Back to Journals » Infection and Drug Resistance » Volume 14
Khat Chewing and Clinical Conditions Determine the Epidemiology of Primary Drug Resistance Tuberculosis in Amhara Region of Ethiopia: A Multicenter Study
Authors Kassa GM , Merid MW, Muluneh AG
Received 20 April 2021
Accepted for publication 18 June 2021
Published 30 June 2021 Volume 2021:14 Pages 2449—2460
DOI https://doi.org/10.2147/IDR.S316268
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Getahun Molla Kassa, Mehari Woldemariam Merid, Atalay Goshu Muluneh
Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences and Specialized Comprehensive Hospitals, University of Gondar, Gondar, Ethiopia
Correspondence: Atalay Goshu Muluneh Email [email protected]
Background: Rifampicin and/or multidrug-resistant tuberculosis (RR/MDR-TB) remains an uncontrolled public health emergency that has been synergized by the recently increased person-to-person transmission in the community as primary RR/MDR-TB, which is defined as RR/MDR-TB in new TB patients with no prior exposure to anti-TB treatment for more than one month. This study aimed to measure the prevalence and associated factors of primary drug-resistance among drug-resistant tuberculosis patients, as evidenced by the Amhara region treatment initiating centers.
Methods: An institutional-based multicenter cross-sectional study was conducted from September 2010 to December 2017, among 580 RR/MDR-TB patients on the second-line anti-TB drug in the Amhara regional state. Data were collected from patient charts and registration books using a standardized data abstraction sheet. The data were entered using Epi-data 4.2.0.0 and transferred to Stata 14 software for further data management and analysis. A bivariable and multivariable binary logistic model was run subsequently, and finally, a p-value of less than 0.05 with a 95% confidence interval (CI) was used to declare the significance of the explanatory variable.
Results: The magnitude of primary drug resistance among drug-resistant tuberculosis patients was 15.69% (95% CI: 12.94, 18.89). Alcohol drinking (adjusted odds ratio [AOR] = 0.31, 95% CI: 0.12– 0.82), khat chewing (AOR = 4.43; 95% CI: 1.67– 11.76), ambulatory and bedridden functional status (AOR = 0.43; 95% CI: 0.24– 0.76) and (AOR = 0.41; 95% CI: 0.19– 0.91), respectively, positive sputum smear result (AOR = 0.48; 95% CI: 0.26– 0.90), and HIV coinfection (AOR= 2.31; 95% CI: 1.31– 4.06) remained statistically significant associated factors of primary RR/MDR-TB.
Conclusion: Primary drug resistance is a public health problem in the study setting. Different behavioral and clinical conditions were significant factors of primary drug-resistant development. Mitigation strategies targeted on the patient’s clinical condition, substance-related behaviors, and universal DST coverage might be very important for early detection and treatment of RR/MDR-TB to prevent community-level transmission.
Keywords: clinical conditions, epidemiology of primary RR/MDR-TB, Ethiopia
Introduction
Drug-Resistant Tuberculosis (DR-TB) remains an international emerging public health crisis that has been reported in all surveyed countries.1 The high mortality, limited treatment options, and rapid spread of DR-TB have become a major hindrance to the global Tuberculosis (TB) control program.2 In 2018, estimated half a million new cases of Rifampicin Resistant TB (RR-TB) cases were reported worldwide, of which 50% were found in India (27%), China (14%), and the Russian Federation (9%). Globally, the proportion of Multidrug-Resistant TB (MDR-TB) from RR-TB was 78%. Both RR-TB and MDR-TB, which are resistant to the most potent first-line anti-TB drugs (rifampicin and isoniazid), require treatment with second-line anti-TB drugs.1
The world’s leading curable cause of infectious disease mortality is TB, with a disproportionate problem in low- and middle-income countries.3 From the 14 high TB, TB/HIV, and MDR-TB profoundly affected countries, eight of them were situated in Africa including Ethiopia. In Ethiopia by the year 2018, there were 741 laboratories confirmed RR/MDR-TB cases and the estimated incidence of RR/MDR-TB case among new and previously treated tuberculosis cases were 0.71% and 16%, respectively.1 The occurrence of DR-TB in new patients with no prior exposure to TB treatment for one or more months is the result of primary drug resistance which represents 3/4th of the annual estimated RR/MDR-TB cases in Ethiopia.4 As reported from a meta-analysis, the most common lineages in Ethiopia were Euro-American (64.8%) followed by East African-Indian (23.0%), Indo-Ocean (7.1%), Ethiopian (4.1%), and East Asian/Beijing (0.2%).5 From new pulmonary tuberculosis (TB) in the Amhara Region of Ethiopia, the T (30.8%), Central Asian/CAS (21.1%), and U (17.7%) families were the predominant isolates strains.6
