Back to Journals » Advances in Medical Education and Practice » Volume 13
Jordanian Radiologists’ Perspectives and Application of Evidence-Based Radiology in Clinical Practice
Authors Alakhras M , Al-Mousa DS , Alwawi D
Received 20 November 2021
Accepted for publication 17 February 2022
Published 23 February 2022 Volume 2022:13 Pages 177—188
DOI https://doi.org/10.2147/AMEP.S348015
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Maram Alakhras,1 Dana S Al-Mousa,1 Duaa Alwawi2
1Department of Allied Medical Sciences, Jordan University of Science and Technology, Irbid, Jordan; 2Department of Occupational Therapy, University of Jordan, Amman, Jordan
Correspondence: Maram Alakhras, Tel +96227201000 Ext 26947, Email [email protected]
Purpose: To evaluate radiologists’ education, knowledge and skills of research, attitude toward evidence-based radiology (EBR), understanding of terms and use of related published work in clinical practice and the association between these variables and sociodemographic characteristics. We also aim to assess the availability of resources and to identify sources and the main barriers to implementing EBR.
Materials and Methods: A total of 87 radiologists completed a questionnaire, which consisted of eight sections related to radiologists’ demographic characteristics, and EBR-related questions. Descriptive statistics were used, and the association between EBR-related parts and sociodemographic characteristics was performed.
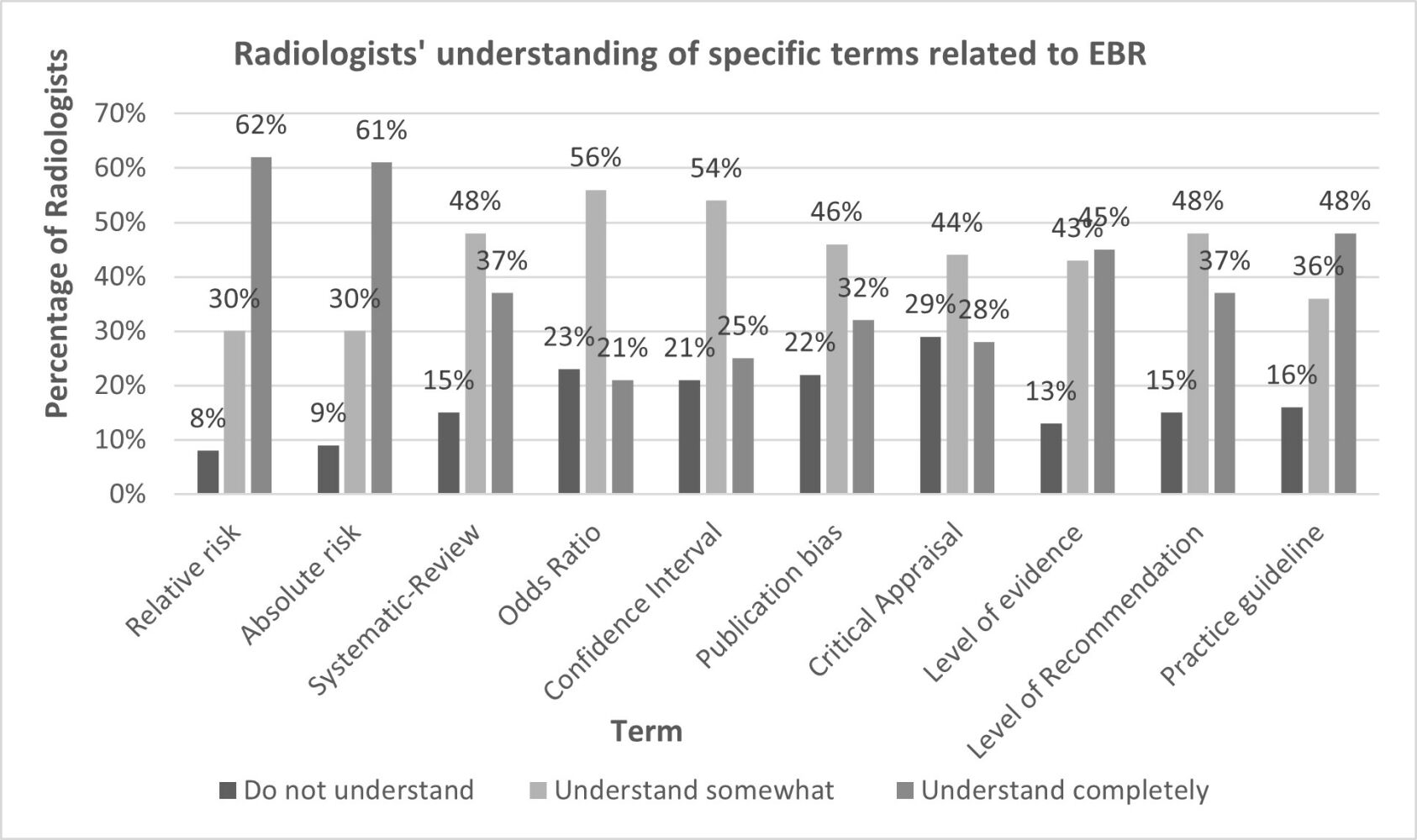
Results: Ninety-three percent of the radiologists believed that EBR is necessary in practice. Only 40% received formal training in search strategies and 29.9% in critical appraisal of research literature during academic preparation. Moreover, 21– 62% of the respondents completely understand specific terms related to EBR. Sixty-three percent stated that they can access relevant databases and the Internet at workplace. Research articles were only used by 24% to make a clinical decision. Almost 50% reported that they read or reviewed ≤ 1 article per month. The primary barrier to implementing EBR was the lack of colleagues’ support. Understanding terms and the number of articles used in clinical decision were significantly related to education (P-value=0.001, 0.007) and hospital section (P-value=0.002, 0.027) respectively.
Conclusion: Radiologists showed positive attitude toward EBR. However, there is a lack in information resources, colleagues’ support, use of published literature, understanding of research terms and the ability of radiologists to access relevant databases at workplaces.
Keywords: clinical decision, research evidence, evidence-based radiology
Graphical Abstract:
Introduction
