Back to Journals » Clinical Epidemiology » Volume 9
Irritable bowel symptoms and the development of common mental disorders and functional somatic syndromes identified in secondary care – a long-term, population-based study
Authors Poulsen CH , Eplov LF , Hjorthøj C , Eliasen M , Skovbjerg S, Dantoft TM , Schröder A , Jørgensen T
Received 9 May 2017
Accepted for publication 3 July 2017
Published 31 July 2017 Volume 2017:9 Pages 393—402
DOI https://doi.org/10.2147/CLEP.S141344
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Irene Petersen
Chalotte Heinsvig Poulsen,1,2 Lene Falgaard Eplov,2 Carsten Hjorthøj,2 Marie Eliasen,1 Sine Skovbjerg,1 Thomas Meinertz Dantoft,1 Andreas Schröder,3 Torben Jørgensen1,4,5
1Research Centre for Prevention and Health, Capital Region of Denmark, Glostrup, 2Copenhagen University Hospital, Mental Health Centre Copenhagen, Hellerup, 3Research Clinic for Functional Disorders and Psychosomatics, Aarhus University Hospital, Aarhus, 4Department of Public Health, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, 5The Faculty of Medicine, Aalborg University, Aalborg, Denmark
Objective: Irritable bowel syndrome (IBS) is associated with mental vulnerability, and half of patients report comorbid somatic and mental symptoms. We aimed to investigate the relationship between an IBS symptom continuum and the subsequent development of common mental disorders (CMDs) and functional somatic syndromes (FSSs).
Methods and study design: A longitudinal population-based study comprising two 5-year follow-up studies, Dan-MONICA 1 (1982–1987) and Inter99 (1999–2004), recruited from the western part of Copenhagen County. The total study population (n = 7,278) was divided into symptom groups according to the degree of IBS definition fulfillment at baseline and/or follow-up and was followed until December 2013 in Danish central registries. Cox regression was used for the analyses, adjusting for age, sex, length of education and cohort membership. In a subsequent analysis, we adjusted for mental vulnerability as a risk factor for both CMDs and FSSs, including IBS.
Results: Over a 5-year period, 51% patients had no IBS symptoms, 17% patients had IBS symptoms without abdominal pain, 22% patients had IBS symptoms including abdominal pain and 10% patients fulfilled the IBS definition. IBS and IBS symptoms including abdominal pain were significantly associated with the development of CMDs and other FSSs identified in secondary care. When adjusting for mental vulnerability, IBS and IBS symptoms including abdominal pain were no longer associated with CMDs, but the significant relationship to other FSSs remained.
Conclusion: In a clinical setting, the perspective should be broadened to individuals not fulfilling the symptom cluster of IBS but who report frequent abdominal pain. Additionally, it is important to combine symptom-based criteria of IBS with psychosocial markers such as mental vulnerability, because it could guide clinicians in decisions regarding prognosis and treatment.
Keywords: functional gastrointestinal symptoms, abdominal pain, comorbidity, somatization, neuroticism
Introduction
With a prevalence of ~11–16%,1,2 “irritable bowel syndrome” (IBS) is a common functional gastrointestinal disorder that is associated with substantial costs for patients, health care systems and society.3 Approximately half of IBS patients report additional mental and somatic symptoms.4 In a Norwegian population-based study, the presence of comorbid symptoms beyond IBS symptoms was associated with a higher functional impairment, more psychological distress and increased health care use.5 Thus, IBS patients have an increased prevalence of mental disorders, especially anxiety and depression.6 Moreover, IBS has a significant symptom overlap with other functional gastrointestinal disorders such as dyspepsia and functional somatic syndromes (FSSs), eg, fibromyalgia and chronic fatigue syndrome.4,7 These findings illustrate the need for more knowledge about the prognosis of IBS, eg, the potential development of mental and functional comorbidities. This knowledge could guide clinicians and policy makers in decisions regarding treatment, disease prevention and health-promoting strategies.
