cervical cancer screening utilization were significantly associated with screened practice to cervical cancer screening at P-value of less than 0.05. In the multivariable analysis, five variables, such as educational status, perceived household monthly income, knowing anyone with cervical cancer, ever received information about cervical cancer screening, and knowledge of cervical cancer screening became significant with practice towards cervical cancer screening at a P-value of less than 0.05.
Participants who attended primary, secondary and diploma and above schooling were 5, 4 and 3 times [(AOR = 4.9, 95% CI: 2.24, 10.89), AOR = 3.4, 95% CI: 1.57, 7.46) and AOR = 3.2, 95% CI: 1.34, 7.61)] more likely to have a practiced towards cervical cancer screening utilization than those who are illiterate in education when controlling the other variables. Regarding perceived household monthly income 200 up to 500 ETB and greater than 500 ETB were two times [(AOR = 2.3, 95% CI: 1.09,5.04) and (AOR= 2.2, 95% CI: 1.37, 3.60)] more likely to have a practiced towards cervical cancer screening utilization comparing with respondents have monthly income less than 200 ETB controlling the other variables. Respondents not knowing anyone with cervical cancer and not ever received information about cervical cancer screening were 60% [(AOR = 0.4, 95% CI: 0.17, 0.75), (0.4, 95% CI: 0.24, 0.68)] less likely to have a practiced towards cervical cancer screening utilization comparing with respondents knowing anyone with cervical cancer and ever received information about cervical cancer screening when controlling the other variables. Concerning knowledge of cervical cancer screening utilization respondents being knowledgeable almost two times (AOR = 1.8, 95% CI: 1.16, 2.69) more likely to have a practice towards cervical cancer screening utilization comparing with respondents not knowledgeable when controlling the other variables (Table 7).
 |
Table 7 The Association Between the Practice of Cervical Cancer Screening Utilization with Different Variables of Women 15–49 Years Age, Adigrat Town, Tigray Regional State Eastern Zone, 2019 |
Discussion
Knowledge of cervical cancer screening, attitude towards its screening, and practice of screening are essential for the prevention of the disease cervical cancer.
The current study was conducted to determine women’s (15–49 years) knowledge, attitude, and practice towards cervical cancer screening and associated factors.
The current study indicated that 46.4%, 53.3%, 38.1%, of participants had knowledge, a positive attitude, and screened on cervical cancer respectively. The current study showed that knowledge of study participants was 46.4%. This finding is higher than the findings were comparable with that of a community-based study conducted in Finote Selam town, in Gondar, reported from Addis Ababa, in North West Ethiopia and female students of Mizan Tepi University, Ethiopia, 30.3%, 31%, 25%, 31%, 33.97% respectively.21,23,31,32 The possible reason for the difference might be that the sample sizes, study period, determine knowledge in the previous study. However, our result is lower than the finding study conducted in Addis Ababa Ethiopia and Uganda, which noted 64.8%, and 55%.33,34 The possible reason for the difference from the study done in Uganda and Addis Ababa could be the variation in educational status between the two study populations and study setting.