The field of medical imaging has grown tremendously in the last three decades with the introduction of new technology, imaging techniques, noninvasive diagnostic examinations, and therapeutic procedures. These developments have been accompanied by a large volume of both peer reviewed and non-peer reviewed medical literature. In order to support evidence-based practice, it is important for radiologists to be able to critically assess the available literature and not simply to accept recommendations from experts.1 However, anecdotally, it is known that radiologists do tend to rely on habits or “experts in the field” for decision-making in their professional practice.
Evidence-based radiology (EBR) describes medical decision-making based on the combination of three main components: the best available medical imaging research evidence, clinical expertise and patient’s expectations.1 The clinical expertise component involves the skills and ability of the radiologist to assess patient history and presentation and to make important decisions in regards to which imaging tests individual patients will most benefit from. As each individual has values and preferences that should also be considered when making clinical decisions, patient’s expectations form a vital EBR component.2 In radiology, the availability of multiple diagnostic and interventional imaging modalities combined with rapid advancement in technology is known to have resulted in radiologists being challenged to assimilate all the information needed to render high-quality cost-effective care.3,4 Radiologists must actively participate in research activities to be able to manage with and be responsive to the continuous development of advanced diagnostic and therapeutic procedures. Hence, the implementation of EBR in both academic and clinical practice should be enforced and facilitated in order to enhance clinical outcomes and quality of life for patients.5
The incorporation of evidence into practice requires radiologists to both understand the published literature and to be able to critically evaluate the strength of the evidence presented. These skills are not usually incorporated into radiology academic curriculums, so radiologists may have limited knowledge and skills in EBR.2 Short courses in evidence-based medicine have been shown to significantly improve a physicians’ knowledge and skills.6 There is however a limited number of studies focused on radiologists’ application of evidence-based practice in medical imaging worldwide.2,7–9 In Jordan, a few studies have investigated evidence-based practice in medicine targeting medical doctors who agreed that research findings may improve patient care.10 However, only a few of the participants understood the technical terms used in evidence-based medicine. Participants noted limited resources and facilities, and high patient numbers as the two major barriers to practicing evidence-based medicine.10 These barriers may also apply to the field of radiology; however, no studies have examined evidence-based practice in radiology.
