Back to Journals » Journal of Pain Research » Volume 15
Is There a Difference in Fear-Avoidance, Beliefs, Anxiety and Depression Between Post-Surgery and Non-Surgical Persistent Spinal Pain Syndrome Patients?
Authors Alves Rodrigues T , de Oliveira EJSG , Morais Costa B, Tajra Mualem Araújo RL , Batista Santos Garcia J
Received 6 November 2021
Accepted for publication 5 February 2022
Published 16 June 2022 Volume 2022:15 Pages 1707—1717
DOI https://doi.org/10.2147/JPR.S348146
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Erika Petersen
Thiago Alves Rodrigues, Eduardo José Silva Gomes de Oliveira, Beatriz Morais Costa, Rayanne Luiza Tajra Mualem Araújo, João Batista Santos Garcia
Chronic Pain Clinic, University Hospital of the Federal University of Maranhão (HU-UFMA), São Luís, Maranhão, Brazil
Correspondence: Thiago Alves Rodrigues, Chronic Pain Clinic, University Hospital of the Federal University of Maranhão (HU-UFMA), Rua do Farol, n. 05. Ed Porto Real, Ap 1101, Ponta do Farol, São Luis, Maranhão, Brazil, CEP 65077-450, Email [email protected]
Introduction: Patients with post-surgery persistent spinal pain syndrome (PSPS) or non-surgical PSPS might be affected by sustained fear-avoidance beliefs (FAB), anxiety and depression. In this scenario, this study aimed to describe those aspects in patients with post-surgery PSPS and non-surgical PSPS.
Methods: This study included patients with PSPS, and non-surgical PSPS, over 18 years, with quarterly evaluations at the Chronic Pain Clinic. After evaluation, demographic and clinical characteristics were obtained. The Beck Depression Inventory-II, Beck Anxiety Inventory, Douleur neuropathique 4 questions, Visual Analog Pain Scale, and Fear-Avoidance Beliefs Questionnaire–Brazilian Version (FABQ-Brazil) were used to evaluate psychological aspects.
Results: Forty-six patients were included, 23 patients with post-surgery PSPS and 23 with non-surgical PSPS. Both groups had high scores in the physical and work domains of the FABQ, high rates of absenteeism and most patients in these groups had moderate-to-severe neuropathic pain and some degree of anxiety and/or depression. The groups showed no statistically significant difference (p > 0.05) when comparing all questionnaires.
Discussion: This is one of the first studies to evaluate FAB and other associated psychological factors, such as anxiety and depression, in patients with post-surgery PSPS in a follow-up several years after surgery and compare with patients diagnosed with non-surgical PSPS. In this study, most patients in both groups had high scores in the FABQ domains, not having statistically relevant difference between groups.
Conclusion: Even though there was no statistically relevant difference between the PSPS patient with or without surgical history in terms of the assessed outcome measures, the described scores for fear-avoidance beliefs, pain, anxiety and depression were high, showing an interference in the daily life activities of those patients.