The rifampicin-resistant TB (RR-TB) and multidrug-resistant TB (MDR-TB) as compared to drug-susceptible tuberculosis for the first-line anti-TB drugs requires longer treatment duration (>9 months Vs 6 months), more toxic and expensive drugs (median ≥ 6430Vs 973 US$ per person), and low treatment success rate (56% Vs 85% globally).1 The End-TB strategy will be further challenged by the rising epidemics of Primary RR/MDR-TB.7
Most of RR/MDR-TB were acquired in the course of first-line anti-tuberculosis treatment due to drug ill-use.8 Currently, there is an increasing incidence of primary infection with drug-resistant strain bacillis.9 The main source cases for community-level DR-TB transmission include those patients with DR-TB who are missed or late to be detected or TB cases who are not receiving effective and adequate treatment.8,10 Despite this, the chance of developing wild-type RR/MDR-TB is extremely unusual to date as primary MDR/RR-TB is up-surging in the general community. This praised incidence of primary RR/MDR-TB amplifies the rate of ongoing person-to-person transmission of primary RR/MDR-TB in the community.8
Previous literature identified several socio-demographic, clinical, and economical risk factors for the development of primary RR/MDR-TB. These include being single, poor education, low living space, poor eating fruits, low income, having mental stress, lacking medical insurance, contact history, and suffering from a chronic debilitating disease.11,12
To date, valid documents on the magnitude and associated factors of primary DR-TB were limited in Ethiopia and the study setting. We, therefore, exploited the routinely collected data for clinical practice to determine the magnitude and associated covariates of primary MDR/RR-TB among patients registered for DR-TB treatment in the Amhara regions of Ethiopia. The result of the study can be used as an input to support the control of DR-TB spread and provide insight for further research.
Methods
Study Design, Setting, and Population
An institution-based multicenter cross-sectional study was conducted on all RR/MDR-TB patients registered for second-line anti-TB drug treatment into the four second-line anti-TB drug treatment-initiating center hospitals (University of Gondar, Boru-Meda, Debre-Markos, and Woldia) in Amhara regional state between September 2010 and December 2017. These four hospitals account for more than 90% of the RR/MDR-TB in the region. The region has the second-highest number of TB cases notified yearly following the Oromia region in the country. Amhara regional state is the second-largest and populated state among the ten regional and two town administrative states in Ethiopia. All the patients were bacteriologically confirmed RR/MDR-TB. The diagnosis of tuberculosis and its drug resistance was made either of the GeneXpert MTB/Rif assay or Line Probe Assay (LPA) and further triangulated by culture-based phenotypic drug susceptibility testing.
All RR/MDR-TB patients registered for second-line anti-TB treatment in the region were the source population, whereas those patients enrolled for treatment from September 2010 to December 2017 in the selected hospitals were the study population. Patients without recorded information on the previous episode of tuberculosis were excluded.
Data Collection and Quality Control
Data were mined from the medical records using a structured data collection form. Baseline sociodemographic, behavioral, and clinical information (including sex, age, residency, marital status, education status, occupation, treatment supporters, housing status, smoking history, history of alcohol drinking, history of khat chewing, anatomical site, functional status, sputum smear result, previous episode of tuberculosis, TB registration group, underlying comorbid diseases, and HIV co-infection) were obtained from medical record reviews. An effort was also invested to assess patients’ contact history with DR-TB patients retrospectively from the contact registration logbook; unfortunately, the contact profiles of the patient were not recorded. To maintain the quality of the data, a half-day hands-on training was given to the data collectors. Data were collected by four master’s degree students under the close supervision of the researchers. The completeness and consistency of the data were inspected and corrected day-to-day.