The aim of this study was to evaluate the level of education, knowledge, skills and attitude toward EBR, understanding of terms related to EBR and use of related published work in clinical practice among Jordanian radiologists; and to assess the association between these variables and sociodemographic characteristics. Additionally, the study sought to assess the availability of EBR resources and to identify potential barriers to implementing EBR in Jordan.
Materials and Methods
Participants and Study Design
Ethical approval was obtained by the Human Ethics Research Committee at Jordan University of Science and Technology (Research number 20190248), and informed written consent was obtained from all participants prior to completing the questionnaire. All radiologists (board-certified specialists in radiology) and radiology residents working at the six main public and private hospitals in the north and central regions of Jordan were invited to participate in the study. A total of 87 radiologists agreed to participate. A self-administered questionnaire was distributed and collected by two research assistants who were familiar with the aims and the details of the study.
Instrument
The questionnaire used in the current study was adapted from a survey used in previous work.8,11–15 The survey consisted of eight sections. The first section included questions related to radiologist demographic and professional characteristics including age, gender, level of education, hospital section, hours worked per week, years of experience, average daily workload, and if the radiologist worked as a clinical instructor for students. The second section included seven 5-point Likert-type agreement scale (strongly agree to strongly disagree) questions related to radiologists’ education, knowledge and research skills. The third section examined radiologists’ personal attitude toward using EBR, which consisted of 15 statements using the same 5-point agreement scale. The fourth section listed 10 terms related to the use of research. Radiologists were asked to rate their understanding of these terms using a 3-point scale (do not understand, understand somewhat, understand completely). The fifth part included six questions concerning the availability of resources and support provided to promote EBR and the radiologists were asked to answer these questions with a yes, no or do not know responses. In the sixth section, the radiologists were requested to rate their use of six clinical decision-making sources (personal experience, colleagues’ opinions, supervisor’s or expert opinion, internet, books, research reviews and articles) using a 5-point scale (never to always). The seventh section included two questions related to the frequency of EBR reading and use of research in clinical practice. Information regarding the barriers to the use of EBR in clinical practice was included in the last section where each radiologist was asked to select up to three barriers.
Data Analysis
Statistical Package for Social Sciences SPSSTM software was used to analyze the data. Descriptive statistics including frequency, percentage, mean, and standard deviation were used to describe demographic and EBR-related data. The percentage of radiologists who agreed with each statement was calculated by combining “strongly agree” and “agree” answers and the percentage of radiologists who disagreed was calculated by combining “strongly disagree” and “disagree” answers.
For the purpose of analysis and to calculate mean values, the 5-point agreement scale used for the attitude and education, knowledge and skills sections were coded on a scale from 1 (strongly disagree) to 5 (strongly agree). The scale of understanding of terms was coded from 1 (do not understand) to 3 (understand completely) and the responses of the use of published research part were given scores from 1 (≤1 article) to 5 (>16 articles).
Study variables were checked for normality using Shapiro–Wilk test, which indicated that all variables were normally distributed. Analysis of means was used to test the association between participants’ responses according to their demographic and professional characteristics using independent t-test to compare the means between two groups and one-way ANOVA to compare the means among three or more groups. A significant finding was set at a P-value of <0.05.
Results
Of the 134 radiologists and radiology residents invited to participate in the study, 107 returned the questionnaire, 20 were excluded from the study due to missing data with only 87 included in the final analysis. As indicated in Table 1, more than half of the participating radiologists were aged between 31 and 40 years and 61% were males. More than two-thirds (68%) held a Bachelor’s degree and 32% had completed higher education; 63% worked in public hospitals. Almost one-half of respondents had 4–10 years of radiology experience and almost the same percentage worked more than 40 hours per week and participated in continuing education courses. A minority (13%) worked as clinical instructors for radiology students.
 |
Table 1 Socio-Demographic and Professional Characteristics of Study Participants (N= 87) |
The reliability coefficient (Cronbach’s alpha α values) of the attitude and knowledge of radiologists towards EBR is calculated as 0.81 for personal attitude towards the use of EBR and 0.83 for education, knowledge, and research skills.