Keywords: fear, depression, anxiety, spine surgery, back pain
Introduction
A significant proportion of patients submitted to lumbar spine surgery present persistent pain with difficult management and worsening of functional capacity1–5.The usual definition of this situation as failed back surgery syndrome includes beliefs that failure of treatment worsens the patient’s condition pathologically, psychologically or both.1–3,6
As the term has been considered an inappropriate and illogical term, some authors have proposed the use of other terms, such as “post lumbar surgery syndrome” (PLSS),6–9 and the new IASP classification, “chronic pain after spinal surgery” (CPSS).10,11 The IASP recommendations eliminate certain terminology such as FBSS in favor of “chronic pain after spinal surgery” (CPSS).10,11 While the elimination of the FBSS terminology may be welcome, the new framework does not fully account for all patients with chronic spinal pain.12
An expert group of pain practitioners and neurosurgeons proposed a replacement terminology, “persistent spinal pain syndrome,” (PSPS), which is divided into Type 1 (no surgery performed) and Type 2 (post-surgery).13 PSPS encompasses the diverse potential symptoms of a syndrome of chronic pain (as per the usual criteria for establishing pain persistence) or recurrent pain of spinal origin, paresthesia, numbness, stiffness, muscle spasms and weakness, and, in some cases, sphincter disturbance. Spinal surgery may or may not have occurred and may or may not be relevant in particular cases.12,13
This definition includes a sense of a prior situation which then continues despite interventions, such as surgery, or altered circumstances (eg, giving up a physically demanding job). The symptoms are chronic, but the underlying predisposition and promoter, are persistent.12,13
The PSPS occurs in between 10% and 40% of the surgeries performed. These patients present a history of chronic axial pain, with or without radicular pain, and may be associated with changes in sensitivity and exacerbation of pain after movement.1–5 Treatment options for PSPS include physical therapy, pain medication, interventional procedures (eg lumbar steroid injections and percutaneous/endoscopic adhesiolysis), neurostimulation and reoperations.4,9
There are several potential anatomical sources of pain in the PSPS. Nociceptive fibres innervate the ligaments of the intervertebral disc complex, facet joints, and myofascial syndrome in paravertebral musculature. They can all play a part in the pathogenesis of the chronic low back pain (CLBP) component in PSPS.14
The events leading to muscular pain probably occur during and after the surgical procedure. During surgery, dissection and prolonged retraction of the paraspinal musculature result in denervation and atrophy14. Major post-operative causes of pain include epidural fibrosis, recurrent disc herniation, stenosis, instability secondary to altered biomechanics following surgery and myofascial pain development. Also, preoperative and intraoperative factors can lead to PSPS, such as poor surgical technique, incorrect level of operation, improper preoperative patient selection and inability to achieve the aim of the surgery in difficult cases.15 Magnetic Resonance Imaging (MRI) has been the most significant and reliable tool for assessing intervertebral disc pathology, with its signal characteristics reflecting the findings of aging or degeneration.16
As PSPS is a chronic pain syndrome resistant to treatment, it affects the social function, work, and daily living of these patients, causing emotional discomfort. As a result, there may be a negative impact on family, social and professional relationships, generating depression, anxiety, and disability, which determine deterioration in the general quality of life.17,18
This condition can be aggravated by fear-avoidance beliefs, in which patients routinely consider the implications of symptoms and the consequences of future actions, associating physical and work activities to worsening or maintaining the painful condition. Such behavior leads to a reduction in physical and work activities, associated with a deterioration in the quality of life and family dynamics, situations of drug dependence, and excessive use of medical services, which can worsen the prognosis of treatment and prolong the rehabilitation process.19,20
The subject of fear-avoidance beliefs in PSPS over a long time span after surgery has been little addressed in the literature. Its approach, together with the assessment of pain and its characteristics and of other psychological factors, such as anxiety and depression, may help to understand how these factors are related. This study aimed to describe the characteristics of patients diagnosed with PSPS in terms of fear-avoidance beliefs, anxiety, and depression and describe magnetic resonance imaging (MRI) findings on surgical PSPS, as it is necessary to better understand how this dynamic can present an important impact on the daily living of these patients.
Materials and Methods
This is a descriptive cross-sectional study that included patients diagnosed with PSPS, with history of lumbar spine surgery for an MRI verified single-level lumbar disc herniation, and non-surgical PSPS, over 18 years of age, who underwent regular follow-up, with medical evaluation every four months at the Chronic Pain Outpatient Clinic of the University Hospital of the Federal University of Maranhão (HUUFMA), from March 2020 to March 2021, in the city of São Luís, state of Maranhão, in northeastern Brazil (Figure 1).
 |
Figure 1 Study flowchart. |
PSPS was identified using the diverse potential symptoms of a syndrome of chronic pain (as per the usual criteria for establishing pain persistence) or recurrent pain of spinal origin, paresthesia, numbness, stiffness, muscle spasms and weakness, and, in some cases, sphincter disturbance. Spinal surgery may or may not have occurred.13
The study was evaluated and accepted by the Ethics Committee of HUUFMA (CAAE 22801019.0.0000.5086/Number 3.804.613). To begin the evaluation, patients were asked about their interest in participating in the study and signed a written informed consent form.