Variables Measurement/Definitions
Based on the Ethiopian Ministry of Health PMDT guideline,4 the outcome variable for this study was primary RR/MDR-TB. The occurrence of RR/MDR-TB in new patients with no prior exposure to anti-TB treatment for one or more months was considered as primary RR/MDR-TB, whereas patients who have received anti-TB drugs for one or more months in the past and again diagnosed with tuberculosis were considered as secondary RR/MDR-TB. Multidrug-resistant TB (MDR-TB) was a TB bacillus that was resistant to rifampicin and isoniazid, with or without resistance to other first-line anti-TB drugs; if the resistance was for rifampicin and other drugs except for isoniazid it is named as Rifampicin Resistant TB (RR-TB).
Tuberculosis patient registration group: New: Patients that have never been treated for TB or have taken anti-TB drugs for less than 1 month. Relapse: Patients who were declared cured or treatment completed at the end of their most recent treatment course, and are now diagnosed with a recurrent episode of TB regardless of duration. Treatment after failure: Patients who came back for treatment after declared treatment failure in their most recent treatment course, as defined by the national guideline. Treatment after lost to follow-up: Patients who were declared lost to follow-up at the end of their most recent course of TB treatment and are now decided to be treated with the full course of TB treatment.
Final treatment outcomes assignment: Cured: Treatment completed according to national recommendation without evidence of failure and three or more consecutive cultures taken at least 30 days apart are negative after the intensive phase. Treatment completed: Treatment completed according to national recommendation without evidence of failure but no record that three or more consecutive cultures taken at least 30 days apart are negative after the intensive phase. Treatment failure: Treatment terminated or the need for permanent regimen change of at least two anti-TB drugs due to lack of sputum conversion by the end of the intensive phase, or bacteriological reversion in the continuation phase after conversion to negative after intensive phase, or evidence of additional acquired resistance to fluoroquinolones or second-line injectable drugs. Died: A patient who dies for any reason during TB treatment. Lost to follow-up (LTFU): A patient who underwent treatment for at least one month and was interrupted for two consecutive months or more. Transfer out: a patient who is transferred to continue treatment in another reporting unit after starting treatment.
Homelessness was defined as patients who lived on the streets or lacked fixed, regular, and adequate nighttime residence. Cigarette smoking: those patients who had every history of smoking were documented as smokers. Khat chewing: Patients chewing khat for any reasons like for recreation, social, or religious purposes were considered chewers.
Data Processing and Statistical Analysis
After data was entered into epi-date 4.2.0.0, it was exported to Stata 14 for further cleaning, coding, recoding, and analysis. The socio-demographic, behavioral, and clinical features of patients were analyzed descriptively. Median with interquartile range and mean with Standard Deviation (SD) were used for skewed and normally distributed continuous variables, respectively. Texts, tables, and figures were used to present results. The Chi-square assumptions were assessed and valued for categorical explanatory variables. A binary logistic regression model was used to evaluate the association between patient characteristics and primary RR/MDR-TB. The Hosmer-Lemeshow goodness-of-fit test was computed to evaluate the model adequacy and multicollinearity was checked using a variance inflation factor. p-values of <0.2 and 0.05 were used as a cut of points to declare statistical significance in the bi- and multivariable binary logistic regression models, respectively. Adjusted Odds Ratio (AOR) with 95% CI was reported for significant variables in the multivariable logistics regression model.
