Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 15
Kinetics of Plasma Cytokines During Two Different Modalities of Extracorporeal Blood Purification in the Critically Ill Covid 19 Patients: A Cohort Study
Authors Ponce D , Zamoner W , Magalhães LE, de Oliveira PGS, Polla P, Barbosa AN , Golim MA, Balbi AL Snr
Received 18 July 2022
Accepted for publication 20 October 2022
Published 2 November 2022 Volume 2022:15 Pages 309—317
DOI https://doi.org/10.2147/IJNRD.S382776
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Daniela Ponce,1 Welder Zamoner,1 Luis Eduardo Magalhães,1 Paula Gabriela Sousa de Oliveira,1 Patricia Polla,2 Alexandre Naime Barbosa,3 Marjorie de Assis Golim,2 André Luís Balbi Snr1
1Department of Internal Medicine, University Estadual Paulista (UNESP), Botucatu, São Paulo, Brazil; 2Clinical Hospital of Botucatu Medical School, Botucatu, São Paulo, Brazil; 3Department of Infectious Disease, University Estadual Paulista (UNESP), Botucatu, São Paulo, Brazil
Correspondence: Daniela Ponce, Department of Internal Medicine – UNESP, Univ Estadual Paulista, Rubião Jr, s/n, Botucatu, SP, 18.618-970, Brazil, Tel/Fax +55 14 3811-6000, Email [email protected]
Background: In the absence of direct therapy for COVID-19, extracorporeal blood treatment (EBT) could represent an option for cytokine removal.
Objective: This study aimed to describe and compare cytokine removal during intermittent haemodialysis (IHD) and continuous renal replacement therapy (CRRT) in COVID-19 patients with Acute Kidney Injury (AKI).
Methods: It was a cohort study that studied patients with COVID-19-related AKI according to KDIGO criteria and admitted at Intensive Care Unit (ICU). Blood samples were collected at the start and end of both IHD using high flux (HF) membranes (10 patients) and continuous venovenous haemodiafiltration (CVVHDF:10 patients) in two sessions for measuring 13 different plasma interleukins and calculating the cytokine removal rate.
Results: There was no difference between the two groups regarding mechanical ventilation, vasoactive drug, age or prognostic scores. Patients treated by CRRT presented higher levels of IL-2 and IL-8 than patients treated by IHD at dialysis start. Cytokine removal ranged from 9% to 78%. Patients treated by CRRT presented higher cytokine removal for IL-2, IL-6 IL-8, IP-10 and TNF. The removal rates of IL-4, IL-10, IL-17A, IFN, MCP-1 and TGF-B1 were similar in two groups. After one session of CVVHDF (24 h), IL-2 and IL-1β levels did not vary significantly, whereas IL-4, IL-6, IL-8, IL-10, IL-17A, TNF, IFN, IP-10, MCP-1, IL-12p70 and TGF-B1 decreased by 33.8– 76%, and this decrease was maintained over the next 24 h. In IHD groups, IL-2, IL-6, TNF, IP-10 and IL-1β levels did not decrease significantly whereas IL-4, IL-8, IL-10, IL-17A, IFN, MCP-1, IL-12p70 and TGF-B1 decreased by 21.8– 72%; however, cytokine levels returned to their initial values after 24 h.
Conclusion: Cytokine removal is lower in IHD using HF membranes than in CVVHDF, and in IHD the removal is transient and selective, which can be associated with mortality during cytokines storm-related COVID-19.