After clinical evaluation, forms were used to obtain the demographic and clinical characteristics of patients. The Beck Depression Inventory-II (BDI-II) and Beck Anxiety Inventory (BAI)21 questionnaires were applied to evaluate anxiety and depression. The scales Douleur neuropathique 4 questions (DN4)22 and Visual Analog Pain Scale (VAS) were used to characterize and measure pain. The Fear-Avoidance Beliefs Questionnaire–Brazilian Version (FAB-Brazil)23,24 was used to specifically assess fear-avoidance beliefs. Also, MRI results in the medical record were evaluated for the presence or absence of abnormalities at each level of the lumbar spine.
BDI-II, a well-known questionnaire to evaluate depression, is composed of 21 items that assess the severity of depressive symptoms on a Likert scale of 0 to 3. In relation to the cut-off points, values between 0 and 13 are considered as “minimum or absence of depression”, values between 14 and 19 as “mild depression”, values between 20 and 28 as “moderate depression” and values between 29 and 63 as “severe depression”.21
BAI, a well-known questionnaire to evaluate anxiety, consists of 21 items describing common symptoms of anxiety on a Likert scale of 0 to 3. For cut-off points, values between 0 and 10 are considered as “minimal or no anxiety”, 11 to 19 “mild anxiety”, 20 to 30 “moderate anxiety” and 31 to 63 “severe anxiety”.21
DN4 is composed of seven items that refer to symptoms and another three that relate to the physical examination, ranging from 0 to 10 points. Values equal to or greater than 4 suggest neuropathic pain.22
The FABQ-Brazil consists of 16 self-reporting items, scored from 0 to 6 on a Likert scale, which is divided into two sub-scales: the one that addresses the fears and beliefs of individuals about physical activities (FABQ-Phys) and work (FABQ-Work). A higher score indicates more strongly held beliefs to avoid physical or work activity out of fear. Scores greater than 15 for FABQ-Phys and greater than 34 for FABQ-Work are considered high values for the belief to avoid physical and work activities out of fear.23–26
The registered population with a diagnosis of post-surgery PSPS followed up in the chronic pain clinic and with the last follow-up performed up to 3 years ago, corresponded to 30 patients. For a confidence interval of 95% and margin of error of 10%, a sample size of 23 patients was found. For comparison purposes, an equal number of patients with chronic low back pain of non-surgical origin were included.
The data were organized in Microsoft Office Excel® and analyzed using the statistical program SPSS 26.0®. For the analysis of numerical variables, the results are presented as the mean, standard deviation, median, minimum, and maximum values, with categorical data shown as absolute (n) and relative (%) frequencies. Normality was verified through the Shapiro–Wilk test. The numerical Student’s t-test was performed for data with a normal distribution and the Mann–Whitney test for those without a normal distribution.
Results
Forty-six patients with regular quarterly follow-up at the Chronic Pain Outpatient Clinic were included in the study, 23 patients diagnosed with post-surgery PSPS (Group 1 – G1) and 23 patients with non-surgical PSPS (Group 2 – G2) (Table 1). Patients with post-surgery PSPS had a spine surgery history with a median of 9 years. Of the total number of patients, 63% (n = 29) had comorbidities, with hypertension (66%), diabetes mellitus (58%) and dyslipidemia (55%) being the most frequent.
 |
Table 1 Sociodemographic Characteristics |
Regarding non-pharmacological treatment, 52.17% (n = 12) in G1 and 52.17% (n = 12) in G2 did some form of rehabilitation. In the pharmacological treatment, among patients with post-surgery PSPS and non-surgical PSPS, used mostly simple analgesics, gabapentinoids, weak or strong opioids, muscle relaxants, tricyclic antidepressants and selective serotonin reuptake inhibitors serotonin and norepinephrine reuptake inhibitors (Table 2). About the use of gabapentinoids, 80% and 83.33% of G1 and G2 used gabapentin, a drug available through the public health system.