Results
Socio-Demographic and Behavioral Characteristics
Out of 588 RR/MDR-TB cases recorded during the study period, we included 580 cases that had a documented history of tuberculosis treatment. The mean and Standard Deviation (SD) of age was 31.36 + 12.29 years, ranging from one to seventy-five years. More than half (56.90%) were male and (52.34%) were urban residents. Approximately half (43.79%) were not formally educated. Of all who have records of ever history of smoking, 13.28% were smokers (Table 1 at the end).
 |
Table 1 Socio-Demographic and Behavioral Characteristics of RR/DR- TB Patients in Amhara Regional State, Ethiopia: 2010–2017 (N=580) |
More than half of the primary and approximately 60% of all RR/MDR-TB patients were from the University of Gondar comprehensive specialized hospital treatment initiating center. The magnitude of the primary RR/MDR-TB was lower in Gondar (12.32%), but it was higher in Woldia (31.37) (Figure 1).
 |
Figure 1 Number of patients from each treatment-initiating center stratified by their primary and secondary RR/MDR-TB status, Amhara regional state, Ethiopia: 2010–2017 (N=580). |
Clinical Characteristics, Final Treatment Outcome, and Development of Adverse Drug Event
Of those with HIV tested 27.41% were co-infected. Nearly 90% and 80% of the patients were pulmonary tuberculosis and sputum smear-positive, respectively. One-third of the patients were working in functional status. The proportion of overall successful treatment outcome (cure plus completed) by discounting those patients still on treatment was 71.63%. Similarly, it was 67.16% for primary and 72.31% for secondary RR/MDR-TB patients. Adverse drug events were less common among the primary as compared to secondary RR/MDR-TB patients, 56.04% and 65.24%, respectively (Table 2 at the end).
 |
Table 2 Clinical Characteristics of RR/DR- TB Patients in Amhara Regional State, Ethiopia: 2010–2017 (N=580) |
We have assessed the presence of statistical significance difference among primary and secondary RR/MDR-TB patients regarding the subsequent development of adverse drug events and successful final treatment outcomes by using the Pearson Chi-square test. And, the difference was found to be insignificant with a p-value of 0.094 and 0.384 consecutively.
The magnitude of primary RR/MDR-TB was an increase in recent years as compared to the year before 2013 due to the implementation of the universal Drug Susceptible Test (DST) (Figure 2).
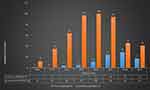 |
Figure 2 Number of RR/DR- TB patients cross-tabulated with the diagnosis year in Amhara regional state, Ethiopia: 2010–2017 (N=580). |
The Magnitude of Primary RR/MDR-TB
Of the total registered RR/MDR-TB patients 91 had no prior episode of tuberculosis. The overall magnitude of primary RR/MDR-TB 15.69% (95% CI: 12.94, 18.89); The magnitude reaches up to 22% in HIV co-infected, 24.14% in homeless, and 24.41% in sputum smear-negative, patients. Undesirably, 391 (67.41%) DR-TB patients were diagnosed for their RR/MDR-TB after the failure of their first-line anti-TB drug treatment. More than half of the study participants 297 (51.55%) had at least two previous episodes of tuberculosis treatment (Figure 3).
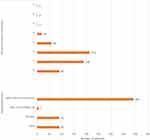 |
Figure 3 Number of previous treatment and registration group of RR/MDR- TB patients in Amhara regional state, Ethiopia: 2010–2017 (N=580). |
Factors Associated with Primary RR/MDR-TB
Those variables that satisfy the chi-square assumption were fitted in the bivariable and multivariable binary logistic regression analysis. From the bivariable binary logistic regression model, age, residency, marital status, treatment supporter, alcohol drinking, khat chewing, functional status, anatomical site of tuberculosis, sputum smear result, comorbidity, and HIV co-infection were significantly associated at a p-value of less than 0.2 and considered in the multivariable logistic regression. There are no significant associations between primary RR/MDR-TB and sex, educational status, occupation, and history of cigarette smoking. In the multivariable binary logistic regression model, alcohol drinking (Adjusted Odds Ratio [AOR] = 0.31, 95% Confidence Interval [CI]: 0.12–0.82), Khat chewing (AOR = 4.43; 95% CI: 1.67–11.76), ambulatory, and bedridden functional status (AOR = 0.43; 95% CI: 0.24–0.76), and (AOR = 0.41; 95% CI: 0.19–0.91), respectively, positive sputum smear result (AOR = 0.48; 95% CI: 0.26–0.90), and HIV coinfection (AOR= 2.31; 95% CI: 1.31–4.06) remained statistically significant (Table 3 at the end of the document). Model fitness was evaluated by the Hosmer-Lemeshow goodness-of-fit test in which the model was suitable (P-value=0.55).
