Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Joint statement for the diagnosis, management, and prevention of chronic obstructive pulmonary disease for Gulf Cooperation Council countries and Middle East–North Africa region, 2017
Authors Mahboub BH , Vats MG , Al Zaabi A, Iqbal MN , Safwat T, Al-Hurish F, Miravitlles M , Singh D, Asad K, Zeineldine S, Al-Hajjaj MS
Received 6 March 2017
Accepted for publication 16 May 2017
Published 9 October 2017 Volume 2017:12 Pages 2869—2890
DOI https://doi.org/10.2147/COPD.S136245
Checked for plagiarism Yes
Editor who approved publication: Dr Richard Russell
Bassam H Mahboub,1,2 Mayank Gian Vats,2 Ashraf Al Zaabi,3 Mohammed Nizam Iqbal,2 Tarek Safwat,4 Fatma Al-Hurish,5 Marc Miravitlles,6 Dave Singh,7 Khaled Asad,8 Salah Zeineldine,9,10 Mohamed S Al Hajjaj1
1College of Medicine, University of Sharjah, Sharjah, 2Department of Pulmonary Medicine, Rashid Hospital, Dubai Health Authority, Dubai, 3Department of Pulmonary Medicine, Zayed Military Hospital, Abu Dhabi, United Arab Emirates; 4Chest Department, Ain Shams University, Cairo, Egypt; 5Department of Pulmonology and Allergy, Al-Sabah Hospital, Kuwait City, Kuwait; 6Department of Pneumology, Hospital Universitari Vall d’Hebron, Barcelona, Spain; 7Centre for Respiratory Medicine and Allergy, University of Manchester, University Hospital of South Manchester, Manchester, UK; 8Pulmonary and Critical Care, Istishari Hospital, Amman, Jordan; 9Faculty of Medicine, 10Hariri School of Nursing, American University of Beirut, Beirut, Lebanon
Abstract: Smoking and subsequent development of COPD is an ever-increasing epidemic in Arabian Gulf and Middle East countries, with no signs of decline. The important fact to be highlighted is that this COPD epidemic of increasing incidence and prevalence is mostly unrecognized by patients, due to the common attribution of symptoms to “smoker’s cough”, and the underdiagnosis and undertreatment by physicians because the common signs and symptoms masquerade as asthma. Consequently, there are long-term adverse effects of missing the diagnosis. The purpose of this review article is to focus upon the status of COPD in Arabian Gulf and Middle East countries, stressing the increasing burden of smoking and COPD, to emphasize the specific factors leading to rise in prevalence of COPD, to bring to light the underdiagnosis and undermanagement of COPD, and to treat COPD in conformity with standard guidelines with local and regional modifications. This review ends with suggestions and recommendations to the health department to formulate policies and to generate awareness among the general public about the side effects of smoking and consequences of COPD.
Keywords: COPD, Gulf Cooperation Council countries, Middle East, prevalence of smoking, water pipe, shisha, medwakh, bakhour
Corrigendum for this paper has been published
Introduction
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines define COPD as
[…] a common preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities caused by significant exposure to noxious particles or gases.1
COPD is responsible for substantial morbidity and mortality globally. The Global Burden of Disease project in 2001 identified COPD as the sixth-leading cause of death in the developing or underdeveloped world, culminating in 4.9% of total deaths.2 As per World Health Organization (WHO) estimates in 2004,3 more than 60 million people are suffering from COPD and approximately 3 million people died directly or indirectly due to COPD. By 2030, COPD will become the third-leading cause of death worldwide according to a WHO prediction. A recent US study identified COPD as the fourth-leading cause of chronic morbidity and mortality, and incidence and prevalence continuously on the rise.4 Despite the fact that around 90% of COPD-related deaths occur in developing or underdeveloped countries, very few data are available in these countries about the burden of COPD.
Although there is no permanent cure for COPD, reduction of risk factors can reduce the progression of the disease, with consequent health-related benefits. The most important risk factors for the development of COPD are smoking (cigarettes, water pipe), air pollution resulting from biomass fuel or coal and wood burning, previous tuberculosis, environmental/occupational exposures, and increasing age.5 The worldwide increase in COPD prevalence is directly related to the increase in prevalence of smoking, especially in women and young adults.
Current status of COPD in Gulf Cooperative Council countries and Middle East–North Africa region
The prevalence of smoking and COPD has risen significantly in Gulf Cooperative Council (GCC) countries and the Middle East–North Africa (MENA) region, due to the lack of knowledge of the risks of smoking and COPD. It is worth noting that in the GCC–MENA region, COPD is largely underdiagnosed/wrongly diagnosed and hence inappropriately treated. Diagnosis of COPD is delayed until it is moderately or severely advanced, due to lack of standardized procedures to diagnose COPD, overreliance on clinicoradiological parameters by clinicians for diagnosis, low general public awareness, indifferent attitudes in physicians and the general public about smoking and COPD, high prevalence of smoking (active and passive) and environmental pollution, nonimplementation of health regulations for smoking cessation, and the dictum that “everything that wheezes is asthma” leading to misdiagnosis of COPD as asthma.
Smoking prevalence and smoking habits
A pandemic of smoking and COPD is sweeping across the Middle East and MENA region. The recently conducted BREATHE study revealed that the adjusted smoking rate in the general population of MENA countries was estimated to be 31.2% (ranging from 15.3% in Morocco to 53.9% in Lebanon). The smoking rate in men ranged from 29.7% in Morocco to 61% in Turkey, whereas in women it ranged from 1.4% in Morocco to 47.3% in Lebanon. Overall, the highest rates were detected in Jordan, Lebanon, Syria, and Turkey.6
Many people in the GCC–MENA region consider smoking cigarettes and water pipes a socializing activity. In this region, tobacco is consumed in different forms, eg, water pipe (narghile/hookah) and medwakh (a pipe used to smoke dokha, a tobacco mixed with herbs and spices “dokha” in Arabic means “dizziness”), and the lack of health regulations to prohibit smoking and shisha in clubs, coffeehouses, and other public places is a major contributor to first and secondhand smoke.7 Water-pipe smoking is highly prevalent in women and the young, due to less cultural stigma associated with water-pipe smoking. It is important to note that the nicotine exposure from daily water-pipe use is considered equivalent to 20 cigarettes/day,8 and it has been found that water-pipe and medwakh smokers have dependence on nicotine and are unable to quit, despite repeated attempts. There is a clear misconception that the water pipe is harmless compared to cigarettes, because the smoke is filtered and the noxious smoking particles absorbed and dissolved in water.9 We discuss regional smoking patterns and burden in later sections.
Other risk factors for COPD relevant to GCC–MENA
The development of COPD and its progression is multifactorial, including complex interplay of genetic/risk factors and environmental exposure. Considering the huge proportion of expatriates in the UAE population, this statement holds further true; however, most of the genetic factors that could be potential contributors to the development of COPD in the GCC–MENA region are unknown, due to a lack of phenotypic and genetic research studies on COPD.
Environmental factors
Outdoor air pollution, occupational exposure to dust and fumes, biomass-smoke inhalation, first- and secondhand smoke, and previous tuberculosis are important environmental factors associated with COPD in the GCC–MENA region. Although tobacco smoking is the most common and important cause for COPD development, the population-attributable fraction of smoking as an etiological cause of COPD ranges from 9.7% to 97.9%. A Swedish cohort observed that the population-attributable fraction of smoking as a cause of COPD was present in 76.2%,10 suggesting that there are other factors contributing to COPD development.
Outdoor air pollution
Outdoor pollution coming mainly from emission of gases/fumes and pollutants from vehicular and industrial emission is an important public health problem in the fast-developed GCC–MENA region. In a community-based study, higher traffic density was found to be significantly associated with lower forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) values in women.11 In a recent survey, Dubai Municipality found that the city ranked very high in vehicular pollution in the developed world, using an on-road vehicle emission-measurement device (measuring percentage scores for levels of harmful pollutants, including hydrocarbons, CO, nitrogen oxides, and CO2). Dubai’s statistical data showed that the number of motor vehicles had increased by an annual average of about 12% in Dubai every year, significantly contributing to air pollution. Frequent dust storms may also lead to acute exacerbation of COPD.
Rapid industrialization and urbanization
Very rapid construction of multistory buildings in the last 2 decades with the significant risk of exposure to harmful construction dust to laborers and nearby residents could have significantly contributed to the development of COPD, especially in the young.
Indoor air pollution
Indoor air pollutants contributing to COPD development are tobacco smoke, by-products of combustion of coal/wood/barbeque, such as nitrogen dioxide, carbon monoxide, volatile organic compounds, and biological allergens.12 Among these, tobacco and biomass-smoke (wood, crop residue, barbeque)13,14 exposure contributes to the development of COPD. A recent meta-analysis showed biomass-smoke exposure to be a significant risk factor for developing COPD.15 However, in view of the rapid urbanization and no or minimal use of biomass fuel, indoor air pollution would not be a significant contributing factor for the young, but could definitely be a contributory factor to COPD in the elderly when biomass fuel was the main source of cooking.
In the GCC–MENA region, traditional Arabian incense (bakhour) is a common source of indoor smoke, and has consistently been found to be associated with worsening of asthma and wheezing bronchitis, especially in children, in many studies. Unfortunately, there are no studies available to establish bakhour as a contributory or worsening cause of COPD; however, scientifically speaking, slow and incomplete combustion of bakhour produces continuous smoke-containing pollutants (toxic gases and chemical particles), including polycyclic aromatic hydrocarbons, CO, benzene, and isoprene, that accumulate easily in indoor environments if ventilation is inadequate or in crowded places,16 and could be a potential indoor risk factor for COPD in the MENA region.
One study with the objective of characterization of particles and gases emitted from Arabian incense revealed that carbon monoxide and oxides of nitrogen concentration in time-weighted averages exceeded current government-regulation values and emissions from environmental tobacco smoke. Charcoal emissions were the main contributor to high CO and NOx concentrations. A significant cell-inflammatory response was observed to smoke components formed from incense burning. Our hazard evaluation suggests that incense burning contributes to indoor air pollution, and could be harmful to human health by worsening asthma and COPD.17
Rationale for GCC–MENA joint statement
To produce this joint statement on COPD in the GCC–MENA region, we searched PubMed, Google Scholar, ResearchGate, Medline, SciSearch, Journal Citation Reports, Science Edition, Embase, Scopus, Directory of Open Access Journals, OAIster, and other research portals extensively for articles published on the burden of COPD in the MENA region, and found that there is scarce material available from the GCC–MENA region. BREATHE was the largest regional study done, with eleven countries participating, focusing on the epidemiology/pathogenesis/standardization of diagnosis/treatment and preventive strategies and covering all other important aspects of this chronic, debilitating, multisystem, inflammatory disease and considering the widely varied sociocultural, demographic, and ethnic background/factors in this part of the world, with its majority of immigrant populations from low/middle socioeconomic class and their different attitudes/beliefs, patterns of smoking, and compliance with treatment.18
We decided to uncover various issues, with particular emphasis on local and regional factors covering all aspects of COPD in this GCC–MENA positional statement, and we recommend that all regional health authorities implement strict policies for the prevention/diagnosis and treatment of this debilitating disease in the GCC–MENA region as per standard evidence-based management strategies with regional modification to reduce the incidence of smoking and consequent COPD and to provide best standardized care to all COPD patients.