In terms of statements related to education, knowledge and skills of EBR, 69% of the participants reported that they had learned the foundations of EBR as part of their academic preparation, 40% received formal training in search strategies for finding research and 30% received formal training in critical appraisal of research literature. A range from 46% to 55% of the respondents stated that they were familiar with medical search engines and that they were confident to find, and critically review relevant research. Almost 60% reported using radiology-based databases to find key literature regarding clinical practice (Table 2).
 |
Table 2 Distribution of Responses Related to Education, Knowledge and Skills and Personal Attitudes Toward the Use of Evidence-Based Radiology (EBR) |
Table 2 shows that in all positively worded statements, more than half of the respondents held a positive belief and attitude toward the use of EBR. Of those, the data showed that more than 80% of the participants agreed or strongly agreed that EBR is necessary in the practice of radiology (Statement 8: 93%), and that research findings are useful in day-to-day practice (Statement 9: 83%). Additionally, 84% of respondents believed that EBR improves the quality of patient care and 82% were interested in learning or improving skills necessary to EBR practice. Several (n=56) respondents believed that EBR does not take into account patient preferences (49%) and that there is a definitive line between research and practice (n=43, 64%). Moreover, 53% of the respondents considered that strong evidence was lacking to support most of the radiology interventions used in practice.
The results of the current study showed that only 21% of the respondents completely understood the term “odds ratio” and 62% the term relative risk. The list of terms and level of understanding of each term are reported in Table 3.
 |
Table 3 Distribution of Responses Related to Understanding of Specific Terms Related to EBR, (N=87) |
Table 4 shows that less than half the respondents answered yes to the questions related to the support provided by the facility to use research in practice and the availability of professional journals in paper form, a resource person to assist in implementing EBR and financial support from their facility to attend educational meetings and conferences. A majority (63.2%) of respondents stated that they had access to the Internet and the ability to access relevant databases at the facility they worked in.
 |
Table 4 Availability of Resources and Support to Promote EBR |
As shown in Table 5, 70% of the respondents relied always on their own individual experience as the main source to make decisions in clinical practice, while research reviews and articles were used always by only 24% of the respondents.
 |
Table 5 Responses Related to Sources Used to Make a Clinical Decision in Radiology Practice |
As indicated in Table 6, the analyses of the association between sociodemographic characteristics and EBR-related sections indicated that the level of participants’ understanding of terms and the number of articles used in clinical decision-making were significantly related to their level of education (P value = 0.001, 0.047) and section of the hospital (P value = 0.002, 0.027), respectively.
 |
Table 6 Associations Between Background Characteristics and Education and Knowledge, Attitude, Use of Research and Understanding of Terms of EPR |
Almost half the respondents reported that they read or reviewed less than one article relevant to their professional practice per month (Figure 1). A small proportion (28% and 33%) reported reading and reviewing between two and five articles per month, respectively.
 |
Figure 1 Distribution of responses related to the number of articles read and used in decision-making per month. |
Figure 2 shows that the three most reported barriers to EBR were the lack of collective support among colleagues (58.6%), lack of information resources (43.7%) and insufficient time (40.2%).
 |
Figure 2 Distribution of responses related to barriers to EBR. |
Discussion
This study included 87 Jordanian radiologists working at the main public and private hospitals in the North and Central regions of Jordan. The number of radiology specialists in these hospitals ranged from 4 to 15 with an average of 8 radiologists per hospital, while the number of radiology residents ranged from 13 to 39 with an average of 30 per hospital. The average number of general radiography, computed tomography (CT) and magnetic resonance imaging (MRI) machines in each hospital was 5, 2 and 2 respectively. To become a radiologist in Jordan, a medical student must undertake a relevant Bachelor’s degree (Doctor of Medicine) for at least 6 years in a governmental university. After successfully completing the degree, the physician receives a temporary professional licence in general medicine. After that, physicians undertake a 12-month internship in all four major specialties: surgery, pediatrics, internal medicine and obstetrics and gynecology to receive a permanent professional licence. After the internship, a 4-year residency program is required to become a qualified resident in radiology. At the end of each year of residency, the physician is required to pass a theoretical and a practical exam. To become a radiology specialist (gain a professional licence in radiology), the physician must pass the Jordanian board exam, which is divided into two parts, one a prerequisite for the second is held during and one after completing the residency program. For job ranking from one level to another, depending on the level, the radiologist must complete 5–7 years of practice, perform three to five research studies, and attend 200–250 hours of conferences.