 |
Table 3 Bivariable and Multivariable Binary Logistic Regression Analysis of Primary RR/MDR-TB Patients in Amhara Regional State, Ethiopia (N= 580) |
Discussion
Information on primary RR/MDR-TB from Ethiopia is inadequate. We, therefore, conducted a multicenter cross-sectional study to explore the magnitude and associated factors of primary MDR/RR-TB from a larger pool of DR-TB patients in the Amhara region of Ethiopia. Which was an indicator of the National Tuberculosis Control Program (NTP) performance in controlling the spread of drug-resistant tuberculosis?
The magnitude of primary RR/MDR-TB varies from country to country. The result of this study confirmed that the magnitude of primary MDR/RR-TB was 15.69% (95% CI: 12.94, 18.89). Our finding was comparable to the results of similar surveys conducted in Ethiopia,13 China,14 and Brazil.15 However, it was lower than studies conducted across the globe, such as Ethiopia (26.9%),16 South Africa (49%),17 the eastern coast of China (53.9),2 Vladimir Region of Russia (73.3%),18 and reports in a review of data for 30 countries having anti-tuberculosis drug resistance surveillance (31%-82%).19 This can be due to these countries taking the lion share of the global DR-TB patients and correspondingly increasing the prevalence of a primary form of RR/MDR-TB through increased transmission.1
On contrary to this, it was higher than the previous reports in Gondar (8.5%)20 and Amhara Regional state (10.7%),21 Ethiopia. A potential reason for this discrepancy might be that previous studies were done, while DST services were provided only for high-risk patients for DR-TB and at the early phase of universal DST implementation for all presumptive tuberculosis patients. The other explanation could be the difference in the study population. Two previous studies were done on sputum smear and culture-positive DR-TB tuberculosis patients, while our study was done on all forms of DR-TB patients. Taking into consideration the Treatment Initiating Centers (TICs), the prevalence of primary RR/MDR-TB was lower in Gondar (12.32%) and Boru-Meda (14.29) but somewhat higher in Debre-Markos (27.66%) and Woldia (31.37%) hospitals. The difference in magnitude of primary MDR/RR-TB across TICs was directly related to the implementation of universal DST for all presumptive tuberculosis patients and the time of the establishment of each TIC. Accordingly, the University of Gondar comprehensive specialized hospital was the first treatment initiating center and provided treatment service for all DR-TB in the region since September 2010, before the exercise of universal DST by the NTPs. Similarly, Boru-Meda TIC has launched the DR-TB treatment at the early phase of the universal DST implementation. However, the remaining two TICs were functioned for the treatment DR-TB during the implementation of universal DST, especially Woldia treatment-initiating center was established and introduced DR-TB treatment at the time of better implementation of the universal DST. We have tried to evaluate the relationship between the time of universal DST implementation and the proportion of primary RR/MDR-TB diagnosis, which clearly showed a linear association (Figure 2). To date, there has been no full access to DST service for all suspected or confirmed tuberculosis patients in Ethiopia. The prevalence of primary DR-TB will be higher if the country permits full DST access for all tuberculosis suspects. The finding from this research pointed out the existence of ongoing transmission of drug-resistant tuberculosis in the community. Late detection and delayed treatment initiation of infectious RR/MDR-TB disease play a major role in increasing epidemics of primary RR/MDR-TB.22 Evidence revealed that a single infectious RR/MDR-TB patient can spread on average to 22 individuals and finally produce more than two new tuberculosis diseased cases.23
After controlling the effect of sex, educational status, occupation, and history of cigarette smoking, the multivariable binary logistic regression analysis disclosed, history of khat chewing and HIV coinfection were positively associated, whereas the history of alcohol intake, poor functional status, and sputum smear positivity at the baseline was negatively associated with the magnitude of primary RR/MDR-TB.