Most of the literature in this field has certain methodological limitations such as cross-sectional design, selected patient populations and uncertainties in delimitation of the FSSs including IBS.4,6,7 Recently, IBS has been defined as a disorder of gut–brain interaction;8 that is why studies focusing on IBS and subsequent development of mental and functional comorbidities have become of increasing interest.9–12 Nevertheless, the focus is on IBS and “non-IBS” cases, although other population-based studies have shown the importance of broadening the perspective to individuals not fulfilling the symptom cluster of IBS.2,13,14 Additionally, other population-based studies have shown that mental vulnerability, illness anxiety and somatic symptom burden predict development of IBS.15,16 These results indicate the need for addressing both somatic and psychological factors in the early examination of individuals with IBS. Mental vulnerability represents both a symptom state related to somatization and a personality trait related to neuroticism.17 Neuroticism has been shown to be a risk marker in the development of common mental disorders (CMDs).18 In addition, both neuroticism and somatization have been linked to the development of IBS and other FSSs.19,20 Therefore, long-term population-based studies taking psychosocial factors such as mental vulnerability into account are warranted. In the present study, we hypothesized that mental and functional comorbidities also are present among individuals not fulfilling the IBS definition. We therefore broadened the perspective to a continuum of IBS symptoms in a general population. Furthermore, we combined cohort studies with Danish nationwide registers and aimed to investigate the association between IBS symptoms and the subsequent development of CMDs and FSSs other than IBS. Additionally, we hypothesized that mental vulnerability can act as a confounder, because it may contribute to both predisposition and maintenance of IBS symptoms.19 We therefore aimed to investigate these associations both with and without taking mental vulnerability into account.
Methods and study design
The study design has previously been presented as a longitudinal study consisting of two population-based cohorts, Dan-MONICA 1 (1982–1987) and Inter99 (1999–2004), both examined twice with 5-year interval.14 The two cohorts were followed until December 2013 in Danish central registries.
Study populations
The two study populations have previously been described in detail.21,22 They were drawn as age- and sex-matched samples from the Danish Civil Registration System (CRS) using computer-generated random numbers. Both study populations were recruited from the western part of Copenhagen County, which constitutes 7% of the total Danish population and is representative of Danes living in the suburbs. In brief, the Dan-MONICA 1 study population comprised 4,807 men and women of ages 30, 40, 50 and 60 years.21 All individuals were invited for a general health examination conducted in 1982–1984. Individuals not of Danish nationality (n = 226) were excluded, reducing the sample to 4,581. Of them, 3,608 (79%) individuals participated in the baseline study. At the 5-year follow-up, 3,498 individuals were accessible for invitation to a similar health examination. Among them, 2,987 (85%) individuals participated. Individuals not responding were re-invited twice.23 The Inter99 study population comprised 13,016 men and women of ages 30, 35, 40, 45, 50, 55 and 60 years.22 Eligible individuals (n = 12,934) were invited for a health screening program conducted in 1999–2001, and 6,906 (53%) individuals turned up for the examination. Individuals with linguistic barriers, alcoholism or drug abuse were excluded, leaving 6,784 (52.5%) participants in the baseline study. The Inter99 study was designed as an intervention study for prevention of ischemic heart disease. The participants were therefore divided into two random samples: a high-intensity intervention group (A) and a low-intensity intervention group (B). At the 5-year follow-up, 6,536 individuals were accessible for invitation to the second study. Among them, 4,513 (69%) individuals participated. Individuals not responding were re-invited.24 Both cohorts comprised information on self-reported IBS symptoms from a questionnaire and were pooled in the present study, reducing the sample to 7,500 individuals who participated both at baseline and at 5-year follow-up. The data from Dan-MONICA 1 and Inter99 are available for researchers who meet the criteria, for access to confidential data contact information: [email protected].
IBS symptom groups
The used IBS definition was based on a symptom cluster of frequent self-reported IBS symptoms in the past 12 months found in a previous study of Dan-MONICA 1: “Individuals stating that they often experience both abdominal pain and distension and, additionally, either borborygmus or altering stool consistency, or both”.25 Frequent IBS symptoms were defined as experiencing them at least once a month (abdominal pain) or frequently or daily/almost constantly (distension, borborymus and altering stool consistency). The total study population was divided into four symptom groups according to the degree of IBS definition fulfillment at baseline and/or 5 years follow-up: 1) IBS; 2) IBS symptoms including abdominal pain; 3) IBS symptoms without abdominal pain and 4) reference group without IBS symptoms. Individuals in group 1 fulfilled the IBS definition at baseline and/or 5-year follow-up. Individuals in group 2 and 3 had IBS symptoms with and without abdominal pain at baseline and/or at 5-year follow-up but did not fulfill the IBS definition at any time. The reference group had no IBS symptoms at baseline or at 5-year follow-up. The symptom groups have previously been presented. The study showed that fulfillment of the used IBS definition delimitated individuals not associated with severe gastrointestinal diseases including inflammatory bowel disorders.14 In total, 222 individuals were excluded from the study population due to missing data on IBS symptoms, reducing the sample to 7,278 individuals.