The current study revealed that ever received information about cervical cancer screening was 70.6%. This finding was higher than the findings study conducted in Mizan Tepi University, in Addis Ababa, Ethiopia, and Nigeria 53.11%, 66.7%, and 40.8%,32,33,35 but lower, when compared with the study done in Gondar, North West Ethiopia which was 78.7% and Ghana, Accra 93.0%.21,36 The discrepancy may be due to time variation, the differences of study setting, and sample size. Our study showed that 53.3% of the women had a favorable attitude towards cervical cancer screening. This result was better than that of a study done in Dessie Town, Ethiopia which documented 42.1%.37 The gap between our study and that of Dessie might be the high proportion of single (unmarried) participants in the Dessie study. There is evidence that single women have a less favorable attitude towards cervical cancer screening. However, the result is lower than the finding of a hospital-based study in India which reported 76%.38 The difference between our study community based and the study in India might be the study setting; hospitalized women might have high health-seeking behavior and better access to information. Our finding was lower than that of a study conducted among market women in Nigeria noted 80.4% had a favorable attitude towards cervical cancer screening.39 The difference might be that in the Nigerian study the participants were shop owners/attendants aged 15 years and above, most of them with higher educational status. The current study revealed that 53.3% had a favorable attitude towards cervical cancer screening This finding was consistent with the study conducted in Addis Ababa, Ethiopia and that Tanzania 50% and 56% of all participants had a favorable attitude towards cervical screening.33,40 Our finding was also lower than the study conducted in Finote Selam town and Mizan Tepi University, Ethiopia 58.1%, and 61.24% of the respondents had a favorable attitude towards cervical cancer screening for cervical cancer.21,32
The current study should that benefits of precancerous cervical cancer screening agreed that 92.3%. This finding was higher than the study conducted in Mizan Tepi University, Ethiopia, and Ghana 44.96% and 87%,32,36 whereas cervical cancer can be severe and harmful agreed that 91.3%. This is higher than the study conducted in Mizan Tepi University, Ethiopia 44.49%,32 and lack of susceptibility cervical carcinoma was 36.8%. This finding is lower than the study conducted in Ghana.36 The discrepancy may be due to time variation, the differences of study setting, study subjects, and sample size. The practice of the current respondents towards screening for cervical cancer was indicated that 38.1% have been screened. This finding is higher than those published in Mizan Tepi University14.83%, Addis Ababa 6.8%, Ethiopia, Tanzania 14%, and Kenya 22%,32,40–42 but the current study was lower than the study conducted in Kinshasa, the Democratic Republic Congo 67.9%.43 The difference might be that in time variation, study design, sample size, and cultural differences. Most of the respondents were not screened, 11.4% believe as they are healthy and 77.6% embarrassment to be screened. The current study of believes as they are healthy lower than the study conducted in Mizan Tepi University 36.84%, whereas 77.6% higher than the previous study 17.7%.32 The discrepancy may be due to time variation, the differences of study setting, study subjects, and sample size.
In the multivariate logistic regression test variables of respondent’s age, educational status, anyone knowing with cervical cancer and ever received cancer information had a significant association with knowledge of cervical cancer screening utilization; at the same time variables of respondent’s of educational status and perceived income of the household had a significant association with an attitude of cervical cancer screening utilization and respondent’s educational status, perceived income of the household, anyone knowing with cervical cancer, ever received information about cancer and knowledge of cervical cancer screening utilization were predictors of cervical cancer screening practice.
The present study identified that the participants with the age of 40 years were increased knowledge of cervical cancer screening utilization by 60% than 29 years. Studies conducted in Gondar,21 Democratic Republic of Congo Kinshasa,43 and in Mekelle zone44 had similar findings respondents were 2.2 and 7.6 and 1.8 times more likely to be knowledgeable on cervical cancer screening utilization. Our study revealed that women with an educational status diploma and above were 3.7 times more likely to be knowledgeable about cervical cancer screening. Studies conducted in Gondar, Democratic Republic of Congo Kinshasa, Finote Selam town, and Dessie town19,21,43,45 had similar findings, respondents, educational status with cervical cancer were 2.2,7.6,7.2 and 8.7 times more likely to be knowledgeable on cervical cancer screening utilization. Our study revealed that women who knew someone who had cervical cancer were increased screening utilization by 86% than did not know someone with cervical cancer; the previous study was done in Gondar and Bale Zone, Ethiopia21,46 were 4.9 and 3.4 times more likely to be knowledgeable on cervical cancer screening utilization than those women who do not know someone with cervical cancer and in the current study ever received information on cervical cancer screening was about 60% than those participants who not ever received information on cervical cancer screening. This is similar studies conducted in Gondar, in Hossana Town and20,21,46 were 8, 2.6, and 3.6 times more likely to be not knowledgeable on cervical cancer screening utilization than those who received information.