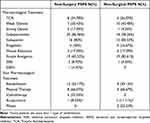 |
Table 2 Pharmacological and Non-Pharmacological Treatment |
Being a small sample and due to the relevance of the problem, intragroup homogeneity can be observed from the prevalence of the use of drugs with psychotropic action, including gabapentinoids, SSRIs, SSRNs, and TCAs (Table 3). Thus, even though there is a multiplicity of medications when evaluating patients individually, this assessment reflects the reality of chronic pain patients.
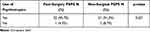 |
Table 3 Use of Psychotropic Agents in PSPS and Non-Surgical PSPS Patients |
The groups showed no statistically significant difference (p > 0.05) when compared with the scores of the VAS, DN4, FABQ-Phys, FABQ-WORK, BDI-II and BAI questionnaires and total dose of gabapentinoids (Table 4).
 |
Table 4 Pain Evaluation, Anxiety, Depression and Fear-Avoidance Beliefs Scores |
Concerning the FABQ questionnaire, in G1, 69.57% (n = 16) and in G2, 65.22% (n = 15) had high scores (≥15) in the FABQ-PHYS domain. As for the FABQ-WORK domain, in G1, 65.22% (n = 15), and in G2, 73.91% (n = 17), had high scores (≥34). When comparing the results, there was no statistically relevant difference between groups in FABQ-PHYS and FABQ-WORK, with p = 0.162 and p = 0.556, respectively.
In BDI-II questionnaires in G1, 34.78% (n = 8) no symptoms, 34.78% (n = 8) mild, 26.09% (n=6) moderate, and 4.35% (n = 1) severe. In G2, 21.74% (n = 5) were classified as no or minimal symptoms of depression, 52.17% (n = 12) mild depression, 21.74% (n = 5) moderate depression and 4.35% (n = 1) severe depression. About the BAI questionnaire, in G1, 30.43% (n = 7) were classified as no or minimal anxiety symptoms, 26.09% (n=6) mild and moderate anxiety, 17.39% (n=4) severe anxiety. In G2, 30.43% (n = 7) no symptoms, 17.39% (n = 4) mild, 43.48% (n=10) moderate, and 8.7% (n=2) severe. When comparing the results, there was no statistically relevant difference between groups in BDI-II and BAI, with p = 0.690 and p = 0.606 respectively.
All patients presented with some intervertebral disc alteration in the evaluation by MRI of the lumbar spine, described in Table 5. Of the patients with post-surgery PSPS, only 8.70% (n = 2) had compression of the L5 nerve root, with no description of involvement of nerve roots in the lumbar spine. In patients with non-surgical PSPS, 4.35% (n = 1) had L2 root displacement, 17.39% (n = 4) L3 root displacement, 26.09% (n = 6) L4 root displacement, 39.13% (n = 9) L5 root displacement and 4.35% (n = 1) S1 root displacement. About the presence of fissures in the annulus fibrosus, 17.39% (n = 4) of PSPS patients had a radial fissure, one on each disc between L2–S1, while in patients with non-surgical low back pain, there were 21.74% (n = 5) descriptions of fissures on each disc between the L1–S1 levels.