Outcomes
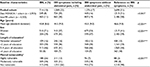
The total study population was linked through the unique personal identification number to the CRS, the Danish Psychiatric Central Research Register (PCRR) and the National Patient Register (NPR). The personal identification number is used in all the registries, insuring complete linkage between databases. The information in the CRS is considered to be of high validity.26 Although both the content and the definitions of single variables may have changed over time, the PCRR and the NPR are considered as valuable tools in epidemiological research.27,28 In this study, we obtained information on psychiatric and somatic inpatient admissions from the PCRR since 1969 and the NPR since 1977 until the end of register extraction (December 31, 2013). From 1995 and onward, the registers also included information of outpatient treatment and emergency room contacts. We based the delimitation of CMDs and other FSSs on systematic reviews and recent register-based studies on the most common mental and functional comorbidities in IBS.4,6,7,10,29 Thus, CMDs were defined as first hospital contact with a diagnosis of a neurotic, stress-related, anxiety or mood affective disorder classified according to the International Classification of Diseases revision 8 (ICD-8) and International Classification of Diseases revision 10 (ICD-10; Table 1). Hypochondriasis was included as an anxiety disorder, because both scientific evidence and clinical evidence support the view that it is a distinct “health anxiety” disorder that can be treated effectively and only partly overlaps with FSSs.30 Other FSSs were defined as first hospital contact for a diagnosis of interstitial cystitis, postviral fatigue syndrome, malaise and fatigue, myalgia/rheumatism unspecified, fibromyalgia, pain not elsewhere classified, temporomandibular joint disorders, sprain and strain of cervical spine (whiplash), somatoform disorders and neurasthenia classified according to ICD-8 and ICD-10 (Table 1).4,6,7,10 In the delimitation, we included unspecific symptom codes due to uncertainties in the registration practice of the syndrome codes.10 We did not include functional gastrointestinal disorders due to the significant symptom overlap with IBS.31,32
Covariates
Age at health examination and sex were obtained from the CRS. Education was self-reported and obtained from the questionnaires used at the health examinations.21,22 Length of education was categorized as no/under education, <2 years of education (short education, special workers or apprentices), 2–4 years of education (middle length education or technician training) and >4 years of education (academic or higher education). Only eight individuals were under education, and they were categorized as individuals not having an education. The Mental Vulnerability Questionnaire was developed by the Military Psychological Services in Denmark in the 1960s and used as a screening instrument to assess mental fitness for military service. The questionnaire was similar to international instruments developed in the same period.33,34 We used the 12-item Mental Vulnerability Scale (Table S1) that was developed from a 22-item scale derived from the original 27-item Mental Vulnerability Questionnaire.35 The 12-item Mental Vulnerability Scale has been shown to be a predictor of several health outcomes, including IBS, upper dyspepsia and depression.15,36–38 Moreover, the 12-item scale has been validated as a reliable and stable measure of overall mental vulnerability.17 Mental vulnerability was categorized as not vulnerable (zero to two affirmative answers), moderately vulnerable (three to four affirmative answers) and highly vulnerable (five or more affirmative answers).