Education, Knowledge and Skills
As the field of radiology continues to be rapidly evolving with constant advances in diagnostic and therapeutic procedures, this represents a real challenge to radiologists to maintain currency around the high number of published clinical findings. It is also important to mention that only a fraction of the available articles are relevant to any individual’s practice, which makes the task even more challenging and the effort required time consuming.16 Therefore, it is desirable that EBR education and training is included as a part of academic preparation to provide the graduate radiologist with the research skills required to inform their clinical decisions. Radiologists not only need to be able to find relevant literature but to develop skills that allow them to critically appraise the available research and integrate it into their practice. In the current study, 69% of the respondents reported having learnt the foundations of EBR; however, only a low percentage of respondents received formal training in search strategies (40%) and in critical appraisal of research literature (30%) as part of their academic preparation. About half (49%) of the respondents were familiar with the key medical search engines and 60% used radiography radiology-based databases to find literature related to their clinical practice. However, a lesser percentage was confident in finding (55%) and critically reviewing (46%) relevant research to answer their clinical questions. This low-level of confidence can be attributed to the small number of articles (one or less) read and used in clinical decision-making per month by almost half the participants and to the limited understanding of research terminology as shown by the current study. According to these findings, we recommend that radiologists should be directed to available resources that provide the basic skills of EBR through a step-by-step series of resources to familiarize them with relevant search engines and how to use them efficiently.16–21 We also suggest formal education and training dedicated to EBR for radiologists to improve their research skills. A previous study reported that an intensive three-day course on evidence-based practice for physicians from various backgrounds and training levels resulted in a significant improvement of knowledge and skills.6 Development of interactive online courses with supervised critical appraisal may also be useful in increasing radiologists’ EBR knowledge and skills.
Radiologists’ Attitude Toward EBR
The results of the current study demonstrated a positive attitude towards EBR with the majority of participants (>80%) believing in the importance of EBR and in the value of research findings for clinical practice and the quality of patient care. These findings were similar to the results reported by other studies performed on radiologists and physicians.7,22,23 In congruence with other studies,8,24 the majority of our respondents (82%) were interested in learning or improving the skills necessary to successfully undertake EBR. However, about half the respondents believe that EBR did not consider patient preferences (49%) and they stated that strong evidence is lacking (53%) to support most of the radiology interventions used in practice. These attitudes and beliefs concerning EBR may be enhanced by providing accelerated educational programs.25
Understanding of Terms Related to EBR
It is crucial that radiologists understand research-related terms that allow them to comprehend the research methodology needed to analyze the available evidence before making a clinical decision. While the majority (62%) of participants fully understood the terms “relative risk” and “absolute risk”, only a small percentage completely understood other common terms such as “odds ratio” (21%) and “confidence interval” (25%). This limited understanding of the terms used in evidence-based practice (EBP) was also reported by other studies.11,12,23 This strongly highlights the need for EBR education for radiologists including familiarization with the main research terminology used in medical research.
Availability of Resources and Support to Promote EBR
The results showed that 63% of the respondents had access to relevant databases through the Internet, and 41% had access to professional journals in paper format. A small percentage of participants reported that their facility supported the use of research in clinical practice (26%). A previous study reported that radiologists and trainees preferred online resources to answer both general and specific imaging questions.26 Introducing radiologists to reliable web-based resources including EBR educational material, webinars, and online journals may be more engaging. The development of quality medical imaging mobile applications can also be an attractive tool to radiologists and trainees.