Keywords: cytokine storm, removal, EBP
Introduction
The World Health Organization declared coronavirus disease 2019 (COVID-19) a pandemic. Although the vast majority of COVID-19 patients suffer from mild symptoms, around 15% of individuals hospitalized for symptomatic COVID-19 infection require admission to intensive care units (ICUs) and, among them, 37% develop acute kidney injury (AKI).1–3 Of those with AKI, 14% required renal replacement therapy (RRT), meaning that 5% of all patients hospitalized with COVID-19 required some form of dialysis support.4 Previous studies have pointed out cytokine storm as a possible cause of aggravation of COVID-19.5 It is a systemic inflammatory reaction that releases a series of cytokines, including TNF‐α, IL‐1β, IL‐2, IL‐6, IFN‐α and MCP‐1, which induce immune cells to release large amounts of free radicals, which are the leading cause of multiple organ failure, including AKI.6
Extracorporeal blood treatment (EBT) has also been proposed as an approach to remove cytokines in patients with sepsis7 and potentially could be beneficial in critically ill patients with COVID-19.8,9
Among the EBT therapies both Intermittent Hemodialysis (iHD) using high flux (HF) or high cut-off membranes (characterized by larger pore size and more effective clearance for medium-molecular-weight molecules such as cytokines), and Continuous RRT can be considered.10 Hybrid treatments such as prolonged intermittent haemodialysis (IHD) incorporate the advantages of both continuous RRT (CRRT) and IHD and are used worldwide in many ICUs.11–13 They may be considered for haemodynamically unstable patients in situations where other forms of CRRT are not available, but data on comparative efficacy and harm are limited.14–17
Prolonged IHD (using HF or high cut-off membranes) and Continuous Venovenous Hemodiafiltration (CVVHDF) are two different modalities of EBT that have the functions of supporting renal function, adsorbing endotoxins and removing inflammatory mediators.18–20
In this paper, we performed a prospective study that aimed to describe and compare cytokine variations and removal during and after IHD and CRRT in COVID-19 patients with AKI.
Methodology
Patients
A prospective cohort study of 20 hospitalized patients diagnosed with AKI related to COVID-19 undergoing RRT (IHD or HDF) was realized in the ICUs of a public and a tertiary university hospital in São Paulo, Brazil, from June to August 2020. Diagnosis of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was confirmed using reverse transcription polymerase chain reaction and the AKI diagnosis and classification were performed according to KDIGO criteria.6 The need for dialysis was indicated by the gap between demand and capacity and also the presence of cytokine storm syndrome (CSS: continuous fever >39°C). Patients were treated with either IHD or CRRT according to local availability and the patient’s clinical status (if noradrenaline use higher than 0.5 ucg/kg/min, patients were treated by prolonged HD or CRRT). Patients with chronic kidney disease (stages IV and V), those needing kidney transplants and individuals under 18 years old were excluded.
This study was registered in the Brazilian Registry of Clinical Trials (ReBEC: number RBR-62y3h7) and approved by the Research Ethics Committee of Botucatu School of Medicine (CAAE: 30451520.6.0000.5411 in 30 April 2020). All research was performed following current regulations and written informed consent was obtained from all participants or their legal guardians.
EBT Procedures
Vascular access was obtained using 12-Fr dual-lumen catheters in an internal jugular vein.
Prolonged iHD
Sessions lasting 6 h were performed with blood flows of 200 mL/min and dialysate flows of 300 mL/min. We used a Fresenius 4008S ARrT Plus dialysis machine (Fresenius Medical Care AG, Bad Homburg, Germany) and HF membranes (polyethersulfone filters, surface area 1.7 m2; Nipro, Germany). The HF membranes were defined according to an estimated pore size of 5 nm, resulting in an in vitro cut-off point of at least 40 kDa (at least 30 kDa for in vivo) and an ultrafiltration coefficient of >20 mmHg.
During the sessions, patients were anticoagulated with an initial 50–100 IU/kg bolus dose of heparin and then at 500–1000 IU/h over the following hours. In cases of contraindication to anticoagulation, the system was washed with 50 mL of 0.9% sodium chloride every 30 min throughout the entire procedure. The concentrations of bicarbonate (26–36 mEq/l), potassium (1–3 mEq/l), sodium (140–145 mEq/l) and calcium (2.5–3.5 mEq/l) in the dialysis bath were adjusted according to examination and the individual needs of the patients. The ultrafiltration rate did not exceed 500 mL/h and the bath temperature was 35–35.5°C.
Crrt
CRRT was operated as continuous venovenous haemodiafiltration (CVVHDF) using an AN69 membrane (ST 100, Baxter) through a Prismaflex CRRT system (Baxter). Due to the clinical conditions, blood flow rates were kept in the range 140–180 mL/min and dialysis doses were 30 mL/kg/h. Patient fluid removal is tailored to the individual’s volume status (100–250 mL/h) and the filter was changed every 48 h.
A regional citrate anticoagulation regimen was adopted, with anticoagulant doses adjusted individually according to the patients’ coagulation state, and a sterile citrate‐containing solution without calcium was infused in predilution mode. In postdilution, a sterile saline solution containing calcium chloride was infused to maintain the postfilter (Ca2+ = 0.25–0.35 mmol/l) and arterial line (Ca2+ = 1–1.2 mEq/l).