Statistical analysis
We analyzed data using SAS 9.3 software (SAS Institute Inc., Cary, NC, USA). The associations between each of the symptom groups, CMDs and FSSs were assessed using Cox proportional hazards regression models to estimate hazard ratios (HRs) with 95% confidence intervals (CIs). Follow-up time was calculated as the time from the 5-year follow-up assessment to event or censoring, because the exposed individuals were defined according to IBS symptoms at both baseline and 5-year follow-up. Individuals who had a diagnosis of a CMD (n = 249) or an FSS (n = 216) before the follow-up assessment were excluded. Furthermore, a total of 282 and 285 individuals were censored due to migration before the follow-up study, leaving 6,747 and 6,777 individuals for the primary analyses of CMDs and FSSs, respectively. Individuals were followed until first contact to the secondary health care system with a CMD or an FSS diagnosis and censored at first migration, death or December 31, 2013, whichever came first. Analyses were adjusted for cohort membership, which was created as a three-level variable consisting of Dan-MONICA 1 and Inter99 intervention group (A) and (B). Additionally, analyses were adjusted for age, sex and length of education. Mental vulnerability can be viewed as a confounder on the outcomes. In a subsequent analysis, we therefore adjusted the results for mental vulnerability and presented the results both with and without this additional adjustment. Furthermore, we conducted a sensitivity analysis where the item “Do you often have pain in different parts of your body, eg, your stomach, neck, back or chest?” was excluded from the 12-item mental vulnerability scale due to the possible symptom overlap with the abdominal pain item in the IBS definition. Moreover, we performed an additional Cox regression to investigate the associations between mental vulnerability and the outcomes. The associations were investigated both with and without taking IBS at baseline into account.
Ethical approval
Dan-MONICA 1 and Inter99 were approved by the local ethical committee at the time of data collection.21,22 The participants were informed that all information was to be used for research purposes only and gave written informed consent. The present study was approved by the Danish Data Protection Agency (2012-58-0009).
Results
The IBS symptom groups and the baseline characteristics are presented in Table 2. Further details can be found elsewhere.14 In the pooled cohort, 714 (10%) patients had IBS, 1,589 (22%) patients had IBS symptoms including abdominal pain, 1,276 (17%) patients had IBS symptoms without abdominal pain and 3,699 (51%) patients reported no IBS symptoms over the 5-year period. At baseline, mental vulnerability significantly increased with increasing fulfillment of the IBS definition. In total, 56% of patients with IBS were moderately/highly vulnerable, whereas 10% of those without IBS symptoms were moderately/highly vulnerable (Table 2).
Development of CMDs and FSSs identified in secondary care
There was an increased risk of CMD development in secondary care both among individuals with IBS and IBS symptoms including abdominal pain (HR: 1.74 [95% CI: 1.18–2.56] and HR: 1.74 [95% CI: 1.31–2.31], respectively; Table 3) compared to individuals reporting no IBS symptoms. IBS symptoms without abdominal pain were not associated with subsequent registration of CMDs identified in secondary care (HR: 1.23 [95% CI: 0.87–1.73]; Table 3). When additionally adjusting the results for mental vulnerability, the HR estimates decreased, and overall, the IBS symptom groups were not significantly associated with CMD development in secondary care (Table 3). The sensitivity analysis using the reduced mental vulnerability scale showed an increased risk of CMD development among individuals with IBS symptoms including abdominal pain, but the overall association between symptom groups and the outcome remained insignificant. Across all symptom groups, depression, other anxiety, reaction to severe stress and adjustment disorders were the most frequent CMDs registered in secondary care (data not shown). There was an increased risk of FSS development in secondary care both among individuals with IBS and IBS symptoms including abdominal pain (HR: 1.94 [95% CI: 1.34–2.80] and HR: 1.76 [95% CI: 1.31–2.35], respectively; Table 4) compared to individuals reporting no IBS symptoms. IBS symptoms without abdominal pain were not associated with subsequent registration of FSSs identified in secondary care (HR: 1.32 [95% CI: 0.94–1.85]; Table 4). When additionally adjusting the results for mental vulnerability, the HR estimates decreased, but the overall association between symptom groups and the development of FSSs remained statistically significant (Table 4). The sensitivity analysis using the reduced mental vulnerability scale slightly increased the HR estimates, and the association remained significant (Table 4). In the registration of FSSs in secondary care, the syndrome codes were infrequently used compared to the unspecified symptom codes. Across all symptom groups, pain not elsewhere classified, myalgia/rheumatism unspecified and malaise and fatigue were the most frequently registered diagnoses (data not shown).