Incidence and prevalence of COPD in GCC–MENA region
More than 3 million people died of COPD in 2012, which is equal to 6% of all deaths globally that year. As per WHO estimates, 65 million people have moderately severe COPD. Estimates show that COPD in 2030 will be the third-leading cause of death worldwide.19 More than 90% of COPD-related deaths occur in low- and middle-income countries. The primary cause of COPD is tobacco smoking (through tobacco use or secondhand smoke). COPD now affects men and women almost equally, due to increased use of tobacco and related products among women in high-income countries. COPD is not curable, but treatment can slow the progression of the disease.
A systemic meta-analysis of spirometry-based studies (n=123 studies) across the world showed growing prevalence of COPD globally, and produced the following results:
- Global prevalence increased from 10.7% (227 million population) in 1990 to 11.7% (384 million population) in 2010 (68.9% increase).
- Overall prevalence in men was 14.3% compared to 7.6% in women.
- The Eastern Mediterranean Region (EMR) showed the highest increase in percentage, from 11.8% in 1990 to 13.4% in 2010 (118.7% increase in the prevalence of smoking).20
Burden of COPD in MENA region
There is a scarcity of studies in Africa, Southeast Asia, and the EMR.20 For the purpose of this review, PubMed was searched for articles published on the burden of COPD in the MENA region/EMR. Twelve studies were short-listed to assess the burden of COPD in the MENA region. BREATHE was the largest regional study done, with eleven countries participating.21 It estimated the prevalence of COPD to be 3.6% in the MENA region, ranging from 1.9% in the UAE to 6.1% in Syria.21 Al Zaabi et al estimated spirometry-based postbronchodilator prevalence to be 3.7% in the UAE.22 Another study in Dubai estimated COPD prevalence to be much higher – at 12.9%.23 This difference in COPD prevalence can be explained, as the latter study resorted to prebronchodilator definition, which does not differentiate a substantial group of asthma patients from COPD, and hence overestimated the prevalence. Recent studies in Saudi Arabia have revealed COPD prevalence of 2.4%–14.2%.21,24,25 The study with high estimated prevalence was conducted in high-risk patients (smokers presenting to primary health clinics) instead of the general population, hence overestimating the results.24 This difference was also noted in Jordan, with COPD prevalence being 5.4% (BREATHE study in general population) vs 8.2% in a study done in male smokers by Al Omari et al.21,26
One recent Egyptian study conducted on a high-risk population categorized study subjects based on risk factors for COPD (smokers, occupational exposure, and biomass fuel-combustion exposure), and estimated threefold-higher prevalence of COPD (9.6% vs 3.5% in BREATHE).21,27 Another spirometry-based study in Egypt estimated the prevalence of COPD to be 6.6%.21,28 Similarly, COPD prevalence in Lebanon was 5.3% in a questionnaire-based BREATHE study, while it was 9.7% in another study using postbronchodilator definition of COPD.21,29 It is obvious that spirometry-based studies produce higher prevalence than questionnaire-based studies.
Burden of Lung Disease (BOLD) studies were conducted in the countries in the GCC–MENA region. Based on BOLD protocol-estimated prevalence of COPD in Tunisia, Saudi Arabia, and Morocco of 7.8%, 4.2%, and 12.6%, respectively, BREATHE COPD-prevalence estimates were 3.7%, 2.4%, and 2.2%, respectively.25,30,31 Underreporting of mild symptoms, smoking prevalence (especially in females), criteria for diagnosis of COPD in BREATHE, and differences in methodology could partially account for this difference.
Estimated sex- and age-based prevalence of COPD also showed varied results. All studies reviewed demonstrated either statistically significant increased prevalence in males over females21,25,29 or no difference.22,23,28 This inconsistency can be explained by the wide variation in smoking prevalence in females within the region, differences in cultural background, and differences in exposure to other risk factors, eg, biomass fuel. Older age in some studies showed higher prevalence of COPD.22,28,31 GOLD stage II (moderate) COPD was found to have the highest prevalence in a majority of the studies that staged the population.22,31
Discussion
What is common?
There is substantial variation in COPD trends, both globally and regionally. Smoking is the single commonest and most important risk factor for COPD. A comparison was made of the various studies done worldwide with those of the MENA region to assess the relationship between prevalence of smoking and prevalence of COPD. There were differences in the study groups, methodology, and definitions used, as already mentioned.
In 2015, over 1.1 billion people smoked tobacco. Although it is declining worldwide and in many countries, the prevalence of tobacco smoking appears to be increasing in the WHO EMR and the African region.32 The BOLD study (from 14 countries worldwide) estimated smoking prevalence of 57.1% and COPD (stage 2 or higher) of 8.1%.33 Similarly, PLATINO (from five Latin countries) estimated average smoking prevalence was 56.8%, with average COPD prevalence of 9.04%.34
The Continuing to Confront COPD survey (updated version) from 13 countries estimated prevalence of smoking and COPD at 65% and 8.2%, respectively.35 BREATHE (inspired by this survey) estimated smoking prevalence of 31.2% and COPD of 3.6% in the MENA region.21 For the sake of comparison, smoking prevalence is almost double in the West compared to the MENA region, with COPD prevalence following the same trend. Needless to say, this is only a rough estimate to support the previously well-established fact that smoking is the commonest risk factor for COPD, with prevalence increasing proportionally.
What is different?
Comparison of studies
There is concern that the incidence and prevalence of COPD have been underestimated in the region, owing to overreliance on clinical diagnosis, with most of the time diagnoses not being based on spirometry or international guidelines.36
Spirometry vs questionnaire-based
BOLD and PLATINO were both spirometry-based studies. Spirometry-based studies from the MENA region reviewed totaled eleven. The first study ever in the region was that of Al Zaabi et al in 2011, and results were comparable to the largest questionnaire-based BREATHE study in the MENA region.21,22 Three studies were based on the BOLD protocol: Al Ghobain et al in Saudi Arabia,25 Daldoul et al in Tunisia,30 and El Rhazi et al in Morocco.31 The other studies have already been described herein.
Differences in study groups
Within the MENA region, significant variation in study groups can explain differences in COPD prevalence determined from the studies. For example, three studies were done in Saudi Arabia using different methodology, including smoking population, BREATHE study questionnaire, and BOLD protocol, which found COPD prevalence to be 14.2%, 2.4%, and 4.2%, respectively.
Comparison of risk factors
Cigarette smoking is the most important risk factor in the development and progression of COPD. However, a substantial number of COPD cases occur in the absence of smoking, especially among young adults and women and in developing countries. The population-attributable fraction of smoking as a cause of COPD was found to be less than 80% in a review by an ad hoc subcommittee of the American Thoracic Society, which revealed that a substantial burden of disease was attributable to nonsmoking and environmental risk factors.37
Specific genetic syndromes are causally related to the development of COPD. Traffic and other outdoor pollution, secondhand smoke, biomass smoke, and occupational exposure are associated with COPD. Chronic uncontrolled asthma and sequelae of untreated chronic tuberculosis are associated with irreversible changes in lung parenchyma and airway remodeling with loss of lung function, but there is still uncertainty about whether there are important phenotypic differences compared with COPD, as is typically seen in clinical settings.37
Tobacco smoking
As per WHO estimates in 2000, the rate of mortality from smoking in the adult population (age >30 years) was 19% in industrialized countries and 9% in developing countries.38 Khattab et al estimated adjusted smoking prevalence to be 31.2% in the MENA region.39 Highest rates were observed in Jordan, Lebanon, Syria, and Turkey. Significant variation was observed in the MENA region for estimated smoking prevalence between countries, ranging from 15.3% in Morocco to 53.9% in Lebanon.
Sex prevalence for smoking ranged from 29.7% in Morocco to 61% in Turkey in men and 1.4% in Morocco to 47.3% in Lebanon in women. Sex differences could be attributed to women having limited access to public places, religious and cultural beliefs, and social stigma. However, an increasing trend of smoking in women may be seen, due to increased marketing of cigarettes, social status, more professionally active women, and Westernization in the region.39
Smoking in the MENA region (particularly water-pipe smoking) is part of the culture. Lack of rules and regulations to ban smoking in public places contributes to the high prevalence of smoking in the region.40 Water-pipe smoking deserves special mention in this region, as it may increase the risk of COPD, lung carcinoma, and other chronic respiratory problems.41–43 Alzaabi et al screened 62,086 subjects in BREATHE, and found that water-pipe use was reported by 2,173 (3.5%, 95% CI 3.4%–3.6%), of whom 934 (43%) smoked both water pipes and cigarettes. The majority of water-pipe users were men (82%) and aged 40–49 years (53.7%). Over 90% of users smoked their water pipe for ≥1 hour per day.42
The prevalence of water-pipe use is high in the EMR. A national survey in Kuwait showed that 57% of men and 69% of women had used a water pipe at least once. Water-pipe use is also common in Egypt, where 22% of 6,762 men from two rural villages reported current or past use.27 Recent data from the EMR show that substantial numbers of adolescents and young adults are now smoking water pipes. In Syria, for example, about half of university students report having used a water pipe, and about a quarter of males currently use it. The picture is similar in Lebanon, where of 1,964 Beirut university students, 30.6% of men and 23.4% of women reported current, weekly water-pipe use in 2001. Across several EMR countries, about 10%–18% of those aged 13–15 years use tobacco products other than cigarettes, most likely water pipes.41
A systematic review of water-pipe use on health outcomes published in 2016 showed chronic bronchitis and COPD were significantly associated (P<0.05) with water-pipe use.21,43–46 Water-pipe use was significantly (P<0.05) associated with COPD in one study,28 and was a significant (P<0.05) risk for developing COPD in another study.43 A large study in UAE nationals found smoking prevalence to be commonest in younger groups, with an increasing trend in medwakh use among the young.47 Passive smoking was also found to be an important risk factor for COPD in developed and developing countries.37,48
Factors other than smoking
The prevalence of COPD among nonsmokers is estimated to be 3%–15%, further validating the role of other risk factors.33,34,37 A cross-sectional study in Lebanon revealed 3.4% of nonsmokers had COPD (GOLD stage I) and 11.75% chronic bronchitis. Lower prevalence in nonsmokers in the MENA region compared to other areas of the world could be attributed to a younger demographic in developing countries.49 The Tunisian BOLD study estimated a prevalence of 4.7% (GOLD stage I) among nonsmokers (45% of COPD in the study were nonsmokers).50
Outdoor pollution and urbanization
There is strong evidence of an association between outdoor pollution and decreased pulmonary function growth during childhood and adolescence, though there are few studies that have defined COPD by spirometry.51–53 SAPALDIA-cohort analysis examined the association between 11-year change in air quality and lung-function decline among 8,047 adult subjects (4,742 had complete follow-up), with significant decline with higher PM10, a measure of particulate matter in the air.54
The AHSMOG study examined survey-based definitions of chronic bronchitis or emphysema only.55,56 The German SALIA study in women showed higher PM10 was related to an increased risk of COPD (GOLD stage I criteria).57 There is also evidence of biological plausibility, in that exposure to air pollutants, such as particulate matter, O3, and NO2, can produce deleterious effects on the airway, irreversible loss of pulmonary function over time, and COPD.58 A case-control study in Lebanon found a statistically significant association between outdoor pollution and chronic bronchitis. It concluded that living close to a busy road/power plant was linked to chronic bronchitis. Dubai was found to ranked highest in the developed world using a pollutant score on account of two variables: volume of cars and emission from each vehicle.40 Rapid urbanization and motorization are responsible for this situation. COPD prevalence was found to be higher in urban dwellers (60% of all cases) in 2010 in a meta-analysis of WHO world regions.20
Biomass fuel
In developing countries, a significant proportion of COPD cases occur among never- or nonsmokers, especially in women cooking with open-fire stoves. The fuel used in these stoves is collectively known as biomass (wood, animal dung, and crop residue). These stoves emit high levels of toxic air pollutants similar to those present in tobacco smoke, with exposure mostly occurring over the entire life span.59 Approximately half the world’s population still uses solid fuels for cooking, and this biomass-fuel usage is even higher in rural areas (up to 80%). Particulate-matter concentrations greatly exceed most governmental standards for outdoor air.37
Several case-control and cross-sectional studies, mostly from developing countries, have found a consistent direct correlation between cooking with biomass fuel and respiratory symptoms, chronic bronchitis, and chronic airflow obstruction, with evidence of an exposure–response relationship, eg, hours of cooking per day and number of years cooking with biomass.60–78 A study from Colombia found that biomass-stove use for ≥10 years was associated with a greater risk of COPD (GOLD stage I).79 Exposure to woodsmoke (barbeques, cooking stoves) was shown to increase the risk of chronic bronchitis in smokers (current or past) in a study in the US.18 In the MENA region, a study in the UAE showed that among COPD patients, biomass exposure was higher (33%) than other risk factors, including cigarette smoking (12% current, 12% past).22 An Egyptian study showed a COPD (GOLD stage I) prevalence of 11.2% in women exposed to biomass fuel; 86.2% of the total females in the exposed group were nonsmokers.27
Other exposure (occupational, Arabian incense)
Consistent direct associations have been observed between exposure to workplace pollutants and COPD in multiple high-quality epidemiological studies.37 Prevalence of exposure to bakhour is high in the MENA region, particularly the Arabian Gulf. It has been found to be an exacerbating factor in asthma not proven to be associated with COPD.22
Genetic factors
α1-Antitrypsin deficiency (AATD) accounts for 1%–2% of COPD cases, especially in the young.40 There are very limited data available in the region to estimate the prevalence of AATD. One study in Saudi Arabia concluded higher-than-expected prevalence of the AATD allele in the Saudi population. Genetics has an important role to play in the prevalence of COPD, and more studies need to be conducted.80
Asthma and tuberculosis
Many studies have the identified presence of irreversible airway obstruction in asthmatics, including nonsmokers, with evidence that longer asthma duration may lead to more severe chronic airway obstruction, due to accelerated loss of pulmonary function.81–84 Because airway obstruction and remodeling can lead directly to COPD, it is likely that asthma, with or without additional risk factors, can later develop into COPD. It remains uncertain, however, whether asthma patients with irreversible airway obstruction are phenotypically and pathologically similar to “typical” COPD patients or if they represent a separate subset of patients. There is limited but suggestive evidence of an association between tuberculosis and chronic airflow obstruction. The evidence is inadequate to show a causal relationship between tuberculosis and COPD worldwide and in the MENA region.
