Back to Journals » Journal of Inflammation Research » Volume 16
Kawasaki Disease Associated Acute Abdomen: Most Require No Surgery
Authors She X , Chen J, Zhou YN, Guo J, Zhao FH, Yi C
Received 11 August 2023
Accepted for publication 7 November 2023
Published 10 November 2023 Volume 2023:16 Pages 5157—5162
DOI https://doi.org/10.2147/JIR.S434982
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Xiang She, Jia Chen, Yu-Neng Zhou, Jun Guo, Feng-Hua Zhao, Cong Yi
Department of Pediatrics, Mianyang Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Mianyang, 621000, People’s Republic of China
Correspondence: Cong Yi, Department of Pediatrics, Mianyang Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Mianyang, 621000, People’s Republic of China, Email [email protected]
Objective: To summarize the clinical features and treatment experiences of patients with Kawasaki disease (KD)-associated acute abdomen (KD-AA).
Methods: We conducted a retrospective case-control study of patients with KD-AA treated at our hospital between January 2006 and November 2022.
Results: Of the 917 children with KD, 43 (4.7%) presented with AA. Of these, 33 with complete information were included in the KD-AA group. Patients with KD-AA were significantly older, with higher neutrophil rate, C‐reactive protein, procalcitonin, and alanine transaminase levels and lower hemoglobin, albumin, and serum sodium levels. Additionally, more patients with KD-AA presented with aseptic meningitis and KD shock syndrome than those with KD alone (all p< 0.05). The two groups did not differ in the incidence of intravenous immunoglobulin (IVIG) resistance, incomplete KD, or coronary artery abnormalities. All patients received aspirin and IVIG therapy, with nine receiving a second dose of IVIG and 11 receiving corticosteroids. Only two patients with KD-AA underwent surgery, and the prognosis of all patients with KD-AA was good.
Conclusion: KD-AA should be suspected in febrile children with abdominal symptoms. Prompt diagnosis of KD-AA is important for early effective treatment to avoid unnecessary surgical harm. KD, complicated by acute abdomen, has a good prognosis.
Keywords: Kawasaki disease, acute abdomen, clinical manifestation, treatment
Introduction
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is an acute febrile disease characterized by non-specific systemic vasculitis of small-to-medium-sized vessels.1 Untreated patients have a 15–25% chance of developing coronary artery abnormalities (CAAs),2 which are the primary causes of acquired heart disease among children in developed countries.3 Acute abdomen is rare in KD and the incidence is 4.6%.4 Without adequate clinical characteristic criteria for KD during the acute febrile phase, these patients are easily misdiagnosed as general surgical emergencies and frequently treated with unnecessary operations, leading to delayed treatment and increased risk of CAAs. We performed this case-control study to summarize the clinical features and treatment experiences of patients with KD-associated acute abdomen (KD-AA) and compare with KD patients without AA.
Patients and Methods
This case-control study was approved by the Mianyang Central Hospital Ethics Committee. The study complied with the Declaration of Helsinki. The informed consent was waived as the study is retrospective (Waiver No. S20230322-01). All participant data were strictly maintained with confidentiality.
We retrospectively reviewed the medical records of patients with KD who were diagnosed with complete or incomplete KD at the Department of Pediatrics, Mianyang Central Hospital, School of Medicine, University of Electronic Science and Technology of China, between January 2006 and November 2022. Two pediatricians diagnosed complete or incomplete KD based on the criteria proposed by the American Heart Association.5 Complete KD was defined as having prolonged fever for ≥5 days and the presence of ≥4 of the following 5 principal clinical features: oral changes, rash, extremity changes, cervical lymphadenopathy, and non-purulent conjunctivitis. Incomplete KD patients had fever lasting ≥5 days but fewer than 4 of the 5 principal clinical features.