There was no statistically significant interaction between the IBS symptom groups and cohort membership on any outcome (p > 0.05). A high/moderate mental vulnerability was statistically significantly associated with subsequent CMDs and FSSs (HR: 2.72 [95% CI: 2.14–3.45] and HR: 1.97 [95% CI: 1.54–2.52], respectively). When accounting for the IBS symptom group at baseline, the estimates slightly decreased (HR: 2.53 [95% CI: 1.96–3.26] and HR: 1.72 [95% CI: 1.32–2.24], respectively), but the overall significant association between mental vulnerability and the outcomes remained (both p < 0.001).
Discussion
Individuals both fulfilling and not fulfilling the IBS definition but who reported IBS symptoms including abdominal pain more often developed CMDs and FSSs identified in secondary care compared to individuals reporting no IBS symptoms. Individuals with IBS symptoms without abdominal pain were not associated with subsequent CMDs or FSSs. When accounting for mental vulnerability, the estimates decreased and only the associations between IBS, IBS symptoms including abdominal pain and the development of other FSSs remained significant.
Interpretation and explanation of the findings
Mental vulnerability is defined as a low threshold for susceptibility.38 Psychometric evaluation has shown that the 12-item mental vulnerability scale has a strong association with somatization and the personality trait neuroticism.17 Somatization refers to a tendency to experience and communicate somatic distress in response to psychosocial stress and seek medical help for it.39 Neuroticism is widely defined as a tendency to experience negative emotions and bodily sensations, especially when threatened, frustrated or facing loss.18 In this study, mental vulnerability showed to be a strong predictor of both outcomes, independent of the presence of IBS. The primary results indicated that when accounting for the tendency to be mentally vulnerable, individuals reporting IBS symptoms in a general population were not more likely to be classified in secondary health care with CMDs than individuals without IBS symptoms. In addition, both neuroticism and somatization have been linked to explain the frequent comorbid symptoms and related functional comorbidities of IBS.4,20 Our study indicated that the association between IBS symptoms and the subsequent registration of other FSSs could not be explained by mental vulnerability only.
Relation to other studies
In this longitudinal study of a general adult Danish population, we found that 10% fulfilled the definition of IBS over a 5-year follow-up period. Moreover, 56% of these individuals reported comorbid symptoms and traits equivalent to a moderate or high mental vulnerability. Mental vulnerability has been shown to be a predictor of increased health care use and a broad variety of health outcomes.37,40,41 In this study, we confirmed previous longitudinal findings that IBS is associated with subsequent development of CMDs.9,11,12 For example, a large register-based study from Taiwan showed an increased risk of depression, anxiety, sleep and bipolar disorders following a diagnosis of IBS.9 However, the study was based on a selected patient population newly diagnosed with IBS caused by gastroenteritis. In our population-based sample, we showed this increased risk also among individuals not fulfilling the symptom cluster of IBS over a 5-year period but who reported frequent abdominal pain. A recent nation-wide Italian cohort study found a significant relationship between migraine/headache, IBS and fatigue among primary care patients and later development of depressive disorders in general practice.42 Our study added that the increased risk of CMDs in secondary care is likely to be explained by subgroups of individuals with IBS symptoms who also are mentally vulnerable.
An 8-year follow-up study of 493 Swedish IBS patients identified in primary care showed a similar mental and functional comorbidity pattern in secondary care compared to our study.10 However, the two studies were difficult to compare due to different methods, differences in delimitation of IBS and lack of information about the specific register diagnoses used. In our population-based study, we showed an increased risk of FSS development also among individuals not fulfilling the IBS definition over a 5-year period but who reported frequent abdominal pain. These findings support the growing recognition that there is a significant overlap among FSSs with persistent pain as a predominant feature. Moreover, there has been a growing recognition of a shared underlying mechanism, primarily central sensitization of the central nervous system.43 In addition, bidirectional communication from the gut to the brain and from the brain to the enteric nervous system is likely to explain symptoms outside the gastrointestinal system.44 Although the precise mechanisms are not fully understood, it is possible that these “gut–brain” pathways play a role in the development of mental comorbidity and functional comorbidity at least in subgroups of patients with IBS.
Methodological considerations
Until now, few population-based studies have investigated the associations between IBS and subsequent CMDs and FSSs identified in secondary care. Furthermore, none of these studies have included mental vulnerability or performed subgroup analyses based on the nature of IBS symptom reporting.9–12 In this study, the exposure was based on the 5-year follow-up period and we focused on the long-term incidence of CMDs and FSSs in the two time periods 1987–2014 and 2004–2014. The linkage to Danish national registers ensured accurate and precise information about deaths, migration and date of first hospital contact with a specific diagnostic code. The diagnoses in the registers were registered by medical specialists in secondary care.