Sex
Across all WHO regions, COPD is more prevalent in men (14.3%) than women (7.6%), suggesting a higher-risk profile among men, with similar results seen in the MENA region: men (5.2%) vs women (1.8%).20,21 Recently, with increased tobacco consumption among women and higher risk of exposure to indoor pollution (biomass fuel used for cooking and heating) in low- and middle-income countries, sex differences in the disease may be reduced.85 For example, in the revised Continuing to Confront COPD survey of North America and Europe done in 2013, women (7.1%) had a higher prevalence of COPD than men (6.2%) in the US only. The other countries showed similar patterns, with higher prevalence in men.35
Burden of COPD in terms of cost and health care-resource consumption
COPD causes burdens in terms of mortality, morbidity, high health care costs, disability, and impaired quality of life.12 The European Union (EU) reported that the direct cost from COPD was over €38.6 billion in 2005, representing about 3% of total health care expenditure.86,87 In 2010, the US government spent nearly $49.9 billion on COPD, including $29.5 billion spent on direct health care compared to $38 billion spent in 2005, with direct health care costs being $22 billion. Direct costs per patient in 2005 were $2,700–$5,900.88,89
The burden in low- and middle-income countries has been comparatively high, owing to relatively low COPD awareness, challenges with COPD diagnosis, and increased exposure to additional risk factors, like combustion of biomass fuel.90 With increasing smoking prevalence in the MENA region, especially in the young, and increased life expectancy, the burden of resource consumption of COPD is likely to increase. The results of the BREATHE study were as follows (monetary quantification was not possible, due to wide variation in the region in terms of structure of health care provision).
- Physician consultation was the most frequent cause of health care-resource use, followed by emergency visits and hospitalizations, with similar hierarchy seen in developed countries.91–96
- Health care consumption showed proportional increase with GOLD severity.
- Frequency of symptoms, exacerbations, and higher COPD-assessment test (CAT) scores resulted in higher burden in terms of resource consumption. Group D in CAT had the highest expenditure, with a sixfold increase in hospitalization and emergency visits. Exacerbation of COPD was the major reason for physician consultation, hospitalization, and emergency visits. This puts emphasis on having individualized approaches in high-risk patients to optimize management of COPD and prevent exacerbations.
- The presence of comorbidities (mainly cardiovascular and diabetes) showed increased hospitalizations (P<0.0001) and hence increased consumption of resources, consistent with other studies.97,98
- Variation was observed within the MENA region, which could be explained by differences in health care systems, eg, availability of health care facilities to the general population and reimbursement processes.99
Diagnosis and assessment of COPD
The diagnosis of COPD should be considered in any patient who is complaining of dyspnea, cough, and sputum production, and who has a history of exposure to risk factors.100,101 To confirm the diagnosis, spirometry should be performed to detect the presence of airflow limitation.102
Clinical presentation
Characteristic symptoms of COPD
Dyspnea
This is simply described as air hunger or increased effort to breathe. It is usually chronic, progressive, and increases with exertion.103 Dyspnea is the most characteristic symptom of COPD, and it represents a major cause of disability and anxiety associated with COPD.
Cough
Chronic cough is the first COPD symptom to develop, initially intermittent, then it becomes every day. It may be productive or unproductive.104
Sputum production
Commonly, small amounts of tenacious sputum are associated with coughing. The term “chronic bronchitis” refers to regular sputum production for ≥3 months in 2 consecutive years with an absence of other conditions that could explain it.105
Wheezing and chest tightness
Wheezes and chest tightness are aspecific symptoms that can be variably present in COPD patients.
Other symptoms
Severe COPD may present with symptoms of cor pulmonale (ankle swelling), fatigue, weight loss, anorexia, anxiety, and depression.106 These symptoms have an important prognostic value,107 and can also be an indicator for other diseases (eg, tuberculosis, lung cancer), and thus should always be investigated.
Medical history
A detailed medical history is required in order to assess:
- exposure to risk factors (smoking, occupational or environmental exposures);
- asthma, allergy, sinusitis, or nasal polyps; respiratory infections in childhood; other respiratory diseases;
- family history of smoking, COPD, or other chronic respiratory disease;
- pattern of symptom development (COPD typically develops in adult life, and most patients develop progressive dyspnea over years, with chronic cough and sputum production);
- history of exacerbations or previous hospitalizations for respiratory disorder;
- presence of comorbidities, such as heart disease, osteoporosis, musculoskeletal disorders, and malignancies that may also contribute to limitation of activity;108
- impact of the disease on the patient’s life, including social and economic impact.
Physical examination
Physical signs as expiratory and inspiratory wheezes, coarse crepitations, and signs of hyperinflation may be present if lung function is significantly impaired. The absence of physical signs does not exclude the diagnosis.109,110
Spirometry
Spirometry is considered the most objective and reproducible test to detect airflow limitation. The test measures the volume of air forcibly exhaled from the point of maximal inspiration (FVC), the volume of air exhaled during the first second of this maneuver (FEV1), and the ratio of these two measurements (FEV1:FVC). Measurements are compared to reference values based on age, sex, height, and race.111 Spirometry of a normal subject is shown in Figure 1A, and that of a COPD patient showing an obstructive pattern in Figure 1B. An obstructive pattern is defined by FEV1:FVC ratio below the fifth percentile of a predicted value, and the shape of the flow–volume curve is concave.
  | Figure 1 Spirometry showing normal (A) and obstructive (B) patterns. |
Assessment of COPD
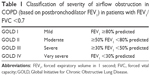
COPD is a complex disease, and hence the objectives of COPD assessment are to determine the severity of disease, risk of exacerbations, and hospital admissions, and its impact on the patient’s health status, quality of life, and risk of death. Knowledge of the previous combined parameters will guide optimum individualized therapy. The following aspects must be considered in COPD assessment: patient symptoms, spirometric abnormality, exacerbation risk, and presence/absence of comorbidities (Table 1).
Assessment of symptoms
A simple measure of breathlessness using the modified Medical Research Council (mMRC) dyspnea scale was previously considered adequate for assessment of symptoms.112,113 However, since COPD has multiple symptomatic effects,114 it is recommended to use more sophisticated tests with comprehensive symptom assessment. Questionnaires like the CAT (http://www.catestonline.org) and clinical COPD questionnaire (CCQ; http://www.ccq.nl) are practical and suitable for this purpose. However, because use of the mMRC is still widespread, an mMRC score ≥2 is still included as a cutoff point for separating “less breathlessness” from “more breathlessness”.115,116
CAT
This is an eight-item unidimensional measure of health-status impairment in COPD.117 It was developed to be applied worldwide, and validated translations are available in many languages. The score ranges from 0 to 40, and CAT scores correlate very closely with the St George’s Respiratory Questionnaire.118
CCQ
This is a ten-item self-administered subjective questionnaire developed to measure clinical control in patients with COPD.119,120 Although the concept of “control” in COPD remains controversial, the CCQ is short and easy to administer. It is reliable, available in many languages, and has been well validated.
Assessment of airflow limitation
Spirometry should be performed using techniques that meet recommended published standards after the administration of an adequate dose of a short-acting inhaled bronchodilator.121 Spirometric measurements should be evaluated by comparison of the results with appropriate reference values based on standard demographic nomograms. The presence of postbronchodilator FEV1/FVC <0.7 confirms airflow obstruction in the patient.
Assessment of exacerbation risk
An exacerbation of COPD is defined as an acute worsening of underlying respiratory symptoms that result in requirement of additional therapy.122 The best predictor of frequent exacerbations (two or more exacerbations per year or one or more leading to hospital admission) is the presence of frequent exacerbations in the past. Low frequency is defined as one (or zero) exacerbation per year or no hospital admission.123 The risk of exacerbations increases significantly in severe and very severe disease. COPD exacerbations are associated with deterioration in health status, increased decline in lung function, and increased risk of death.124
Assessment of comorbidities
Other diseases related to smoking and aging may coexist with COPD,125 and COPD itself may lead to multiple systemic effects, including but not limited to cardiovascular disease, skeletal muscle dysfunction, metabolic syndrome, osteoporosis, depression, and lung cancer.126,127 Comorbidities should be looked for routinely and treated appropriately in any patient with COPD.