Regarding the attitude of participants on cervical cancer screening utilization, the current study showed educational status primary, secondary, and diploma and above were 2.7, 2.6 and 2.9 times more likely have a favorable attitude on cervical cancer screening utilization than those who participants have not favorable attitude. This is similar to studies conducted in Hossana Town, Hadiya zone, and in India20,38 were 7.6 and 15.3 times more likely have a favorable attitude on cervical cancer screening utilization and perceived monthly income of participants for those greater than 500 ETB was 4.8 times more likely have a favorable attitude on cervical cancer screening utilization than less than 200 ETB, this is a similar study conducted in India.38
Concerning the practice of participants on cervical cancer screening utilization, the current study revealed that educational status primary, secondary and diploma and above were 4.9, 3.4, and 3.2 times more likely have screened for cervical cancer than those who participants illiterate and perceived income 200 to 500 ETB were 2.3 and 2.2 times more likely have the experiences to uptake cervical cancer screening than perceived income less than 200 ETB. This was similar to studies conducted in India, in Addis Ababa and Arba Minch Town31,38,47 were 3.9, 3.2, and 3.6 times more likely have screened for cervical cancer. Participants who knew someone who had cervical cancer was increased screening utilization by 60% than did not know someone with cervical cancer; this was in line with the study conducted in Addis Ababa33 and the current study indicated that ever received information on cervical cancer screening was about 60% screened than those participants who did not ever receive information on cervical cancer screening; this is similar with the study conducted in Hadiya zone, south Ethiopia and Kenya were 4.5 and 6.6 times more likely those participants whoever received information on cervical cancer screening were screened.20,48
Regarding knowledge of cervical cancer for screened was 1.8 times more likely knowledgeable on screening cervical cancer than those participants not knowledgeable; the current study was in line with a study conducted in Mekelle Town, Hadiya Zone, South Ethiopia, and Northwest Ethiopia were 2.4,11 and 3.0 times more likely knowledgeable on screening cervical cancer practice than not knowledgeable.20,44,49
Conclusion
Factors like age, educational status, anyone knowing with cervical cancer and ever received cancer information had a significant association with knowledge of cervical cancer screening utilization. Educational status and perceived income of the household had a significant association with an attitude of cervical cancer screening utilization. Educational status perceived income of the household, anyone knowing with cervical cancer, ever received cancer information, and knowledge of cervical cancer screening utilization were predictors of cervical cancer screening practice.
Recommendation
Based on the findings here are encountered to recommends:
- TRHB and Adigrat zonal health bureau should work at large on women’s health especially those who are at their age are at the reproductive and have enough knowledge, attitude, and practice cervical screening before they become ill. Give short and long training hierarchically from regional to district health bureau.
Abbreviations
AIDS, acquired immunodeficiency virus; AOD, adjusted odds ratio; Cc, cervical cancer; COD, crude odds ratio; ETB, Ethiopian Birr; HH, household; HIV, human immunodeficiency virus; HPV, human papilloma-virus; MPH, master’s in public health; ROC, receiver operating characteristic; STD, sexually transmitted disease; STI, sexually transmitted infections; TRHB, Tigray Regional Health Bureau; VIF, variance inflation factor.
Data Sharing Statement
Data produced or analyzed during this study are included in this published paper. The datasets can be requested to the corresponding author.
Ethics Approval and Consent to Participate
Ethical clearance was permitted by the Ethical Review Board of Adigrat University, College of Medicine, and Health Sciences with the reference number of Notification of Expedited Approval ERC 1321/2019. Every precaution took to protect the privacy of research subjects and the confidentiality of their personal information. The data collector checked whether the study participants had a relationship or not. Participation by individuals capable of giving informed consent as subjects in this research were voluntary. Written informed consent was gotten from every participant for 18 years old and above whereas written informed consent was obtained from a parent or guardian for participants 15-17 years old. Participants capable of giving informed consent, each potential subject was adequately informed of the aims, methods, sources of funding, any possible conflicts of interest, and institutional affiliations of the researcher. The potential subject was informed of the right to refuse to participate in the study or to withdraw consent to participate at any time without reprisal. After ensuring that the potential subject understood the information, the data collector appropriately qualified individuals should seek the potential subject’s freely-given informed consent, preferably in writing. The collected data did not comprise identifying information, and the collected data were used for this study only.