 |
Table 5 Lumbar Magnetic Resonance Findings |
Discussion
This is one of the first studies that evaluates fear-avoidance beliefs and other associated psychological factors, such as anxiety and depression, in patients with post-surgery PSPS in a follow-up several years after surgery and compares with patients diagnosed with non-surgical PSPS. In this study, most patients in both groups had high scores in the FABQ domains, revealing sustained fear-avoidance beliefs in work and physical activities in these patients, but did not have a statistically relevant difference between groups. Fear-avoidance beliefs are derived both from emotional fears of pain and injury and from beliefs based on information about the spine, causes of spinal degeneration, and the importance of pain. They have a negative impact on the treatment of PSPS by increasing the deficiency and prolonging the rehabilitation period.18–20,23,25,26
Compared to this study, the literature on fear-avoidance beliefs in patients with planned lumbar spine surgery or short to mid-term follow-up after surgery, involves assessment in the preoperative period of lumbar spine surgery, as a possible prognostic factor for chronic postoperative pain, associated or not with an assessment in a postoperative follow-up, as a predictor of response to pain treatment.27,28
Studies in patients with CLBP support the conceptual framework of the fear-avoidance model, which implies that fear of pain may lead to avoidance behavior.18–20,23,25,26 Avoidance behavior results in disuse, disability, and depression, and maintains the original negative appraisal in a deleterious cycle.18,20,27 In CLBP, high fear-avoidance belief scores were indicators of poor outcomes in the subacute phase and influenced the treatment response in conservative treatments.18–20 Patients with sustained fear-avoidance beliefs present better results when this behavior is approached in their treatments than when these beliefs are ignored, and they remain in a vicious cycle of social exclusion, making it necessary to adapt treatment strategies if this condition is identified.19,20
In another study performed in the Northeast region of Brazil, there was a prevalence of 60% of post-surgery PSPS in patients who underwent spinal surgery. The patients presented higher rates of neuropathic pain, with severe pain and reduced quality of life and functional capacity.17 In this study, the patients with PSPS and non-surgical PSPS with regular follow-up in the chronic pain outpatient clinic showed high rates of fear-avoidance beliefs, with the presence of anxiety and depression. They were also inserted in the context of absence of physical and work activities, in which most received some type of benefit related to the health condition. These findings corroborate other studies that demonstrated low rates of quality of life, associated with anxiety and depression in these patients, in addition to high rates of absenteeism and a significant socioeconomic impact.17,18
Many patients with chronic pain present associated comorbidities such as depression, anxiety, sleep disorders, and fatigue, which lead to a deterioration in the quality of life in general.29 Persistent pain generates a psychological influence, which can be related to the development of anxiety and depression. Environmental factors play a more significant role in disability and may exacerbate or contribute to the maintenance of the painful condition, affecting the quality of life of these patients.1–4
Previous studies of neural mechanisms underlying pain and negative emotions have shown that the thalamus plays important roles in depression. In particular, the pulvinar nucleus in the thalamus is mutually and extensively connected with the prefrontal cortex, sensory cortex, superior colliculus and amygdala30 and plays very important roles in contextual sensory and emotional response, as well as pain.31–34 In addition, the dysfunction of pulvinar has been reported to be associated with the cognitive and emotional deficits in depression.35,36 In this study, most of the patients in the post-surgery PSPS and non-surgical PSPS group had some degree of anxiety and/or depression as shown in the BAI and BDI-II questionnaires, results similar to other studies,17,37 but did not have a statistically significant difference between groups.
Even though there are few studies in developing countries, it has been demonstrated that the population with CLBP in developing countries also has a higher prevalence of anxiety and depression and a higher risk of developing psychological disorders.37,38 Anxiety and depression are barriers to adherence to treatment in various conditions of chronic pain, worsening the prognosis, and contributing to a loss of functional capacity.39 This relationship between pain and mental health differs from developed countries, as there is a greater impact of factors such as unfavorable socioeconomic conditions, the concern with the maintenance of work that generates family income and also the difficulty of access to adequate treatment that has a strong influence on the psychological condition of this population.
Concerning MRI findings, since the patients underwent MRI in different institutions, there was no standardization of the details of the findings, which did not allow an analysis using validated scores to grade the level of degeneration present in the structures of the lumbar spine. In a study, patients with chronic non-specific LBP, persisting Modic 1, decreasing disc height, and increasing bony endplate lesions were associated with persisting pain, while decrease in signal intensity of the disc was associated with decrease in pain.40
The patients included in this study demonstrate the difficulty of managing the pain of patients with post-surgery PSPS, because even with optimized and individualized treatment for each case, they presented pain levels that ranged from moderate-to-severe intensity most of the time. PSPS is often refractory to drug therapy.4,9 Revisional surgery, to remove epidural fibrosis, is only effective in 5% to 30% of the cases.9 Interventional procedures, like percutaneous adhesiolysis, and physical therapy are supported by moderate to strong evidence.9 While the strongest long-term evidence exists for the effectiveness of spinal cord stimulation (SCS), it is often reserved as a last-resort treatment modality.9 Epiduroscopy, a minimally invasive endoscopic procedure, is a relatively unknown interventional treatment, and when correctly indicated, it demonstrates to be a promising therapy for PSPS.41 Even though it is available in Brazil, in a context of few resources in a developing country and in one of the states with the worst living conditions, more recent techniques, such as epiduroscopy, are not widely available in the public health system as a suggested intervention for this syndrome.