Combined COPD assessment
The combined assessment of COPD helps to categorize patients into one of four groups (Figure 2), which helps guide therapy. To classify patients into a specific group, we perform the following steps.
  | Figure 2 Refined ABCD assessment tool (simpler version). |
Symptom assessment
If the patient has fewer symptoms (CAT <10) or less breathlessness (mMRC grade 0–1), then he/she belongs in the boxes on the left. If the patient has more symptoms (CAT ≥10) and/or more breathlessness (mMRC grade ≥2); then they belong in the boxes on the right.
Risk-of-exacerbation assessment
To detect if the patient has high or low risk, we choose the higher risk of the following three methods:
- Assess the number of exacerbations the patient has had within the previous 12 months (zero or one indicate low risk [lower part of box], while two or more exacerbations indicate high risk [upper part of box]).
- Determine whether the patient has had one or more hospitalization in the previous year for a COPD exacerbation, indicating high risk (upper part of box).
- The latest GOLD 2017 document refines the ABCD assessment tool by separating spirometry grades from the “ABCD” groups.
Further clinical phenotyping
The Spanish guidelines for COPD (GesEPOC) recognize the importance of characterizing patients by clinical phenotype, helping to customize treatment according to the characteristics of each patient, and identifying clinical phenotypes that may help to identify group of patients with different mortality and treatment responses.128–130 GesEPOC identify four phenotypes, and these are of value in deciding which anti-inflammatory treatments should be given to patients: nonexacerbators, mixed COPD (asthma phenotype), exacerbators with chronic bronchitis phenotype, and exacerbators with emphysema phenotype.
Asthma–COPD overlap syndrome (ACOS)
Those patients who are characterized by persistent airflow limitation with several features, usually associated with asthma and several features usually associated with COPD. Asthma–COPD overlap syndrome (ACOS) is therefore identified in clinical practice by the features that it shares with both asthma and COPD.131 Recently suggested criteria for the diagnosis of ACOS follow (Table 2).
Role of eosinophils
The prevalence of eosinophilic inflammation in COPD patients is unknown. We do not know whether patients with sputum or blood eosinophilia represent a stable COPD phenotype over time. Prospective clinical trials are required to determine a cutoff threshold for blood eosinophils that predicts future exacerbation risk in COPD patients with an exacerbation history and to clarify the blood-eosinophil cutoff value that can be used in clinical practice. The most commonly reported value in the literature is 2%; however, there have been many other cutoff values reported.132 The ACOS committee generally felt that a 2% threshold lacked sufficient specificity to diagnose eosinophilic airway inflammation. Until more evidence is available, the committee endorses a higher threshold of peripheral blood-eosinophil count of ≥300 cells/μL to increase the specificity of the biomarkers to diagnose eosinophilic airway inflammation as a minor criterion for ACOS.133,134 It has been found that many physicians in GCC–MENA follow the clinical phenotype approach of COPD treatment, and there is evidence that this approach has the potential to reduce the risk of exacerbation and assessment of different medium- and long-term mortality; however, large multicenter trials are needed to validate the evidence fully.
Additional investigations
Imaging
Radiological signs that may suggest COPD include signs of lung hyperinflation (flattened diaphragm and increase in retrosternal airspace volume), hyperlucency of the lungs, and rapid tapering of vascular markings (Table 3). However, radiological assessment in COPD patients, either chest X-ray or computed tomography (CT), may be helpful to exclude other diagnoses or to detect associated comorbidities (pulmonary fibrosis, pleural diseases, and cardiomegaly). Chest CT scans are recommended prior to lung-volume-reduction surgery in emphysema.135
  | Table 3 Differential diagnosis of COPD |
Lung volume and diffusion capacity
Body plethysmography may document increased residual volume and increased total lung capacity, which indicates air trapping and pulmonary hyperinflation. Measurement of lung CO-diffusion capacity provides information on the functional impact of emphysema in COPD.
Pulse oximetry and arterial blood-gas measurement
Pulse oximetry should be used to assess all stable patients with FEV1 <35% predicted, clinical signs suggestive of respiratory failure, or right-side heart failure. If peripheral saturation is <92%, arterial blood gases should be done and action taken accordingly.136
Screening for α1-antitrypsin deficiency
Younger patients (<45 years) with lower-lobe emphysema should be screened. A serum concentration of AAT below 15%–20% of the normal value is highly suggestive of homozygous AATD.
Exercise testing
Objectively measured exercise impairment assessed by a reduction in self-paced walking distance137 or during incremental exercise testing in a laboratory138 is a powerful indicator of health-status impairment and predictor of prognosis.139 Walking tests can be useful for assessing disability, and are used to assess the effectiveness of pulmonary rehabilitation.
Composite scores
Several variables may be combined in a composite score to try to identify disease severity. One of these scores is the BODE (body-mass index, obstruction, dyspnea, exercise) index, which has been found to be a better predictor of subsequent survival than any component alone.140
Pharmacological management of COPD
The GOLD 2017 management strategy recommends a combined assessment of COPD based on symptoms and exacerbations to categorize patients into clinical phenotypes (groups A–D). These groups have distinct pharmacological treatment recommendations covering initial management and a stepwise approach to follow-up treatment. We have used the principles of GOLD 2017 to make pharmacological treatment recommendations using a format that will hopefully be easy to follow for the practicing clinician.
GOLD recognizes that some of its pharmacological treatment algorithms are only partly based on evidence. Most of our recommendations are similar to GOLD, but we highlight recommendations that differ and key areas where more evidence is needed. The evidence for the various pharmacological treatments for COPD is firstly summarized, followed by recommendations for initial and follow-up treatment.
Clinical evidence for pharmacological treatment
Long-acting muscarinic antagonists (LAMAs) improve symptoms, lung function, and exercise performance and reduce exacerbation rates.141,142 Long-acting β2-agonists (LABAs) also address these parameters, but have less effect on exacerbations than LAMAs.143–145 Long-acting bronchodilators provide a convenient treatment option, with prolonged duration of action compared to short-acting bronchodilators.
Dual-bronchodilator combination inhalers containing both a LAMA and LABA have a greater effect on lung function and symptoms than long-acting bronchodilator monotherapies.146 LAMA–LABA combinations have a greater impact on exacerbations than long-acting bronchodilator monotherapies,147 although only one study has been performed in COPD patients with a history of exacerbations.148 Inhaled corticosteroid (ICS)–LABA combinations improve lung function and symptoms, and several clinical trials in COPD patients with exacerbation history have shown an effect on exacerbation prevention: recent studies have shown an approximately 25% exacerbation-rate reduction due to the ICS component.143,149,150 Long-term use of ICS is associated with side effects, including pneumonia,143,149,150 bone fractures,151 cataracts,152 diabetes,153 and mycobacterial infection.154 Pneumonia has been highlighted as a clinical concern, but the rate of these events is low and appears to be greater in certain subgroups, such as older patients and those with low body-mass index, low FEV1, and a history of pneumonia.155,156 Overall, the benefits of ICS–LABA combinations on exacerbation prevention outweigh the risks.
One clinical trial (the FLAME study) has compared ICS–LABA with LABA–LAMA in COPD patients with an exacerbation history. There was a greater impact of LABA–LAMA on exacerbations.157 More studies are needed to confirm this finding in wider patient populations, and with different drugs within these classes.
Triple therapy refers to the combination of ICS plus LABA plus LAMA, either in a single combination or as separate inhalers. Triple therapy improves lung function and symptoms and reduces exacerbations compared to LAMA monotherapy or ICS–LABA treatment.158,159 There are currently insufficient data on the comparison of triple therapy and LAMA–LABA treatment.
Roflumilast (AstraZeneca, Cambridge, UK) is a PDE4 inhibitor that has anti-inflammatory effects, reducing exacerbations in COPD patients with FEV1 <50%, a history of exacerbations, and chronic bronchitis.160 Long-term macrolide-antibiotic use reduces exacerbation rates, but it is unclear whether this is due to antibacterial or anti-inflammatory activity.161 There are risks of increased bacterial resistance with long-term macrolide use, and the clinical phenotype of patients most likely to respond has not been conclusively described. The evidence for the use of mucolytics to prevent exacerbations is inconsistent.
Initial pharmacological treatment
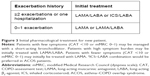
COPD patients at initial diagnosis should be categorized as either “frequent exacerbators”, suffering two or more exacerbations (requiring oral steroids and/or antibiotics) or one hospitalization in the last year, or those with low exacerbation frequency (“infrequent exacerbators”), experiencing one (or zero) exacerbation in the previous year. Symptoms should be assessed using mMRC score or CAT score. Initial pharmacological treatment is described in Figure 3, and key points are summarized in Table 4.
Infrequent exacerbators
COPD patients with low exacerbation frequency should initially receive long-acting bronchodilator treatment without the need for ICS. Patients should be started on a LAMA. Some patients with a very high degree of symptoms at initial presentation can be started with a LAMA–LABA combination inhaler, although the exact clinical characteristics favoring this approach have not been defined.
Frequent exacerbators
Frequent exacerbators should commence on either a LAMA–LABA or an ICS–LABA combination, both of which address symptoms and exacerbations. GOLD also proposes these options, but favors LAMA–LABA, due to the risk of pneumonia associated with ICS and the results of the FLAME trial. We do not follow this approach favoring LAMA–LABA, as the number of clinical trials showing that different ICS–LABA combinations reduce exacerbations far outweigh the number of exacerbation trials with LAMA–LABA combinations, and the results of FLAME require confirmation. Furthermore, many COPD patients have very low pneumonia risk.
GOLD advocates an individualized approach to COPD treatment, and identifies characteristics that favor ICS–LABA treatment response, such as the presence of asthma features or higher blood-eosinophil counts. We recommend an individual approach to decide the most appropriate treatment (ICS–LABA or LAMA–LABA), based on factors already described that predict ICS benefit or risk.
COPD patients with a low symptom burden (CAT score <10 or mMRC score 0–1) may be managed initially with a lower level of treatment than already described. For infrequent exacerbators, a short-acting BA and/or short-acting MA can be used initially, although often such patients need to step up to long-acting bronchodilator treatment. Frequent exacerbators with a low symptom burden may be managed initially with a LAMA.
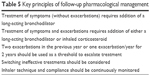
Pharmacological treatment at follow-up
At follow-up, escalation of treatment should be based on whether the patient requires further treatment for symptoms only, or symptoms and exacerbations; it is uncommon for patients to suffer exacerbations without the need to treat symptoms. Follow-up pharmacological treatment is described in Figure 4, and key points are summarized in Table 5.
  | Figure 4 Follow-up treatment of COPD patients. |
  | Table 5 Key principles of follow-up pharmacological management |
Treatment of symptoms only
The need to treat symptoms further should be based on an individual assessment of dyspnea, exercise capacity, and quality of life. Follow-up treatment of symptoms alone (without exacerbations) may require the addition of further long-acting bronchodilator treatment; there is no need to add an ICS. Patients treated with LAMA monotherapy can be escalated to a LAMA–LABA combination, while those treated with ICS–LABA can be escalated to triple therapy (ICS–LABA–LAMA). For patients with significant symptoms despite LAMA–LABA treatment, nonpharmacological approaches should be readdressed (eg, pulmonary rehabilitation, check for comorbidities), as well as checking inhaler technique and compliance.