The available data were not collected to define IBS according to the present Rome IV criteria.8 The Rome criteria developed at the time of data collection were not sufficient to define IBS in a general population (abdominal pain was not mandatory and the criteria did not require any frequency of symptoms).45 Therefore, we used an IBS definition defined according to valid statistical criteria in population-based data.25,46 However, it was a limitation that we only had information on self-reported IBS symptoms in the past 12 months and no information on symptom duration and severity. This could have introduced some misclassification of IBS. Nevertheless, in this study, we focused on self-reported IBS symptoms in a general population and not on incident IBS patients. With this symptom approach, we did not delimitate IBS from other functional gastrointestinal disorders.
The focus on IBS symptoms among individuals participating in two general health examinations could have introduced some selection bias toward a more healthy population sample. Some of the nonparticipants and the nonattenders to the 5-year follow-up studies could have been individuals with persistent and severe symptoms. Moreover, the exclusion of previous diagnoses with CMDs and FSSs could have excluded the most vulnerable individuals. This could imply an underestimation of the association between fulfillment of IBS and the outcomes. The possible selection bias may be largest in the Inter99 study due to the low participation rate and its intervention design. However, we found no significant interaction between cohort membership and the IBS symptom groups in relation to the outcomes, indicating that this selection bias was of lower importance. Nevertheless, Koloski et al. have shown that gut-brain pathways in IBS are bi-directional.12 Therefore, the study design limited the focus to individuals with IBS developing mental and functional comorbidities later in life. Individuals were randomly selected from the CRS and were therefore equally likely to be selected to the study. However, only individuals of age 30–60 years were invited, and individuals not of Danish nationality were excluded, because the study is primarily generalizable to an adult Danish-speaking population. In relation to the outcomes, we only had information about severe CMDs treated in secondary care and we did not have information about milder versions of these conditions treated in primary care. Moreover, the registration practice of FSSs across medical specialties is unclear and may have changed over time. We addressed this limitation by including unspecific symptom diagnoses in our delimitation of FSSs. As expected, the syndrome diagnoses were infrequently used compared to the unspecific symptom diagnoses. Finally, we included few potential confounders due to uncertainties about risk factors to IBS and did not address other possible explaining factors such as gastrointestinal infections,16 food intolerances47 and use of medicine.48
Conclusion and implications
Mental vulnerability may explain the increased risk of CMD development in secondary care among individuals reporting IBS symptoms. Moreover, individuals with abdominal pain including those fulfilling the IBS definition have an increased risk of FSS development in secondary care, and this association cannot be explained by mental vulnerability only. These findings support the recognition of a significant overlap among FSSs. In a clinical setting, it is important to broaden the perspective to patients not fulfilling the symptom cluster of IBS and especially patients reporting frequent abdominal pain. Additionally, it is important to combine symptom-based criteria of IBS with psychosocial markers such as mental vulnerability, because it could guide clinicians in decisions regarding prognosis and treatment.
Acknowledgments
The authors would like to thank the participants and the team behind the Dan-MONICA 1 and the Inter99 study at the Research Centre for Prevention and Health, the Capital Region of Denmark, for their thorough work in collecting and assuring data of high quality. This study was a part of the Danish Study of Functional Disorders (DanFunD) funded by the Lundbeck Foundation (grant number R155-2013-14070) and TrygFonden (grant number 7-11-0213). The DanFunD scientific management group consists of Professor MD DMSc Torben Jørgensen (PI), Professor MD DMSc Per Fink, Senior Consultant MD PhD Lene Falgaard Eplov, Senior Researcher MSc PhD Sine Skovbjerg and Head of Research MD DMSc Jesper Mehlsen.