Consent for Publication
Consent of publication for this research is Adigrat University, College of Medicine and Health Science, public health department, and participants.
Acknowledgments
The authors would like to acknowledge the Adigrat University College of Health Science for ethical approval. We also would like to thank our acknowledgment to data gatherers and the study participants because without them the whole part will be meaningless. Adigrat University has economically supported the process of data collection.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Not applicable to this section.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Integrated Africa Cancer Factsheet. Focusing on cervical cancer, Girls & Women Health, Sexual & Reproductive Health, HIV & Maternal Health. 2014.
2. WHO. International agency for research on cancer: latest world cancer statistics. 2013.
3. Zur Hausen H. Papillomaviruses in the causation of human cancers – a brief historical account. Virology. 2009;384:260–265. doi:10.1016/j.virol.2008.11.046
4. Louie KS, de Sanjose S, Mayaud P. Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: a comprehensive review. Trop Med Int Health. 2009;14:1287–1302. doi:10.1111/j.1365-3156.2009.02372.x
5. ICO Information Centre on HPV and Cancer, HPV Information Center. Human Papillomavirus and related diseases report. Worldwide. 2016
6. Bekele A, Baay M, Mekonnen Z, Suleman S, Chatterjee S. Human papillomavirus type distribution among women with cervical pathology – a study over 4 years at Jimma Hospital, southwest Ethiopia. Trop Med Int Health. 2010;15(8):890–893. doi:10.1111/j.1365-3156.2010.02552.x
7. Abate SA. Trends of cervical cancer in Ethiopia. Cervical Cancer. 2015;1(1):1–4.
8. Jemal A, Bray F, Forman D, et al. Cancer burden in Africa and opportunities for prevention. Cancer. 2012;118(18):4372–4384. doi:10.1002/cncr.27410
9. Human papillomavirus and related cancers, summary report update. Available from: http://screening.iarc.fr/doc/Human%20Papillomavirus%20and%20Related%20Cancers.pdf.
10. Goldie SJ, O’shea M, Campos NG, Diaz M, Sweet S, Kim SY. Health and economic outcomes of HPV 16, 18 vaccinations in 72 GAVI-eligible countries. Vaccine. 2008;26(32):4080–4093. doi:10.1016/j.vaccine.2008.04.053
11. Arbyn M, Castellsagué X, de Sanjosé S, et al. Worldwide burden of cervical cancer in 2008. Ann Oncol. 2011;22(12):2675–2686. doi:10.1093/annonc/mdr015
12. Denny LA, Anorlu R. Cervical cancer in Africa. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1434–1438. doi:10.1158/1055-9965.EPI-12-0334
13. Globocan. Cancer incidence, mortality, and prevalence worldwide. Int Agency Res Cancer. 2008.
14. Human papillomavirus and related cancers, summary report update. Available from: http://screening.iarc.fr/doc/Human%20Papillomavirus%20and%20Related%20Cancers.pdf.
15. Waktola EA, Mihret W, Bekele L. HPV and burden of cervical cancer in East Africa. Gynecol Oncol. 2005;99(Suppl 3):201–202. doi:10.1016/j.ygyno.2005.07.083
16. Kress CM, Sharling L, Owen-smith AA, Desalegn D, Blumberg HM, Goedken J. Knowledge, attitudes, and practices regarding cervical cancer and screening among Ethiopian health care workers. Int J Women’s Health. 2015;7:765–772.
17. Oche MO, Kaoje AU, Gana G, Ango JT. Cancer of the cervix and cervical screening: current knowledge, attitude, and practices of female health workers in Sokoto, Nigeria. Int J Med Med Sci. 2013;5(4):184–190.