Treatment of symptoms and exacerbations
Clinical trials have shown a benefit for various combination treatments (ie, triple therapy, ICS–LABA, and LABA–LAMA) in patients with a history of one or more exacerbations in the last year.8–10,17,19 The natural history of exacerbations is that a proportion of patients with one exacerbation in the previous year will experience none the following year.162 We recommend that escalation of treatment is appropriate for patients with one exacerbation/year for each of the previous 2 years or two or more exacerbations (or one hospitalization) in the previous year.
Patients suffering with symptoms and exacerbations at follow-up can receive either an additional bronchodilator or ICS treatment. Patients treated with a LAMA can be escalated to a LAMA–LABA combination or switched to an ICS–LABA combination. Patients receiving ICS–LABA or LAMA–LABA can be escalated to triple therapy or treatment can be switched from one of these combinations to the other. Switching treatment is recommended in situations where the previous pharmacological treatment provided no or little clinical benefit. For patients established on triple therapy and still suffering with exacerbations, individual clinical characteristics can be used to decide to add further treatment: chronic bronchitis (add roflumilast or mucolytics as an alternative), evidence of bacterial infection or bronchiectasis (add azithromycin [Zithromax®; Pfizer, New York, NY, USA]).
Stepping down treatment
There are some situations in clinical practice where a step down in treatment should be considered. These are where an ICS–LABA combination has been inappropriately prescribed to a patient suffering with symptoms who has never experienced an exacerbation, for whom ICS withdrawal should be considered, and where the treatment of a patient has been escalated, but there has been either no or little clinical benefit, in which case a step down or switching of treatment should be considered.
Differences between drugs of the same class
The recommendations provided assume that the drugs within each class have similar effects. For the main drug classes recommended (LAMA, ICS–LABA, and LAMA–LABA), clinical trial data show generally similar effects of drugs (within a class) in terms of clinical efficacy, although direct comparisons in the same study are often lacking. On a practical level, the major differences between drugs within a class are the inhaler device and the need for once- or twice-daily delivery. It is important to check that the patient can use the inhaler device selected, and that the dosing regime is appropriate for the patient. Twice-daily dosing may be more suitable for patients with nighttime/early-morning symptoms, although an advantage for twice-daily vs once-daily dosing in this regard has not been definitively proven.
Blood eosinophils
Post hoc analysis of clinical trials in COPD patients with an exacerbation history has demonstrated that higher blood-eosinophil counts predict an increased effect of ICS on exacerbation-rate reduction.163,164 This observation has now been confirmed in a prospective randomized controlled trial (Vestbo et al, unpublished data, 2017). The blood-eosinophil cutoff values that should be used in clinical practice to predict a beneficial effect of ICS have yet to be defined.
Nonpharmacological management of COPD
As discussed earlier and in view of COPD being a systemic disease, comprehensive management of COPD includes nonpharmacological management incorporating various modalities to support already-declined lung functions, improve quality of life, and prevent morbidity and mortality consequent to COPD.
Self-management education
Education is an important component of the nonpharmacological aspect of COPD. Topics covered in education programs include smoking cessation, detailed knowledge about COPD, general and specific approaches to therapy and other aspects of COPD, strategies to minimize symptoms, primarily dyspnea, and initial management of exacerbations.1 It is important to recognize that patient education alone does not change behavior or motivate patients, but if done appropriately can increase ability to cope with the stress of illness and improve health status. Self-help groups and group discussion may also help in encouraging COPD patients to follow a healthy lifestyle.
Pulmonary rehabilitation
GOLD 2017 guidelines stress that pulmonary rehabilitation should be a keystone in the management plan of COPD patients, underscoring its importance and effectiveness. Pulmonary rehabilitation is defined as a comprehensive intervention based on a thorough assessment of the COPD patient and delivering such interventions as exercise, behavior, and education to improve the quality of life of COPD patients.
The American Thoracic Society – European Respiratory Society joint statement states that all symptomatic patients, particularly those with systemic manifestations of COPD, benefit from rehabilitation, while the GOLD 2017 statement recommends it for patients with high symptoms burden and risk of exacerbation (groups B–D). These patients should be encouraged to participate in well-structured rehabilitation programs, taking into account individual patients’ characteristics and comorbidities.165,166 Patients planned for lung-volume-reduction surgery should also be included both preoperatively and postoperatively.167 Evidence-based best practice for rehabilitation programs includes structured and supervised exercise training, smoking cessation, nutrition therapy, and self-management skills.
Adherence and cooperation are needed for rehabilitation programs, and patients who have active heart disease or are limited due to joint or orthopedic illness may be unable to join a program. Should active smokers be participating in such programs, whether they are motivated to adhere continues to be a field of investigation. Clearly, degree of FEV1 is not a contraindication, as the American College of Chest Physicians recommends rehabilitation for those with FEV1 <50%.168 Pulmonary rehabilitation benefits include improving quality of life, body strength, and exercise tolerance. It also reduces exacerbation rate, and this in turn will affect the health care burden of COPD. However, the most interesting and debatable issue is rehabilitation’s impact on mortality, a question not resolved, yet with some indication that pulmonary rehabilitation may improve COPD mortality.169
Exercise training
A combination of constant-load or interval training with strength training of upper- and lower-extremity muscle groups and goals of endurance training to 60%–80% of symptom-limited maximum work or heart rate is preferred,170,171 or to Borg dyspnea or fatigue score of 4–6.172 Exercise training should be done after full optimization of LAMA–LABA therapy.
Smoking cessation
First and foremost in nonpharmacological management of COPD is that it includes smoking cessation. Data are currently clear that stopping smoking is important, as it decreases or halts decline in FEV1. In fact, the Lung Health Study revealed an improvement in lung function within a year or so of quitting smoking, and such data also push physicians to help patients to stop rather than reduce cigarette-smoke intake.173 A Finnish study has shown a survival benefit among those who stop smoking, regardless of COPD stage.174 Clearly, most attention has been focused on nicotine-replacement therapy, particularly combination-delivery systems (nicotine patch and nasal spray most preferred). There is also nicotine gum, lozenges, and inhalers. Research has shown nonpharmacologic approaches, such as behavioral counseling or hypnosis, especially when combined with nicotine patches, to be rewarding.175
Nonnicotine therapy may include bupropion (Impax Laboratories, Inc., Hayward, CA, USA) and venlafaxine (Pfizer), which help in increasing quit rates. Electronic cigarettes’ role in smoking cessation is uncertain, and they are not US Food and Drug Administration-approved. A few studies have formally evaluated nicotine craving when using electronic cigarettes, with mixed results. Although patients support the use of electronic cigarettes in smoking cessation, more structured studies on safety and efficacy should be done to determine whether these products can play a role in smoking cessation.176
Vaccination
Influenza vaccination is recommended for all patients with COPD. The pneumococcal vaccines PCV13 and PPSV23 are recommended for all patients >65 years of age. PPSV23 is also recommended for younger COPD patients with significant comorbidities, including heart and lung disease.177
Nutritional support
Nutritional supplementation is recommended for malnourished COPD patients. There are positive effects on body weight, fat mass, and fat-free mass when nutritional supplementation is provided and when used during exercise training, and demonstrated significant improvements in 6-minute walk test, respiratory muscle strength, and health status.178
Oxygen therapy
Long-term oxygen therapy is indicated for stable patients who have PaO2 ≤55 mmHg or SaO2 ≤88% with or without hypercapnia confirmed twice over a 3-weeks period, or those with PaO2 of 55–60 mmHg or SaO2 of 88%, evidence of pulmonary artery hypertension, and peripheral edema suggesting of congestive heart failure or polycythemia. Patients should be reevaluated after 2–3 months, with repeat arterial blood gas or SaO2 test done to assess need for continued oxygen therapy.
Ventilatory support
Long-term or nocturnal noninvasive ventilation may be considered in selected COPD patients, especially those with pronounced daytime hypercapnia and history of recurrent/recent hospitalization, although review data are not sufficient to support or refute this recommendation.179
Interventional pulmonology/endoscopic lung-volume reduction
In selected COPD patients with heterogeneous emphysema and significant overinflation refractory to optimized medical treatment, endoscopic lung-volume reduction by placement of endobronchial valves and coils could be considered after thorough evaluation of the individual patient and at highly specialized centers.180
Surgical intervention
In carefully selected COPD patients with large bulla with compressive effects or risk of spontaneous rupture surgical, bullectomy may be considered to relive the compressive effects of bullae. Some thoracic surgery centers in the GCC region are doing such surgeries after complete evaluation. Lung-volume-reduction surgery is another option in selected COPD patients. However, these modalities should be considered only after detailed assessment of patients, including extent and pattern of emphysema on high-resolution CT scan, presence of fissure integrity, absent collateral ventilation, and centers with high expertise.
Lung transplant
This is an option for very severe advanced COPD refractory to maximal pharmacological and nonpharmacological therapy, and following are the criteria for considering lung transplant: COPD patient with progressive disease, not a candidate for endoscopic or surgical lung-volume reduction, BODE index score of 5–6, PaCO2 >50 mmHg and/or PaO2 <60 mmHg, and FEV1 <25% predicted.181 Other variables to be considered include more than three severe exacerbations in last year, exacerbation with hypercapnic respiratory failure, and pulmonary artery hypertension.182
Joint committee recommendations and suggestions to curtail COPD in GCC–MENA region
Accurate information about the prevalence and types of tobacco use is essential to deliver effective public health policy. Implementation of effective public health strategies, including education and awareness of the general public, strict health regulations aimed at smoking reduction, and managing and preventing COPD, is very important. The main obstacle to this is the lack of data related to prevalence and burden of COPD with consequent prohibition in governmental health-planning strategies to curb COPD incidence and prevalence. There is a great deal of room for improvement in COPD care in the GCC–MENA region, and current trends suggest the following developments are possible and highly desirable.
- More accurate data on illness, exacerbations, natural history, cost and deaths related to COPD, particularly in areas where no data are available, will provide a stronger foundation for fighting against COPD.
- Studies of the effectiveness of current prevention, education, medication, rehabilitation, and terminal care will help to spread best practice and drive higher standards of COPD care.
- New therapeutic modalities will inhibit the decline in lung function and improve the overall quality of life of COPD patients.
- As smoking remains the key risk factor for COPD, measures that will reduce the burden of disease include more effective smoking-cessation interventions and techniques to encourage people to quit smoking, strict surveillance of harmful occupational exposure, and protection in early childhood against harmful exposure and events that affect the lung.
- Health ministries and the general public need to be made aware of the high burden of COPD in the MENA region, and these countries should implement common strategies for effective prevention, diagnosis, and treatment of this disabling and life-threatening disease.
Research needs
Comprehensive research is needed in key areas related to COPD:
- As smoking rates in UAE are increasing along with the rise in other risk factors for COPD, with resultant increased COPD incidence and prevalence, there is a need to know how this will affect the course, management, and prognosis of the disease, along with effects on health care systems.
- Although spirometry is a prerequisite in COPD studies, more extensive characterization of the disease than that offered by spirometry is required. Novel imaging techniques and biomarkers offer the potential to characterize subgroups or phenotypes of COPD. Cohort studies should be conducted to assess the long-term natural history of COPD and its phenotypes.
- No data are available about the prevalence, incidence, or natural history of various phenotypes of COPD, and their economic burden on the UAE (studies under progress, personal communication).
- Our knowledge of the pathogenesis of COPD and how this can be modified is still limited. Novel molecular and genetic techniques offer promising possibilities for gaining important knowledge on disease mechanisms, which opens up possibilities for development of new drugs.