Author contributions
CHP contributed to the conception and design of the study, performed and interpreted all the analyses of the data and drafted the manuscript. TJ and LFE contributed to the conception and design of the study and interpretation of the data and provided supervision. CH contributed to the conception and design of the study and interpretation of the data and supervised the statistical analyses. ME contributed to the conception and design of the study and interpretation of the data. TMD, SS and AS contributed to the conception and design of the study. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80. | ||
Krogsgaard LR, Engsbro AL, Bytzer P. The epidemiology of irritable bowel syndrome in Denmark. A population-based survey in adults ≤50 years of age. Scand J Gastroenterol. 2013;48(5):523–529. | ||
Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther. 2014;40(9):1023–1034. | ||
Riedl A, Schmidtmann M, Stengel A, et al. Somatic comorbidities of irritable bowel syndrome: a systematic analysis. J Psychosom Res. 2008;64(6):573–582. | ||
Vandvik PO, Lydersen S, Farup PG. Prevalence, comorbidity and impact of irritable bowel syndrome in Norway. Scand J Gastroenterol. 2006;41(6):650–656. | ||
Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20(20):6024–6030. | ||
Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002;122(4):1140–1156. | ||
Drossman DA, Hasler WL. Rome IV – functional GI disorders: disorders of Gut-Brain Interaction. Gastroenterology. 2016;150(6):1257–1261. | ||
Lee Y-T, Hu L-Y, Shen C-C, et al. Risk of psychiatric disorders following irritable bowel syndrome: a nationwide population-based cohort study. PLoS One. 2015;10(7):e0133283. | ||
Faresjö Å, Grodzinsky E, Hallert C, Timpka T. Patients with irritable bowel syndrome are more burdened by co-morbidity and worry about serious diseases than healthy controls- eight years follow-up of IBS patients in primary care. BMC Public Health. 2013;13:1. | ||
Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther. 2016;44(6):592–600. | ||
Koloski NA, Jones M, Kalantar J, Weltman M, Zaguirre J, Talley NJ. The brain-gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut. 2012;61(9):1284–1290. | ||
Talley NJ, Weaver AL, Zinsmeister AR, Melton LJI. Onset and disappearance of gastrointestinal symptoms and functional gastrointestinal disorders. Am J Epidemiol. 1992;136(2):165–177. | ||
Heinsvig Poulsen C, Falgaard Eplov L, Hjorthøj C, et al. Gastrointestinal symptoms related to the irritable bowel syndrome – a longitudinal population-based register study. Scand J Gastroenterol. 2016;51(4):420–426. | ||
Kay L, Jørgensen T, Jensen KH. The epidemiology of irritable bowel syndrome in a random population: prevalence, incidence, natural history and risk factors. J Intern Med. 1994;236(1):23–30. | ||
Löwe B, Lohse A, Andresen V, Vettorazzi E, Rose M, Broicher W. The development of irritable bowel syndrome: a prospective community-based cohort study. Am J Gastroenterol. 2016;111(9):1320–1329. | ||
Eplov LF, Petersen J, Jørgensen T, et al. The Mental Vulnerability Questionnaire: a psychometric evaluation. Scand J Psychol. 2010;51(6):548–554. | ||
Ormel J, Jeronimus BF, Kotov R, et al. Neuroticism and common mental disorders: meaning and utility of a complex relationship. Clin Psychol Rev. 2013;33(5):686–697. | ||
Hauser G, Pletikosic S, Tkalcic M. Cognitive behavioral approach to understanding irritable bowel syndrome. World J Gastroenterol. 2014;20(22):6744. | ||
Muscatello MRA, Bruno A, Mento C, Pandolfo G, Zoccali RA. Personality traits and emotional patterns in irritable bowel syndrome. World J Gastroenterol. 2016;22(28):6402. | ||
Jørgensen T. Prevalence of gallstones in a Danish population. Am J Epidemiol. 1987;126(5):912–921. | ||
Jørgensen T, Borch-Johnsen K, Thomsen TF, Ibsen H, Glümer C, Pisinger C. A randomized non-pharmacological intervention study for prevention of ischaemic heart disease: baseline results Inter99. Eur J Cardiovasc Prev Rehabil. 2003;10(5):377–386. | ||