Cytokine Removal During Dialysis
We measured plasma concentrations of cytokines (IL-2, IL-4, IL-6, IL-8, IL-10, IL-17A, TNF, IFN, IP-10, IL-12p70, MCP and free active TGF-B1) at the initial (T0) and final (Tf) dialysis session (6 h for prolonged IHD and 24 h for CRRT) over 2 days. Blood samples and dialysate were collected in non-heparinized tubes, immediately centrifuged at 4000 rpm for 10 min (4°C) and then subsequently stored at –70°C until assayed. Quantification of cytokines was determined by enzyme-linked immunosorbent assay (ELISA) using LEGENDplexTM Human Essential Immune Response Panel (13-plex San Diego, CA, USA) according to the manufacturer’s instructions. Assay sensitivity limits were 0.22 pg/mL for IL-2, 2.84 pg/mL for IL-4, 2.0 pg/mL for IL-6, 2.50 pg/mL for IL-8, 3.14 pg/mL for TNF-α, 1.25 pg/mL for IL-10, 6.32 pg/mL for IP-10, 2.27 pg/mL for IL-1b, 1.8 pg/mL for MCP-1, 1.36 pg/mL for IL-17A, 3.0 pg/mL for INF, and 1.89 pg/mL for IL-12p70. All measured cytokines had molecular weight between 8 and 35 kDa (IL-2: 15kDa, IL4: 18 kDa, IL-6: 28 kDa, IL-8: 12 kDa, IL-10:19 kDa, IL −8: 8 kDa, TNF 17 kDa, MCP-1: 10 kDa, IFN 18 kDa, IL 17A: 35 kDa, IL12p70: 35kDa).
We calculated cytokine removal according to the formula Cf – C0 / Cf x 100, where C0 is the cytokine concentration at the initial dialysis session and Cf is the cytokine concentration.
Statistical Analysis
SPSS 19.0 software was used for statistical analysis. Frequency measures were calculated for categorical variables; measurement of continuous variables conforming to a normal distribution were expressed as mean ± standard deviation and those not conforming to a normal distribution were expressed as median with interquartile range. Comparison of data before and after treatment was performed by paired t-test or non-parametric test for continuous variables and by chi-squared test for categorical variables.
Results
We evaluated cytokine removal in 20 patients with COVID-19-related AKI undergoing prolonged IHD (10 patients) or CRRT (CVVHDF). There was no difference between the IHD and CVVHDF groups regarding mechanical ventilation, vasoactive drug use, age or prognostic scores (APACHE II and SOFA). Patients did not receive tocilizumab. On dialysis, these patients presented elevated levels of cytokines measured at the start of the dialysis session, as shown in Table 1. Patients treated by CRRT presented higher levels of IL-2 and IL-8 than patients treated by prolonged IHD at T0 (before the start of dialysis).
 |
Table 1 Clinical and Laboratory Characteristics in AKI-Related to COVID Patients Admitted in ICU According to Renal Acute Support Modality |
Table 2 provides details of cytokine removal during the dialysis session. Cytokine removal ranged from 9% to 78%. Patients treated by CRRT presented higher cytokine removal rates than those treated by prolonged IHD for IL-2, IL-6, IL-8, IP-10 and TN. The removal rates of IL-4, IL-10, IL-1β, IL-17A, IFN, MCP-1 and free active TGF-B1 were similar in the two groups.
 |
Table 2 Cytokines Removal During Prolonged iHD and CVVHDF |
After one session of CVVHDF (24 h) the IL-2 and IL-1β levels did not vary significantly whereas IL-4, IL-6, IL-8, IL-10, IL-17A, TNF, IFN, IP-10, MCP-1, IL-12p70 and free active TGF-B1 decreased by 33.8–76%, and this decrease was maintained over the next 24 h, as shown in Figure 1. In the prolonged IHD groups, IL-2, IL-6, TNF, IP-10 and IL-1β did not decrease significantly but IL-4, IL-8, IL-10, IL-17A, IFN, MCP-1, IL-12p70 and free active TGF-B1 decreased by 21.8–72%. However, all cytokine levels returned to their initial values, despite their removal by prolonged IHD (Figure 2).