In our study, only 32% of the respondents indicated that their facility provided financial support to attend educational meetings. Attending conferences and scientific meetings is an important way to learn about current and best practices in the field and to develop professional knowledge. This is of particular importance in radiology due to the fast-paced advances in technology. However, the high cost of conference attendance may limit participation and institutional or grant funding can reduce out-of-pocket participant expenses.
The current study also showed that only 41% of the respondents reported that a resource person was available to assist them with implementing EBR. The presence of a librarian or a clinical evidence-based information specialist to assist in finding relevant literature may relieve the burden faced by radiologists and reduce the amount of time spent by them to identify, find and review research.
Sources to Make a Clinical Decision
The traditional source of knowledge in medical education has focused on experts in the field, which assumes that an expert in a specific area has sufficient experience in clinical decision-making.27 However, it must be noted that an individual’s experience may lack objectivity, and therefore clinical decision-making should be based on the best peer reviewed evidence. In the current study, 93% of the respondents stated that they “always” or “often” use their personal experience and around 76% used their colleagues or expert opinions. However, a lower percentage of respondents stated that they always or often rely on the use of the internet (65%), books (39%) and research articles (49%) to make a clinical decision. The lack of resources in the workplace, which was identified as one of the main barriers to undertaking EBR, may be a key reason as to why the respondents reported relying more on their personal experience, their colleagues’ or expert opinions.
Attention to Literature
Research findings in radiology are often biased by weakness in study methodology and/or small sample size,27 so it is important for radiologists to not only find and read relevant published work but also to review, critically appraise and evaluate the quality of the available research to avoid making the wrong clinical decision. Our participants’ attention to the literature was limited with almost half the respondents reading or reviewing less than one article relevant to their work per month and a small proportion (28% and 33%) reading and reviewing between two and five articles in each month, respectively. This might be partially attributed to insufficient time and the lack of resources, which were identified as two of the main barriers to EBR.
Barriers to EBR
Apart from a lack of information resources and insufficient time, a lack of collective support among colleagues was reported as the third main barrier to EBR. Similarly, a lack of collective support and limited access to literature were also identified by physicians in other studies as key barriers to applying evidence-based practice.28 These impediments to EBR need to be addressed to improve the effective and efficient use of the available evidence. It was believed that working together and the exchange of information between colleagues could help make the right clinical decisions. Academic and medical institutions should make efforts to increase intra-professional learning through support between colleagues, which can be achieved by facilitating face-to-face discussions and establishing online dashboards. Also, institutions should update their resources to facilitate EBR processes, including Internet access in the workplace, medical databases, a resource person to assist in the implementation of EBR and paper-based articles.
Inadequate time for EBR in clinical practice was a barrier reported by our participants and in other studies.23,29–31 This highlights the importance of establishing a system that allows quick identification of the best available evidence for clinical decision-making and to allocate dedicated time for research activities and EBR education in workplaces.
While sociodemographic characteristics were not significantly associated with attitude, knowledge and skills, the results showed that the radiologists’ understanding of terms related to EBR was significantly associated with their level of education. Those with higher education (Masters and PhD degrees) had a greater understanding than those with a Bachelor’s degree (P-value = 0.001). Similar findings were reported by other studies,32 which can be explained by research experience and more exposure to research-related terminology through higher education. The results also showed that participants who work at private hospitals had a higher level of understanding of EBR terminology (P-value = 0.002). This can be partially attributed to the better knowledge, skills and education shown by radiologists working at private hospitals compared with those who worked at public hospitals, even though the difference was not significant.
The current study showed that participant use of research in terms of the number of articles read and reviewed per month was also associated with educational level and hospital section. Participants with a higher level of education indicated lower use of research than Bachelor’s degree (only) holders, this result was unexpected. Future research is required to test if there is a correlation between the different aspects of EBR identified in the current study.
This study has some limitations including a small sample size. We recommend undertaking a larger study to include all areas of Jordan, not only the North and Central regions. However, we believe that our sample is representative of the population from which it was drawn. Another limitation is that the participants were asked if they “understood” research-related terms on a 3-point Likert scale. It would have been much more informative if we had tested the understanding of participants using a set of multiple-choice questions for example or numerical questions in which participants were to calculate the absolute risk and the relative risk of having a certain condition for example.