In chronic pain treatment, a common goal is to provide a lasting and significant reduction in suffering, with improvements in overall functioning and health-related quality of life. The subject of fear-avoidance beliefs, even being widely studied in non-surgical PSPS, is not well discussed in post-surgery PSPS. Moreover, there are few studies that analyze fear-avoidance beliefs in association with anxiety and depression in PSPS, even though they are an important part of the psychological assessment. This highlights the importance of this study by assessing fear of pain, anxiety, and depression in PSPS through the specific questionnaires, such as FABQ, BDI-II, and BAI.
As for the limitations of the study, it can be noted the small sample of patients, justified by the fact that the study was conducted at a center specialized in chronic pain, which receives patients diagnosed with PSPS many years after the surgery. Also, about the surgery group, as they are patients who started the follow-up in the chronic pain clinic after surgery, it was not possible to have a pre-surgery baseline questionnaire, which does not allow to conclude if depression/anxiety appeared after surgery or if they already existed before. In addition, it was not possible to retrieve data from the patients’ surgeries to specify the type of spine surgery performed.
Conclusion
Although there was no statistically relevant difference between the PSPS patients with or without surgery in terms of the assessed outcome measures, the described scores for fear-avoidance beliefs, pain, anxiety and depression were high, showing an interference in the daily life activities of those patients, leading these patients to stay further in a cycle of social exclusion. This approach contributes to a better understanding of how this syndrome can influence fear-avoidance beliefs and affect psychological factors of the patients, reinforcing behaviors that are associated with worse results in the treatment of pain and end up prolonging the rehabilitation process. Thus, it makes evident the need for interdisciplinary management of the PSPS, associating interventions that may have positive effects on the combination of physical, psychological, and social interactions that involve the daily living of these patients.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the University Hospital of Federal University of Maranhão (CAAE 22801019.0.0000.5086/Number 3.804.613).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgment
The authors would like to thank the University Hospital, Federal University of Maranhão (HUUFMA) for providing assistance in performing the research.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest in relation to this work.
References
1. Thomson S. Failed back surgery syndrome – definition, epidemiology and demographics. Br J Pain. 2013;7(1):56–59. doi:10.1177/2049463713479096
2. Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res. 2016;9:979–987. doi:10.2147/JPR.S92776
3. Chan C, Peng P. Failed back surgery syndrome. Pain Med. 2011;12(4):577–606. doi:10.1111/j.1526-4637.2011.01089.x
4. Cho JH, Lee JH, Song KS, et al. Treatment outcomes for patients with failed back surgery. Pain Physician. 2017;20(1):29–43. doi:10.36076/ppj.2017.1.E29