18. McCarey C, Pirek D, Tebeu PM, Boulvain M, Doh AS, Petignat P. Awareness of HPV and cervical cancer prevention among Cameroonian health care workers. BMC Women’s Health. 2011;11:45. doi:10.1186/1472-6874-11-45
19. Geremew AB, Gelagay AA, Azale T. Comprehensive knowledge on cervical cancer, attitude towards its screening and associated factors among women aged 30–49 years in Finote Selam town, northwest Ethiopia. Reprod Health. 2018;15:29
20. Habtu Y, Yohannes S, Laelago T. Health seeking behavior and its determinants for cervical cancer among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: community based cross sectional study. BMC Cancer. 2018;18:298.
21. Getahun F, Mazengia F, Abuhay M, Birhanu Z. Comprehensive knowledge about cervical cancer is low among women in North West, Ethiopia. BMC Cancer. 2013;13:2. doi:10.1186/1471-2407-13-2
22. Gebreegziabher M, Asefa NG, Berhe S. Factors affecting the practices of cervical cancer screening among female nurses at public health institutions in Mekelle Town, Northern Ethiopia, 2014: a cross-sectional study. J Cancer Res. 2016;2016:7. doi:10.1155/2016/4743075
23. WHO, ICO. Human papillomavirus and related cancers in Ethiopia. In Summary report. 2009
24. Urasa M, Darj E. Knowledge of cervical cancer and screening practices of nurses at a regional hospital in Tanzania. Afri Health Sci. 2011;11(1):48–57.
25. Tran NT, Taylor R, Choe SI, Pyo HS, Kim OS, So HC. Knowledge, Attitude, and Practice (KAP) concerning cervical cancer and screening among rural and urban female healthcare practitioners in the Democratic People’s Republic of Korea. Asian Pac J Cancer Prev. 2011;12(11):3023–3028.
26. Tchounga BK, Jaquet A, Coffie PA, et al. Cervical cancer prevention in reproductive health services: knowledge, attitudes, and practices of midwives in Côte d’Ivoire, West Africa. BMC Health Serv Res. 2014;14:165. doi:10.1186/1472-6963-14-165
27. Rashied AM, Abbas IM. Barriers for up taking the Pap smear among nurse-midwives in Baghdad City Hospitals. Kufa J Nurs Sci. 2014;4(3):1–12.
28. Ben-Natan M, Adir O. Screening for cervical cancer among Israeli lesbian women. Int Nurs Rev. 2009;56(4):433–441. doi:10.1111/j.1466-7657.2009.00728.x
29. Hyacinth HI, Adekeye OA, Ibeh JN, Osoba T, Medeiros R. Cervical cancer, and Pap smear awareness and utilization of Pap smear test among federal civil servants in North Central Nigeria. PLoS One. 2012;7(10):e46583. doi:10.1371/journal.pone.0046583
30. Adigrat town health office. (2018). Eastern Zone Tigray Regional State, Ethiopia.
31. Belete N, Tsige Y, Mellie H. Willingness and acceptability of cervical cancer screening among women living with HIV/AIDS in Addis Ababa, Ethiopia: a cross-sectional study. Gynecol Oncol Res Prac. 2015;2:6. doi:10.1186/s40661-015-0012-3
32. Mulatu K, Motma A, Seid M, et al. Assessment of knowledge, attitude, and practice on cervical cancer screening among female students of Mizan Tepi University, Ethiopia, 2016. Cancer Biol Ther Oncol. 2017;1:1.
33. Eyerusalem Getachew: knowledge attitude and practice on cervical cancer and screening among reproductive health service clients, Addis Ababa, Ethiopia. 2015
34. Mukama T, Ndejjo R, Musabyimana A, Halage AA, Musoke D. Women’s knowledge and attitudes towards cervical cancer prevention: a cross -sectional study in eastern Uganda. BMC Women’s Health. 2017;17:9. doi:10.1186/s12905-017-0365-3
35. Wong LP, Wong YL, Low WY, Khoo EM, Shuib R. Knowledge and awareness of cervical cancer and screening among Malaysian women who have never had a Pap smear: a qualitative study. Singapore Med J. 2009;50:49–53.