Case patients (KD-AA patients) were defined as patients with KD complicated by acute abdomen, which refers to intra-abdominal pathology, including thoracic pathology, with an onset of less than 1 week that may require urgent interventions, such as surgery, mainly including acute appendicitis, cholecystitis, intestinal obstruction, acute pancreatitis, etc.6 Case patients were excluded when they had incomplete laboratory data or had an acute abdomen caused by infections, trauma, or etiologies other than KD. For each case patient, we randomly identified four sex-matched KD patients without acute abdomen as the control group. We retrospectively collected and analyzed the medical records of these children, including demographic data, clinical information, laboratory parameters, echocardiogram data, treatment, and outcomes.
IVIG resistance was defined as persistent or recrudescent fever (>38°C) at least 36 hours and <7 days after completion of first IVIG infusion.5 KD shock syndrome (KDSS) was defined as patients with KD presenting systolic hypotension for age, a sustained decrease in systolic blood pressure from baseline of ≥20%, or clinical signs of poor perfusion.7 CAAs were determined based on normalized Z scores for body surface area, including both dilations (2≤z-score<2.5) and aneurysms (z-score≥2.5).5
Data analysis was performed using IBM SPSS Statistics 22.0. Normality was tested using Shapiro–Wilk test. Continuous data were expressed as mean and standard deviation (mean±SD) for normal distribution or as median (interquartile range, IQR) for non-normal distribution and analyzed by Student’s t-test for parametric data or Mann–Whitney U-test for non-parametric data. Categorical data were expressed as number (percentage) and analyzed by Chi-square or Fisher’s exact test, when appropriate. P values<0.05 considered statistically significant.
Results
Between January 2006 and November 2022, 917 patients (551 boys and 366 girls) were diagnosed with KD. Of these, 43 (27 boys and 16 girls) had a clinical diagnosis of co-existing acute abdomen, corresponding to a prevalence of AA in KD of 4.7% (43/917). Cholecystitis and intestinal obstruction were the most frequent acute abdominal conditions observed in 29 (67.4%) and 11 (25.6%) patients, respectively. In addition, there were six (14.0%) patients with acute appendicitis, three (7.0%) with acute pancreatitis, three (7.0%) with acute peritonitis, and one (2.3%) each with intestinal volvulus, ileal perforation, and intussusception (Table 1). Among them, 11 had two or more concurrent acute abdominal diseases.
 |
Table 1 Diagnoses of KD-AA Patients |
After excluding those with incomplete laboratory data, 33 patients were included in the KD-AA group. Patients’ clinical characteristics are shown in Table 2. The KD-AA group comprised 21 boys and 12 girls. Patients with KD-AA were statistically significantly older (4.0±2.8 years vs 2.6±1.9 years, p=0.011). The two groups had no significant difference in sex or the diagnostic criteria for complete KD. However, non-specific symptoms such as vomiting, tachypnea, irritability, and aseptic meningitis were significantly more frequent in the KD-AA group than in the KD group (p=0.003, p<0.001, p=0.005, and p=0.001, respectively). As most patients were too young to articulate their symptoms, abdominal pain was not included in the statistical evaluations.
 |
Table 2 Clinical Characteristics and Laboratory Findings of Patients with KD-AA or KD |
Laboratory findings of the two groups are summarized in Table 2. We found that the neutrophil rate, C-reactive protein, procalcitonin, and alanine transaminase levels were significantly higher in the KD-AA group than in the KD control group (p=0.001, p=0.004, p<0.001, and p=0.018, respectively). However, hemoglobin, albumin and serum sodium levels were lower in the KD-AA group than in the KD control group (p<0.001, p<0.001, and p=0.005, respectively). Other laboratory parameters showed no significant differences between the two groups.
The treatment and outcomes of the two groups are presented in Table 3. After KD diagnosis, all patients received aspirin and intravenous immunoglobulin (IVIG) therapy, and most showed rapid clinical improvement. Only two patients with KD-AA underwent surgery. One patient was diagnosed with acute appendicitis and underwent a laparoscopic appendectomy at a local hospital before admission, with no postoperative remission of symptoms. The other patient developed ileal perforation and underwent resection of the necrotic intestine and ileostomy. Pathological examination revealed extensive necrosis with a massive infiltration of inflammatory cells. Moreover, none of the patients with KD-AA excluded from this study underwent surgery. The incidence of IVIG resistance was higher but statistically insignificant in the KD-AA group compared to the KD group (p=0.13). These patients required further therapeutic intervention, consisting of a second dose of IVIG and/or corticosteroids. Compared with the KD group, the KD-AA group was significantly more likely to be treated with corticosteroids and develop KDSS (p<0.001, p=0.001, respectively). There were no significant differences in the incidence of incomplete KD or cardiac complications (CAAs, valve regurgitation, and pericardial effusion) between the groups (all p>0.05). Furthermore, KD-AA patients were hospitalized for two days longer than KD patients (p=0.009). All patients were discharged with good outcomes. On long-term follow-up, no residual sequelae were observed in the digestive system.