5. Rapti E, Damigos D, Apostolara P, Roka V, Tzavara C, Lionis C. Patients with chronic pain: evaluating depression and their quality of life in a single center study in Greece. BMC Psychol. 2019;7(1). doi:10.1186/s40359-019-0366-0
6. Helm IS, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 2012;15(4):435–462. doi:10.36076/ppj.2012/15/E435
7. Klessinger S. Zygapophysial joint pain in post lumbar surgery syndrome. The efficacy of medial branch blocks and radiofrequency neurotomy. Pain Med. 2013;14(3):374–377. doi:10.1111/pme.12012
8. Hayek S, Helm S, Benyamin R, Singh V, Bryce D, Smith H. Effectiveness of spinal endoscopic adhesiolysis in post lumbar surgery syndrome: a systematic review. Pain Physician. 2009;12:419–435. doi:10.36076/ppj.2009/12/419
9. Amirdelfan K, Webster L, Poree L, Sukul V, McRoberts P. Treatment options for failed back surgery syndrome patients with refractory chronic pain: an evidence based approach. Spine. 2017;42(14):S41–S52. doi:10.1097/BRS.0000000000002217
10. Treede RD, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19–27. doi:10.1097/j.pain.0000000000001384
11. Schug SA, Lavand’homme P, Barke A, Korwisi B, Rief W, Treede RD. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. Pain. 2019;160(1):45–52. doi:10.1097/j.pain.0000000000001413
12. Petersen EA, Schatman ME, Sayed D, Deer T. Persistent spinal pain syndrome: new terminology for a new era. J Pain Res. 2021;14:1627–1630. doi:10.2147/JPR.S320923
13. Christelis N, Simpson B, Russo M, et al. Persistent spinal pain syndrome: a proposal for failed back surgery syndrome and ICD-11. Pain Med. 2021;22(4):807–818. doi:10.1093/pm/pnab015
14. Rigoard P, Blond S, David R, Mertens P. Pathophysiological characterisation of back pain generators in failed back surgery syndrome (part B). Neurochirurgie. 2015;61(S1):S35–S44. doi:10.1016/j.neuchi.2014.10.104
15. Clancy C, Quinn A, Wilson F. The aetiologies of failed back surgery syndrome: a systematic review. J Back Musculoskelet Rehabil. 2017;30(3):395–402. doi:10.3233/BMR-150318
16. Rahyussalim AJ, Zufar MLL, Kurniawati T. Significance of the association between disc degeneration changes on imaging and low back pain: a review article. Asian Spine J. 2020;14(2):245–257. doi:10.31616/ASJ.2019.0046
17. Garcia JBS, Rodrigues DP, Leite DRB, et al. Clinical evaluation of the post-laminectomy syndrome in public hospitals in the city of São Luís, Brazil Musculoskeletal Disorders. BMC Res Notes. 2015;8(1). doi:10.1186/s13104-015-1400-9
18. Trinderup JS, Fisker A, Juhl CB, Petersen T. Fear avoidance beliefs as a predictor for long-term sick leave, disability and pain in patients with chronic low back pain. BMC Musculoskelet Disord. 2018;19(1). doi:10.1186/s12891-018-2351-9
19. Rainville J, Smeets RJEM, Bendix T, Tveito TH, Poiraudeau S, Indahl AJ. Fear-avoidance beliefs and pain avoidance in low back pain - Translating research into clinical practice. Spine J. 2011;11(9):895–903. doi:10.1016/j.spinee.2011.08.006
20. Wertli MM, Rasmussen-Barr E, Held U, Weiser S, Bachmann LM, Brunner F. Fear-avoidance beliefs - A moderator of treatment efficacy in patients with low back pain: a systematic review. Spine J. 2014;14(11):2658–2678. doi:10.1016/j.spinee.2014.02.033