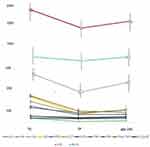 |
Figure 1 Variations of cytokine levels during and 24h after end of CRRT. Abbreviations: T0, start of dialysis; TF, end of dialysis. |
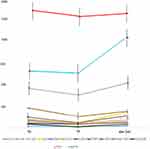 |
Figure 2 Variations of cytokine levels during and 24h after end of prolonged iHD. Abbreviations: T0, start of dialysis; TF, end of dialysis. |
Discussion
COVID‐19 is an epidemic of global concern and previous studies have pointed out CSS as a possible cause of aggravation.5 Usually, the anti-inflammatory response and tissue repair processes are mild and self-limiting. However, if the cytokines, such as TNF-α, IL-6, IL-1, and IFN, continue to increase, they can stimulate pathological reactions such as diffuse alveolar damage, transparent membrane formation, and pulmonary fibrosis.19 Cytokines, when entering the circulation, can induce extensive endothelial dysfunction, disseminated intravascular coagulation, and MODS.
Since Covid‐19‐induced organ damage is mainly mediated by cytokine storm, strategies to early reduce or remove inflammatory cytokines could be effective in preventing MODS.9
EBT is considered an important means for removing cytokines from patients with sepsis and also the main advocated technology of organ support therapy for patients with severe COVID‐19. Prolonged IHD (using HF or high cut-off membranes) and CVVHDF are two different modalities of EBT that have the functions of supporting renal function, adsorbing endotoxins and removing inflammatory mediators.20
Prolonged IHD is a hybrid treatment that incorporates the advantages of both CRRT and IHD and is used worldwide in many ICUs but mainly in developing countries12–14 where other forms of CRRT are not available due to the high costs. A systematic review and meta-analysis including 17 studies during 2000–2014 (7 randomized controlled trials and 10 observational studies involving 533 and 675 patients, respectively) focused on the impact of prolonged intermittent RRT and CRRT on mortality and renal recovery17 and showed no difference in mortality between the two modalities.
We evaluated cytokine removal in patients with COVID-19-related AKI undergoing prolonged IHD using HF membranes or CVVHDF. Our study showed that cytokine removal ranged from 9% to 78%. Patients treated by CRRT presented higher cytokine removal rates for IL-2, IL-6, IL-8, IP-10 and TNF than patients treated by prolonged IHD. The removal rates of IL-4, IL-10, IL-1β, IL-17A, IFN, MCP-1 and free active TGF-B1 were similar in the two groups. It is well known that cytokine removal depends on time of therapy, molecular weight of each cytokine and type of membrane. For example, the AN69 membranes used in CRRT have a highly hydrophilic hydrogel structure, and in vitro experiments have confirmed that they can effectively adsorb inflammatory mediators. Also, CRRT sessions last 24h while PHD sessions last 12h, explaining higher cytokine removal as IL-2, IL-6 and TNF in CRRT groups than PHD group.21–23
After one session of CVVHDF (24 h) the IL-2 and IL-1β levels did not vary significantly whereas IL-4, IL-6, IL-8, IL-10, IL-17A, TNF, IFN, IP-10, MCP-1, IL-12p70 and free active TGF-B1 decreased by 33.8–76%, and this decrease was maintained over the next 24 h. These findings are in accordance with previous studies.10,19 The application of EBT is helpful for the removal of cytokines and may be beneficial for improving the clinical outcome of critically ill patients. Commonly used EBT therapies are plasma exchange and high-dose CRRT. Previous studies have suggested that therapeutic plasma exchange and CRRT play an important role in the treatment of severe haemophagocytic syndrome and sepsis in critically ill children and adult patients with AKI by reducing the levels of cytokines (such as TNF-α and IL-6) and improving the SOFA (sequential organ failure assessment) score after the application of CRRT.21–23
CRRT with the recently developed CytoSorb and oXiris (commercially available haemoadsorption and haemodiafilters that utilize EBT) has been designed to reduce systemic cytokine burden. Numerous case reports and case series have suggested improved clinical outcomes with CytoSorb in patients with septic shock.24
Recently, Villa et al25 showed that EBT with oXiris decreased the serum IL-6 level, attenuated systemic inflammation, improved multi-organ dysfunction and reduced the expected ICU mortality rate in 37 patients with COVID-19. This shows that CRRT has become a multi‐organ support rather than pure renal replacement among these patients, due to the development of new medical and membrane technology, and provides opportunity and conditions for further treatment that may improve patient outcome.