Jensen KH, Jørgensen T. Incidence of gallstones in a Danish population. Gastroenterology. 1991;100(3):790–794. | ||
Jørgensen T, Jacobsen RK, Toft U, Aadahl M, Glümer C, Pisinger C. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ. 2014;348:g3617. | ||
Kay L, Jørgensen T. Redefining abdominal syndromes. Results of a population-based study. Scand J Gastroenterol. 1996;31(5):469–475. | ||
Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(7 suppl):22–25. | ||
Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7 suppl):54–57. | ||
Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 suppl):30–33. | ||
Liu C-J, Hu L-Y, Yeh C-M, et al. Irritable brain caused by irritable bowel? A nationwide analysis for irritable bowel syndrome and risk of bipolar disorder. PLoS One. 2015;10(3):e0118209. | ||
Schröder A, Dimsdale JE. Management of Somatic Symptoms. Scientific American Medicine. 2014. | ||
Agréus L, Svärdsudd K, Nyrén O, Tibblin G. Irritable bowel syndrome and dyspepsia in the general population: overlap and lack of stability over time. Gastroenterology. 1995;109(3):671–680. | ||
Rasmussen S, Jensen TH, Henriksen SL, et al. Overlap of symptoms of gastroesophageal reflux disease, dyspepsia and irritable bowel syndrome in the general population. Scand J Gastroenterol. 2015;50(2):162–169. | ||
Langner TS. A twenty-two item screening score of psychiatric symptoms indicating impairment. J Health Hum Behav. 1962;3:269–276. | ||
Levav I, Arnon A, Portnoy A. Two shortened versions of the Cornell Medical Index – a new test of their validity. Int J Epidemiol. 1977;6(2):135–141. | ||
Andersen E, Sørensen S. Måling Af Psykisk Sårbarhed. En Analyse Af Visse Egenskaber Ved Sårbarhedstesten. Universitetets Statistiske Institut, København. Research Report Nr. 58. 1979. Danish. | ||
Kay L, Jørgensen T. Epidemiology of upper dyspepsia in a random population. Prevalence, incidence, natural history, and risk factors. Scand J Gastroenterol. 1994;29(1):2–6. | ||
Østergaard D, Dalton SO, Bidstrup PE, et al. Mental vulnerability as a risk factor for depression: a prospective cohort study in Denmark. Int J Soc Psychiatry. 2012;58(3):306–314. | ||
Kühl PH, Martini S. Psykisk Sårbare. Sociale Livsbetingelser. [Psychically Vulnerable Persons. Their Social and Living Conditions]. Denmark: The Danish National Institute of Social Research; 1981. | ||
Lipowski ZJ. Somatization: the concept and its clinical application. Am J Psychiatry. 1988;145(11):1358–1368. | ||
Eplov LF, Jørgensen T, Birket-Smith M, Petersen J, Johansen C, Mortensen EL. Mental vulnerability – a risk factor for ischemic heart disease. J Psychosom Res. 2006;60(2):169–176. | ||
Thorvaldsen P, Sørensen EB. Psychological vulnerability as a predictor for short-term outcome in lumbar spine surgery. A prospective study (Part II). Acta Neurochir (Wien). 1990;102(1–2):58–61. | ||
Castellini G, Pecchioli S, Cricelli I, et al. How to early recognize mood disorders in primary care: a nationwide, population-based, cohort study. Eur Psychiatry. 2016;37:63–69. | ||
Yunus M. Editorial review (thematic issue: an update on central sensitivity syndromes and the issues of nosology and psychobiology). Curr Rheumatol Rev. 2015;11(2):70–85. | ||
Coss-Adame E, Rao SSC. Brain and gut interactions in irritable bowel syndrome: new paradigms and new understandings. Curr Gastroenterol Rep. 2014;16(4):379. | ||
Kay L, Jørgensen T, Lanng C. Irritable bowel syndrome: which definitions are consistent? J Intern Med. 1998;244(6):489–494. | ||
Kendell RE. Clinical validity. Psychol Med. 1989;19(1):45–55. | ||
Mansueto P, D’Alcamo A, Seidita A, Carroccio A. Food allergy in irritable bowel syndrome: the case of non-celiac wheat sensitivity. World J Gastroenterol. 2015;21(23):7089–7109. | ||
Faresjo A, Grodzinsky E, Johansson S, Wallander M-A, Faresjo T, Timpka T. Self-reported use of pharmaceuticals among patients with irritable bowel syndrome in primary care. J Manag Care Pharm. 2008;14(9):870–877. |
Supplementary material
  | Table S1 The 12-item mental vulnerability scale |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.