Conclusions
The radiologists participating in this study in general demonstrated a positive attitude toward EBR. However, a lack of information resources, colleague support, use of published literature in clinical practice, understanding of research terms and access to relevant databases in the workplace were identified. Understanding the participating radiologists’ beliefs, attitudes, skills and their perceived barriers to EBR are important steps towards improving EBR in radiology practice. Improved EBR education in the undergraduate academic curriculum, internship, and residency programs, and in platforms used in the workplace is desirable. Continuous efforts are also needed to ensure availability and ease of access to peer-reviewed resources. The results of this research may contribute to providing the necessary baseline data for these improvements.
Acknowledgments
The authors would like to thank all participating radiologists.
Disclosure
The authors report no conflicts of interest in this work.
References
1. García Villar C. Evidence-based radiology for diagnostic imaging: what it is and how to practice it. Radiol Engl Ed. 2011;53(4):326–334. doi:10.1016/j.rxeng.2011.02.001
2. Tong A, Mahady SE, Craig JC, Lau G, Peduto AJ, Loy C. Radiologists’ perspectives about evidence-based medicine and their clinical practice: a semistructured interview study. BMJ Open. 2014;4(12):e006199. doi:10.1136/bmjopen-2014-006199
3. Evidence-Based Radiology Working Group. Evidence-based radiology: a new approach to the practice of radiology. Radiology. 2001;220(3):566–575. doi:10.1148/radiol.2203001465
4. Medina LS, Blackmore CC, Applegate KE, eds. Evidence-Based Imaging: Improving the Quality of Imaging in Patient Care.
5. Lehane E, Leahy-Warren P, O’Riordan C, et al. Evidence-based practice education for healthcare professions: an expert view. BMJ Evid Based Med. 2019;24(3):103–108. doi:10.1136/bmjebm-2018-111019
6. Fritsche L. Do short courses in evidence based medicine improve knowledge and skills? Validation of Berlin questionnaire and before and after study of courses in evidence based medicine. BMJ. 2002;325(7376):1338–1341. doi:10.1136/bmj.325.7376.1338
7. Anuradha C, Jacob KS, Shyamkumar NK, Sridhar G. Evidence-based practice in radiology: knowledge, attitude and perceived barriers to practice among residents in radiology. Eur J Radiol. 2013;82(5):894–897. doi:10.1016/j.ejrad.2013.01.026
8. Antwi WK. Evidence-based practice in radiography: attitudes, beliefs, knowledge and practices of radiographers in Ghana. OMICS J Radiol. 2015;04(01). doi:10.4172/2167-7964.1000176
9. Veness M, Rikard-Bell G, Ward J. Views of Australian and New Zealand radiation oncologists and registrars about evidence-based medicine and their access to Internet based sources of evidence: EBM AND ANZ RADIATION ONCOLOGISTS. Australas Radiol. 2003;47(4):409–415. doi:10.1046/j.1440-1673.2003.01211.x
10. Al Omari M, Khader Y, Jadallah K, Dauod AS, Al-shdifat AAK, Khasawneh NM. Evidence-based medicine among hospital doctors in Jordan: awareness, attitude and practice: evidence-based practice among hospital doctors. J Eval Clin Pract. 2009;15(6):1137–1141. doi:10.1111/j.1365-2753.2009.01260.x
11. Al-Ansary LA. The place of evidence-based medicine among primary health care physicians in Riyadh region, Saudi Arabia. Fam Pract. 2002;19(5):537–542. doi:10.1093/fampra/19.5.537
12. McColl A, Smith H, White P, Field J. General practitioners’ perceptions of the route to evidence based medicine: a questionnaire survey. BMJ. 1998;316(7128):361–365. doi:10.1136/bmj.316.7128.361