In our study, we observed that prolonged IHD using HF membranes only partially and transiently removed plasma IL-4, IL-8, IL-10, IL-17A, IFN, MCP-1, IL-12p10 and free active TGF-B1, and did not remove IL-2, IL-6, TNF, IP-10 or IL-1β. The kinetics of plasma cytokine levels after IHD in patients with COVID-19-related AKI have not been reported previously and studies on sepsis-related AKI are scarce. Mayeur et al26 evaluated cytokine removal in 10 patients with sepsis-related AKI treated with IHD using HF membranes (polymethymethacrylate haemodialyser). During IHD, the IL-6 level did not vary significantly whereas IL-8 and IL-10 were reduced by 31.8 ± 21.2% and 36.3 ± 26%, respectively. After 3 h, both IL-8 and IL-10 returned to their initial values.
The rebound phenomenon, which can be applied to the shift of soluble molecules from tissues to the intravascular compartment through a concentration gradient until a new equilibrium is reached, can explain the transient cytokine reduction. Cytokines are heavier and less diffusive molecules than urea or potassium, therefore this rebound could reflect a cytokine concentration gradient between tissue and vascular compartments that appeared during IHD. After IHD, a progressive release of cytokines from dialysis-induced hypoperfused tissue to the intravascular compartment may occur until a new equilibrium is reached.
There were several limitations to this study: it was a descriptive research study without a control group due to the specificity of the disease; the small sample size may have led to deviation of the results; we did not analyse the cytokine levels in dialysate and thus did not calculate their clearance; and we did not evaluate the association between cytokine removal and stabilization of haemodynamic status and improvement of organ function.
Despite these limitations, our results show that cytokine removal is lower by prolonged IHD using HF membranes than by CVVHDF. Furthermore, prolonged IHD allows a transient and selective decrease in cytokines that can be correlated with mortality during septic shock or CSS-related COVID-19.
Further studies will be necessary to more clearly define the roles of cytokines removal by different types of EBT and its relation to clinical outcome.
Data Sharing Statement
All data generated or analysed during this study can be included in this published article if necessary.
Statement
This study complies with the Declaration of Helsinki.
Ethics Approval and Consent to Participate
This study was registered in the Brazilian Registry of clinical trials (ReBEC) under number RBR-62y3h7 and was approved by the Research Ethics Committee of Botucatu School of Medicine (CAAE 30451520.6.0000.5411). All patients have given written informed consent:
Acknowledgements
We thank all nurses that assist patients with COVI 19 in Clinical Hospital from Botucatu School of Medicine.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study has no funding.
Disclosure
Prof. Dr. Alexandre Naime Barbosa reports grants and/or personal fees from GSK, Abbvie, Boehringer Ingelheim, Celltrion, Gilead, Janssen, Medictalks, MSD, Pfizer, Sanofi Pasteur, Takeda, Wyethand, and Dr. Reedy’s; non-financial support from Eurofarma, outside the submitted work. The authors declare that they have no other competing interests in this work.