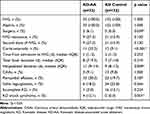 |
Table 3 Treatment and Outcomes of Patients with KD-AA or KD |
Discussion
KD is a systemic inflammatory reaction that may affect various organ systems, including the cardiovascular, nervous, urinary, respiratory, hematological, musculoskeletal, and gastrointestinal systems.8 Gastrointestinal symptoms occur in 25–30% of patients with KD as markers of severity;9 common clinical manifestations include vomiting, diarrhea, abdominal pain, and abdominal distension. However, acute abdomen is rare in KD. In our study, 43 patients had KD-AA (4.7% of the total patients with KD). Although the present study showed similar results regarding the prevalence of acute abdomen in KD as in previous studies,4 studies are still insufficient, as most are case reports.
Each organ of the digestive system can be affected. KD-AA reported in this study included cholecystitis (67.4%), intestinal obstruction (25.6%), acute appendicitis (14.0%), acute pancreatitis (7.0%), acute peritonitis (7.0%), intestinal volvulus (2.3%), ileal perforation (2.3%), and intussusception (2.3%). Vomiting and diarrhea are the most common presenting features reported in previous studies.4,10,11 The pathogenesis of acute abdomen in KD probably relates to vasculitis of small-to-medium-sized vessels in the abdominal viscera.
The demographics of our patients with KD-AA were similar to those of previous studies; that is, a male predominance and a trend toward older age were observed.4,10,12,13 In addition, as in previous reports, the prevalence of involvement of organs other than the digestive tract in patients with KD-AA was higher than that in KD patients.4 Our data also corroborate previously described laboratory abnormalities in patients with KD-AA, including higher C-reactive protein and alanine transaminase levels and lower hemoglobin and albumin.4,9,13 Furthermore, we found that KD-AA patients had higher levels of neutrophil percentage and procalcitonin and lower serum sodium level, which has not been described in other studies. These results may be related to the higher degree of inflammation present in KD-AA.
In reported patients with KD presenting with an acute abdomen, almost all patients were treated with surgery aggressively because of the failure to consider KD in these patients initially; the symptoms did not improve postoperatively. However, symptoms improved rapidly with prompt diagnosis and adequate treatment of KD with IVIG and aspirin.4,13–15 In our study, all but two patients were treated with medical treatment only and showed improvement. KD patients with abdominal symptoms are at relatively higher risk of IVIG resistance and developing coronary aneurysms, because of the delayed diagnosis of KD.9 However, we found no significant difference in IVIG resistance or CAAs between the groups, aided by the increased awareness of KD-AA. It is additionally notable that KD-AA is associated with higher incidence of KDSS, that means KD-AA patients maybe develop more severe disease, that is similar than other previous literature reports.16,17 Therefore, the prompt diagnosis and treatment of KD is important for both management and prognosis.
The strength of this study is the large number of patients with KD-AA we studied and the results added to the limited literature on KD-AA. This study had some limitations. First, there may have been bias due to the study′s retrospective design. Second, the single-center sample may have affected the generalizability of the results. Therefore, multicenter studies are recommended.
In conclusion, our findings indicate that the incidence of acute abdomen is relatively low among patients with KD. Patients with KD-AA are more likely to exhibit a more severe inflammatory burden and develop aseptic meningitis and KDSS than those with KD alone. KD-AA should be considered in the differential diagnosis of febrile children with abdominal symptoms. Supportive medical treatments should be initially considered. Once KD is diagnosed, standard therapy with IVIG and aspirin should be administered immediately to avoid unnecessary surgical harm. However, prompt surgery is necessary when patients present with serious complications such as strangulated/mechanical bowel obstruction, infarction, or perforation. The overall prognosis of patients with KD-AA is satisfactory.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This study was supported by a research project from Mianyang Central Hospital (No.2023KY025).