13. Shuval K, Shachak A, Linn S, Brezis M, Reis S. Evaluating primary care doctors’ evidence-based medicine skills in a busy clinical setting: primary care doctors EBM skills. J Eval Clin Pract. 2007;13(4):576–580. doi:10.1111/j.1365-2753.2007.00805.x
14. Valdes K, von der Heyde R. Attitudes and opinions of evidence-based practice among hand therapists: a survey study. J Hand Ther. 2012;25(3):288–296. doi:10.1016/j.jht.2012.02.001
15. Döpp CME, Steultjens EMJ, Radel J. A Survey of evidence-based practise among Dutch occupational therapists: EBP among Dutch OTs. Occup Ther Int. 2012;19(1):17–27. doi:10.1002/oti.324
16. Dodd JD, MacEneaney PM, Malone DE. Evidence-based radiology: how to quickly assess the validity and strength of publications in the diagnostic radiology literature. Eur Radiol. 2004;14(5):915–922. doi:10.1007/s00330-003-2145-8
17. Kelly AM. Evidence-based radiology: step 1—ask. Semin Roentgenol. 2009;44(3):140–146. doi:10.1053/j.ro.2009.03.011
18. Kelly AM. Evidence-based radiology: step 2—searching the literature (search). Semin Roentgenol. 2009;44(3):147–152. doi:10.1053/j.ro.2009.03.012
19. Cronin P. Evidence-based radiology: step 3—critical appraisal of diagnostic literature. Semin Roentgenol. 2009;44(3):158–165. doi:10.1053/j.ro.2009.03.016
20. Cronin P. Evidence-based radiology: step 4—apply. Semin Roentgenol. 2009;44(3):180–181. doi:10.1053/j.ro.2009.03.004
21. Cronin P. Evidence-based radiology: step 5—evaluate. Semin Roentgenol. 2009;44(3):182–183. doi:10.1053/j.ro.2009.03.005
22. Mayer J. The attitudes of Australian GPs to evidence-based medicine: a focus group study. Fam Pract. 1999;16(6):627–632. doi:10.1093/fampra/16.6.627
23. Barghouti F, Halaseh L, Said T, Mousa AH, Dabdoub A. Evidence-based medicine among Jordanian family physicians: awareness, attitude, and knowledge. Can Fam Physician. 2009;55(7):e6–e13.
24. Freeman AC, Sweeney K. Why general practitioners do not implement evidence: qualitative study. BMJ. 2001;323(7321):1100. doi:10.1136/bmj.323.7321.1100
25. Varnell G, Haas B, Duke G, Hudson K. Effect of an educational intervention on attitudes toward and implementation of evidence-based practice. Worldviews Evid Based Nurs. 2008;5(4):172–181. doi:10.1111/j.1741-6787.2008.00124.x
26. Niederhauser BD, Liaw K, McDonald R, Thomas KB, Hudson KT, Kallmes DF. Pick up a book or “Google It?” A survey of radiologist and trainee-preferred references and resources. J Digit Imaging. 2014;27(1):26–32. doi:10.1007/s10278-013-9638-z
27. Medina LS, Blackmore CC. Evidence-based radiology: review and dissemination. Radiology. 2007;244(2):331–336. doi:10.1148/radiol.2442051766
28. Craig JC, Irwig LM, Stockler MR. Evidence-based medicine: useful tools for decision making. Med J Aust. 2001;174(5):248–253. doi:10.5694/j.1326-5377.2001.tb143250.x
29. Amin FA, Fedorowicz Z, Montgomery AJ. A study of knowledge and attitudes towards the use of evidence-based medicine among primary health care physicians in Bahrain. Saudi Med J. 2006;27(9):1394–1396.
30. Chan GC, Teng CL. Primary care doctors’ perceptions towards evidence-based medicine in Melaka State: a questionnaire study. Med J Malaysia. 2005;60(2):130–133.
31. Scott I, Heyworth R, Fairweather P. The use of evidence-based medicine in the practice of consultant physicians. Results of a questionnaire survey. Aust N Z J Med. 2000;30(3):319–326. doi:10.1111/j.1445-5994.2000.tb00832.x
32. Madhavji A, Araujo EA, Kim KB, Buschang PH. Attitudes, awareness, and barriers toward evidence-based practice in orthodontics. Am J Orthod Dentofacial Orthop. 2011;140(3):309–316.e2. doi:10.1016/j.ajodo.2010.05.023
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