References
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi:10.1016/S0140-6736(20)30183-5
2. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052. doi:10.1001/jama.2020.6775
3. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–539. doi:10.1007/s00281-017-0629-x
4. Hirsch J, Ng J, Ross D, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98:209–218. doi:10.1016/j.kint.2020.05.006
5. Ronco C, Reis T, De Rosa S. Coronavirus epidemic and extracorporeal therapies in intensive care: si vis pacem para bellum. Blood Purif. 2020;49:255–258. doi:10.1159/000507039
6. Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473–474. doi:10.1126/science.abb8925
7. Lh D, Widiasta A, Ghrahani R, Hilmanto D, Rachmadi D. Therapeutic plasma exchange as a promising therapeutic modality in the management of acute cytokine storms and secondary prevention of chronic kidney disease in children during pandemic. Int J Pharm Res. 2022. doi:10.31838/ijpr/2021.13.02.259
8. Ronco C, Reis T, Husain-Syed F. Management of acute kidney injury in patients with COVID-19. Lancet. 2020;229. doi:10.1016/S2213-2600(20)30229-0
9. Ronco C, Reis T. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nature Reviews Nephr. 2020;16:308–310. doi:10.1038/s41581-020-0284-7
10. Stamm O, Latscha U, Janecek P, Campana A. Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138. doi:10.1016/s0002-9378(16)33297-5
11. Monard C, Rimmelé T, Ronco C. Extracorporeal blood purification therapies for sepsis. Blood Purif. 2019;47((suppl 3):):2–15. doi:10.1159/000499520
12. Ponce D, Abrão JM, Albino BB, et al. Extended daily dialysis in acute kidney injury patients: metabolic and fluid control and risk factors for death. PLoS One. 2013;8:e81697. doi:10.1371/journal.pone.0081697
13. Albino BB, Balbi AL, Abrao JM, et al. Dialysis complications in acute kidney injury patients treated with prolonged intermittent renal replacement therapy sessions lasting 10 versus 6 hours: results of a randomized clinical trial. Artif Organs. 2015;39:423–431. doi:10.1111/aor.12408
14. Fieghen HE, Friedrich JO, Burns KE, et al. The hemodynamic tolerability and feasibility of sustained low efficiency dialysis in the management of critically ill patients with acute kidney injury. BMC Nephrol. 2010;11:32. doi:10.1186/1471-2369-11-32
15. Marshall MR, Ma T, Galler D, et al. Sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring renal replacement therapy: towards an adequate therapy. Nephrol Dial Transplant. 2004;19:877–884. doi:10.1093/ndt/gfg625
16. Holt BG, White JJ, Kuthiala A, et al. Sustained low-efficiency daily dialysis with hemofiltration for acute kidney injury in the presence of sepsis. Clin Nephrol. 2008;69:40–46. doi:10.5414/CNP69040
17. Kumar VA, Yeun JY, Depner TA, et al. Extended daily dialysis vs. continuous hemodialysis for ICU patients with acute renal failure: a two-year single center report. Int J Artif Organs. 2004;27:371–379. doi:10.1177/039139880402700505
18. Rachmadi D, Widiasta A, Sukandar H, Sekarwana N, Hilmanto D. The association between kidney function and the severity of COVID-19 in children. Open Access Maced J Med Sci. 2022;10(B):1473–1478. doi:10.3889/oamjms.2022.9784
19. Chen G, Zhou Y, Ma J, Xia P, Qin Y, Li X. Is there a role for blood purification therapies targeting cytokine storm syndrome in critically severe COVID-19 patients? Ren Fail. 2020;42(1):483–488. doi:10.1080/0886022X.2020.1764369
20. Villa G, Zaragoza JJ, Sharma A, Neri M, Gaudio R, Ronco C. Cytokine removal with high cut-off membrane: review of literature. Blood Purif. 2014;38:167–173. doi:10.1159/000369155
21. Madelaine T, Page M, Prothet J, et al. Super high-flux continuous hemodialysis in septic shock: a case report. Nephrol Ther. 2013;9:497–500. doi:10.1016/j.nephro.2013.07.370
22. Kade G, Wiśniewska M, Lubas A, Rzeszotarska A, Korsak J. The treatment of septic shock with continuous venovenous hemodialysis using high cut-off dialyzer in patient after immediate circulatory arrest. Przegl Lek. 2013;70:698–700. doi:10.1016/0002-9378(76)90154-x
23. Chelazzi C, Giugni D, Giannoni C, Villa G, De Gaudio AR. Use of continuous venovenous hemodiafiltration with a high cutoff membrane in a patient with severe acute pancreatitis. J Nephrol. 2012;2:78–81.
24. Ronco C, Bonello M, Bordoni V, et al. Extracorporeal therapies in non-renal disease: treatment of sepsis and the peak concentration hypothesis. Blood Purif. 2004;22:164–174. doi:10.1159/000074937
25. Villa G, Romagnoli S, De Rosa S, et al. Blood purification therapy with a hemodiafilter featuring enhanced adsorptive properties for cytokine removal in patients presenting COVID-19: a pilot study. Critical Care. 2020;24:605.
26. Mayeur N, Rostaing L, Nogier MB, et al. Kinetics of plasmatic cytokines and cystatin C during and after hemodialysis in septic shock-related acute renal failure. Critical Care. 2010;14:R115. doi:10.1186/cc9064
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