Suggestions to health authorities
Strict policies for control of sale of smoking products, prohibition of smoking near schools and public places, imposition of large penalties for violators, and increased tax prices on tobacco and related products should be implemented. Tobacco merchandisers should be obliged to distribute packages displaying graphics stating the negative effects of the smoking habit. However, it is not clear whether these measures would really cut down the prevalence of smoking and COPD morbidity and mortality.
Conclusion
A comprehensive assessment is required for the accurate diagnosis of COPD, assessment of symptoms, and risk of exacerbation. Phenotypic classification may further help. In the MENA region, studies are under way to assess the phenotypic variants of COPD and to correlate various aspects of COPD with phenotypic evaluation, which would give us better insight into the pathogenesis of COPD in the coming years. In the MENA region, most pulmonary physicians follow the standard GOLD recommendations; however with the recent availability of LAMA–LABA/ICS–LABA once daily, triple-combination LAMA–LABA–ICS, newer inhaler devices, and many pharmaceutical companies providing affordable inhalers with good efficacy, we hope that in future pharmacological management of COPD will be more in accordance with GOLD 2017.
In the context of nonpharmacologic management of COPD in the MENA region, there are many shortcomings: most patients are underdiagnosed/undertreated, are diagnosed by general practitioners (GPs) or internal medicine doctors, the unavailability of spirometry for confirmation of diagnosis, noncompliance among patients, low socioeconomic-class patients and patients from various sociodemographic backgrounds with different attitudes about disease and its management, absence of well-structured pulmonary rehabilitation programs, lack of dedicated/trained staff for delivering standard rehabilitation programs in most hospitals, and unaffordability of patients for noninvasive ventilation and oxygen machines.
In the last decade, there have been tremendous improvements in the care of COPD patients in the GCC region, but still the facilities for interventional pulmonology are in their infancy. In the near future, we anticipate some new upcoming state-of-the-art interventional pulmonology centers that will provide endoscopic lung-volume reduction for selected COPD patients. In the GCC region, few centers are doing surgical lung-volume reduction or bullectomy. These centers could broaden the scope of services to cater to increasing number of COPD patients who need surgical interventions. Governments should provide adequate professional training and facilities for the developments of such centers (interventional pulmonology/thoracic surgery and lung-transplant centers) in the GCC region.
Studies are ongoing to evaluate the harmful chemical constituents of shisha and medwakh, and to determine their causal association with COPD. Considering the increased awareness among patients and physicians over last decade, we hope that the nonpharmacological management of COPD will improve on a par with standard evidence-based practice done in other developed countries.
Acknowledgments
The joint committee of the GCC and the MENA region for COPD would like to convey its sincerest thanks for the support from AstraZeneca, Novartis, and Boehringer Ingelheim.
Disclosure
The authors report no conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. 2017. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd. Accessed January 12, 2017. | ||
Murray CJ, Lopez AD, Mathers CD, Stein C. The Global Burden of Disease 2000 project: aims, methods and data sources. 2001. Available from: http://www.who.int/healthinfo/paper36.pdf. Accessed January 22, 2017. | ||
World Health Organization. The Global Burden of Disease: 2004 Update. Geneva: WHO; 2008. | ||
Devine JF. Chronic obstructive pulmonary disease: an overview. Am Health Drug Benefits. 2008;1:34–42. | ||
World Health Organization. Risk factors for chronic respiratory diseases. In: Bousquet J, Khaltaev N, editors. Global Surveillance, Prevention and Control of Chronic Respiratory Diseases: A Comprehensive Approach. Geneva: WHO; 2007:37–55. | ||
Khattab A, Javaid A, Iraqi G, et al. Smoking habits in the Middle East and North Africa: results of the BREATHE study. Respir Med. 2012;106 (Suppl 2):S16–S24. | ||
Riachy M, Rehayem C, Khoury C, et al. [Are narghile smokers different from cigarette smokers?] Rev Mal Respir. 2008;25:313–318. French. | ||
Neergaard J, Singh P, Job J, Montgomery S. Waterpipe smoking and nicotine exposure: a review of the current evidence. Nicotine Tob Res. 2007;9:987–994. | ||
Maziak W, Eissenberg T, Ward KD. Patterns of waterpipe use and dependence: implications for intervention development. Pharmacol Biochem Behav. 2005;80:173–179. | ||
Lindberg A, Eriksson B, Larsson LG, Rönmark E, Sandström T, Lundbäck B. Seven-year cumulative incidence of COPD in an age-stratified general population sample. Chest. 2006;129:879–885. | ||
Kan H, Heiss G, Rose KM, Whitsel E, Lurmann F, London SJ. Traffic exposure and lung function in adults: the Atherosclerosis Risk in Communities study. Thorax. 2007;62:873–879. | ||
Polatli M, Kheder AB, Wali S, et al. Chronic obstructive pulmonary disease and associated healthcare resource consumption in the Middle East and North Africa: the BREATHE study. Respir Med. 2012;106 (Suppl 2):S75–S85. | ||
Yin P, Jiang CQ, Cheng KK, et al. Passive smoking exposure and risk of COPD among adults in China: the Guangzhou Biobank Cohort study. Lancet. 2007;370:751–757. | ||
Eisner MD, Balmes J, Katz PP, Trupin L, Yelin EH, Blanc PD. Lifetime environmental tobacco smoke exposure and the risk of chronic obstructive pulmonary disease. Environ Health. 2005;4:7. | ||
Hu G, Zhou Y, Tian J, et al. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest. 2010;138:20–31. | ||
Lin TC, Krishnaswamy G, Chi DS. Incense smoke: clinical, structural and molecular effects on airway disease. Clin Mol Allergy. 2008;6:3. | ||
Cohen R, Sexton KG, Yeatts KB. Hazard assessment of United Arab Emirates (UAE) incense smoke. Sci Total Environ. 2013;458–460:176–186. | ||
El Hasnaoui A, Rashid N, Lahlou A, Salhi H, Doble A, Nejjari C. Chronic obstructive pulmonary disease in the adult population within the Middle East and North Africa region: rationale and design of the BREATHE study. Respir Med. 2012;106 (Suppl 2):S3–S15. | ||
World Health Organization. Chronic obstructive pulmonary disease (COPD). 2016. Available from: www.who.int/mediacentre/factsheets/fs315/en. Accessed January 15,2017. | ||
Adeloye D, Chua S, Lee CW, et al. Global and regional estimates of COPD prevalence: systemic review and meta-analysis. J Glob Health. 2015;5:020415. | ||
Tageldin MA, Nafti S, Khan JA, et al. Distribution of COPD-related symptoms in the Middle East and North Africa: results of the BREATHE study. Respir Med. 2012;106 (Suppl 2):S25–S32. | ||
Al Zaabi A, Asad F, Abdou J, et al. Prevalence of COPD in Abu Dhabi, United Arab Emirates. Respir Med. 2011;105:566–570. | ||
Mahboub B, Alzaabi A, Soriano JB, et al. Case-finding of chronic obstructive pulmonary disease with questionnaire, peak flow measurements and spirometry: a cross-sectional study. BMC Res Notes. 2014;7:241. | ||
Al Ghobain M, Al-Hajjaj MS, Wali SO. Prevalence of chronic obstructive pulmonary disease among smokers attending primary healthcare clinics in Saudi Arabia. Ann Saudi Med. 2011;31:129–133. | ||
Al Ghobain M, Alhamad EH, Alorainy HS, Al Kassimi F, Lababidi H, Al-Hajjaj MS. The prevalence of chronic obstructive pulmonary disease in Riyadh, Saudi Arabia: a BOLD study. Int J Tuberc Lung Dis. 2015;9:1252–1257. | ||
Al Omari M, Khassawneh BY, Khader Y, Dauod AS, Bergus G. Prevalence of chronic obstructive pulmonary disease among adult male cigarettes smokers: a community-based study in Jordan. Int J Chron Obstruct Pulmon Dis. 2014;9:753–758. | ||
Said AF, Ewis AA, Omran AA, Magdy ME, Saleeb MF. Prevalence and predictors of chronic obstructive pulmonary disease among high-risk Egyptians. Egypt J Bronchol. 2015;9:27–33. | ||
Badway MS, Hamed AF, Yousef FM. Prevalence of chronic obstructive pulmonary disease (COPD) in Qena Governorate. Egypt J Chest Dis Tuberc. 2016;65:29–34. | ||
Waked M, Khayat G, Salameh P. Chronic obstructive pulmonary disease prevalence in Lebanon: a cross-sectional descriptive study. Clin Epidemiol. 2011;3:315–323. | ||
Daldoul H, Denguezli M, Jithoo A, et al. Prevalence of COPD and tobacco smoking in Tunisia: results from the BOLD study. Int J Environ Res Public Health. 2013;10:7257–7271. | ||
El Rhazi K, Nejjari C, BenJelloun MC, El Biaze M, Attassi M, Garcia-Larsen V. Prevalence of chronic obstructive pulmonary disease in Fez, Morocco: results from the BOLD study. Int J Tuberc Lung Dis. 2016;20:136–141. | ||
World Health Organization. Prevalence of tobacco smoking. Available from: http://www.who.int/gho/tobacco/use/en. Accessed January 15, 2017. | ||
Jithoo A, Enright PL, Burney P, et al. Case-finding options for COPD: results from the Burden of Obstructive Lung Disease Study. Eur Respir J. 2013;41:548–555. | ||
Menezes AM, Perez-Padilla R, Jardim JR, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366:1875–1881. | ||
Landis SH, Muellerova H, Mannino DM, et al. Continuing to Confront COPD international patient survey: methods, COPD prevalence, and disease burden in 2012–2013. Int J Chron Obstruct Pulmon Dis. 2014;9:597–611. | ||
Kart L, Akkoyunlu ME, Bayram M, et al. COPD: an underdiagnosed disease at hospital environment. Wien Klin Wochenschr. 2014;126:73–78. | ||
Eisner MD, Anthonisen N, Coultas D, et al. An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182:693–718. | ||
Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362:847–852. | ||
Khattab A, Javaid A, Iraqi G, et al. Smoking habits in the Middle East and North Africa: results of the BREATHE study. Respir Med. 2012;106 (Suppl 2):S16–S24. | ||
Al Zaabi A, Mahboub BH, Vats MG, Iqbal MN, Vats DM. Chronic obstructive pulmonary disease in Middle East and UAE: an unrecognized underestimated epidemic. J Lung Pulm Respir Res. 2016;3:00089. | ||
Maziak W, Ward KD, Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tob Control. 2004;13:327–333. | ||
Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of water pipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39:834–857. | ||
She J, Yang P, Wang Y, et al. Chinese water-pipe smoking and the risk of COPD. Chest. 2014;146:924–931. | ||
Haddad L, Kelly DL, Weglicki LS, Barnett TE, Ferrell AV, Ghadban R. A systematic review of effects of waterpipe smoking on cardiovascular and respiratory health outcomes. Tob Use Insights. 2016;9:13–28. | ||