Khat chewing increases the odds of acquiring primary MDR/RR-TB by four times. Even though works of the literature were lacking in this regard, the strong association between khat chewing and primary RR/MDR-TB could be because khat is an endogenous stimulant plant in which people have chewed it in groups in an enclosed space for different drives in Ethiopia. These enclosed/crowded and poorly ventilated spaces may favor the high person-to-person transmission of DR-TB. However, we did not find a biological relationship between khat chewing and TB from the kinds of the literature which might be a research question for future researchers.
HIV confection was another independent and positively associated factor with the high prevalence of primary MDR/RR-TB. This was supported by a report from a systematic review and meta-analysis done to examine the association between HIV infection and MDR-TB.24 This might be explained via the frequent health facility visit of HIV-coinfected patients for acute and chronic HIV care and repeated hospitalization for different opportunistic infection management that possibly craft the chance of exposure to drug-resistant tuberculosis bacilli in settings where DR-TB is prevalent and poor tuberculosis infection control is practiced. Also, HIV-infected patients were at higher risk of active DR-TB disease progression because of suppressed immunity.25 Moreover, the absence of prophylaxes for drug-resistant tuberculosis for HIV-coinfected patients as drug-susceptible tuberculosis such as isoniazid preventive therapy (IPT) may play its share in the increased occurrence of primary MDR/RR-TB. The high percentage of HIV coinfection (27.41%) in our finding compared to the reported HIV coinfection (5%) in drug-susceptible tuberculosis in Ethiopia will be another research question to be investigated.
The current study also showed that patients with a history of alcohol intake had 69% less likely to acquire primary RR/MDR-TB, while on the other hand, they were at a higher chance of developing secondary DR-TB. Several studies identified that alcohol consumption was an important population-level risk factor for secondary DR-TB due to the negative impact of alcohol on TB treatment adherence, impaired immune response, and increased risks of adverse drug events. Concurrent alcoholism treatment for alcoholic tuberculosis patients as a medical problem is largely desired to minimize the increased incidence of DR-TB.26–29
Patients with working functional status compared with those with poor functional status (bedridden and ambulatory) were having a lower odds of having primary RR/MDR-TB. We have tabulated and evidenced from our data that most of the poor functional status patients had a repeated history of tuberculosis treatment. The most likely incriminating cause of the worst functional status could be these repeated previous tuberculosis attacks, which result in a secondary form of RR/MDR-TB rather than a primary form of drug resistance.
Those DR-TB patients with positive sputum smear results at the baseline were 52% or less likely to have a primary form of DR-TB. To the best of our knowledge, we cannot find any literature reporting sputum smear results as a factor for primary drug-resistant development. But the study reports that smear positivity does not affect primary drug-resistance among drug-resistant patients.25
Limitations
We are confident that our research proved strong evidence for policymakers and researchers, but it might not be free of limitations. The cross-sectional nature of the study design and unavailability of data on a sensitive indicator of primary transmission of tuberculosis within the communities like contact history and nosocomial transmission is the main limitation of this study.
Conclusion
Primary drug-resistant tuberculosis continues as a public health problem in Ethiopia. History of alcohol drinking and khat chewing, ambulatory and bedridden functional status, positive sputum smear result, and HIV co-infection were significantly associated with the development of primary MDR/RR-TB. The result of the study is essential to inform policymakers and stakeholders as input to support the control and prevention of DR-TB spread and will provide insight for further research. Mitigation strategies targeted on baseline patient’s clinical conditions and improving substance-related behaviors might be very important to reduce the burden of primary drug resistance tuberculosis.
Abbreviations
DR-TB, drug-resistant tuberculosis; TB, tuberculosis; RR-TB, rifampicin resistance tuberculosis; MDR-TB, multidrug-resistant tuberculosis; DST, drug susceptibility testing; HIV, human immunodeficiency virus; OR, odds ratio; CI, confidence interval; NTP, National Tuberculosis Control Program.
Data Sharing Statement
All data are included in the manuscript.