36. Adanu RM. Cervical cancer knowledge and screening in Accra, Ghana. J Woman Health Gend Base Med. 2002;11:487–488. doi:10.1089/152460902760277822
37. Andargie A, Reddy PS. Knowledge, attitude, practice, and associated factors of cervical cancer screening among women in Dessie referral hospital and Dessie health center, Northeast Ethiopia. Glob J Res Anal. 2016;4.
38. Bansal AB, Pakhare AP, Kapoor N, Mehrotra R, Kokane AM. Knowledge, attitude, and practices related to cervical cancer among adult women: a hospital-based cross-sectional study. J Nat Sci Biol Med. 2015;6:324. doi:10.4103/0976-9668.159993
39. Ahmed SA, Sabitu K, Idris SH, Ahmed R. Knowledge, attitude, and practice of cervical cancer screening among market women in Zaria, Nigeria. Niger Med J. 2013;54:316. doi:10.4103/0300-1652.122337
40. John J. The Knowledge, Attitude, Practice and Perceived Barriers Towards Screening for Premalignant Cervical Lesions Among Women Age 18years and Above, in Songea Urban, Ruvuma. Tanzania: Muhimbili University of Health and Allied Sciences; 2011.
41. Gichangi P, Estamble B, Bwayo J, et al. Knowledge and practice about cervical cancer and Pap smear testing among patients at Kenyatta National Hospital. Int J Gynecol Cancer. 2003;13:827–833. doi:10.1111/j.1525-1438.2003.13612.x
42. Terefe Y, Gaym A. Knowledge, attitude and practice of screening for carcinoma of the cervix among reproductive health clients at three teaching hospitals. Ethiopian J Reprod Health. 2008;2(1).
43. Ali-Risasiet C, Mulumba P, Verdonck K, Vanden BD, Praet M. Knowledge, attitude, and practice about cancer of the uterine cervix among women living in Kinshasa, the Democratic Republic of Congo. BMC Women’s Health. 2014;14:30. doi:10.1186/1472-6874-14-30
44. Bayu H, Berhe Y, Mulat A, Alemu A, Grce M. Cervical cancer screening service uptake and associated factors among age eligible women in Mekelle Zone, Northern Ethiopia, 2015: a community based study using health belief model. PLoS One. 2016;11(3):e0149908. doi:10.1371/journal.pone.0149908
45. Mitiku I, Tefera F, Paraskevis D. Knowledge about cervical cancer and associated factors among 15–49-year-old women in Dessie Town, Northeast Ethiopia. PLoS One. 2016;11(9):e0163136. doi:10.1371/journal.pone.0163136
46. Tefera TB, Kerbo AA, Gonfa DB, Haile MT. Knowledge of cervical cancer and its associated factors among reproductive age women at robe and Goba towns, bale zone, Southeast Ethiopia. Global J Med. 2016;16(1).
47. Gebru Z, Gerbaba M, Dirar A. Utilization of cervical carcinoma screening service and associated factors among currently married women in Arba Minch Town, Southern Ethiopia. J Women’s Health Care. 2016;5:297. doi:10.4172/2167-0420.1000297
48. Nyangasi M, Nkonge NG, Gathitu E, et al. Predictors of cervical cancer screening among Kenyan women: results of a nested case-control study in a nationally representative survey. BMC Public Health. 2018;18(3):1221. doi:10.1186/s12889-018-6054-9
49. Erku DA, Netere AK, Mersha AG, Abebe SA, Mekuria AB, Belachew SA. Comprehensive knowledge and uptake of cervical cancer screening is low among women living with HIV/AIDS in Northwest Ethiopia. Gynecol Oncol Res Pract. 2017;4(1):20. doi:10.1186/s40661-017-0057-6
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