Salameh P, Waked M, Khoury F, et al. Waterpipe smoking and dependence are associated with chronic bronchitis: a case-control study in Lebanon. East Mediterr Health J. 2012;18:996–1004. | ||
Mohammad Y, Shaaban R, Al-Zahab BA, Khaltaev N, Bousquet J, Dubaybo B. Impact of active and passive smoking as risk factors for asthma and COPD in women presenting to primary care in Syria: first report by the WHO-GARD survey group. Int J Chron Obstruct Pulmon Dis. 2013;8:473–482. | ||
Al-Houqani M, Ali R, Hajat C. Tobacco smoking using medwakh is an emerging health problem: evidence from a large cross-sectional survey in the United Arab Emirates. PLoS One. 2012;7:e39189. | ||
Salameh P, Salame J, Khayat G, et al. Exposure to outdoor air pollution and chronic bronchitis in adults: a case-control study. Int J Occup Environ Med. 2012;3:165–177. | ||
Waked M, Salame J, Khayat G, Salameh P. Correlates of COPD and chronic bronchitis in nonsmokers: data from a cross-sectional study. Int J Chron Obstruct Pulmon Dis. 2012;7:577–585. | ||
Denguezli M, Daldoul H, Harrabi I, et al. COPD in nonsmokers: reports from the Tunisian population-based Burden of Obstructive Lung Disease study. PLoS One. 2016;11:e0151981. | ||
Gauderman WJ, Avol E, Gilliland F, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med. 2004;351:1057–1067. | ||
Gauderman WJ, Vora H, McConnell R, et al. Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study. Lancet. 2007;369:571–577. | ||
Rojas-Martinez R, Perez-Padilla R, Olaiz-Fernandez G, et al. Lung function growth in children with long-term exposure to air pollutants in Mexico City. Am J Respir Crit Care Med. 2007;176:377–384. | ||
Downs SH, Schindler C, Liu LJ, et al. Reduced exposure to PM10 and attenuated age-related decline in lung function. N Engl J Med. 2007;357:2338–2347. | ||
Euler G, Abbey D, Magie A, Hodgkin J. Chronic obstructive pulmonary disease symptom effects of long-term cumulative exposure to ambient levels of total suspended particulates and sulfur dioxide in California Seventh-Day Adventist residents. Arch Environ Health. 1987;42:213–222. | ||
Abbey D, Burchette R, Knutsen S, McDonnel W, Lebowitz M, Enright P. Long-term particulate and other pollutants and lung function in nonsmokers. Am J Respir Crit Care Med. 1998;158:289–298. | ||
Schikowski T, Sugiri D, Ranft U, et al. Long-term air pollution exposure and living close to busy roads are associated with COPD in women. Respir Res. 2005;6:152. | ||
Andersen ZJ, Hvidberg M, Jensen SS, et al. COPD and long-term exposure to traffic-related air pollution: a cohort study. Am J Respir Crit Care Med. 2011;183:455–461. | ||
Smith KR. Biofuels, Air Pollution, and Health. New York: Plenum Press; 1987. | ||
Pandey M, Basnyat B, Neupane R. Chronic bronchitis and cor pulmonale in Nepal. Lung India. 1988;6:209–210. | ||
Albalak R, Frisancho AR, Keeler GJ. Domestic biomass fuel combustion and chronic bronchitis in two rural Bolivian villages. Thorax. 1999;54:1004–1008. | ||
Behera D. An analysis of effect of common domestic fuels on respiratory function. Indian J Chest Dis Allied Sci. 1997;39:235–243. | ||
Behera D, Jindal SK. Respiratory symptoms in Indian women using domestic cooking fuels. Chest. 1991;100:385–388. | ||
Behera D, Jindal SK, Malhotra HS. Ventilatory function in non-smoking rural Indian women using different cooking fuels. Respiration. 1994;61:89–92. | ||
Cetinkaya F, Gülmez I, Aydin T, Oztürk Y, Ozesmi M, Demir R. Prevalence of chronic bronchitis and associated risk factors in a rural area of Kayseri, central Anatolia, Turkey. Monaldi Arch Chest Dis. 2000;55:189–193. | ||
Dossing M, Khan J, al-Rabiah F. Risk factors for chronic obstructive lung disease in Saudi Arabia. Respir Med. 1994;88:519–522. | ||
Ekici A, Ekici M, Kurtipek E, et al. Obstructive airway diseases in women exposed to biomass smoke. Environ Res. 2005;99:93–98. | ||
Kiraz K, Kart L, Demir R, et al. Chronic pulmonary disease in rural women exposed to biomass fumes. Clin Invest Med. 2003;26:243–248. | ||
Pandey MR. Domestic smoke pollution and chronic bronchitis in a rural community of the hill region of Nepal. Thorax. 1984;39:337–339. | ||
Pérez-Padilla R, Regalado J, Vedal S, et al. Exposure to biomass smoke and chronic airway disease in Mexican women: a case-control study. Am J Respir Crit Care Med. 1996;154:701–706. | ||
Regalado J, Pérez-Padilla R, Sansores R, et al. The effect of biomass burning on respiratory symptoms and lung function in rural Mexican women. Am J Respir Crit Care Med. 2006;174:901–905. | ||
Shrestha IL, Shrestha SL. Indoor air pollution from biomass fuels and respiratory health of the exposed population in Nepalese households. Int J Occup Environ Health. 2005;11:150–160. | ||
Menezes AM, Victora CG, Rigatto M. Prevalence and risk factors for chronic bronchitis in Pelotas, RS, Brazil: a population-based study. Thorax. 1994;49:1217–1221. | ||
Dutt D, Srinivasa DK, Rotti SB, Sahai A, Konar D. Effect of indoor air pollution on the respiratory system of women using different fuels for cooking in an urban slum of Pondicherry. Natl Med J India. 1996;9:113–117. | ||
Ellegard A. Cooking fuel smoke and respiratory symptoms among women in low-income areas in Maputo. Environ Health Perspect. 1996;104:980–985. | ||
Liu S, Zhou Y, Wang X, et al. Biomass fuels are the probable risk factor for chronic obstructive pulmonary disease in rural south China. Thorax. 2007;62:889–897. | ||
Dennis RJ, Maldonado D, Norman S, Baena E, Martinez G. Wood-smoke exposure and risk for obstructive airways disease among women. Chest. 1996;109:115–119. | ||
Orozco-Levi M, Garcia-Aymerich J, Villar J, Ramirez-Sarmiento A, Anto JM, Gea J. Wood smoke exposure and risk of chronic obstructive pulmonary disease. Eur Respir J. 2006;27:542–546. | ||
Caballero A, Torres-Duque CA, Jaramillo C, et al. Prevalence of COPD in five Colombian cities situated at low, medium, and high altitude (PREPOCOL study). Chest. 2008;133:343–349. | ||
Aljarallah B, Ali A, Dowaidar M, Settin A. Prevalence of α-1-antitrypsin gene mutations in Saudi Arabia. Saudi J Gastroenterol. 2011;17:256–260. | ||
Brown PJ, Greville HW, Finucane KE. Asthma and irreversible airflow obstruction. Thorax. 1984;39:131–136. | ||
Ulrik CS, Backer V. Nonreversible airflow obstruction in life-long nonsmokers with moderate to severe asthma. Eur Respir J. 1999;14:892–896. | ||
Cassino C, Berger KI, Goldring RM, et al. Duration of asthma and physiologic outcomes in elderly nonsmokers. Am J Respir Crit Care Med. 2000;162:1423–1428. | ||
Connolly CK, Chan NS, Prescott RJ. The relationship between age and duration of asthma and the presence of persistent obstruction in asthma. Postgrad Med J. 1988;64:422–425. | ||
Beaglehole R, Bonita R, Alleyne G, et al. UN High-Level Meeting on Non-Communicable Diseases: addressing four questions. Lancet. 2011;378:449–455. | ||
European COPD Coalition. Prevalence in EU. Available from: http://www.copdcoalition.eu/about-copd/prevalence. Accessed January 14, 2017. | ||
Chapman KR, Mannino DM, Soriano JB, et al. Epidemiology and costs of chronic obstructive pulmonary disease. Eur Respir J. 2006;27:188–207. | ||
Centers for Disease Control and Prevention. Chronic obstructive pulmonary disease among adults: United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:938–943. | ||
Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD. 2006;3:211–218. | ||
Mehrotra A, Oluwole AM, Gordon SB. The burden of COPD in Africa: a literature review and prospective survey of the availability of spirometry for COPD diagnosis in Africa. Trop Med Int Health. 2009;14:840–848. | ||
Shaya FT, El Khoury AC, Samant ND, Scharf SM. Utilization of health care resources in a high-risk Medicaid population with chronic obstructive pulmonary disease. Phys Ther. 2006;31:261–268. | ||
Menzin J, Boulanger L, Marton J, et al. The economic burden of chronic obstructive pulmonary disease (COPD) in a U.S. Medicare population. Respir Med. 2008;102:124856. | ||
Chung F, Barnes N, Allen M, et al. Assessing the burden of respiratory disease in the UK. Respir Med. 2002;96:963–975. | ||
Mannino DM, Bradman S. The epidemiology and economics of chronic pulmonary obstructive disease. Proc Am Thorac Soc. 2007;4:502–506. | ||
Wouters EF. The burden of COPD in the Netherlands: results from the Confronting COPD survey. Respir Med. 2003;97 (Suppl C):S51–S59. | ||
Wouters EF. Economic analysis of the Confronting COPD survey: an overview of results. Respir Med. 2003;97 (Suppl C):S3–S14. | ||
Simon-Tuval T, Scharf SM, Maimon N, Bernhard-Scharf BJ, Reuveni H, Tarasiuk A. Determinants of elevated healthcare utilization in patients with COPD. Respir Res. 2011;12:7. | ||
Dalal AA, Shah M, Lunacsek O, Hanania NA. Clinical and economic burden of patients diagnosed with COPD with comorbid cardiovascular disease. Respir Res. 2011;105:1516–1522. | ||
Alzaabi A, Mahboub B, Salhi H, Kajingu W, Rashid N, El-Hasnaoui A. Waterpipe use in the Middle East and North Africa: data from the Breathe study. Nicotine Tob Res. Epub 2016 Oct 10. | ||
Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J. 2011;37:264–272. | ||
de los Monteros MJ, Peña C, Hurtado EJ, Jareño J, Miravitlles M. Variability of respiratory symptoms in severe COPD. Arch Bronconeumol. 2012;48:3–7. | ||
Zwar NA, Marks GB, Hermiz O, et al. Predictors of accuracy of diagnosis of chronic obstructive pulmonary disease in general practice. Med J Aust. 2011;195:168–171. | ||
Simon PM, Schwartzstein RM, Weiss JW, Fencl V, Teghtsoonian M, Weinberger SE. Distinguishable types of dyspnea in patients with shortness of breath. Am Rev Respir Dis. 1990;142:1009–1014. | ||
Burrows B, Niden AH, Barclay WR, et al. Chronic obstructive lung disease – II: relationship of clinical and physiologic findings to the severity of airways obstruction. Am Rev Respir Dis. 1965;91:665–678. | ||
[No authors listed]. Definition and classification of chronic bronchitis for clinical and epidemiological purposes. Lancet. 1965;1:775–779. | ||
Schols AM, Soeters PB, Dingemans AM, Mostert R, Frantzen PJ, Wouters EF. Prevalence and characteristics of nutritional depletion in patients with stable COPD eligible for pulmonary rehabilitation. Am Rev Respir Dis. 1993;147:1151–1156. | ||
Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157:1791–1797. | ||
Holguin F, Folch E, Redd SC, Mannino DM. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest. 2005;128:2005–2011. | ||
Kesten S, Chapman KR. Physician perceptions and management of COPD. Chest. 1993;104:254–258. | ||
Loveridge B, West P, Kryger MH, Anthonisen NR. Alteration in breathing pattern with progression of chronic obstructive pulmonary disease. Am Rev Respir Dis. 1986;134:930–934. | ||
Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968. | ||
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–586. | ||
Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121:1434–1440. | ||
Jones PW. Health status measurement in chronic obstructive pulmonary disease. Thorax. 2001;56:880–887. | ||
Jones P, Tabberer M, Chen WH. Creating scenarios of the impact of COPD and their relationship to COPD assessment test (CATTM) scores. BMC Pul Med. 2011;11:42. | ||
Jones PW, Adamek L, Nadeau G, Banik N. Comparisons of health status scores with MRC grades in COPD: implications for the GOLD 2011 classification. Eur Respir J. 2013;42:647–654. | ||
Jones PW. COPD assessment test: rationale, development, validation and performance. COPD. 2013;10:269–271. | ||
van der Molen T, Willemse BW, Schokker S, ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the clinical COPD questionnaire. Health Qual Life Outcomes. 2003;1:13. | ||
Reda AA, Kotz D, Kocks JW, Wesseling G, van Schayck CP. Reliability and validity of the clinical COPD questionnaire and chronic respiratory questionnaire. Respir Med. 2010;104:1675–1682. | ||
Miller MR, Hankinson J, Brusasco V, et al. Standardization of spirometry. Eur Respir J. 2005;26:319–338. | ||
Buist AS, Mcburnie MA, Vollmer WM, et al. International variations in the prevalence of COPD (the BOLD study): a population based prevalence study. Lancet. 2007;370:741–750. | ||
Hurst JR, Wedzicha JA. What is (and what is not) a COPD exacerbation: thoughts from the new GOLD guidelines. Thorax. 2007;62:198–199. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363:1128–1138. | ||
Soler-Cataluña JJ, Martínez-García MA, Sánchez PR, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60:925–931. | ||
Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128:2099–2107. | ||
Lange P, Nyboe J, Appleyard M, Jensen G, Schnohr P. Ventilatory function and chronic mucus hypersecretion as predictors of death from lung cancer. Am Rev Respir Dis. 1990;141:613–617. | ||
Skillrud DM, Offord KP, Miller RD. Higher risk of lung cancer in chronic obstructive pulmonary disease: a prospective, matched, controlled study. Ann Intern Med. 1986;105:503–507. | ||
Burgel PR, Roche N, Paillasseur JL, et al. Clinical COPD phenotypes identified by cluster analysis: validation with mortality. Eur Respir J. 2012;40:495–496. | ||
Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish COPD guidelines (GesEPOC): pharmacological treatment of stable COPD. Arch Bronconeumol. 2012;48:247–257. | ||
Garcia-Aymerich J, Gómez FP, Benet M, et al. Identification and prospective validation of clinically relevant chronic obstructive pulmonary disease (COPD) phenotypes. Thorax. 2011;66:430–437. | ||
Sin DD, Miravitlles M, Mannino DM, et al. What is asthma-COPD overlap syndrome (ACOS)? Towards a consensus definition from a round table discussion. Eur Respir J. 2016;48:664–673. | ||
Pavord ID, Lettis S, Locantore N, et al. Blood eosinophils and inhaled corticosteroid/long-acting β-2 agonist efficacy in COPD. Thorax. 2016;71:118–125. | ||
Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomized controlled trials. Lancet Respir Med. 2015;3:435–442. | ||
Bafadhel M, Davies L, Calverley PM, Aaron SD, Brightling CE, Pavord ID. Blood eosinophil guided prednisolone therapy for exacerbations of COPD: a further analysis. Eur Respir J. 2014;44:789–791. | ||
Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med. 2003;348:2059–2073. | ||
Kelly AM, McAlpine R, Kyle E. How accurate are pulse oximeters in patients with acute exacerbations of chronic obstructive airways disease? Respir Med. 2001;95:336–340. | ||
Pinto-Plata VM, Cote C, Cabral H, Taylor J, Celli BR. The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J. 2004;23:28–33. | ||
Oga T, Nishimura K, Tsukino M, Sato S, Hajiro T. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health status. Am J Respir Crit Care Med. 2003;167:544–549. | ||
Jones PW. Health status measurement in chronic obstructive pulmonary disease. Thorax. 2001;56:880–887. | ||
Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–1012. | ||
Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359:1543–1554. | ||
Beeh KM, Singh D, Di Scala L, Drollmann A. Once-daily NVA237 improves exercise tolerance from the first dose in patients with COPD: the GLOW3 trial. Int J Chron Obstruct Pulmon Dis. 2012;7:503–513. | ||
Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356:775–789. | ||
Decramer ML, Chapman KR, Dahl R, et al. Once-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group study. Lancet Respir Med. 2013;1:524–533. | ||
Vogelmeier C, Hederer B, Glaab T, et al. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011;364:1093–1103. | ||
Singh D. New combination bronchodilators for chronic obstructive pulmonary disease: current evidence and future perspectives. Br J Clin Pharmacol. 2015;79:695–708. | ||
Bateman ED, Chapman KR, Singh D, et al. Aclidinium bromide and formoterol fumarate as a fixed-dose combination in COPD: pooled analysis of symptoms and exacerbations from two six-month, multicentre, randomised studies (ACLIFORM and AUGMENT). Respir Res. 2015;16:92. | ||
Wedzicha JA, Decramer M, Ficker JH, et al. Analysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group study. Lancet Respir Med. 2013;1:199–209. | ||
Wedzicha JA, Singh D, Vestbo J, et al. Extrafine beclomethasone/formoterol in severe COPD patients with history of exacerbations. Respir Med. 2014;108:1153–1162. | ||
Singh D, Corradi M, Spinola M, Petruzzelli S, Papi A. Extrafine beclometasone diproprionate/formoterol fumarate: a review of its effects in chronic obstructive pulmonary disease. NPJ Prim Care Respir Med. 2016;26:16030. | ||
Loke YK, Cavallazzi R, Singh S. Risk of fractures with inhaled corticosteroids in COPD: systematic review and meta-analysis of randomised controlled trials and observational studies. Thorax. 2011;66:699–708. | ||
Wang JJ, Rochtchina E, Tan AG, Cumming RG, Leeder SR, Mitchell P. Use of inhaled and oral corticosteroids and the long-term risk of cataract. Ophthalmology. 2009;116:652–657. | ||
Suissa S, Kezouh A, Ernst P. Inhaled corticosteroids and the risks of diabetes onset and progression. Am J Med. 2010;123:1001–1006. | ||
Lee CH, Kim K, Hyun MK, Jang EJ, Lee NR, Yim JJ. Use of inhaled corticosteroids and the risk of tuberculosis. Thorax. 2013;68:1105–1113. | ||
Crim C, Dransfield MT, Bourbeau J, et al. Pneumonia risk with inhaled fluticasone furoate and vilanterol compared with vilanterol alone in patients with COPD. Ann Am Thorac Soc. 2015;12:27–34. | ||
Festic E, Scanlon PD. Incident pneumonia and mortality in patients with chronic obstructive pulmonary disease: a double effect of inhaled corticosteroids? Am J Respir Crit Care Med. 2015;191:141–148. | ||
Wedzicha JA, Banerji D, Chapman KR, et al. Indacaterol-glycopyrronium versus salmeterol-fluticasone for COPD. N Engl J Med. 2016;374:2222–2234. | ||
Welte T, Miravitlles M, Hernandez P, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;180:741–750. | ||
Singh D, Papi A, Corradi M, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388:963–973. | ||
Martinez FJ, Calverley PM, Goehring UM, Brose M, Fabbri LM, Rabe KF. Effect of roflumilast on exacerbations in patients with severe chronic obstructive pulmonary disease uncontrolled by combination therapy (REACT): a multicentre randomised controlled trial. Lancet. 2015;385:857–866. | ||
Han MK, Tayob N, Murray S, et al. Predictors of chronic obstructive pulmonary disease exacerbation reduction in response to daily azithromycin therapy. Am J Respir Crit Care Med. 2014;189:1503–1508. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363:1128–1138. | ||
Siddiqui SH, Guasconi A, Vestbo J, et al. Blood eosinophils: a biomarker of response to extrafine beclomethasone/formoterol in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;192:523–525. | ||
Pascoe S, Locantore N, Dransfield M, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015;3:435–442. | ||
Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Resp Crit Care Med. 2013;188:e13–e64. | ||
Garvey C, Bayles MP, Hamm LF, et al. Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary disease: review of selected guidelines. J Cardiopulm Rehabil Prev. 2016;6:75–83. | ||
Ries AL, Make BJ, Lee SM, et al. The effects of pulmonary rehabilitation in the National Emphysema Treatment Trial. Chest. 2005;128:3799–3809. | ||
Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155:179–191. | ||
Puhan MA, Scharplatz M, Troosters T, Steurer J. Respiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality: a systematic review. Respir Res. 2005 Jun 8;6:54. | ||
Ortega F, Toal J, Cejudo P, et al. Comparison of effects of strength and endurance training in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care Med. 2002;166:669–674. | ||
Garber CE, Blissmer B, Deschenes MR, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuro-motor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. | ||
Horowitz MB, Littenberg B, Mahler DA. Dyspnea ratings for prescribing exercise intensity in patients with COPD. Chest. 1996;109:1169–1175. | ||
Scanlon PD, Connett JE, Waller LA, et al. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease: the Lung Health Study. Am J Respir Crit Care Med. 2000;161:381–390. | ||
Pelkonen M, Tukiainen H, Tervahauta M, et al. Pulmonary function, smoking cessation and 30-year mortality in middle aged Finnish men. Thorax. 2000;55:746–750. | ||
Carmody TP, Duncan C, Simon JA, et al. Hypnosis for smoking cessation: a randomized trial. Nicotine Tob Res. 2008;10:811–818. | ||
Odum LE, O’Dell KA, Schepers JS. Electronic cigarettes: do they have a role in smoking cessation? J Pharm Pract. 2012;25:611–614. | ||
Tomczyk S, Bennett NM, Stoecker C, et al. Use of 13-valent pneumococcal conjugate vaccine and 23-valent vaccine among adults aged ≥65 years: recommendations of the Advisory Committee on Immunization Practice (ACIP), MMWR Morb Mortal Wkly Rep. 2014;63:822–825. | ||
Ferreira IM, Brooks D, White J, Goldstein R. Nutritional supplementation for stable COPD. Cochrane Database Syst Rev. 2012;12:CD000998. | ||
Struik FM, Lacasse Y, Goldstein R, Kerstjens HM, Wijkstra PJ. Nocturnal non-invasive positive pressure for stable COPD. Cochrane Database Syst Rev. 2013:CD002878. | ||
Tiong LU, Davies R, Gibson PG, et al. Lung volume reduction surgery for diffuse emphysema. Cochrane Database Syst Rev. 2006:CD001001. | ||
Weill D, Benden C, Corris PA, et al. A consensus document for the selection of lung transplant candidates – 2014: an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2015;34:1–15. | ||
International Society for Heart and Lung Transplantation. Overall lung transplantation statistics. 2016. Available from: https://www.ishlt.org/registries/slides.asp?slides=heartLungRegistry. Accessed July 19, 2017. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.