Disclosure
The authors have no relevant financial or non-financial interests to disclose.
References
1. Burns JC, Glodé MP. Kawasaki syndrome. Lancet. 2004;364(9433):533–544. doi:10.1016/S0140-6736(04)16814-1
2. Kato H, Sugimura T, Akagi T, et al. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation. 1996;94(6):1379–1385. doi:10.1161/01.CIR.94.6.1379
3. Eleftheriou D, Levin M, Shingadia D, Tulloh R, Klein NJ, Brogan PA. Management of Kawasaki disease. Arch Dis Child. 2014;99(1):74–83. doi:10.1136/archdischild-2012-302841
4. Zulian F, Falcini F, Zancan L, et al. Acute surgical abdomen as presenting manifestation of Kawasaki disease. J Pediatr. 2003;142(6):731–735. doi:10.1067/mpd.2003.232
5. McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–e999. doi:10.1161/CIR.0000000000000484
6. Mayumi T, Yoshida M, Tazuma S, et al. Practice guidelines for primary care of acute abdomen 2015. J Hepatobiliary Pancreat Sci. 2016;23(1):3–36. doi:10.1002/jhbp.303
7. Kanegaye JT, Wilder MS, Molkara D, et al. Recognition of a Kawasaki disease shock syndrome. Pediatrics. 2009;123(5):e783–e789. doi:10.1542/peds.2008-1871
8. Lee W, Cheah CS, Suhaini SA, et al. Clinical manifestations and laboratory findings of Kawasaki disease: beyond the classic diagnostic features. Medicina. 2022;58(6):734. doi:10.3390/medicina58060734
9. Fabi M, Corinaldesi E, Pierantoni L, et al. Gastrointestinal presentation of Kawasaki disease: a red flag for severe disease? PLoS One. 2018;13(9):e0202658. doi:10.1371/journal.pone.0202658
10. Yaniv L, Jaffe M, Shaoul R. The surgical manifestations of the intestinal tract in Kawasaki disease. J Pediatr Surg. 2005;40(9):e1–e4. doi:10.1016/j.jpedsurg.2005.05.063
11. Colomba C, La Placa S, Saporito L, et al. Intestinal involvement in Kawasaki Disease. J Pediatr. 2018;202:186–193. doi:10.1016/j.jpeds.2018.06.034
12. Huang YN, Liu LH, Chen JJ, Tai YL, Duh YC, Lin CY. Appendicitis as a leading manifestation of Kawasaki Disease in older children. Children (Basel). 2022;9(2):193. doi:10.3390/children9020193
13. Kuroda K, Stottlemyre M. Acute appendicitis associated with Kawasaki disease: case report and review of the literature. Cureus. 2021;13(10):e18997. doi:10.7759/cureus.18997
14. Velez-Tirado N, Ridaura-Sanz C, Venegas-Montoya E, et al. Acute abdomen in Kawasaki disease. Indian J Pediatr. 2019;86(12):1151–1152. doi:10.1007/s12098-019-03048-6
15. Hou JW, Chang MH, Wu MH, Lee CY. Kawasaki disease complicated by gallbladder hydrops mimicking acute abdomen: a report of three cases. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1989;30(1):52–60.
16. Gámez-González LB, Murata C, Muñoz-Ramírez M, Yamazaki-Nakashimada M. Clinical manifestations associated with Kawasaki disease shock syndrome in Mexican children. Eur J Pediatr. 2013;172(3):337–342. doi:10.1007/s00431-012-1879-1
17. Yi C, She X, Chen J. Kawasaki disease complicated with shock syndrome, macrophage activation syndrome, and acute abdomen in children: two case reports. Front Pediatr. 2023;11:1152242. doi:10.3389/fped.2023.1152242
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