21. Cunha J. Manual Da Versão Em Português Das Escalas Beck. Casa do Psicólogo; 2001.
22. Bouhassira D, Attal N, Alchaar H, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005;114(1):29–36. doi:10.1016/j.pain.2004.12.010
23. Waddell G, Newton M, Henderson I, Somerville D, Main CJ, Fear-avoidance beliefs A. Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–168. doi:10.1016/0304-3959(93)90127-B
24. Abreu AM, De, Faria CDC, Cardoso SMV DM, Teixeira-Salmela LF. Versão brasileira do Fear Avoidance Beliefs Questionnaire. Cadernos de Saúde Pública. 2008;24(3):615–623. doi:10.1590/S0102-311X2008000300015
25. Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82(10):973–983. doi:10.1093/ptj/82.10.973
26. Williamson E. Fear Avoidance Beliefs Questionnaire (FABQ). Aust J Physiother. 2006;52(2):149. doi:10.1016/S0004-9514(06)70052-6
27. Burgstaller JM, Wertli MM, Steurer J, Kessels AGH, Held U, Gramke HF. The influence of pre- and postoperative fear avoidance beliefs on postoperative pain and disability in patients with lumbar spinal stenosis. Spine. 2017;42(7):E425–E432. doi:10.1097/BRS.0000000000001845
28. Havakeshian S, Mannion AF. Negative beliefs and psychological disturbance in spine surgery patients: a cause or consequence of a poor treatment outcome? Eur Spine J. 2013;22(12):2827–2835. doi:10.1007/s00586-013-2822-5
29. Lerman SF, Rudich Z, Brill S, Shalev H, Shahar G. Longitudinal associations between depression, anxiety, pain, and pain-related disability in chronic pain patients. Psychosom Med. 2015;77(3):333–341. doi:10.1097/PSY.0000000000000158
30. Zhou N, Masterson SP, Damron JK, Guido W, Bickford ME. The mouse pulvinar nucleus links the lateral extrastriate cortex, striatum, and amygdala. J Neurosci. 2018;38(2):347–362. doi:10.1523/JNEUROSCI.1279-17.2017
31. Chou X, Fang Q, Yan L, et al. Contextual and cross-modality modulation of auditory cortical processing through pulvinar mediated suppression. eLife. 2020;9. doi:10.7554/eLife.54157
32. Fang Q, Chou X, Peng B, Zhong W, Zhang LI, Tao HW. A differential circuit via retino-colliculo-pulvinar pathway enhances feature selectivity in visual cortex through surround suppression. Neuron. 2020;105(2):355–369.e6. doi:10.1016/j.neuron.2019.10.027
33. Ibrahim LA, Mesik L, Ji X, et al. Cross-modality sharpening of visual cortical processing through layer-1-mediated inhibition and disinhibition. Neuron. 2016;89(5):1031–1045. doi:10.1016/j.neuron.2016.01.027
34. Froesel M, Cappe C, Ben Hamed S. A multisensory perspective onto primate pulvinar functions. Neurosci Biobehav Rev. 2021;125:231–243. doi:10.1016/j.neubiorev.2021.02.043
35. Li J, Chen J, Kong W, Li X, Hu B. Abnormal core functional connectivity on the pathology of MDD and antidepressant treatment: a systematic review. J Affect Disord. 2022;296:622–634. doi:10.1016/j.jad.2021.09.074
36. McTeague LM, Rosenberg BM, Lopez JW, et al. Identification of common neural circuit disruptions in emotional processing across psychiatric disorders. Am J Psychiatry. 2020;177(5):411–421. doi:10.1176/appi.ajp.2019.18111271
37. Stubbs B, Koyanagi A, Thompson T, et al. The epidemiology of back pain and its relationship with depression, psychosis, anxiety, sleep disturbances, and stress sensitivity: data from 43 low- and middle-income countries. Gen Hosp Psychiatry. 2016;43:63–70. doi:10.1016/j.genhosppsych.2016.09.008
38. Gerrits MMJG, van Oppen P, van Marwijk HWJ, Penninx BWJH, van der Horst HE. Pain and the onset of depressive and anxiety disorders. Pain. 2014;155(1):53–59. doi:10.1016/j.pain.2013.09.005
39. Tagliaferri SD, Miller CT, Owen PJ, et al. Domains of chronic low back pain and assessing treatment effectiveness: a clinical perspective. Pain Pract. 2020;20(2):211–225. doi:10.1111/papr.12846
40. Luoma K, Vehmas T, Kerttula L, Grönblad M, Rinne E. Chronic low back pain in relation to Modic changes, bony endplate lesions, and disc degeneration in a prospective MRI study. Eur Spine J. 2016;25(9):2873–2881. doi:10.1007/s00586-016-4715-x
41. Geudeke MW, Krediet AC, Bilecen S, Huygen FJPM, Rijsdijk M. Effectiveness of epiduroscopy for patients with failed back surgery syndrome: a systematic review and meta‐analysis. Pain Pract. 2021;21(4):468–481. doi:10.1111/papr.12974
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