Ethical Statement
Ethical clearance was obtained from the institute of public health’s ethical review board on behalf of the University of Gondar. Permission and support letters were also obtained from the Amhara Public Health Institution, the management committee of each hospital, and TB ward heads. Thus, informed consent was waived as we received the institutional support letter, and we do not have contact with patients to access the data. The confidentiality of the data was maintained. Personal identifiers were removed from data files and were stored in a physically separate and secure location. This research follows based on the Helsinki declaration of ethics in human subjects.
Acknowledgments
We were recognized and valued the willingness of all the hospitals and healthcare providers to conduct this research. We the authors were thankful for all the data collectors.
Author Contributions
GMK conceptualizesd and drafted the manuscript. AGM and MHW participated in the study design. All authors contributed to data analysis, drafting or revising the article have agreed on the journal to which the article will be submitted, gave final approval for the version to be published, and agree to be accountable for all aspects of the work.
Funding
No funding was received.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Global Tuberculosis Report. Geneva: World Health Organization; 2019.
2. He XC, Zhang XX, Zhao JN, et al. Epidemiological Trends of Drug-Resistant Tuberculosis in China From 2007 to 2014: a Retrospective Study. Medicine. 2016;95(15):e3336. doi:10.1097/MD.0000000000003336
3. Bloom BR, Atun R, Cohen T, et al. Tuberculosis. In: Holmes KK, Bertozzi S, Bloom BR, Jha P, editors. Major Infectious Diseases. Washington (DC): The International Bank for Reconstruction and Development/The World Bank © 2017 International Bank for Reconstruction and Development/The World Bank; 2017.
4. Ministry of Health-Ethiopia. National Programmatic Management of Drug-Resistant TB (PMDT) in Ethiopia. Ministry of Health-Ethiopia; 2019.
5. Tulu B, Ameni G. Spoligotyping based genetic diversity of Mycobacterium tuberculosis in Ethiopia: a systematic review. BMC Infect Dis. 2018;18(1):140. doi:10.1186/s12879-018-3046-4
6. Yimer SA, Hailu E, Derese Y, Bjune GA, Holm-Hansen C. Spoligotyping of Mycobacterium tuberculosis isolates among pulmonary tuberculosis patients in Amhara Region, Ethiopia. APMIS. 2013;121(9):878–885. doi:10.1111/apm.12046
7. Schito M, Hanna D, Zumla A. Tuberculosis eradication versus control. Int j Infect Dis. 2017;56:10–13. doi:10.1016/j.ijid.2016.11.007
8. World Health Organization. WHO Consolidated Guidelines on Drug-Resistant Tuberculosis Treatment. Geneva: World Health Organization; 2019.
9. Adhvaryu M, Vakharia B. Drug-resistant tuberculosis: emerging treatment options. Clin Pharmacol. 2011;3:51–67. doi:10.2147/CPAA.S11597
10. Yashodhara BM, Huat CB, Naik LN, Umakanth S, Hande M, Pappachan JM. Multidrug and extensively drug-resistant tuberculosis from a general practice perspective. Infect Drug Resist. 2010;3:115–122. doi:10.2147/IDR.S10743
11. Li WB, Zhang YQ, Xing J, Ma ZY, Qu YH, Li XX. Factors associated with primary transmission of multidrug-resistant tuberculosis compared with healthy controls in Henan Province, China. Infect Dis Poverty. 2015;4:14. doi:10.1186/s40249-015-0045-1
12. Li XX, Lu W, Zu RQ, et al. Comparing risk factors for primary multidrug-resistant tuberculosis and primary drug-susceptible tuberculosis in Jiangsu province, China: a matched-pairs case-control study. Am J Trop Med Hyg. 2015;92(2):280–285. doi:10.4269/ajtmh.13-0717
13. Tefera KT, Mesfin N, Reta MM, Sisay MM, Tamirat KS. Treatment delay and associated factors among adults with drug resistant tuberculosis at treatment initiating centers in the Amhara regional state, Ethiopia. BMC Infect Dis. 2019;19(1):489. doi:10.1186/s12879-019-4112-2
14. Alene KA, Yi H, Viney K, et al. Treatment outcomes of patients with multidrug-resistant and extensively drug resistant tuberculosis in Hunan Province, China. BMC Infect Dis. 2017;17(1):573. doi:10.1186/s12879-017-2662-8
15. Bastos ML, Cosme LB, Fregona G. Treatment outcomes of MDR-tuberculosis patients in Brazil: a retrospective cohort analysis. BMC Infect Dis. 2017;17(1):718. doi:10.1186/s12879-017-2810-1
16. Limenih YA, Workie DL. Survival analysis of time to cure on multi-drug resistance tuberculosis patients in Amhara region, Ethiopia. BMC Public Health. 2019;19(1):165. doi:10.1186/s12889-019-6500-3
17. Maharaj J, Ross A, Maharaj NR, Campbell L. Multidrug-resistant tuberculosis in KwaZulu-Natal, South Africa: an overview of patients’ reported knowledge and attitudes. African j Primary Health Care Family Med. 2016;8(1):e1–6. doi:10.4102/phcfm.v8i1.1089
18. Ershova JV, Volchenkov GV, Kaminski DA, et al. Epidemiology of Primary Multidrug-Resistant Tuberculosis, Vladimir Region, Russia. Antimicrob Resist Infect Control. 2015;21(11):2048–2051.
19. Royce S, Falzon D, van Weezenbeek C, et al. Multidrug resistance in new tuberculosis patients: burden and implications. Int j Tuberculosis Lung Dis. 2013;17(4):511–513. doi:10.5588/ijtld.12.0286
20. Shibabaw A, Gelaw B, Wang SH, Tessema B. Time to sputum smear and culture conversions in multidrug resistant tuberculosis at University of Gondar Hospital, Northwest Ethiopia. PLoS One. 2018;13(6):e0198080. doi:10.1371/journal.pone.0198080
21. Yihunie Akalu T, Muchie KF, Alemu Gelaye K. Time to sputum culture conversion and its determinants among Multi-drug resistant Tuberculosis patients at public hospitals of the Amhara Regional State: a multicenter retrospective follow up study. PLoS Med. 2018;13(6):e0199320. doi:10.1371/journal.pone.0199320
22. Kendall EA, Azman AS, Cobelens FG, Dowdy DW. MDR-TB treatment as prevention: the projected population-level impact of expanded treatment for multidrug-resistant tuberculosis. PLoS One. 2017;12(3):e0172748. doi:10.1371/journal.pone.0172748
23. Azman AS, Cobelens FG, Dowdy DW, Song WM. Primary drug resistance of mycobacterium tuberculosis in Shandong, China, 2004–2018. PLoS One. 2019;20(1):223.
24. Mesfin YM, Hailemariam D, Biadgilign S, Kibret KT. Association between HIV/AIDS and multi-drug resistance tuberculosis: a systematic review and meta-analysis. PLoS One. 2014;9(1):e82235. doi:10.1371/journal.pone.0082235
25. Conaty SJ, Hayward AC, Story A, Glynn JR, Drobniewski FA, Watson JM. Explaining risk factors for drug-resistant tuberculosis in England and Wales: contribution of primary and secondary drug resistance. Epidemiol Infect. 2004;132(6):1099–1108. doi:10.1017/S0950268804002869
26. Sharma M, Roy N, Banerjee R, Kishore J, Jakhar A. Determinants of Drug Resistance in Previously-Treated Pulmonary Tuberculosis Patients Registered at a Chest Clinic in South Delhi, India. Cureus. 2019;11(8):e5541.
27. Desissa F, Workineh T, Beyene T. Risk factors for the occurrence of multidrug-resistant tuberculosis among patients undergoing multidrug-resistant tuberculosis treatment in East Shoa, Ethiopia. PLoS One. 2018;18(1):422.
28. Silva DR, Muñoz-Torrico M, Duarte R, et al. Risk factors for tuberculosis: diabetes, smoking, alcohol use, and the use of other drugs. J Brasileiro De Pneumologia. 2018;44(2):145–152. doi:10.1590/s1806-37562017000000443
29. Likhtanskiĭ GP. Experience with the compulsory treatment of patients with pulmonary tuberculosis and alcoholism. Likars’ka Sprava. 1992;1(2):105–107.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
